- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
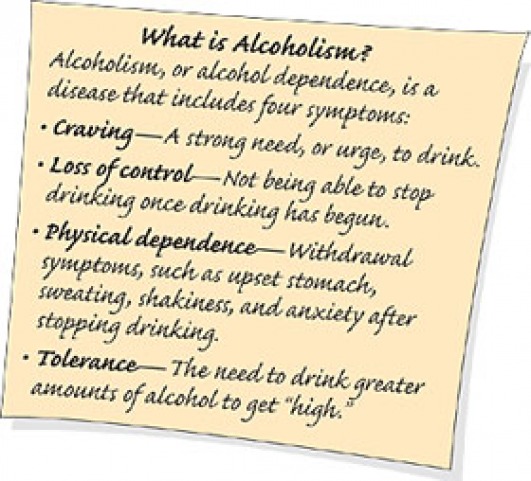
Alcoholism and Alcohol Abuse
Alcohol use disorder (AUD) is a medical condition that doctors diagnose when a patient’s drinking causes distress or harm. The condition can range from mild to severe and is diagnosed when a patient answers “yes” to two or more of the following questions.
In the past year, have you:
- Had times when you ended up drinking more, or longer than you intended?
- More than once wanted to cut down or stop drinking, or tried to, but couldn’t?
- Spent a lot of time drinking? Or being sick or getting over the aftereffects?
- Experienced craving — a strong need, or urge, to drink?
- Found that drinking — or being sick from drinking — often interfered with taking care of your home or family? Or caused job troubles? Or schoolproblems?
- Continued to drink even though it was causing trouble with your family or friends?
- Given up or cut back on activities that were important or interesting to you, or gave you pleasure, in order to drink?
- More than once gotten into situations while or after drinking that increased your chances of getting hurt (such as driving, swimming, using machinery, walking in a dangerous area, or having unsafe sex)?
- Continued to drink even though it was making you feel depressed or anxious or adding to another health problem? Or after having had a memory blackout?
- Had to drink much more than you once did to get the effect you want? Or found that your usual number of drinks had much less effect than before?
- Found that when the effects of alcohol were wearing off, you had withdrawal symptoms, such as trouble sleeping, shakiness, irritability, anxiety, depression, restlessness, nausea, or sweating? Or sensed things that were not there?
If you answer
Yes to 2-3 of these questions, you have a mild disorder.
Yes to 4-5 means moderate
Yes to 6 or more means severe.
Denial is a hallmark of alcoholism and people with alcohol dependence tend to minimize the extent of their drinking.
Introduction
Alcoholism is characterized by a preoccupation with alcohol and impaired control over alcohol intake. Alcoholism is a chronic, often progressive disease. Left untreated, alcoholism can be fatal.
You may continue to abuse alcohol despite serious adverse health, personal, work-related and financial consequences. Alcoholism usually involves physical dependence on alcohol, but genetic, psychological and social factors contribute to the addiction as well.
It's possible to have a problem with alcohol, but not display all the characteristics of alcoholism. This is known as "alcohol abuse," which means you engage in excessive drinking that causes health or social problems, but you aren't dependent on alcohol and haven't fully lost control over the use of alcohol.
According to the National Council on Alcoholism and Drug Dependence, almost 18 million Americans abuse alcohol. Each year more than 100,000 Americans die of alcohol-related causes. Alcohol is a factor in nearly half of all U.S. traffic deaths.
Alcoholism and alcohol abuse cause major social, economic and public health problems. Various treatments are available, and self-help groups can provide ongoing support for people recovering from alcoholism.
Signs and symptoms
Before treatment or recovery, most people with alcoholism deny that they have a drinking problem. Other indications of alcoholism and alcohol abuse include:
- Drinking alone or in secret
- Being unable to limit the amount of alcohol you drink
- Not remembering conversations or commitments, sometimes referred to as "blacking out"
- Making a ritual of having drinks before, with or after dinner and becoming annoyed when this ritual is disturbed or questioned
- Losing interest in activities and hobbies that used to bring pleasure
- Feeling a need or compulsion to drink
- Irritability when your usual drinking time nears, especially if alcohol isn't available
- Keeping alcohol in unlikely places at home, at work or in the car
- Gulping drinks, ordering doubles, becoming intoxicated intentionally to feel good or drinking to feel "normal"
- Having legal problems or problems with relationships, employment or finances
- Building a tolerance to alcohol so that you need an increasing number of drinks to feel alcohol's effects
- Experiencing physical withdrawal symptoms — such as nausea, sweating and shaking — if you don't drink
If you've ever wondered if your own alcohol consumption crosses the line of abuse or dependence, ask yourself these questions: The "CAGE" questions:
- Do you think you need to cut back on your alcohol consumption?
- Are you annoyed when other people comment on or criticize your drinking habits?
- Do you feel guilty about your drinking?
- Do you need a drink as soon as you get up? "Eye opener"
Causes
Alcohol addiction — physical dependence on alcohol — occurs gradually as drinking alcohol alters the balance of some chemicals in your brain, such as gamma-aminobutyric acid (GABA), which inhibits impulsiveness, and glutamate, which excites the nervous system. Alcohol also raises the levels of dopamine in the brain, which is associated with the pleasurable aspects of drinking alcohol. Excessive, long-term drinking can deplete or increase the levels of some of these chemicals, causing your body to crave alcohol to restore good feelings or to avoid negative feelings.
Other factors can lead to excessive drinking that contributes to the addiction process. These include:
- Genetics. Certain genetic factors may cause a person to be vulnerable to alcoholism or other addictions.
- Emotional state. High levels of stress, anxiety or emotional pain can lead some people to drink alcohol to block out the turmoil. Certain stress hormones may be associated with alcoholism.
- Psychological factors. Having low-self esteem or depression may make you more likely to abuse alcohol. Having friends or a close partner who drinks regularly — but who may not abuse alcohol — could promote excessive drinking on your part. It may be difficult for you to distance yourself from these "enablers" or at least from their drinking habits.
- Social and cultural factors. The glamorous way that drinking alcohol is portrayed in advertising and in the media may send the message that it's OK to drink excessively.
Steady drinking over time can produce a physical dependence on alcohol. Drinking more than 15 drinks a week for men or 12 drinks a week for women increases the risk of developing dependence on alcohol. However, drinking by itself is just one of the risk factors that contribute to alcoholism. Other risk factors include:
- Age. People who begin drinking at an early age — by age 16 or earlier — are at a higher risk of alcohol dependence or abuse.
- Genetics. Your genetic makeup may increase your risk of alcohol dependency.
- Sex. Men are more likely to become dependent on or abuse alcohol than are women.
- Family history. The risk of alcoholism is higher for people who had a parent or parents who abused alcohol.
- Emotional disorders. Being severely depressed or having anxiety places you at a greater risk of abusing alcohol. Adults with attention-deficit/hyperactivity disorder also may be more likely to become dependent on alcohol.
When to seek medical advice
Because denial is frequently a characteristic of alcoholism, it's unlikely that people who are dependent on or who abuse alcohol will seek medical treatment on their own. Often it takes family members, friends or co-workers to persuade them to undergo screening for alcoholism or to seek treatment.
If you feel that your drinking is a problem — you feel guilty about your drinking and just can't control it — talk with your doctor about treatment options. Also talk with your doctor if you find that you need a drink first thing in the morning and that you need an increasing amount of alcohol before you start feeling its effects.
Screening and diagnosis
It's often difficult for doctors to decide which people to screen for an alcohol problem. For example, signs and symptoms such as memory loss or falling might be the result of aging rather than indications of alcohol abuse. Or people may complain to doctors about digestive problems or pain or weakness, but never reveal their abuse of alcohol.
A doctor who suspects an alcohol problem may ask a number of questions regarding drinking habits in order to get an indication of the amount of drinking. If answers to those questions indicate possible alcoholism or alcohol abuse, the doctor may do a short screening test using a standardized questionnaire.
Blood alcohol tests aren't useful in diagnosing alcoholism because the tests indicate consumption only at that particular time. They don't offer clues about long-term alcohol use. Other blood tests that measure the size of red blood cells, which increase with long-term alcohol use, and a factor known as carbohydrate-deficient transferrin may indicate heavy alcohol consumption. Sometimes other tests indicate health problems that may be alcohol related, such as tests showing liver damage or reduced testosterone levels in men.
Denial is a hallmark of alcoholism and people with alcohol dependence tend to minimize the extent of their drinking. The doctor may ask for permission to speak with family members or friends. Concerned family members may also contact the doctor on their own to discuss their concerns. However, confidentiality rules prevent the doctor from giving out any information without consent.
Complications
Alcohol depresses your central nervous system. In some people, the initial reaction may be stimulation. But as you continue to drink, you become sedated. Alcohol lowers your inhibitions and affects your thoughts, emotions and judgment. In sufficient amounts, alcohol impairs speech and muscle coordination. Too much alcohol can severely depress the vital centers of your brain. A heavy drinking binge may even cause a life-threatening coma.
Over time, excessive alcohol use can cause fatigue and short-term memory loss, as well as weakness and paralysis of your eye muscles. Other severe health effects may include:
- Liver disorders. Drinking heavily can cause alcoholic hepatitis, an inflammation of the liver. Signs and symptoms may include loss of appetite, nausea, vomiting, abdominal pain and tenderness, fever, yellowing of the skin (jaundice) and sometimes confusion. After years of drinking, hepatitis may lead to cirrhosis, the irreversible and progressive destruction and scarring of liver tissue.
- Gastrointestinal problems. Alcohol can result in inflammation of the lining of the stomach (gastritis) and interfere with absorption of the B vitamins — particularly folic acid and thiamin — and other nutrients. Heavy drinking can also damage your pancreas, which produces the hormones that regulate your metabolism and the enzymes that help digest fats, proteins and carbohydrates.
- Cardiovascular problems. Excessive drinking can lead to high blood pressure and damage your heart muscle (cardiomyopathy). These conditions can increase your risk of heart failure or stroke.
- Diabetes complications. Alcohol prevents the release of glucose from your liver and can increase the risk of low blood sugar (hypoglycemia). This is dangerous if you have diabetes and are already taking insulin to lower your blood sugar level.
- Sexual function and menstruation. Alcohol abuse can cause erectile dysfunction in men. In women, it can interrupt menstruation.
- Birth defects. Alcohol use during pregnancy may cause fetal alcohol syndrome. This condition results in birth defects, including a small head, heart defects, a shortening of the eyelids and various other abnormalities. Developmental disabilities are likely as well.
- Bone loss. Alcohol may interfere with the production of new bone. This can lead to thinning bones and an increased risk of fractures.
- Neurological complications. Excessive drinking can affect your nervous system, causing numbness of your hands and feet, disordered thinking and dementia.
- Increased risk of cancer. Chronic alcohol abuse has been linked to a higher risk of cancer of the esophagus, larynx, liver and colon.
- Domestic abuse and divorce
- Poor performance at work or school
- Increased likelihood of motor vehicle fatalities and arrest for drunken driving
- Greater susceptibility to accidental injuries from other causes
- Higher incidence of suicide and murder
Most people with alcoholism or those who abuse alcohol enter treatment reluctantly because they deny that they have a problem. Health problems or legal difficulties may prompt treatment. Intervention helps some people recognize and accept the need for treatment. If you're concerned about a friend or family member, discuss intervention with a professional.
Various treatments are available to help people with alcohol problems. Depending on the circumstances, treatment may involve an evaluation, a brief intervention, an outpatient program or counseling, or a residential inpatient stay.
Determining your level of dependence
The first step in treatment is to determine whether you're alcohol dependent. If you haven't lost control over your use of alcohol, treatment may involve reducing your drinking. If you're dependent on alcohol, simply cutting back is ineffective. Abstinence must be part of your treatment goal.
If you aren't dependent on alcohol but are experiencing the adverse effects of drinking, the goal of treatment is to reduce alcohol-related problems — often through counseling or a brief intervention, which usually involves alcohol-abuse specialists who can establish a specific treatment plan. Interventions may include goal setting, behavioral modification techniques, use of self-help manuals, counseling and follow-up care at a treatment center.
Counseling may take many forms. With cognitive behavior therapy, you and your therapist identify distorted thoughts and beliefs that trigger psychological stress. You learn new ways to view and cope with traumatic events. Emphasis is placed on developing a sense of mastery and control of your thoughts and feelings.
Another option may be aversion therapy, in which drinking alcohol is paired with a strong aversive response — such as nausea or vomiting induced by a medication. After repeated pairing, the alcohol itself causes the aversive response, which decreases the likelihood of relapse.
Residential treatment programs
Many residential alcoholism treatment programs in the United States include abstinence, individual and group therapy, participation in alcoholism support groups, such as Alcoholics Anonymous (AA), educational lectures, family involvement, work assignments, activity therapy and the use of counselors and professional staff experienced in treating alcoholism.
Here is what you might expect from a typical residential treatment program:
- Detoxification and withdrawal. Treatment may begin with a program of detoxification, usually taking about four to seven days. You may need to take sedating medications to prevent delirium tremens or other withdrawal seizures.
- Medical assessment and treatment. Common medical problems related to alcoholism are high blood pressure, increased blood sugar, and liver and heart disease.
- Psychological support and psychiatric treatment. Group and individual counseling and therapy support recovery from the psychological aspects of alcoholism. Many treatment programs also offer couples and family therapy because family support can be an important part of the recovery process. In fact, involving a spouse in the treatment process may increase the chances of successful recovery.
- Emphasis on acceptance and abstinence. Effective treatment is impossible unless you accept that you're addicted and currently unable to control your drinking.
- Drug treatments. An alcohol-sensitizing drug called disulfiram (Antabuse) may be a strong deterrent. Disulfiram won't cure alcoholism nor can it remove the compulsion to drink. But if you drink alcohol, the drug produces a severe physical reaction that includes flushing, nausea, vomiting and headaches. Naltrexone (ReVia), a drug long known to block the narcotic high, also reduces the urge to drink. Acamprosate (Campral) is an anti-craving medication that may help you combat alcohol cravings and remain abstinent from alcohol. Unlike disulfiram, naltrexone and acamprosate don't make you feel sick soon after taking a drink. Drugs approved for other purposes that show promise with alcoholism include:
- Gabapentin (for epilepsy, pain):Lessens anxiety and other withdrawal symptoms
- Topiramate (for epilepsy, migraines): May limit impulsiveness
- Varenicline (for quitting smoking):Blocks receptors associ¬ated with cravings
- Continuing support. Aftercare programs and support groups help people recovering from alcoholism or alcohol abuse abstain from drinking, manage relapses and cope with necessary lifestyle changes.
Knowing and recognizing a family history of alcoholism for you or others is an important step toward seeking treatment before alcohol use or alcohol abuse progresses to alcoholism.
Early intervention is particularly important to prevent alcohol dependence in teenagers. Alcohol use among teens increases dramatically during the high-school years, and leads to serious consequences for many teens. Each year in the United States, alcohol-related automobile accidents are a major cause of teen deaths. Alcohol also is often a cause in other teenage deaths, including drownings, suicides and homicides. Teens who drink are more likely to become sexually active, have sex more frequently and engage in risky, unprotected sex than teens who don't drink.
For young people, the likelihood of addiction depends on the influence of parents, peers and other role models, susceptibility to advertising, how early in life they begin to use alcohol, the psychological need for alcohol and genetic factors that may predispose them to addiction.
If you have a teenager, be alert to signs and symptoms that may indicate a problem with alcohol:
- Less or no interest in activities and hobbies
- Bloodshot eyes, slurred speech and memory lapses
- Difficulties or changes in relationships with friends, often characterized by joining a new crowd
- Declining grades and problems in school
- Frequent mood changes and defensive behavior
Coping skills
Many people seeking to end their alcohol dependence or abuse, and their family members, find that participating in support groups is an essential part of coping with the disease, preventing or dealing with relapses, and staying sober.
Alcoholics Anonymous
The fellowship of Alcoholics Anonymous (AA) was formed in 1935. As a self-help group of people recovering from alcoholism, AA offers a sober peer group as an effective model for achieving total abstinence.
The AA program is built around 12 steps, which are straightforward suggestions for people who choose to lead sober lives. As guides to recovery, the 12 steps help those with alcoholism to accept their powerlessness over alcohol. They stress the necessity for honesty about the past and present.
Recovery in AA is based on accepting the unique experience of each person. Through listening and sharing stories, people who abuse or are dependent on alcohol learn they aren't alone. There are no fees for membership or requirements for following the 12 steps — only a willingness to try to remain sober.
God grant me the serenity
To accept the things I cannot change;
Courage to change the things I can;
And wisdom to know the difference.
Living one day at a time;
Enjoying one moment at a time;
Accepting hardships as the pathway to peace;
Al-Anon and Alateen
Eventually family members of people recovering from alcoholism formed a complementary self-help group called Al-Anon. Al-Anon is designed for people who are affected by someone else's alcoholism. In sharing their stories, they gain a greater understanding of how the disease affects the entire family. Al-Anon accepts the 12 steps of AA as the principles by which participants are to conduct their lives. It also emphasizes the need to learn detachment and forgiveness. In many communities, Alateen groups also are available for teenage children of those with alcoholism.
Your doctor or counselor can refer you to an AA group or other local support group. These groups are also commonly listed in the phone book, in the local newspaper and on the Web.
Complementary and alternative medicine
Acupuncture, the insertion of hair-thin needles under the skin, may relieve cravings for alcohol and alleviate some of the symptoms of alcohol withdrawal, such as tremors and fatigue. Acupuncture may also reduce anxiety and depression, which lead some people to drink alcohol.
TESTING RESOURCES
• AlcoholScreening.org6 -- an interactive tool, based on the Alcohol Use Disorders Identification Test (AUDIT), developed by the World Health Organization.
• Michigan Alcohol Screening Test (MAST) -- 22 yes-or-no questions. Available on many sites, including this one7
• The RAPS4 Alcohol Screening Test8 -- a four-question quiz designed to be used by doctors for a quick indication of possible problems.
• The CAGE Test9 -- one of the oldest screening tools to diagnose alcohol problems over a lifetime.
• Is AA For You?10 -- Twelve questions that can help you decide if you want to give it a try.
• National Council on Drug and Alcohol Abuse's 20-question test11 for teenagers.
--M.B.
Are You an Alcoholic?
Melinda Beck : WSJ Article : January 8, 2008
The holidays are over. Resolutions are wearing thin. It's a time of year when many people wonder if they have a drinking problem.
More than 30% of Americans engage in risky drinking at some point in their lives, according to the National Institute on Alcohol Abuse and Alcoholism. But there's no consensus on exactly what an "alcoholic" is. Even Alcoholics Anonymous relies on alcoholics to diagnose themselves.
Researchers have made up dozens of screening tests over the years. According to one developed for Johns Hopkins University Hospital years ago that still pops up on the Web, I'm "definitely an alcoholic" because I answered yes to at least three of 20 questions: I "crave a drink at a definite time of day" (evenings, mostly) and drink alone (sometimes) and drink to "escape from worries or troubles" (doesn't everyone who drinks?).
But Alcoholscreening.org3 says I'm "below the range usually associated with harmful drinking or alcoholism" since I have only a glass or two of wine when I drink.
The authoritative American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, or DSM-IV, separates alcohol abuse from alcohol dependence, based partly on the problems the drinking causes. You qualify for a diagnosis of "abuse" if you've done any one of these in the past year: drunk alcohol in hazardous situations, like driving; kept drinking despite social or interpersonal problems; had legal problems related to alcohol or failed to fulfill major obligations at work, school or home because of drinking.
You've moved on to "dependence" if you've done any three of these seven: drunk more or longer than you intended; been unable to cut down or stop; needed more alcohol to get the same effect; had withdrawal symptoms without it; spent more time drinking or recovering; neglected other activities or continued to drink despite psychological or physical problems.
Experts long believed that abuse progressed to dependence, which almost inevitably became chronic and relapsing -- but that was based on observing severely addicted people in treatment programs. Several large new surveys have shown that drinking patterns in the general population are much more varied, with milder forms of dependence. Some 43% of daily heavy drinkers don't fit into either DSM-IV category, according to one big national sample, even though they are setting themselves up for serious health and addiction problems.
Abuse vs. Dependence
"Some people will abuse alcohol -- driving drunk, for example -- but they only drink heavily once a month. They can remain stable for a long time and not progress to dependence," says Mark L. Willenbring, director of the division of treatment and recovery research at the NIAAA. "And people can be dependent and not have abuse problems at all. They're successful students. They're good parents, good workers. They watch their weight. They go the gym. Then they go home and have four martinis or two bottles of wine. Are they alcoholics? You bet. And the goal is to get treatment for these folks, earlier, that is acceptable and attractive and effective."
To that end, some experts want the DSM-V -- the new edition now being compiled -- to combine abuse and dependence into a single "alcohol-use disorder" that ranges in severity, taking into account harmful drinking patterns and other symptoms. The aim is for simmering problems to be spotted sooner.
As one former treatment counselor says, "The conventional wisdom held that alcoholics had to hit bottom before they could get better. We'd like to raise that bottom so that people don't have to fall as far before they get help."
Many heavy drinkers are very high-functioning -- until they can't function anymore. "Alcoholics can be high achievers in the short run, because they're driven and compulsive," says Charlie, a New York attorney who, like all AA members, wants to remain anonymous. Charlie was drinking about a fifth of Johnnie Walker most nights when it began to show. "I'd tell my secretary I was in a meeting with a client, but I'd be home and only starting to feel human by about noon. Then I'd try to do eight hours of work in four hours," he says. This went on for seven years, until he finally went into rehab. He's been sober now for 26 years.
Charlie says many heavy drinkers, especially those who grew up around alcoholics, set a private benchmark in their denial. "They say to themselves, 'As long as I'm not making a fool of myself in a bar, or drinking in the morning, or as long as I'm still showing up for work, then I'm not an alcoholic.'"
You know you've hit bottom, he adds, "when your behavior spirals downward faster than you can lower your standards."
Thinking You're Immune
Ruth, a nursing supervisor in Las Vegas, hid her quart-a-day whiskey habit from work for about five years -- "until my husband and my employer both invited me out of those positions at the same time," she says. "That got my attention."
Both of Ruth's parents died of alcohol-related illnesses, but she thought her medical training would protect her from getting seriously addicted. Doctors and clergy who drink heavily often have the notion that they are somehow immune to the problems they see in others, she observes, and affluent people can pay others to take care of them. "People with less money and less education often get the message faster," she says, now that she's been sober for 37 years.
NIAAA officials say that in recognizing a drinking problem, the label "alcoholic" is less important than harmful patterns of drinking, which they describe as drinking too much, too fast or too much, too often.
Too much, too fast means consuming more than four drinks in two hours for men, and more than three in two hours for women. That's a level that, on average, makes people legally drunk and impairs brain function. (A standard U.S. drink, by the way, is 12 oz. of beer, 5 oz. of wine or a 1.5 oz. shot of 80 proof spirits, according to government agencies.)
Even if you stay within those limits each day, you can be drinking too much, too often, if you have more than 14 drinks a week for men, and more than 7 for women. That's the kind of chronic use that raises the risks of a long list of health problems, including liver and cardiovascular disease, pancreatitis, dementia, depression and numerous cancers.
How those weekly drinks are distributed is also important. "If you drink seven drinks in two days, that's hazardous -- you're drunk two days a week," says Ting-Kai Li, the NIAAA's director. "If you drink two a day for seven days, that's not harmful. In fact, it may even be beneficial for some people, lowering their cardiovascular risk."
Individual responses to alcohol vary, of course, based on genetics, brain chemistry, metabolism and other factors. Your risk is already elevated if you have a family history of alcohol abuse, have health problems such as depression, take certain medications or you started drinking at an early age. "If you have a family history or other co-morbidity, then the general advice is, don't drink at all," says Dr. Li.
If you're worried that you may be drinking too much, you've already met a key criterion on some screening tests. (Like the old saying about mice in your house, if you think you have a problem, you probably do.)
Counting drinks very carefully to stay within the limit can be a sign of trouble too, says Ruth. "The glass keeps getting bigger and bigger or you forget to add the mixer." She suggests trying to go 30 or 60 days without drinking. "If it doesn't bother you, you're OK. But if you're desperate for that 30 days to end, or you can't make it, then get help." She suggests trying one of AA's public information meetings. "If you're not an alcoholic, you can't catch it from them," she says.
Your family doctor is another place to start. The NIAAA recently issued a guide for primary-care physicians (www.niaaa.nih.gov/guide4) to enlist their help in spotting alcohol problems. It starts with a single screening question: How many times in the last year have you had five or more drinks (four or more for women) in a day? If the answer is even once, doctors are advised to discuss the risks of harmful drinking with their patients, along with steps patients can take to cut back, including new medications that can help curb alcohol cravings.
In Remission
The encouraging news from the NIAAA's recent research is that many people do cut down or quit on their own. "That's the real mind blower," says Dr. Willenbring. "Only about 15% of the people who develop alcohol dependence in their lifetime have the severe, relapsing form. Most people -- 72% -- have a single episode [of addiction] lasting on average three or four years and then they go into remission and stay there. A lot of them are abstaining." For many people, that spate of heavy drinking happens in college -- the peak years are 18 to 24, says Dr. Willenbring. "Then they mature out of it and get on with their lives."
For those who don't, alcoholism, however it's defined, is still a profound problem, and the third leading cause of preventable death in the U.S., after smoking and obesity. But being aware of your risks and cutting down now if you need to may prevent you from becoming one of those statistics.
CORRECTIONS & AMPLIFICATIONS: The National Institute on Alcohol Abuse and Alcoholism's guide for primary-care physicians to spot alcohol problems in their patients starts with a single screening question: How many times in the last year have you had five or more drinks (four or more for women) in a day? An earlier version of the Health Journal column on Jan. 8 misstated the question as more than five drinks for men and more than four for women.
5 Sub-types of Alcoholics
- The young adult subtype accounts for about 32% of U.S. alcoholics. They're young adults who rarely seek help for alcohol dependence. About 24 years old, they became alcoholics by age 20, on average. They drink less frequently than other alcoholics, but they tend to binge drink when they drink. This is the largest subtype.
- The young antisocial subtype comprises 21% of U.S. alcoholics. They are 26 years old, on average. More than half have antisocial personality disorder. They tended to start drinking at 15 and became alcoholics by 18 -- earlier than other subtypes. They are more likely to smoke tobacco and pot. The young antisocial subtype and the young adult subtype don't overlap, Moss tells WebMD.
- The functional subtype accounts for about 19% of U.S. alcoholics. They're generally middle-aged, working adults who tend to have stable relationships, more education, and higher incomes than other alcoholics. They tend to drink every other day, often consuming five or more drinks on drinking days.
- The intermediate familial subtype makes up nearly 19% of U.S. alcoholics. Nearly half have close relatives who are alcoholics. Alcoholics in this subtype typically began drinking by 17 and became alcoholics in their early 30s.
- The chronic severe subtype is the rarest subtype, accounting for about 9% of U.S. alcoholics. This subtype mainly includes men, has the highest divorce rate, and frequently includes users of illicit drugs
High- Functioning, but Still Alcoholics
By Jane E. Brody : NY Times Article : May 5, 2009
Sarah Allen Benton is hardly your stereotypical alcoholic. She has a master of science degree from Northeastern University and is a licensed mental health counselor at Emmanuel College in Boston. In recovery from alcoholism for the last five years, she has written an enlightening new book about people like herself, “Understanding the High-Functioning Alcoholic” (Praeger Publishers).
As Ms. Benton describes them, high-functioning alcoholics are able to maintain respectable, even high-profile lives, usually with a home, family, job and friends. That balancing act continues until something dreadful happens that reveals the truth — to themselves or to others — and forces the person to enter a treatment program or lose everything that means anything.
A Hidden Problem
Typical high-functioning alcoholics, or H.F.A.’s as Ms. Benton calls them, are in denial about their abuse of alcohol. Coworkers, relatives and friends often enable the abusive behavior to continue by refusing to acknowledge and confront it.
“The story of the H.F.A. is seldom told,” Ms. Benton writes, “for it is not one of obvious tragedy, but that of silent suffering.”
Based on surveys and professional experience, she estimates that as many as half of all alcoholics are high-functioning types. The abuse can go on for decades until and unless some alcohol-related crisis occurs, like being arrested for drunken driving, exposed for having made unwanted sexual advances or being asked for a divorce when their spouses can no longer tolerate the abusive drinking.
Or, like Ms. Benton, they may seek help after recognizing that no matter what they try, they are unable to drink normally and fear that sooner or later their luck will run out.
Many well-known people have publicly acknowledged their battles with alcohol and entered recovery before their lives were destroyed. Among those listed by Ms. Benton are Betty Ford, the astronaut Buzz Aldrin, the actresses Elizabeth Taylor and Mary Tyler Moore, the actor Robin Williams, the singers Keith Urban and Eric Clapton, the football legend Joe Namath and former President George W. Bush.
But there are millions of others — including dentists and doctors, professors and teachers, lawyers and judges, journalists and authors, firemen and C.E.O.’s of major companies — who work for years while abusing alcohol, sometimes putting their lives, and the lives of others, at great risk. Surgeons have been known to operate with shaking hands, yet colleagues who knew or suspected that alcohol abuse was the cause failed to confront the doctor. Employees who suspect a problem often cover up for their bosses.
Ms. Benton emphasized that people in positions of power are often the hardest to detect and help because they tend not to be closely supervised at work, they are assumed to be able to deal successfully with the pressures of their jobs, their high pay enables them to escape the financial consequences of excessive drinking, and they see drinking as their reward for hard work.
As the writer Pete Hamill said in his memoir, “A Drinking Life,” “If I was able to function, to get the work done, there was no reason to worry about drinking. It was part of living, one of the rewards.”
In some cases, the culture of the workplace fosters high-functioning alcoholism. Abusive drinking was once commonplace among journalists, who had “liquid lunches” and frequently met for drinks after work. When work and social lives blend, excessive drinking may be considered part of the job.
Double Lives
A further problem in identifying and getting help for high-functioning alcoholics is that they often do not meet the criteria for alcohol abuse described in the psychiatric diagnostic manual. They have good jobs, perform the expected tasks of daily life and avoid legal problems.
As Dr. Mark L. Willenbring of the National Institute for Alcohol Abuse and Alcoholism put it in Ms. Benton’s book: “People can be dependent and not have abuse problems at all. They’re successful students. They’re good parents, good workers. They watch their weight. They go to the gym. Then they go home and have four martinis or two bottles of wine. Are they alcoholics? You bet.”
As for herself, Ms. Benton said: “Having outside accomplishments led me and others to excuse my drinking and avoid categorizing me as an alcoholic. My success was the mask that disguised the underlying demon and fed my denial.”
Even those who recognize they have an alcohol problem may avoid seeking help because they perceive it as a sign of weakness.
High-functioning alcoholics are highly skilled at leading double lives, Ms. Benton wrote. They appear to the outside world to be managing life well and defy the alcoholic stereotype by being fashionable, physically attractive, even elegant. They also tend to hide their excessive consumption by drinking alone or sneaking alcohol before or after a social event, and disguising or excusing the odor of alcohol on their breath.
High-functioning alcoholics also may not be physically addicted to alcohol, abstaining for days or weeks without suffering withdrawal symptoms. But they are psychologically dependent on alcohol, often focused on when they can drink again and convinced that they need to drink in certain settings. They are also likely to experience blackouts, remembering nothing the next day about a night of heavy drinking, with only a hangover as evidence of their abusive behavior.
“But just because people are high-functioning doesn’t mean they are not putting themselves and others in danger,” Ms. Benton said in an interview. Under the influence of excessive amounts of alcohol, they may operate motor vehicles or dangerous machinery or engage in risky sexual encounters. They may be picked up for driving under the influence, miss important professional or family obligations or repeatedly arrive late to work. And, Ms. Benton said, “They can face the same health risks as a lower-functioning alcoholic.”
Knowing the Signs
In the interview, Ms. Benton listed several characteristics that can help people recognize themselves as high-functioning alcoholics:
¶They have trouble controlling their intake even after deciding that they will drink no more alcohol than a given amount.
¶They find themselves thinking obsessively about drinking — when and where and with whom they will drink next.
¶When they drink, they behave in ways that are uncharacteristic of their sober self.
¶They experience blackouts, unable to remember what took place during a drinking bout.
“It’s not the number of drinks that defines an alcoholic,” Ms. Benton said. “It’s what happens to you when you’re drinking.”
Adult Binge Drinkers Prefer Beer
By The AP : August 7, 2007
Binge drinkers are more likely to have a beer can in hand than a shot glass, new research shows.
Unless you're talking about teens. They prefer the hard stuff.
The stereotype-shattering findings are reported in two studies by the U.S. Centers for Disease Control and Prevention.
Access may play a major role in the choices of the two age groups, experts suggested.
For adults, beer is cheaper and easy to find, sold in gas stations and grocery stores. However, for teens, it may be easier to filch free booze from their parents' liquor cupboards, one of the researchers said.
Binge drinking -- no matter which type of alcohol -- is bad for your health. Excessive alcohol is acutely dangerous because of its role in car crashes, violence and other traumatic injury, and is blamed for 75,000 deaths annually.
The study of adult binge drinkers found that nearly 75 percent mainly or exclusively drank beer, 17 percent focused on liquor, and 9 percent were wine drinkers. A binge drinker was defined as someone who had five or more alcoholic drinks on at least one occasion in the last 30 days.
About 15 percent of U.S. adults fit that profile, and most are men, according to federal statistics.
''This is behavior that is common,'' said the CDC's Dr. Timothy Naimi, lead author of a study of 14,000 adult binge drinkers. ''It boils down to drinking to get drunk.''
Researchers also looked at bingers who drank a variety of beverages -- for example, a few after-work beers, a cocktail before dinner and wine with dinner. That research showed beer accounted for 67 percent of binge drinks consumed, liquor for 22 percent and wine for 11 percent.
Beer was expected to be high on the list: It accounts for about 55 percent of the alcohol sold in the United States, as measured by the gallon, according to sales tax statistics.
But the fact that beer is such an overwhelming favorite of binge drinkers contradicts a Hollywood stereotype of hard drinkers clutching a bottle instead of a six-pack.
That perception may help explain why beer is No. 1, Naimi said. Because of a governmental focus on the dangers of liquor, beer is generally less expensive, and easier to get.
The volume of beer advertising on television is also a factor, said Gail DiSabatino, vice president for student affairs at Clemson University.
''If you watch a commercial during any NCAA championship, or the big sporting events, beer is promoted heavily,'' she said.
In a separate study, a different team of researchers looked at 2005 survey data for public high school students in Arkansas, Nebraska, New Mexico and Wyoming. The survey was anonymous. Results were based on about 4,000 responses.
The pilot study found that liquor was the most commonly consumed alcoholic beverage among teens who reported binge drinking. In Arkansas, liquor accounted for 49 percent of binge drinks, with beer, malt beverages, wine and wine coolers making up the rest. The hard stuff also was clearly ahead in Wyoming and New Mexico. In Nebraska, liquor and beer consumption were virtually tied.
Because the study was smaller and more geographically limited, it's difficult to equate it with the national study of adults, DiSabatino observed.
Asked why high school binge drinkers might prefer liquor, DiSabatino noted studies that show many youths get their alcohol from home.
It may be easier to snatch drinks from a liquor cabinet than beers from the fridge. ''It might not be as noticed,'' DiSabatino said.
There are other motivations for teens, said Jennifer Cremeens, a former CDC epidemiologist who co-authored the high school study.
Liquor can be easier to conceal from parents, mixed in a cup with juice or soda. It's also more potent. ''Liquor's quicker,'' Cremeens said.
The study of adult bingers was published for release Tuesday in the American Journal of Preventive Medicine, and was based on data from a national random-digit-dial survey done in 2003 and 2004.
The study of teen drinkers was published recently in the CDC's Morbidity and Mortality Weekly Report.
To Your Health: New Web Site Helps Predict Alcohol Problems
Melinda Beck : WSJ Article : March 10, 2009
The conventional wisdom used to be that alcoholics had to hit bottom before they got better. But it can be a long, slow way down. A new government Web site called "Rethinking Drinking" aims to help people recognize problem patterns earlier and catch themselves before they fall.
"Most people don't know what 'drink responsibly' means -- they think it means not getting tanked," says Mark Willenbring, director of treatment and recovery research at the National Institute of Alcohol Abuse and Alcoholism. "But there are levels of drinking that raise your risk for alcohol problems just like high cholesterol raises your risk for heart disease."
Behind the NIAAA's effort is a new understanding that there is a spectrum of alcohol-use disorders, which some experts hope will replace the current criteria for "abuse" and "dependence." The old definitions were based on observing addicts in treatment. Several large studies of drinking in the general population show that some patterns clearly pave the way for future problems.
The NIAAA say you are at "low-risk" for serious problems if you consume no more than four standard-size alcoholic drinks a day for a man or no more than three for a woman. That may sound like a lot, but you can't drink like that every day. The weekly "low-risk" limit is no more than 14 drinks for a man or seven for a woman. Drinking more daily, or weekly or both carries higher risk of abuse or dependence.
At www.rethinkingdrinking.niaaa.nih.gov, you can plug in your average consumption and see how you compare with the general population and problem drinkers. Since this is anonymous, you can try different amounts and see what they mean.
Some 37% of Americans always stay within the daily and weekly limits, according to the site. Only two in 100 of them progress to serious alcohol problems.
But 19% of Americans exceed either the daily or weekly levels; one in 12 of those people has already progressed to alcohol abuse or alcoholism. About 9% of Americans exceeds both the weekly and daily limits; half of them have alcohol problems.
Very few Americans exceed the weekly limits without exceeding the daily limitations, according to Dr. Willenbring. That contrasts with drinking patterns in Europe, where people are more likely to have wine with lunch and dinner on a daily basis.
About 35% of Americans don't drink at all. "That can be a real eye-opener for people who drink heavily and surround themselves with other people who drink a lot," says Ann Bradley, an NIAAA spokeswoman.
Even "low-risk" drinking can be risky for people with bipolar disorder, liver disease, abnormal heart rhythm and chronic pain, the Web site notes. It also links to a list of dozens of medications that can react adversely with alcohol, including drugs for high blood pressure, high cholesterol, pain and depression.
The limits are lower for women than men not just because of their size. According to the NIAAA, women's bodies tend to have less water so the alcohol tends to become more concentrated and more damaging to organs like the liver.
The Web site also notes that being able to "hold" a lot of liquor is actually a warning sign of dependence. And driving and judgment can be impaired even if you don't feel a buzz.
Safer Spirits
Most people are at low risk for alcohol problems if they stay within these limits:
- Men: No more than four standard-size drinks on any single day and no more than 14 weekly.
- Women: No more than three standard-size drinks on any single day and no more than seven weekly.
Knowing the size and strength of a "standard" drink is critical, so the site has a size chart and a content calculator. Some cocktails contain as much alcohol as three standard drinks. A wine bottle usually holds five 5-oz. glasses.
"Rethinking Drinking" leaves it up to you whether and when to change your habits, though it notes that alcohol is a factor in many fatal accidents and increases the risk of heart and liver disease, depression, sleep disorders, diabetes and many cancers. One section discusses the merits of cutting down versus quitting completely. Another lists pros and cons to consider—including "I'd need another way to wind down."
In focus groups when the site was tested, "some people got very quiet and engaged when they got to this part. It turned into an intervention," says Maureen Gardner, who co-authored the program.
The site also lists strategies for changing drinking habits, from "space and pace" (no more than one per hour) to "avoiding triggers" (recognizing external situations and internal emotions that tempt you to drink). An "urge tracker" lets you record times when you wanted a drink and why, what you did and what you might have done differently. A section on "refusal skills" helps you plan ahead to say no in social situations.
Dr. Willenbring hopes the site, and a downloadable print version, provides a tool for doctors, clergy and others who counsel people concerned about their drinking habits.
Awareness already seems to be rising, says Eileen Travis, director of a New York City Bar Association program that assists lawyers with substance abuse. "We get calls all the time from people who say they think they have a problem and want to stop before it gets bad—many more than in the past, when the only people we dealt with were in trouble in some way," she says.
Studies show that just five minutes of discussion with a primary-care doctor can reduce heavy drinking by 25%. Exploring online all by yourself might be just as useful.
RESPONSIBLE DRINKING
Alcohol affects women differently than men. Women become more impaired than men do after drinking the same amount of alcohol, even when differences in body weight are taken into account. This is because women's bodies have less water than men's bodies. Because alcohol mixes with body water, a given amount of alcohol becomes more highly concentrated in a woman's body than in a man's. In other words, it would be like dropping the same amount of alcohol into a much smaller pail of water. That is why the recommended drinking limit for women is lower than for men.
Here are some hints for maintaining a moderate blood alcohol concentration:
- Don't be fooled. The contents of the typical bottle or can of beer, glass of wine, or liquor drink (mixed drink or straight liquor) each contain virtually identical amounts of pure alcohol. When it comes to alcohol, a drink is a drink is a drink and are they all the same to a breathalyzer. For more, visit Standard Drinks.
- Know your limit. If you are not sure, experiment at home with your spouse or some other responsible individual. Explain what you are attempting to learn. Most people find that they can consume one drink per hour without any ill effects. Also, experiment with the "http://www.intox.com/wheel/drinkwheel.asp", which is very informative.
- Eat food while you drink. Food, especially high protein food such as meat and cheese will help slow the absorption of alcohol into your body.
- Sip your drink. If you gulp a drink, you also lose the pleasure of savoring its flavors and aromas.
- Don't participate in "chugging" contests or other drinking games.
- Accept a drink only when you really want one. If someone tries to force a drink on you, ask for a non-alcohol beverage instead. If that doesn't work, "lose" your drink by setting it down somewhere and leaving it.
- Skip a drink now and then. Having a non-alcoholic drink between alcoholic ones will help keep your blood alcohol content level down, as does spacing out your alcoholic drinks
- A good general guideline for most people is to limit consumption of alcohol beverages to one drink (beer, wine or spirits) per hour.
- Keep active; don't just sit around and drink. If you stay active you tend to drink less and to be more aware of any effects alcohol may be having on you.
- Beware of unfamiliar drinks. Some drinks, such as zombies and other fruit drinks, can be deceiving as the alcohol content is not detectable. Therefore, it is difficult to space them properly.
- Use alcohol carefully in connection with pharmaceuticals. Ask your physician or pharmacist about any precautions or prohibitions and follow any advice received.
Testing the Limits of Tipsy
Many Factors Alter the Effects of Alcohol; A Party Experiment
By Melinda Beck : WSJ : August 2, 2011
How much alcohol does it take to reach a blood-alcohol level of .08%, the legal intoxication level in all 50 states? Since Alcohol clearly affects some people more than others, Melinda Beck looks at whether that affects their blood-alcohol level?
How much alcohol does it take to get intoxicated?
Many people figure a few beers at a ballgame or a couple of glasses of wine with dinner won't put them over the legal limit for driving. But how alcohol affects people is highly individual, with a number of factors in the mix.
Quick shots of liquor hit the bloodstream faster than slow sips of wine. Drinking on an empty stomach impairs reflexes more than consuming alcohol with food. And women and older drinkers generally hit legal intoxication levels sooner than men and younger people.
Carbonated beverages raise alcohol levels faster, because the gas irritates the stomach lining, causing alcohol to be absorbed faster. (Sweet or caffeinated alcoholic drinks aren't absorbed any faster, it just seems that way because people often consume more of them than they realize.)
Party MathAt a recent dinner, guests were asked to eat and drink as they normally would and test periodically with a home breathalyzer. Click above to view the results.
Many Asians have a genetic variation that gives them a flush and a very rapid heartbeat from even a small amount of alcohol.
And factors like fatigue, stress, illness and depression can magnify alcohol's impact.
Eileen Wolter was driving home from an office Christmas party she had organized in Los Angeles in 1998. "I was definitely under a lot of stress," she says. She had had several mixed drinks, a few glasses of wine and very little food, but thought she was fine—until she took a turn too fast and hit a stop sign. She was driving with a flat tire and a broken wheel, causing even more car damage. A police car stopped to see if she was OK, and she flunked a breathalyzer test. "I blew a .09," says Ms. Wolter, who was arrested, fined $2,000 and sentenced to community service and alcohol education classes.
"I wasn't hurt—just humiliated and angry and scared. Dealing with all of it—and the fact that I could have hurt myself or someone else—made me realize what a stupid chance I'd taken," says Ms. Wolter, now a 40-year-old writer and mother of two who says she will never drink that way and drive again.
Drinkers who think they can tell when they've had enough are very often wrong. "Alcohol can affect your reflexes even if you feel fine," says Samir Zakhari, director of the division of metabolism and health effects at the National Institute of Alcohol Abuse and Alcoholism.
That's a key reason why many experts urge people who plan to drink any amount of alcohol not to drive, and vice versa.
Getty ImagesMany Asians have a genetic variation that gives them a flush and a very rapid heartbeat from even a small amount of alcohol.
In the U.S., it is illegal for adults to drive with a blood-alcohol concentration (BAC) at or above .08%, which represents the percentage of alcohol in the bloodstream. For drivers under 21, any alcohol in the blood is illegal.
The legal limit, once as high as .15% in some states, is now .08% in all 50 states. Some experts still consider it generous. Reaction time starts to slow at only half that amount, and much of the world sets stricter limits. It's .02% in China, .03% in most of India and .05% in much of Europe.
Home Breathalyzers: Useful, but Results VaryFrom a $5 keychain gizmo to a $2,000 desktop device, dozens of blood-alcohol testers are on the market today, allowing consumers to test themselves, their guests—even their wayward teenagers.
Most work in the same way: You wait as a digital counter counts down, then inhale deeply and blow into a plastic mouthpiece or across a small hole. The devices don't directly measure blood-alcohol concentration (BAC), but a derivative in breath. They convert it to BAC and display it on a digital screen, sometimes adding 'caution' or 'danger.
We tested three models at our BAC party and found that in general, the smaller the device, the higher the reading—not necessarily a bad thing, we decided. But they were all within a hundredth of a percentage point, whether it was the BreakKey, a $69 keychain model weighing less than an ounce, the AlcoHAWK Slim Digital Alcohol Breath Tester ($55), or the BACtrack Select S80 Breathalyzer ($249) that had a readout to an extra digit—worth it to the guest who wracked up a .079% score, just shy of the .08% limit. (The $5 Wingman Sport Breathalyzer, which arrived after the party, gave a consistently higher reading compared with the others in a second test -- .190 after a single glass of wine, while the BACtrack and the AlcoHAWK both read .04. The BreakKey had mysteriously stopped functioning and kept reading "Blow… Hard."
Results can be thrown off by vigorous exercise, medical conditions like acid reflux and diabetes—even dieting, which can raise the level of acetones in a person's breath that some devices falsely read as alcohol. Mouthwashes that contain alcohol can also make readings high, although manufacturers say that newer breathalyzers that use fuel-cell technology don't give as many false-positive readings as those made with semiconductors.
Most police departments use fuel-cell models for preliminary readings in the field and tabletop versions at the station that are accurate enough to use in court. Police breathalyzers must also be approved by the National Highway Transportation Safety Administration, while consumers models sold in the U.S. need clearance from the Food and Drug Administration.
If used too soon after a person has imbibed, many breathalyzers will inadvertently measure the vapor left in the mouth rather than the level derived from blood, which is why most models advise users not to test for least 20 minutes after drinking or eating to get an accurate reading.
Many of the devices urge consumers to keep them in their cars or their purses to test themselves before getting behind the wheel. But many experts and advocacy groups worry that they can give people a false sense of complacency.
Samir Fakhari, director of the division of metabolism at the National Institute of Alcohol Abuse and Alcoholism, says that home breathalyzers may be reasonably accurate in giving 'an approximation of your BAC.' But he worries that they can be misused, misinterpreted and even befuddle someone who is truly inebriated. 'It's a better idea not to drink at all if you're driving,' he says.
—Melinda Beck
Many communities plan to join a nationwide crackdown on impaired driving between Aug. 19 and Sept. 11, including saturation patrols and sobriety checkpoints, especially during nighttime hours.
Such efforts have helped cut alcohol-related traffic deaths in the U.S. by almost 50% since 1980, though the number has plateaued in recent years at nearly 11,000 deaths annually, or one-third of all highway fatalities.
How does BAC work? One of the most important factors is how fast the alcohol is consumed, says Dr. Zakhari. It goes first to the stomach, then to the small intestine, where it is absorbed into the bloodstream and carried to the liver, where it is metabolized by liver enzymes.
"The liver can only break down the alcohol at the rate of about one drink per hour," says Dr. Zakhari, who likens it to how fast a ticket-taker can let concert-goers through a gate.
Consuming one drink slowly over an entire hour is unlikely to make a person inebriated, he says. But drinking more than that amount, or the same amount faster, will overwhelm the liver. The excess alcohol "goes into the bloodstream and every other organ in the body, including the brain," he says.
Once that happens, only time can unwind the effects, Dr. Zakhari says. BAC generally falls by .015% per hour for both men and women—but will rise again if you keep drinking. Drinking coffee, having a shower or splashing cold water on your face may make you feel more alert, but won't change your BAC.
Consuming food along with alcohol causes it to be absorbed more slowly, since a valve at the base of the stomach closes to allow for digestion before sending it along. Without this stop, the alcohol travels to the small intestine and into the liver faster.
What you eat along with the alcohol doesn't matter very much in terms of BAC. Fat, in, say, a marbled steak, slows the passage of food through the intestine, but only to a small extent. Likewise, drinking milk before consuming alcohol would have a negligible effect on blood levels.
Weight matters more than height, Dr. Zakhari says. A man who is 6-foot-4 and weighs 180 pounds will be as affected as a man who is 5-foot-4 and 180 pounds. But a man who is 6-foot-4 and 220 pounds will have a lower BAC after consuming the same amount. Women's bodies also tend to have less water than men's, which means the same amount of alcohol will yield an even higher BAC.
That was readily apparent at a recent dinner party, where guests were served alcohol and tested throughout the evening. A 110-pound woman, for example, reached a BAC of .079% with less than two drinks, while a 160-pound woman the same height had .05% on three.
Age matters, too. Older peoples' livers metabolize alcohol more slowly than younger people's. But excess alcohol can do more damage to young brains, since some portions are still developing, particularly those that govern impulse control and executive function.
Women's menstrual cycles are yet another factor: Alcohol metabolism increases about 10% right after ovulation.
People who drink heavily and regularly don't get as intoxicated as novice drinkers do on the same amount of alcohol, and tend to have a lower BAC because their livers eventually produce more of a particular enzyme (Cytochrome P450 IIE1) that breaks down alcohol more quickly.
But that may sometimes lull them into a dangerous complacency. Randy Strain, had just finished a stint with the Air Force, where off-duty drinking was common, in 2008 when he and his girlfriend were driving home on a rural road in Illinois after what he thinks were "about 20 beers." They were going about 80 miles per hour when they passed three police cars that were soon on his tail.
The ensuing 14 traffic violations and a DUI could have yielded a jail sentence, but a judge, noting his military service, only restricted his driver's license for six months, fined him $2,000 and ordered him to take 24 hours of classes.
Still, "it was a life-changing experience," says Mr. Strain, 27, of Oak Park, Ill. "Now I go out max one night a week and take a cab home. I will not even get into a car if I or someone else has been drinking."
The Drink Wheel
On-Line BrAC Calculator
About Disclaimer
About the Drink Wheel
The Intoximeters Inc. 'Drink Wheel'1 is a form that you can fill out. Upon completion we will instantly compute your estimated blood/breath alcohol concentration ('BAC') based on the information that you have provided and return that estimate to you. It is presented as a public service to Intoximeters web site visitors. Its primary purpose is to provide useful information about the responsible use of alcohol.
Why is it called a 'Drink Wheel'?
We call it the 'Drink Wheel' because it is based on various paper and cardboard BAC calculators that are given out in alcohol awareness programs, some of which are in the form of a wheel that you can spin around to calculate your estimated BAC based on what and how much you have had to drink.
Disclaimer
It would be extremely foolish for us to pretend that our 'Drink Wheel' can tell you what your BAC actually is, first because it would open us up to an incredible amount of potential liability and second if it really did work accurately there would be no need for anyone to buy the instruments that we make and sell.
A person's actual BAC is dependent on many complex factors, including their physical condition (body composition, health etc...) and what they have recently ingested (including food, water, medications and other drugs). This site includes a more detailed discussion of the Pharmacology and Disposition of alcohol in humans.
The results that are generated are rough estimates of an average healthy person's BAC assuming typical beverage sizes, recipes and alcohol content. The BAC estimates generated by the Drink Wheel should not be used to infer anyone's fitness to work, drive or perform any other task or duty.
A standard drink contains about 14 grams (about 0.6 fluid ounces of pure alcohol. Below are some approximate drink equivalents:
- 12 oz. of beer or cooler
- 8-9 oz. of malt liquor
- 5 oz. of table wine
- 3-4 oz. of fortified wine
- 2-3 oz. of cordial, liqueur or aperitif
- 1.5 oz. of brandy or spirits
Types of Alcohol Problems
- Relatively low levels of alcohol consumption may increase risk for motor vehicle crashes, medication interactions, fetal effects, strokes caused by bleeding, and certain cancers.
- Alcohol use disorders include alcohol dependence (known as alcoholism) and alcohol abuse.
- Alcohol abuse is characterized by clinically significant impairment or distress but does not entail physical dependence.
- Alcohol dependence (alcoholism) is characterized by 10 diagnostic criteria according to the DSM-IV. These criteria include: impaired control over drinking, tolerance, withdrawal syndrome when alcohol is removed, neglect of normal activities for drinking, and continued drinking despite recurrent related physical or psychological problems.
Who Has An Alcohol Problem?
- 25 percent of U.S. children are exposed to alcohol abuse or dependence in the family.
- Between 2001 and 2002, the prevalence of alcohol abuse was highest among Native Americans (5.75%) followed by Whites (5.10%), Blacks (3.29%), Hispanics (3.9%), and Asians (2.13%).
- Alcohol abuse and dependence is more common among males than females and decrease with aging.
- Between 2001 and 2002, 8.5 percent of adult Americans –17.6 million -- met DSM-IV diagnostic criteria for either alcohol dependence or alcohol abuse.
Harmful Effects of Alcohol
- Alcohol–related crashes (i.e., those in which a driver or pedestrian had a blood alcohol concentration [BAC] greater than zero) account for 41 percent of all fatal car accidents .
- Alcohol use contributes to a range of chronic health consequences including cancer and cardiovascular disease.
- Alcohol use has been associated with increased risk of traumatic injury including: motor vehicle crashes, bicycling accidents, pedestrians, falls, fires, injuries in sports and recreational activities, interpersonal violence, and self–inflicted injuries.
- The economic costs of alcohol abuse in the United States are estimated to be approximately $185 billion annually.
Alcohol and Women
- Women are more vulnerable than men to many of the medical consequences of alcohol use. Alcoholic women develop cirrhosis, damage of the heart muscle (i.e., cardiomyopathy), and nerves (i.e., peripheral neuropathy) after fewer years of heavy drinking than alcoholic men.
- Women develop organ damage faster, and at lower levels of alcohol consumption then men. This is because a woman’s body generally has less water than a man’s causing their blood alcohol content to reach higher level, faster.
- Alcohol use may affect female reproductive. Adolescent girls who consume even moderate amounts of alcohol may experience disrupted growth and puberty. Heavy drinking in adult women can disrupt normal menstrual cycling and reproductive functions. Alcohol abuse and alcoholism can cause women to suffer from infertility, increased risk for spontaneous abortion, and impaired fetal growth and development.
- Women overall drink less than men but are more likely to experience adverse consequences including damage to the heart muscle, liver, and brain, trauma resulting from auto crashes, interpersonal violence, and death.
- The progression of alcoholism appears to be faster in women than in men.
Alcohol and Older Drinkers
- Alcohol-related problems, including interactions with prescription and over-the counter drugs, account for most of the substance related problems experienced by older adults.
- Heavy alcohol consumption is known to result in memory deficits. Heavy alcohol consumption also may increase the risk for Alzheimer’s disease in both genders and in women in particular, as they appear to be more vulnerable than men to alcohol–induced brain damage.
- Because of age-related body changes, the National Institute on Alcohol Abuse and Alcoholism recommends that older drinkers consume no more than one drink a day.
Alcohol and Youth
- Young persons reporting first use of alcohol before age 15 were more than 5 times as likely to have past alcohol dependence or abuse compared with persons who first used alcohol at age 21 or older (16 % vs. 3%) .
- Approximately 20% of 8 th graders, 35% of 10 th graders, and 48% of 12th graders report having consumed alcohol during the past month.
- About 12% of 8 th, 22% of 10 th, and 28% of 12th graders report binge drinking (five or more drinks on a single occasion during the past two weeks).
- Almost 40% of high school seniors perceive no great risk in consuming four to five drinks nearly every day.
Alcohol and College Students
- In 2002, 64% of full-time college students (aged 18-22) reported consuming at least one alcoholic drink in the past 30 days.
- Over 44% of full-time college students reported consuming five or more drinks on the same occasion at least once in the past 30 days.
- 1700 college students between the ages of 18 and 24 die each year from alcohol-related unintentional injuries, including motor vehicle crashes.
- Nearly 600,000 students between the ages of 18 and 24 are unintentionally injured under the influence of alcohol.
- Nearly 700,000 students between the ages of 18 and 24 are assaulted each year by another student who has been drinking.