- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
VITAMINS, MINERALS AND SUPPLEMENTS
Multivitamins: So Many Types, So Many Labels
By Melinda Beck : WSJ : June 21, 2011
Your mother made you take them. Many doctors agree. Even the Flintstones seem to endorse them. But do you really need a multivitamin?
How do you know if you need a multivitamin? And how do you choose which one? Melinda Beck explains.
The answer is ... probably not, although much depends on your age, gender, diet and health. One thing is certain: A one-size-fits-all multivitamin can't precisely meet everyone's needs. People over 50 need extra vitamin B-12, but not as much iron as many multivitamins contain. Children who take adult multivitamins may be getting too much vitamin A. And many women need a separate supplement to get extra calcium, since it's too bulky to fit into a multivitamin.
No wonder the vitamin aisle is so confusing, as manufacturers tailor products for different population segments. One-A-Day brand alone offers 14 versions, from Men's 50+ Advantage to Vitacrave Gummies for kids.
Reading labels can lead to even more confusion. Recommended Dietary Allowances (RDA) for vitamins and minerals, which are set by the independent Institute of Medicine, differ by an individual's age and gender. But for convenience, the Food and Drug Administration requires dietary supplements to list a single Daily Value, usually the highest needed.
For some people, that's too high: The RDA for iron, for example, is 8 milligrams for men and postmenopausal women. But the Daily Value on supplement labels is 18 milligrams, the amount recommended for women of childbearing age. What's more, the Daily Values haven't been updated since 1968, even though the institute's recommendations for some vitamins and minerals have changed.
"In some cases, they are wildly off," says Paul Coates, director of the National Institute of Health's Office of Dietary Supplements. An FDA spokeswoman said the agency is considering revisions.
There is no standard multivitamin formula. The term applies to any combination of vitamins and minerals in any strength, as long as they are listed on the label.
The label may not even exactly match what's in the bottle. ConsumerLab, a supplement-testing company, reported last week that 10 of 38 multivitamin brands tested contained either more or less of some ingredients than the label indicated.
And price was no predictor of quality. Some multivitamins selling for less than 10 cents a day performed better on the tests than those selling for 50 cents or more.
The Council for Responsible Nutrition, a trade group that represents most multivitamin and other supplement makers, says, "It concerns us anytime ConsumerLab says we don't meet label claims," says CRN's chief executive and president. Steven Mister. "But there is nothing in the report that suggests that consumers are getting levels that will do them harm."
Are multivitamins even necessary? The dietary supplement industry likens them to nutritional insurance—filling in gaps when people don't eat perfectly balanced meals.
That rationale has helped make multivitamins, introduced in the 1940s, the best-selling dietary supplement, with more than $4.8 billion in sales in 2008, according to Nutrition Business Journal. A third of American adults take them regularly. Use is particularly high among women, children, physicians, the elderly and people with high incomes, low body-mass indexes and healthy eating habits, according to government surveys.
Given those traits and demographics, people most likely to benefit from multivitamins—due to unhealthy habits—also are least likely to take them. Conversely, because people who take multivitamins tend to have other healthy habits, it's difficult to prove what effect multivitamins have, if any, in overall health.
Looking at randomized controlled trials, the gold standard for determining cause-and-effect, a NIH panel in 2007 concluded that "the present evidence is insufficient to recommend either for or against the use of [multivitamins and minerals] by the American public to prevent chronic disease." A 2003 U.S. Preventive Services Task Force report found insufficient evidence either for or against taking multivitamins to prevent cancer or cardiovascular disease.
The dietary-supplement trade group says observational studies have shown benefits, including a lower risk of cataracts and colon cancer, and fewer colds.
Such studies, though, can't determine cause and effect, only association. And several large observational trials have come to opposite conclusions.
A study in the American Journal of Epidemiology this year that followed 182,000 people in Hawaii and California for 11 years found no association between multivitamin use and deaths from cancer, cardiovascular disease or any cause.
Compared with over-the-counter and prescription drugs, dietary supplements are lightly regulated. Makers don't need to demonstrate that they are safe or effective. But there are limits to what they can claim. Ads that use terms such as "support" breast health or mental alertness must note that such statements haven't been evaluated by the FDA and that the product isn't intended to diagnose, treat, cure or prevent any disease.
Still, a scientific consensus has emerged that some groups of people do require more of certain nutrients than they are likely to get from food. Women who might become pregnant should get an additional 400 micrograms a day of folic acid, to reduce the risk of serious neurological issues in a fetus that may occur even before a woman knows she is pregnant.
People over age 50 should get the recommended 2.4 micrograms of vitamin B-12 from supplements or fortified foods because they become less able to absorb it from food as they age. Vegetarians and vegans also need extra B-12.
Infants who are being breastfed should get 400 International Units (IUs) a day of supplement vitamin D until they are weaned. In fact, most Americans need 600 IUs per day, according to a 2010 report from the Institute of Medicine. People who get minimal sun exposure and don't consume much salmon or milk also should supplement their Vitamin D.
On the other hand, some people may get too much of certain nutrients, depending on their age and health, particularly if they use the current Daily Values listed on labels as a guide. For example, 100% of the current Daily Value for vitamin A is 5,000 IUs—which is over the Institute of Medicine's safe upper limit of 2,000 IUs for children and far beyond the RDA for children ages 1 through 3 of just 1,000 IUs. Excess vitamin A can cause headaches, hair loss, visual disturbances and a possibly increased risk of osteoporosis. And smokers should avoid taking extra beta carotene, which has been linked to increased risk of lung cancer.
The consumer-advocacy group Center for Science in the Public Interest has asked the FDA to require warning labels on multivitamins and other supplements for some of these conditions.
Officials at the dietary-supplement trade group say evidence of the need for such warnings is scant, and the upper limit for vitamins is still safe. "That's not to say that if you cross that threshold, you will have a fatal condition," says Duffy MacKay, a naturopathic doctor and CRN vice president.
Given all the complexities, it pays to discuss individual needs with a doctor, dietitian or other health professional. Some people may find the à la carte approach works best. Others may like the extra "insurance" provided by a multivitamin targeted to their age and sex.
Dr. Coates, of the NIH, says based on the best evidence, "If you are taking multivitamins, there is no reason to stop, and if you are not taking them, there is no reason to start. You are unlikely to harm yourself, whatever you're doing."
What Do You Lack? Probably Vitamin D
By Jane E. Brody : NY Times : July 26, 2010
Vitamin D promises to be the most talked-about and written-about supplement of the decade. While studies continue to refine optimal blood levels and recommended dietary amounts, the fact remains that a huge part of the population — from robust newborns to the frail elderly, and many others in between — are deficient in this essential nutrient.
If the findings of existing clinical trials hold up in future research, the potential consequences of this deficiency are likely to go far beyond inadequate bone development and excessive bone loss that can result in falls and fractures. Every tissue in the body, including the brain, heart, muscles and immune system, has receptors for vitamin D, meaning that this nutrient is needed at proper levels for these tissues to function well.
Studies indicate that the effects of a vitamin D deficiency include an elevated risk of developing (and dying from) cancers of the colon, breast and prostate; high blood pressure and cardiovascular disease; osteoarthritis; and immune-system abnormalities that can result in infections and autoimmune disorders like multiple sclerosis, Type 1 diabetes and rheumatoid arthritis.
Most people in the modern world have lifestyles that prevent them from acquiring the levels of vitamin D that evolution intended us to have. The sun’s ultraviolet-B rays absorbed through the skin are the body’s main source of this nutrient. Early humans evolved near the equator, where sun exposure is intense year round, and minimally clothed people spent most of the day outdoors.
“As a species, we do not get as much sun exposure as we used to, and dietary sources of vitamin D are minimal,” Dr. Edward Giovannucci, nutrition researcher at the Harvard School of Public Health, wrote in The Archives of Internal Medicine. Previtamin D forms in sun-exposed skin, and 10 to 15 percent of the previtamin is immediately converted to vitamin D, the form found in supplements. Vitamin D, in turn, is changed in the liver to 25-hydroxyvitamin D, the main circulating form. Finally, the kidneys convert 25-hydroxyvitamin D into the nutrient’s biologically active form, 1,25-dihydroxyvitamin D, also known as vitamin D hormone.
A person’s vitamin D level is measured in the blood as 25-hydroxyvitamin D, considered the best indicator of sufficiency. A recent study showed that maximum bone density is achieved when the blood serum level of 25-hydroxyvitamin D reaches 40 nanograms per milliliter or more.
“Throughout most of human evolution,” Dr. Giovannucci wrote, “when the vitamin D system was developing, the ‘natural’ level of 25-hydroxyvitamin D was probably around 50 nanograms per milliliter or higher. In modern societies, few people attain such high levels.”
A Common Deficiency
Although more foods today are supplemented with vitamin D, experts say it is rarely possible to consume adequate amounts through foods. The main dietary sources are wild-caught oily fish (salmon, mackerel, bluefish, and canned tuna) and fortified milk and baby formula, cereal and orange juice.
People in colder regions form their year’s supply of natural vitamin D in summer, when ultraviolet-B rays are most direct. But the less sun exposure, the darker a person’s skin and the more sunscreen used, the less previtamin D is formed and the lower the serum levels of the vitamin. People who are sun-phobic, babies who are exclusively breast-fed, the elderly and those living in nursing homes are particularly at risk of a serious vitamin D deficiency.
Dr. Michael Holick of Boston University, a leading expert on vitamin D and author of “The Vitamin D Solution” (Penguin Press, 2010), said in an interview, “We want everyone to be above 30 nanograms per milliliter, but currently in the United States, Caucasians average 18 to 22 nanograms and African-Americans average 13 to 15 nanograms.” African-American women are 10 times as likely to have levels at or below 15 nanograms as white women, the third National Health and Nutrition Examination Survey found.
Such low levels could account for the high incidence of several chronic diseases in this country, Dr. Holick maintains. For example, he said, in the Northeast, where sun exposure is reduced and vitamin D levels consequently are lower, cancer rates are higher than in the South. Likewise, rates of high blood pressure, heart disease, and prostate cancer are higher among dark-skinned Americans than among whites.
The rising incidence of Type 1 diabetes may be due, in part, to the current practice of protecting the young from sun exposure. When newborn infants in Finland were given 2,000 international units a day, Type 1 diabetes fell by 88 percent, Dr. Holick said.
The current recommended intake of vitamin D, established by the Institute of Medicine, is 200 I.U. a day from birth to age 50 (including pregnant women); 400 for adults aged 50 to 70; and 600 for those older than 70. While a revision upward of these amounts is in the works, most experts expect it will err on the low side. Dr. Holick, among others, recommends a daily supplement of 1,000 to 2,000 units for all sun-deprived individuals, pregnant and lactating women, and adults older than 50. The American Academy of Pediatrics recommends that breast-fed infants receive a daily supplement of 400 units until they are weaned and consuming a quart or more each day of fortified milk or formula.
Given appropriate sun exposure in summer, it is possible to meet the body’s yearlong need for vitamin D. But so many factors influence the rate of vitamin D formation in skin that it is difficult to establish a universal public health recommendation. Asked for a general recommendation, Dr. Holick suggests going outside in summer unprotected by sunscreen (except for the face, which should always be protected) wearing minimal clothing from 10 a.m. to 3 p.m. two or three times a week for 5 to 10 minutes.
Slathering skin with sunscreen with an SPF of 30 will reduce exposure to ultraviolet-B rays by 95 to 98 percent. But if you make enough vitamin D in your skin in summer, it can meet the body’s needs for the rest of the year, Dr. Holick said.
Can You Get Too Much?
If acquired naturally through skin, the body’s supply of vitamin D has a built-in cutoff. When enough is made, further exposure to sunlight will destroy any excess. Not so when the source is an ingested supplement, which goes directly to the liver.
Symptoms of vitamin D toxicity include nausea, vomiting, poor appetite, constipation, weakness and weight loss, as well as dangerous amounts of calcium that can result in kidney stones, confusion and abnormal heart rhythms.
But both Dr. Giovannucci and Dr. Holick say it is very hard to reach such toxic levels. Healthy adults have taken 10,000 I.U. a day for six months or longer with no adverse effects. People with a serious vitamin D deficiency are often prescribed weekly doses of 50,000 units until the problem is corrected. To minimize the risk of any long-term toxicity, these experts recommend that adults take a daily supplement of 1,000 to 2,000 units.
An Oldie Vies for Nutrient of the Decade
By Jane E. Brody : NY Times : February 19, 2008
The so-called sunshine vitamin is poised to become the nutrient of the decade, if a host of recent findings are to be believed. Vitamin D, an essential nutrient found in a limited number of foods, has long been renowned for its role in creating strong bones, which is why it is added to milk.
Now a growing legion of medical researchers have raised strong doubts about the adequacy of currently recommended levels of intake, from birth through the sunset years. The researchers maintain, based on a plethora of studies, that vitamin D levels considered adequate to prevent bone malformations like rickets in children are not optimal to counter a host of serious ailments that are now linked to low vitamin D levels.
To be sure, not all medical experts are convinced of the need for or the desirability of raising the amount of vitamin D people should receive, either through sunlight, foods, supplements or all three. The federal committee that establishes daily recommended levels of nutrients has resisted all efforts to increase vitaminD intake significantly, partly because the members are not convinced of assertions for its health-promoting potential and partly because of time-worn fears of toxicity.
This column will present the facts as currently known, but be forewarned. In the end, you will have to decide for yourself how much of this vital nutrient to consume each and every day and how to obtain it.
Where to Obtain It
Through most of human history, sunlight was the primary source of vitamin D, which is formed in skin exposed to ultraviolet B radiation (the UV light that causes sunburns). Thus, to determine how much vitaminD is needed from food and supplements, take into account factors like skin color, where you live, time of year, time spent out of doors, use of sunscreens and coverups and age.
Sun avoiders and dark-skinned people absorb less UV radiation. People in the northern two-thirds of the country make little or no vitamin D in winter, and older people make less vitamin D in their skin and are less able to convert it into the hormone that the body uses. In addition, babies fed just breast milk consume little vitamin D unless given a supplement.
In addition to fortified drinks like milk, soy milk and some juices, the limited number of vitamin D food sources include oily fish like salmon, mackerel, bluefish, catfish, sardines and tuna, as well as cod liver oil and fish oils. The amount of vitamin D in breakfast cereals is minimal at best. As for supplements, vitamin D is found in prenatal vitamins, multivitamins, calcium-vitamin D combinations and plain vitamin D. Check the label, and select brands that contain vitamin D3, or cholecalciferol. D2, or ergocalciferol, is 25 percent less effective.
Vitamin D content is listed on labels in international units (I.U.). An eight-ounce glass of milk or fortified orange juice is supposed to contain 100 I.U. Most brands of multivitamins provide 400 a day. Half a cup of canned red salmon has about 940, and three ounces of cooked catfish about 570.
Myriad Links to Health
Let’s start with the least controversial role of vitamin D — strong bones. Last year, a 15-member team of nutrition experts noted in The American Journal of Clinical Nutrition that “randomized trials using the currently recommended intakes of 400 I.U. vitamin D a day have shown no appreciable reduction in fracture risk.”
“In contrast,” the experts continued, “trials using 700 to 800 I.U. found less fracture incidence, with and without supplemental calcium. This change may result from both improved bone health and reduction in falls due to greater muscle strength.”
A Swiss study of women in their 80s found greater leg strength and half as many falls among those who took 800 I.U. of vitamin D a day for three months along with 1,200 milligrams of calcium, compared with women who took just calcium. Greater strength and better balance have been found in older people with high blood levels of vitamin D.
In animal studies, vitamin D has strikingly reduced tumor growth, and a large number of observational studies in people have linked low vitamin D levels to an increased risk of cancer, including cancers of the breast, rectum, ovary, prostate, stomach, bladder, esophagus, kidney, lung, pancreas and uterus, as well as Hodgkin’s lymphoma and multiple myeloma.
Researchers at Creighton University in Omaha conducted a double-blind, randomized, placebo-controlled trial (the most reliable form of clinical research) among 1,179 community-living, healthy postmenopausal women. They reported last year in The American Journal of Clinical Nutrition that over the course of four years, those taking calcium and 1,100 I.U. of vitamin D3 each day developed about 80 percent fewer cancers than those who took just calcium or a placebo.
Vitamin D seems to dampen an overactive immune system. The incidence of autoimmune diseases like Type 1 diabetes and multiple sclerosis has been linked to low levels of vitamin D. A study published on Dec. 20, 2006, in The Journal of the American Medical Association examined the risk of developing multiple sclerosis among more than seven million military recruits followed for up to 12 years. Among whites, but not blacks or Hispanics, the risk of developing M.S. increased with ever lower levels of vitamin D in their blood serum before age 20.
A study published in Neurology in 2004 found a 40 percent lower risk of M.S. in women who took at least 400 I.U. of vitamin D a day.
Likewise, a study of a national sample of non-Hispanic whites found a 75 percent lower risk of diabetesvitamin D.
Vitamin D is a fat-soluble vitamin that when consumed or made in the skin can be stored in body fat. In summer, as little as five minutes of sun a day on unprotected hands and face can replete the body’s supply. Any excess can be stored for later use. But for most people during the rest of the year, the body needs dietary help.
Furthermore, the general increase in obesity has introduced a worrisome factor, the tendency for body fat to hold on to vitamin D, thus reducing its overall availability.
As for a maximum safe dose, researchers like Bruce W. Hollis, a pediatric nutritionist at the Medical University of South Carolina in Charleston, maintain that the current top level of 2,000 I.U. is based on shaky evidence indeed — a study of six patients in India. Dr. Hollis has been giving pregnant women 4,000 I.U. a day, and nursing women 6,000, with no adverse effects. Other experts, however, are concerned that high vitamin D levels (above 800 I.U.) with calcium can raise the risk of kidney stones in susceptible people.
Phys Ed: Can Vitamin D Improve Your Athletic Performance?
By Gretchen Reynolds : NY Times Article : September 23, 2009
When scientists at the Australian Institute of Sport recently decided to check the Vitamin D status of some of that country’s elite female gymnasts, their findings were fairly alarming. Of the 18 gymnasts tested, 15 had levels that were “below current recommended guidelines for optimal bone health,” the study’s authors report. Six of these had Vitamin D levels that would qualify as medically deficient. Unlike other nutrients, Vitamin D can be obtained by exposure to ultraviolet radiation from sunlight, as well as through foods or supplements. Of course, female gymnasts are a unique and specialized bunch, not known for the quality or quantity of their diets, or for getting outside much.
But in another study presented at a conference earlier this year, researchers found that many of a group of distance runners also had poor Vitamin D status. Forty percent of the runners, who trained outdoors in sunny Baton Rouge, Louisiana, had insufficient Vitamin D. “It was something of a surprise,” says D. Enette Larson-Meyer, an assistant professor in the Department of Family and Consumer Sciences at the University of Wyoming and one of the authors of the study.
Vitamin D is an often overlooked element in athletic achievement, a “sleeper nutrient,” says John Anderson, a professor emeritus of nutrition at the University of North Carolina and one of the authors of a review article published online in May about Vitamin D and athletic performance. Vitamin D once was thought to be primarily involved in bone development. But a growing body of research suggests that it’s vital in multiple different bodily functions, including allowing body cells to utilize calcium (which is essential for cell metabolism), muscle fibers to develop and grow normally, and the immune system to function properly. “Almost every cell in the body has receptors” for Vitamin D, Anderson says. “It can up-regulate and down-regulate hundreds, maybe even thousands of genes,” Larson-Meyer says. “We’re only at the start of understanding how important it is.”
But many of us, it seems, no matter how active and scrupulous we are about health, don’t get enough Vitamin D. Nowadays, “many people aren’t going outside very much,” Johnson says, and most of us
assiduously apply sunscreen and take other precautions when we do. The Baton Rouge runners, for instance, most likely “ran early in the morning or late in the day,” Larson-Meyer says, reducing their chances of heat stroke or sunburn, but also reducing their exposure to sunlight.
Meanwhile, dietary sources of Vitamin D are meager. Cod-liver oil provides a whopping dose. But a glass of fortified milk provides a fraction of what scientists now think we need per day. (A major study published online in the journal Pediatrics last month concluded that more than 60 percent of American children, or almost 51 million kids, have “insufficient” levels of Vitamin D and another 9 percent, or 7.6 million children, are clinically “deficient,” a serious condition. Cases of childhood rickets, a bone disease caused by lack of Vitamin D, have been rising in the U.S. in recent years.)
Although few studies have looked closely at the issue of Vitamin D and athletic performance, those that have are suggestive. A series of strange but evocative studies undertaken decades ago in Russia and Germany, for instance, hint that the Eastern Bloc nations may have depended in part on sunlamps and Vitamin D to produce their preternaturally well-muscled and world-beating athletes. In one of the studies, four Russian sprinters were doused with artificial, ultraviolet light. Another group wasn’t. Both trained identically for the 100-meter dash. The control group lowered their sprint times by 1.7 percent. The radiated runners, in comparison, improved by an impressive 7.4 percent.
More recently, when researchers tested the vertical jumping ability of a small group of adolescent athletes, Larson-Meyer says, “they found that those who had the lowest levels of Vitamin D tended not to jump as high,” intimating that too little of the nutrient may impair muscle power. Low levels might also contribute to sports injuries, in part because Vitamin D is so important for bone and muscle health. In a Creighton University study of female naval recruits, stress fractures were reduced significantly after the women started taking supplements of Vitamin D and calcium.
A number of recent studies also have shown that, among athletes who train outside year-round, maximal oxygen intake tends to be highest in late summer, Johnson says. The athletes, in other words, are fittest in August, when ultraviolet radiation from the sun is near its zenith. They often then experience an abrupt drop in maximal oxygen intake,
beginning as early as September, even thought they continue to train just as hard. This decline coincides with the autumnal lengthening of the angle of sunlight. Less ultraviolet radiation reaches the earth and, apparently, sports performance suffers.
Concerned now about your Vitamin D status? You can learn your status with a simple blood test. An at-home version is available through the Web site of the Vitamin D Council. (Use of the tests is restricted in some states, including New York. See the website for details.) Be sure that any test checks the level of 25(OH)D in your blood. This level “should generally be above 50 nanograms per milliliter,” Larson-Meyer says.
If your levels are low, talk to your doctor about the best response. Sunlight is one easy, if controversial, fix. “Most dermatologists will still tell you that no amount of sun exposure is safe,” Johnson says.
But Larson-Meyer and other Vitamin D researchers aren’t so sure. “There’s no good, scientific evidence that five to thirty minutes of sunlight a few times a week is harmful,” she says.
Or try supplements. “1,000 IU a day and much more for people who are deficient” is probably close to ideal, Larson-Meyer says. This, by the way, is about double the current recommended daily allowance. Most experts anticipate that this allowance will be revised upward soon. Consult with your doctor before beginning supplements. Overdoses of Vitamin D are rare, but can occur.
Finally, stay tuned. “In the next few years, we’re going to be learning much more” about the role of vitamin D in bodily function and sports performance, Larson-Meyer says.
Vitamins: An Overview
Vitamins are a group of substances essential for normal cell function, growth and development.
There are 13 essential vitamins. That means they are needed for the body to function. They are:
Vitamins are grouped into two categories:
Each vitamin has specific functions. You can develop health problems (deficiency disease) if you do not get enough of a particular vitamin.
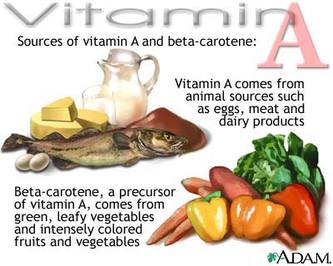
Vitamin A helps form and maintain healthy teeth, bones, soft tissue, mucous membranes, and skin.
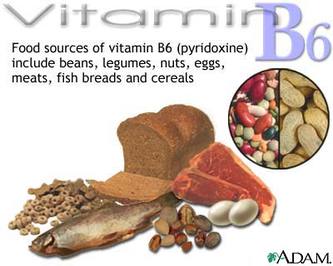
Vitamin B6 is also called pyridoxine. The more protein you eat, the more vitamin B6 is needed to help the body use protein. Vitamin B6 helps form red blood cells and maintain brain function, among other things.
Vitamin B12 , like the other B vitamins, is important for metabolism. It also helps form red blood cells and maintain the central nervous system.
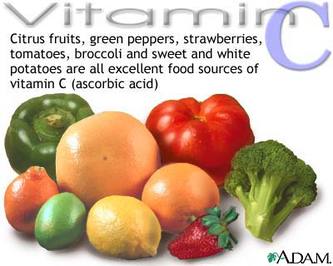
Vitamin C , also called ascorbic acid, is an antioxidant that promotes healthy teeth and gums. It helps the body absorb iron and maintain healthy tissue. It also promotes wound healing.
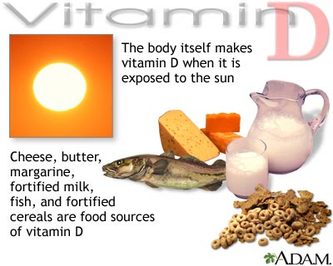
Vitamin D is also known as the "sunshine vitamin," since it is made by the body after being in the sun. Ten to 15 minutes of sunshine 3 times a week is enough to produce the body's requirement of vitamin D. However, many people living in sunny climates still do not make enough vitamin D and need more from their diet or supplements. Vitamin D helps the body absorb calcium, which you need for the normal development and maintenance of healthy teeth and bones. It also helps maintain proper blood levels of calcium and phosphorus.
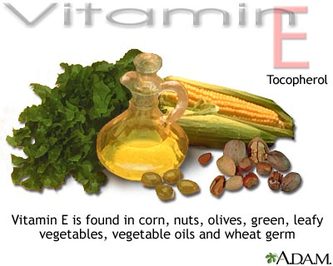
Vitamin E is an antioxidant also known as tocopherol. It plays a role in the formation of red blood cells and helps the body use vitamin K.
Vitamin K is not listed among the essential vitamins, but without it blood would not stick together (coagulate). Some studies suggest that it helps promote strong bones in the elderly.
Biotin is essential for the metabolism of proteins and carbohydrates, and in the production of hormones and cholesterol.
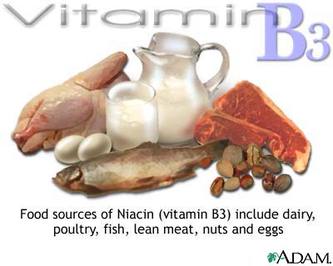
Niacin is a B vitamin that helps maintain healthy skin and nerves. It is also has cholesterol-lowering effects.
Folate works with vitamin B12 to help form red blood cells. It is necessary for the production of DNA, which controls tissue growth and cell function. Any woman who is pregnant should be sure to get enough folate. Low levels of folate are linked to birth defects such as spina bifida. Many foods are now fortified with folic acid.
Pantothenic acid is essential for the metabolism of food. It is also plays a role in the production of hormones and cholesterol.
Riboflavin (B2) works with the other B vitamins. It is important for body growth and the production of red blood cells.
Thiamine (B1) helps the body cells change carbohydrates into energy. It is also essential for heart function and healthy nerve cells.
Food Sources:
FAT-SOLUBLE VITAMINS
Vitamin A:
Vitamin D:
Vitamin E:
Vitamin K:
WATER-SOLUBLE VITAMINS
Folate:
Niacin (B3):
Pantothenic acid and biotin
Thiamine (B1):
Vitamin B12:
Vitamin C (ascorbic acid)
Side Effects
Many people think that if some is good, a lot is better. This is not always the case. High doses of certain vitamins can be poisonous. Ask your doctor what is best for you.
Recommendations
The Food and Nutrition Board at the Institute of Medicine establish recommended dietary allowances (RDAs) for vitamins. The recommendations reflect how much of each nutrient you should receive on a daily basis, based on the known nutritional needs of practically all healthy people.
The best way to get the daily requirement of essential vitamins is to eat a balanced diet that contains a variety of foods from the food guide pyramid.
Specific recommendations for each vitamin depend on age, gender, and other factors (such as pregnancy).
There are 13 essential vitamins. That means they are needed for the body to function. They are:
- Vitamin A
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamin B1 (thiamine)
- Vitamin B2 (riboflavin)
- Vitamin B3 (niacin)
- Pantothenic acid
- Biotin
- Vitamin B6
- Vitamin B12
- Folate (folic acid)
Vitamins are grouped into two categories:
- Fat-soluble vitamins are stored in the body''s fatty tissue.
- Water-soluble vitamins must be used by the body right away. Any left over water-soluble vitamins leave the body through the urine. Vitamin B12 is the only water-soluble vitamin that can be stored in the liver for many years.
Each vitamin has specific functions. You can develop health problems (deficiency disease) if you do not get enough of a particular vitamin.
Vitamin A helps form and maintain healthy teeth, bones, soft tissue, mucous membranes, and skin.
Vitamin B6 is also called pyridoxine. The more protein you eat, the more vitamin B6 is needed to help the body use protein. Vitamin B6 helps form red blood cells and maintain brain function, among other things.
Vitamin B12 , like the other B vitamins, is important for metabolism. It also helps form red blood cells and maintain the central nervous system.
Vitamin C , also called ascorbic acid, is an antioxidant that promotes healthy teeth and gums. It helps the body absorb iron and maintain healthy tissue. It also promotes wound healing.
Vitamin D is also known as the "sunshine vitamin," since it is made by the body after being in the sun. Ten to 15 minutes of sunshine 3 times a week is enough to produce the body's requirement of vitamin D. However, many people living in sunny climates still do not make enough vitamin D and need more from their diet or supplements. Vitamin D helps the body absorb calcium, which you need for the normal development and maintenance of healthy teeth and bones. It also helps maintain proper blood levels of calcium and phosphorus.
Vitamin E is an antioxidant also known as tocopherol. It plays a role in the formation of red blood cells and helps the body use vitamin K.
Vitamin K is not listed among the essential vitamins, but without it blood would not stick together (coagulate). Some studies suggest that it helps promote strong bones in the elderly.
Biotin is essential for the metabolism of proteins and carbohydrates, and in the production of hormones and cholesterol.
Niacin is a B vitamin that helps maintain healthy skin and nerves. It is also has cholesterol-lowering effects.
Folate works with vitamin B12 to help form red blood cells. It is necessary for the production of DNA, which controls tissue growth and cell function. Any woman who is pregnant should be sure to get enough folate. Low levels of folate are linked to birth defects such as spina bifida. Many foods are now fortified with folic acid.
Pantothenic acid is essential for the metabolism of food. It is also plays a role in the production of hormones and cholesterol.
Riboflavin (B2) works with the other B vitamins. It is important for body growth and the production of red blood cells.
Thiamine (B1) helps the body cells change carbohydrates into energy. It is also essential for heart function and healthy nerve cells.
Food Sources:
FAT-SOLUBLE VITAMINS
Vitamin A:
- Eggs
- Meat
- Milk
- Cheese
- Cream
- Liver
- Kidney
- Cod
- Halibut fish oil
Vitamin D:
- Cheese
- Butter
- Margarine
- Cream
- Fortified milk
- Fish
- Oysters
- Cereals
Vitamin E:
- Wheat germ
- Corn
- Nuts
- Seeds
- Olives
- Spinach and other green leafy vegetables
- Asparagus
- Vegetable oils and products made from vegetable oils, such as margarine
Vitamin K:
- Cabbage
- Cauliflower
- Spinach
- Soybeans
- Cereals
WATER-SOLUBLE VITAMINS
Folate:
- Green, leafy vegetables
- Fortified foods
Niacin (B3):
- Dairy products
- Poultry
- Fish
- Lean meats
- Nuts
- Eggs
- Legumes
- Enriched breads and cereals
Pantothenic acid and biotin
- Eggs
- Fish
- Dairy products
- Whole-grain cereals
- Legumes
- Yeast
- Broccoli and other vegetables in the cabbage family
- White and sweet potatoes
- Lean beef
Thiamine (B1):
- Fortified breads, cereals, and pasta
- Whole grains
- Lean meats
- Fish
- Dried beans
- Peas
- Soybeans
- Dairy products
- Fruits and vegetables
Vitamin B12:
- Meat
- Eggs
- Poultry
- Shellfish
- Milk and milk products
Vitamin C (ascorbic acid)
- Citrus fruits and juices
- Strawberries
- Tomatoes
- Broccoli
- Turnip and other greens
- Sweet and white potatoes
- Cantaloupe
Side Effects
Many people think that if some is good, a lot is better. This is not always the case. High doses of certain vitamins can be poisonous. Ask your doctor what is best for you.
Recommendations
The Food and Nutrition Board at the Institute of Medicine establish recommended dietary allowances (RDAs) for vitamins. The recommendations reflect how much of each nutrient you should receive on a daily basis, based on the known nutritional needs of practically all healthy people.
The best way to get the daily requirement of essential vitamins is to eat a balanced diet that contains a variety of foods from the food guide pyramid.
Specific recommendations for each vitamin depend on age, gender, and other factors (such as pregnancy).
Dietary supplements: Nutrition in a pill?
When using dietary supplements, assess your needs, evaluate the merits of taking supplements, and understand how to choose and use them.
By Mayo Clinic staff
Dietary supplements aren't intended to be a food substitute because they can't replicate all of the nutrients and benefits of whole foods, such as fruits and vegetables. So if you're generally healthy and eat a balanced diet, daily dietary supplements may not be worth the expense. However, if you can't eat enough healthy foods or have certain conditions, you may benefit from taking a daily dietary supplement
Whole foods: Your best source of micronutrients Whole foods are your best sources of vitamins and minerals. They offer three main benefits over dietary supplements:
However, if you can't eat enough healthy foods, you may benefit from taking a daily dietary supplement. Dietary supplements may be appropriate if you:
Choosing and using dietary supplements If you decide to take a vitamin or mineral supplement, consider these tips:
When using dietary supplements, assess your needs, evaluate the merits of taking supplements, and understand how to choose and use them.
By Mayo Clinic staff
Dietary supplements aren't intended to be a food substitute because they can't replicate all of the nutrients and benefits of whole foods, such as fruits and vegetables. So if you're generally healthy and eat a balanced diet, daily dietary supplements may not be worth the expense. However, if you can't eat enough healthy foods or have certain conditions, you may benefit from taking a daily dietary supplement
Whole foods: Your best source of micronutrients Whole foods are your best sources of vitamins and minerals. They offer three main benefits over dietary supplements:
- Greater nutrition. Whole foods are complex, containing a variety of the micronutrients your body needs — not just one. An orange, for example, provides vitamin C plus some beta carotene, calcium and other nutrients. A vitamin C supplement lacks these other micronutrients.
- Essential fiber. Whole foods provide dietary fiber. Fiber, as part of a healthy diet, can help prevent certain diseases, such as type 2 diabetes and heart disease, and it can also help manage constipation.
- Protective substances. Whole foods contain other substances recognized as important for good health. Fruits and vegetables, for example, contain naturally occurring food substances called phytochemicals, which may help protect you against cancer, heart disease, diabetes and high blood pressure. Many are also good sources of antioxidants — substances that slow down oxidation, a natural process that leads to cell and tissue damage.
However, if you can't eat enough healthy foods, you may benefit from taking a daily dietary supplement. Dietary supplements may be appropriate if you:
- Don't eat well or consume less than 1,600 calories a day
- Are a vegan or a vegetarian who eats a limited variety of foods
- Are pregnant, trying to get pregnant or breast-feeding
- Are a woman who experiences heavy bleeding during your menstrual period
- Are a postmenopausal woman
- Have a medical condition that affects how your body absorbs, uses or excretes nutrients, such as chronic diarrhea, food allergies, food intolerance or a disease of the liver, gallbladder, intestines or pancreas
- Have had surgery on your digestive tract and are not able to digest and absorb nutrients properly
Choosing and using dietary supplements If you decide to take a vitamin or mineral supplement, consider these tips:
- Check the supplement label. Read labels carefully. Product labels can tell you what the active ingredient or ingredients are, which nutrients are included, the serving size — for example, capsule, packet or teaspoonful — and the amount of nutrients in each serving.
- Avoid supplements that provide megadoses. In general, choose a multivitamin-mineral supplement that provides about 100 percent of the Daily Value (DV) of all the vitamins and minerals, rather than one which has, for example, 500 percent of the DV for one vitamin and only 20 percent of the DV for another. The exception to this is calcium. You may notice that calcium-containing supplements don't provide 100 percent of the DV. If they did, the tablets would be too large to swallow.
- Look for USP on the label. This ensures that the supplement meets the standards for strength, purity, disintegration and dissolution established by the testing organization U.S. Pharmacopeia (USP).
- Check expiration dates. Dietary supplements can lose potency over time, especially in hot and humid climates. If a supplement doesn't have an expiration date, don't buy it. If your supplements have expired, discard them.
- Store all vitamin and mineral supplements safely. Put supplements in a locked cabinet or other secure location out of children's reach. Don't leave supplements on the counter or rely on child-resistant packaging. Store dietary supplements in a dry, cool place. Avoid hot, humid storage locations, such as in the bathroom.
- Check alerts and advisories. The Food and Drug Administration keeps a list of dietary supplements that are under regulatory review or that have been reported to cause adverse effects. Check its website periodically for updates.