- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Celiac Disease
or Gluten Sensitive Enteropathy
Celiac Disease, a Common, but Elusive, Diagnosis
By Jane E. Brody : NY Times : September 29, 2014
The trouble for Daniel Tully, then 12 and an excellent student and athlete in Brooklyn, began 20 months ago, when he developed what seemed like a virus that kept recurring, each time sending him to bed and keeping him from school for a week.
In January, he came down with an intestinal bug from which he never seemed to recover. He developed severe headaches whenever he tried to read or concentrate, became extremely weak, mentally foggy and unable to go to school at all. He vomited violently after meals, lost weight, and eventually could not walk unaided.
“I had to carry him to the bathroom,” recalled his father, Ed Tully.
When a child develops such a devastating constellation of symptoms, you’d think his doctors might consider testing for celiac disease, an autoimmune reaction to dietary gluten that can destroy the small intestine. Awareness of the problem has never been greater.
But even in the most sophisticated medical settings, the diagnosis can be missed or the tests done incorrectly. Over four days in a local hospital, Daniel’s doctors performed an intestinal biopsy. But only two samples were taken, which missed the severe damage in his small intestine.
He finally saw a pediatric immunologist and was given the blood test specific for celiac disease. It was unequivocally positive. The diagnosis was confirmed by a second intestinal biopsy, this time with the recommended six or more samples.
Daniel began a strict gluten-free diet five months ago and is gradually recovering. With intensive physical therapy and a diet rich in meat, he is regaining lost strength, weight and stamina. His doctors say it may take a year, but he eventually will achieve normal growth — as long as he sticks religiously to the diet.
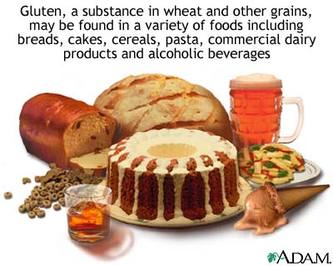
Gluten is a protein in grains like wheat, rye and barley that contains gliadin peptides. In people with celiac disease, these can trigger an autoimmune reaction that damages the villi, tiny projections lining the small intestine that absorb nutrients from food into the body. Like Daniel, people with celiac disease must avoid wheat, rye or barley, or any of the thousands of products or ingredients made from these grains. Some must also abstain from oats.
The disease runs in families: Some of Daniel’s first and second cousins have it, and Daniel’s younger sister is now being tested for it.
First-degree relatives of someone with celiac disease should also be tested for it, even if they have no symptoms. If another person in the immediate family has the disease, second-degree relatives should be tested, Dr. Joseph A. Murray, a gastroenterologist at the Mayo Clinic, said in an interview.
“Celiac disease is now five times more common than it was 50 years ago, and that’s not just the result of better diagnoses,” said Dr. Murray, who is also editor of “Mayo Clinic Going Gluten Free,” to be published in November. “We looked at old stored blood samples, and that showed a real increase in incidence.”
For reasons unknown, celiac disease now affects one in 100 Caucasians, Dr. Murray said. It does occur in other racial groups, but is believed to be much less common.
Hygienic extremes may be to blame for the increase: Overzealous cleanliness has been linked to a rise in autoimmune diseases. But experts speculate the increase also may have to do with how grains are bred these days, or the overreliance on formula to feed infants. Although traditionally considered a disease that shows up in childhood, people of all ages may develop it. One person I know was diagnosed in his 50s, another in her 60s.
But the overwhelming majority of people with celiac disease remain undiagnosed. The most recent data show that only 17 percent of Americans with the disease know they have it. Those who are not avoiding gluten risk developing a host of debilitating, sometimes fatal complications, including cancer.
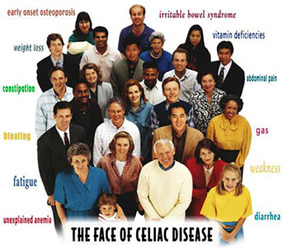
A main reason for this lag in detection is the long and confusing list of signs and symptoms, some of which may be mild enough to be easily ignored or attributed to another condition, like irritable bowel syndrome or an allergy.
Abdominal pain and bloating are the most common signs. But according to a recent review in JAMA Pediatrics, possible symptoms include chronic or intermittent constipation; vomiting;loss of appetite; weight loss (or, in children, growth failure); fatigue;iron deficiency anemia; abnormal dental enamel; mouth ulcers;arthritis and joint pain; bone loss and fractures; short stature; delayed puberty; unexplained infertility and miscarriage; recurring headaches; loss of feeling in hands and feet; poor coordination and unsteadiness; seizures; depression; hallucinations, anxiety and panic attacks. “Doctors have to raise their index of suspicion,” Dr. Murray said. “At least half of patients don’t have diarrhea. It can present in so many ways.”
About one-third of his patients had asked doctors on their own for testing, he added. It is critically important to be tested before going on a gluten-free diet, which can disguise the intestinal damage characteristic of the condition. Those already eating a restricted diet would have to return to gluten (say, eating two slices of bread a day for two weeks) for the test to be accurate.
Avoiding gluten has become easier in recent years as companies have loaded store shelves with gluten-free foods. A new Food and Drug Administration rule stipulates that any food labeled gluten-free must contain less than 20 parts per million of gluten, considered harmless for most celiac patients.
All uncoated, unprocessed meats, poultry, fish, beans, nuts, vegetables and fruits are naturally gluten-free, and can be labeled as such. But to be safe, consumers must read labels diligently to spot hidden hazards, like hydrolyzed vegetable protein, and learn to ask detailed questions about how food is prepared when dining out. Even reusing water in which wheat pasta is cooked can be hazardous.
KEY CLINICAL POINTS IN CELIAC DISEASE
• Once considered a gastrointestinal disorder that mainly affects white children, celiac disease is now known to affect persons of different ages, races, and ethnic groups, and it may be manifested without any gastrointestinal symptoms.
• Measurement of IgA anti–tissue transglutaminase antibodies is the preferred initial screening test for celiac disease because of its high sensitivity and specificity, but it performs poorly in patients with IgA deficiency (which is more common in patients with celiac disease than in the general population).
• The diagnosis is confirmed by means of upper endoscopy with duodenal biopsy, although recent guidelines suggest that biopsy may not be necessary in selected children with strong clinical and serologic evidence of celiac disease.
• Given the undisputable role of gluten in causing celiac disease enteropathy, the cornerstone of treatment is the implementation of a strict gluten-free diet for life.
• Gluten sensitivity may occur in the absence of celiac disease, and a definitive diagnosis should be made before implementing a lifelong gluten-free diet.
The Overlooked Diagnosis of Celiac Disease
By Carolyn Sayre : NY Times Article : December 16, 2009
It took three decades to figure out what was making Donna Sawka so sick. Her symptoms — bloating, chronic diarrhea and weight loss — began early in childhood, and they only became worse as she aged.
Nine years ago, after developing severe anemia, a specialist told Ms. Sawka that she had celiac disease. The digestive disorder causes damage to the small intestine when gluten, a protein found in wheat, barley and rye, is ingested. People with the disease need to follow a strict gluten-free diet for the rest of their lives to avoid serious complications like osteoporosis and lymphoma, an immune system cancer.
Ms. Sawka, 48, of Fairless Hills, Pa., said she “was overwhelmed” upon learning she had the disease.
“I kept thinking about everything I wouldn’t be able to eat,” she went on. “I couldn’t even receive communion at church.”
Ms. Sawka’s reaction is a familiar one at the support group she attends. It takes the average patient 10 years to receive a diagnosis. And according to specialists, they are the lucky ones. Studies show that 3 million Americans, or 1 in every 133 people, have celiac disease. But 95 percent of them have yet to learn they have it, according to the National Institutes of Health.
“The entire disease and all of its manifestations are incredibly underdiagnosed,” said Dr. Charles Bongiorno, the chief of the division of gastroenterology and hepatology at the University of Medicine and Dentistry of New Jersey. “Patients often have it for a decade or two before they are diagnosed.”
Celiac disease is often difficult to detect because the symptoms vary so widely from person to person. Ten years ago, the medical community thought it was a rare disorder that affected only 1 in every 10,000 people, primarily children who had digestive problems and failure to thrive.
But physicians now know that the disease is much more common. Most patients never experience the so-called classic symptoms: bloating, chronic diarrhea and stomach upset. Instead, the signs are often as nebulous as anemia, infertility and osteoporosis.
“It’s a problem,” said Dr. Ritu Verma, section chief of gastroenterology, hepatology and nutrition and director of the Children’s Celiac Center at the Children’s Hospital of Philadelphia. “The majority of patients do not have the traditional signs and symptoms. If someone’s only presenting symptom is anemia, physicians will think of a hundred other things before they think of celiac disease.”
As a result, the condition is also commonly mistaken for other ailments. Ms. Sawka, for one, was told she had everything from irritable bowel syndrome to lupus to an allergic reaction from a spider bite before celiac disease was confirmed.
Part of the problem is also a lack of education among physicians, particularly internists. According to Dr. Bongiorno, most primary care physicians are simply unaware of new research that shows the disease is common and can manifest itself in unusual ways.
“They think it is an exotic malady,” he explained. “That persistent fallacy causes a less-than-appropriate effort to order the right blood tests and refer to gastroenterologists for care.”
In 2006, the National Institutes of Health started a campaign to raise awareness of the disease among both the general public and physicians. A goal was to increase rates of diagnosis because, unlike many ailments, there is a definitive way to stop celiac disease from progressing once it is recognized.
“The vast majority of cases experience a complete remission from symptoms once they are diagnosed and go on a gluten-free diet,” said Dr. Stefano Guandalini, director of the University of Chicago Celiac Disease Center. “So essentially, you have no disease. That is what makes it all the more important to be diagnosed.”
And there is no better time to be on a gluten-free diet. In 2008, 832 gluten-free products entered the market, nearly 6 times the number that debuted in 2003. Last year, gluten-free even emerged as a fad diet in the general population.
“The quantity and quality of these products is amazing,” said Dr. Alessio Fasano, the medical director of the Center for Celiac Research at the University of Maryland Medical Center.
Dr. Fasano said gluten-free products used to taste like cardboard but had significantly improved in recent years. “The only problem,” he said, “is that they cost five or six times more than their normal counterparts.”
Researchers are also beginning to experiment with drugs that may be able to block the immune response to gluten, much like a lactate pill. If the clinical trials are successful, individuals with celiac disease may be someday able to ingest small amounts of gluten.
Until then, the gluten-free diet is working for patients like Ms. Sawka. “I am perfect now,” she said after 35 years of feeling sick. “Every system in my body was in an uproar, and then everything just quieted down.”
Expert Q & A
Effective Management of Celiac Disease
By Carolyn Sayre : New York Times Article : December 16, 2009
Dr. Ritu Verma is the section chief of gastroenterology, hepatology and nutrition and director of the Children’s Celiac Center at the Children’s Hospital of Philadelphia.
Q: You have two children with celiac disease. Did that inspire your work at the center?
A: No. I have been a gastroenterologist for much longer than that. I think it is one of the most fascinating diseases. I used to say to my patients, “If God ever said you have to have a disease, I would say give me celiacs.” There is an end point to it. If you change your diet, your intestines and body are as good as someone who does not have it. There is no other condition in medicine that you can cure — and you can call it a cure — just by changing your diet. There are no needles involved. If you think about it, it is probably the easiest disease to have.
Q: How do patients with celiac disease control their condition through diet?
A: They have to go on a gluten-free diet. That means a diet that does not have any wheat, barley or rye in it. You have to read labels for anything that goes in your mouth every time, because the manufacturer may switch ingredients on you. It is not just food — it is also medicine and cosmetics and, for little children, even Play-Doh and things like that. I had one patient who couldn’t figure out why her blood tests weren’t improving. Finally, she realized her shampoo had gluten in it, and she was ingesting it when she bit her nails.
Q: What can someone with celiac disease eat?
A: There is a lot that they can eat. They can eat any fruits, vegetables or meat; also corn, potatoes, beans, lentils, soymilk and eggs. Most people will eat a lot of Indian and Mediterranean food. Spanish food is also popular, because you can have the corn tortillas. Really, it is just the regular pasta, the bread and the cookies that you can’t have.
Q: Can people with celiac disease eat out at restaurants?
A: Many restaurants now have gluten-free menus. We have done a lot of education with restaurants through the National Foundation for Celiac Awareness and their Appetite for Awareness campaign.
Q: How big of a problem is cross-contamination for people trying to maintain a gluten-free diet?
A: Keeping the diet is easy as far as reading labels, but when you go out to eat you have to talk to the chef and make sure there is no cross-contamination. For example, if you went out to eat for breakfast you would probably think that eggs were safe, but some places use flour to make an omelet. You have to quiz the chef about every ingredient. It is overwhelming, especially when you are just diagnosed.
Q: The number of gluten-free products has increased significantly over the last five years. What has changed?
A: It is an increase in awareness. Five years ago, the National Institutes of Health had this whole session on celiac disease. From there, the North American Society for Pediatric Gastrointerology, Hepatology, and Nutrition started a series of lectures for physicians. Then came the legislation last year that foods would have to be labeled. Awareness has really been building.
Q: Gluten-free and wheat-free labels seem similar, but they mean very different things. Do patients often confuse the two?
A: Yes. That is where the recent labeling became a little dangerous. Foods would say “this does not contain wheat,” but it didn’t say anything about barley and rye. And then there is a whole controversy about oats. So a lot of people would say this is wheat-free, it must be gluten-free. A lot of education is needed about this. Gluten-free is wheat-free, but not the other way around.
Q: Is it important for newly diagnosed patients to work with a dietician?
A: Yes. Patients who are diagnosed and try to figure it out by themselves have a very difficult time and often give up. It is almost impossible to get the proper training yourself. It is also an extremely expensive diet. Going to the store and seeing a loaf of bread costs $8 is enough to make some people say “forget it” or go partially gluten-free, which can make themselves feel better. Dietitians and support groups are really the key to success for people with celiac disease. It is an overwhelming condition.
Q: What happens when patients stop eating gluten?
A: When you have celiac disease, there is damage to the lining of your small intestine. There is something called the villi, these finger-like projections that you look at under the microscope. In people who have celiac disease, the gluten damages the lining of the small intestine and the villi. Once you go on a gluten-free diet, these villi actually start healing and forming back again. If you do another biopsy on someone who has been on a gluten-free diet and is doing well, the small intestine and the villi will be back to normal.
Q: How strictly do patients need to follow the diet if the small intestine and villi will heal after a few months on a gluten-free diet?
A: When you start eating the gluten again, it affects your immune system. So your intestines will heal, but your immune system gets primed. It goes haywire and starts sending out these signals to the rest of your body. Your thyroid and other parts of your body can be affected, and those don’t heal. So it is not just a matter of healing your intestine; it is also a matter of healing your body and protesting this long-term risk of lymphoma that you can develop years down the line. The commitment has to be for life. So you can imagine how tough that is for patients, especially when they start feeling better. How many of us finish a course of antibiotics and when we start feeling better say, “O.K., I am done.”
Q: Physicians used to think celiac disease occurred mostly in childhood. Is any group particularly at risk?
A: A lot of people are diagnosed when they are older now. That is because they are not presenting with the traditional symptoms that young people had. It can really be in any ethnic background. It used to be someone who is Irish or French Canadian, but that is another myth taught in medical schools. It was thought that it was seen in boys more than girls, but that is still up in the air.
Q: Are there any other ways to control celiac disease?
A: Right now, it is only diet. But there are a lot of companies coming up with pills. One of them is actually almost in Phase III trials in adults, and it is thought that it will come out in the next few years. The idea is that people who take this pill would be covered if they went out and had cross contamination. The danger to this pill, of course, is people who would go out and eat regular pizza. We have to wait and see if it is safe enough for that. Right now it is only being tested to protect against the small amount of gluten that may be in someone’s diet.
Q: Are there any efforts to make a celiac vaccine?
A: There are some people who are working on a vaccine. The problem with a vaccine is that there are many different H.L.A. (human leukocyte antigens) types associated with celiac disease, so a vaccine will not be very easy. But I know the person who is looking at the vaccine is trying to develop one for the HLA-DQ2 type, because that is the more lethal one in terms of the long-term risks of cancer.
Questions for Your Doctor
What to Ask About Celiac Disease
By Carolyn Sayre : NY Times Article : December 16, 2009
Confronting a new diagnosis can be frightening — and because research changes so often, confusing. Here are some questions you may not think to ask your doctor, along with notes on why they’re important.
What is celiac disease?
Celiac disease is a digestive condition that causes an immune reaction in the small intestine when gluten, a protein found in wheat, barley and rye, is ingested. Gluten damages the tiny hairlike protrusions known as villi, which line the small intestine, and makes them unable to absorb nutrients from food like fat and protein. As a result, people with celiac disease typically become malnourished.
How common is celiac disease?
It has long been thought that celiac disease was a very rare condition that occurred only in childhood. Researchers now know that the disease is actually more common and affects both children and adults. Three million Americans, or 1 in every 133 people, have celiac disease, but only about 5 percent of them have been diagnosed, according to the National Institutes of Health.
What causes celiac disease?
Physicians are not sure why the disease occurs. But they do know that it is an inherited disorder. The incidence rises to 1 in 22 among people who have an immediate family member with celiac disease. Some researchers say the disease is activated in those who are genetically predisposed by extreme stressors like pregnancy, surgery or a viral infection. Patients with celiac disease also tend to have other autoimmune diseases, which cause the immune system to attack healthy cells and tissue, Like Type 1 diabetes, rheumatoid arthritis and Sjogren’s syndrome.
Does celiac disease always cause digestive problems?
No. Part of the reason why celiac disease is so often overlooked is because it manifests in many different ways. Classic symptoms like bloating, chronic diarrhea, stomach upset and weight loss do not always occur. Patients may instead have symptoms like anemia, bone or joint pain, fatigue, infertility, an itchy rash, osteoporosis or seizures.
Is it common for people with celiac disease to develop a rash?
Dermatitis herpetiformis, an itchy and blistering skin rash, which is commonly found on the elbows, knees or buttocks, occurs in some 15 percent to 25 percent of all patients. People with the rash usually do not have digestive symptoms.
How is celiac disease diagnosed?
Celiac disease is detected by a blood test that looks for elevated levels of autoantibodies proteins that damage the body’s healthy cells and tissues by mistake. It is important that patients continue to eat a regular diet containing gluten before the test; otherwise, the results may come back false positive. If the blood test is positive, most physicians will order an endoscopy, a procedure that lets the doctor look inside the stomach using a thin, flexible tube, to confirm the results. During the endoscopy, the physician will take samples — biopsies — of the intestinal tissue and examine the villi for damage.
Are tests for celiac disease accurate in infants and young children?
The blood test used to diagnose celiac disease is less reliable in children under age 2. If your physician suspects the condition after a negative test result, he or she will follow-up with an endoscopy.
Are there any treatments for celiac disease?
The only way to treat the disease is to follow a gluten-free diet, which eliminates foods and products containing barley, rye and wheat. Most patients’ symptoms will subside, and the damage to their small intestine will heal after just a few months on the diet. Researchers are working on drugs that may be able help people with celiac disease better tolerate gluten.
Which foods have gluten?
Gluten is a protein that is found in barley, rye and wheat. It is found in cereal, grains, pasta and most processed foods. Certain products like lip balms, medications and vitamins may also contain gluten. It is important that people with celiac disease read food and product labels carefully.
Will I ever be able to eat pasta and bread again?
People with celiac disease need to follow a gluten-free diet for the rest of their lives to avoid damaging the small intestine again. Many grocery stores carry special gluten-free bread and pasta products. In 2001, the gluten-free marketplace was a modest $210 million industry. Market researchers project it will reach $1.7 billion by the end of 2010, representing more than a sevenfold increase in just a decade.
What are the long-term complications of celiac disease?
Patients who follow a gluten-free diet rarely have problems. However, failure to adhere to a gluten-free lifestyle can cause serious consequences like anemia, infertility, lymphomas (cancers of the lymph glands) and osteoporosis.
Many people with celiac disease experience bone density loss. Are newly diagnosed patients screened routinely for osteoporosis or osteopenia?
It depends on your doctor. Some physicians will order a DEXA scan, which is a special type of X-ray that measures bone density, in adults and sometimes children, particularly those with a history of fractures. But it is not always standard practice. If you are concerned that you might have bone density loss, discuss taking the test with your physician.
Can supplements help celiac disease?
Sometimes. Patients with celiac disease may benefit from taking a multivitamin and supplements like calcium, iron and vitamin B12. The results of your blood tests and DEXA scan will help your physician determine if supplements are right for you. Supplements should never be used as a replacement for a gluten-free diet.
Should I be screened for celiac disease?
It is a personal decision. Most physicians will recommend that people who have an immediate family member with celiac disease be screened.
5 Things to Know
Hope for Patients With Celiac Disease
By Carolyn Sayre : NY Times Article : December 16, 2009
Dr. Charles Bongiorno is the chief of the division of gastroenterology and hepatology at the University of Medicine and Dentistry of New Jersey. “There is hope for patients,” Dr. Bongiorno said of the condition that can be overwhelming for the newly diagnosed. “There is not always going to be bad news.” Here are the five things he thinks everyone should know about the disease:
Celiac disease is underdiagnosed.
Researchers estimate that 1 in every 133 people have the digestive disorder. However, 95 percent of cases have not yet been diagnosed, according to the National Institutes of Health. It is difficult to detect the disease because the symptoms are so variable. Many physicians commonly misdiagnose the disease as other conditions like irritable bowel syndrome.
The classic symptoms are not very common.
It used to be thought that celiac disease always manifested itself in patients as digestive problems like bloating, chronic diarrhea, stomach pain and weight loss. But physicians now know that individuals with the disease have a host of less obvious symptoms including anemia, depression, infertility, osteoporosis and rashes.
Doctors often overlook celiac disease.
The condition is extremely underdiagnosed in patients. Many primary care physicians are unaware that the condition is so common and can manifest itself in unusual ways. If you are concerned that you may celiac disease, it is important that you talk with your physician about being tested. The earlier the disease is diagnosed, the better.
There is a treatment for celiac disease, and it has a very high success rate.
People with the disorder need to maintain a very restrictive gluten-free diet for the rest of their lives. The good news, however, is that the diet typically causes all of the symptoms of the disease to subside. It also repairs the damage that has been done to the intestines and helps avoid major complications that can develop like cancer and osteoporosis.
Those with celiac disease can have a good quality of life.
The diagnosis of celiac disease can be overwhelming for patients, because the diet is so restrictive. Yet a growing number of food manufacturers now make special gluten-free bread and pasta products. Many restaurants are also beginning to offer gluten-free menus. There are also support groups that patients can attend. Contact the National Foundation for Celiac Awareness, which includes advice and support.
Jury Is Still Out on Gluten, the Latest Dietary Villain
By Kate Murphy : NY Times Article : May 8, 2007
Brandi Walzer, a 29-year-old cartographer in Savannah, Ga., loves bread, not to mention pizza and beer. But she tries to avoid them, because they contain gluten — a substance she says upsets her stomach, aggravates her arthritis and touches off depression.
She is among a growing number of Americans who believe that gluten — a protein found in wheat, barley and rye — is responsible for a variety of ills, from skin eruptions to infertility to anxiety to gas. Though diagnostic tests have not indicated she has an allergy or sensitivity to gluten, she nonetheless says she is better off without it.
“I struggle with sticking to a gluten-free diet,” she said, “but when I do, I feel much better.”
There is no question that eating gluten aggravates celiac disease, an autoimmune disorder that damages the small intestine and interferes with absorption of nutrients. But doctors say it is unclear whether gluten can be blamed for other problems.
Nevertheless, it has become a popular dietary villain. Gluten-free foods are popping up on grocery-store shelves and restaurant menus, including those of national chains like P. F. Chang’s and Outback Steakhouse. Warnings of gluten’s evils are common on alternative medicine Web sites and message boards.
“A lot of alternative practitioners like chiropractors have picked up on it and are waving around magic silver balls, crystals and such, telling people they have gluten intolerance,” said Dr. Don W. Powell, a gastroenterologist at the University of Texas Medical Branch at Galveston.
Sloane Miller, a 35-year-old freelance editor in New York, went on a gluten-free diet six months ago on the advice of her acupuncturist, even though a blood test and a biopsy indicated that she did not have celiacdisease. Long plagued with gastrointestinal distress and believing that she might have an undetectable sensitivity to gluten, Ms. Miller said giving it up was “worth a try.”
Dr. Joseph A. Murray, a gastroenterologist at the Mayo Clinic in Rochester, Minn., who specializes in diagnosing and treating celiac disease, says such advice may be misguided. “There’s this ‘go blame gluten’ thing going on,” he said. “It’s difficult to sort out science from the belief.”
To be sure, whole wheat and other cereal grains that contain gluten can be hard to digest. The bran and germ components tend to pass through the alimentary canal intact, which is why they are often prescribed as a sort of natural broom to relieve constipation — and why they can also cause gas and diarrhea.
Processed and refined wheat products can cause a spike in blood sugar, followed by a drop, that can also make people feel ill. “If you stop eating the beloved Twinkie or fast foods because they contain wheat, then sure you’re going to feel better,” Dr. Murray said. Indeed, many people go on a gluten-free diet not to cure some ill but to lose weight by cutting down on carbohydrates.
Gluten is relatively new to the human diet, as wheat cultivation began only some 10,000 years ago. Now it is ubiquitous, not only in processed foods (including salad dressings, ice cream and peanut butter) but even in the adhesives on envelopes as well as in lipsticks and lotions. “It’s very hard to get away from gluten,” said Dr. Powell of the University of Texas.
Gluten is also making headlines now, because some Chinese suppliers are accused of slipping the industrial chemical melamine into wheat gluten that was added to American pet food, resulting in a product recall. But there is no indication that the contaminated gluten got into the human food supply.
While gluten allergies that provoke an immune response like hives or respiratory problems are rare, celiacdisease is more common than once thought. The prevalence in North America was previously estimated at about 1 in 3,000, but several studies published in the last three years indicate that it is closer to 1 in 100 — and 1 in 22 for those with risk factors like having an immediate relative with celiac disease.
Though no one knows for sure, the revised numbers can probably be attributed to increasing incidence as well as better screening tools. “Chances are now that people actually know someone who has it,” said Dr. Peter H. R. Green, director of the Celiac Disease Center at Columbia University College of Physicians and Surgeons.
With increased awareness, he said, more people have begun to suspect that they have celiac disease or some milder form of gluten intolerance and decide to eliminate wheat, barley and rye from their diet without proper diagnosis. Ms. Walzer, for example, gave up gluten a year and half ago upon learning she had symptoms similar to those of a co-worker with celiac disease.
Though no test for celiac disease is definitive, the most powerful indicator is a blood test widely used for three years that measures levels of antitissue transglutaminase, or anti-tTG, the antibodies to an enzyme the body secretes when gluten irritates or damages the small intestine.
People with celiac disease have high levels of anti-tTG, suggesting that the body is attacking its own secretions. This autoimmune response leads to destruction of the lining of the small intestine and consequent malabsorption of nutrients. (The test will not be accurate if someone has already stopped eating gluten.) The blood test is usually followed by a duodenal biopsy before a diagnosis of celiac disease is made. The final proof is reversal of symptoms on a gluten-free diet.
Earlier blood tests and a DNA test were far less predictive, and celiac disease has been difficult to identify, especially because its symptoms vary widely. Ann Austin McCormick, a 64-year-old retired elementary school principal in Crosslake, Minn., said she had chronic diarrhea and anemia before she got a diagnosis of celiac disease five years ago. Colin Leslie, a 15-year-old high school student in Rye, N.Y., said he suffered from severe joint pain and headaches before receiving a diagnosis in 2005.
Still others have no symptoms at all — merely a latent form of the disease that may become apparent only after a stressful physiological or psychological event like a serious illness or death of a spouse.
Researchers in the United States, Italy and Great Britain have hypothesized that the incidence of celiacdisease is on the rise worldwide because wheat has become so prevalent in the Western diet that humans are actually overdosing on it. While debatable, this view could also account for cases like those of Ms. Walzer and Ms. Miller, who believe they have subclinical gluten sensitivity.
Currently, the only treatment for celiac disease or a more subjective gluten sensitivity is to avoid eating anything containing gluten. Sensing an opportunity, several companies, including Alba Therapeutics and Alvine Pharmaceuticals Inc., are working to find drugs to inhibit the destructive autoimmune response to gluten that is characteristic of celiac disease.
And dietary supplement makers are in a race to develop enzyme formulations that will help people digest gluten, just as lactase pills and drops were developed in the 1980s to help people digest lactose in dairy products.
But with supermarkets brimming with gluten-free breads, cereals, cakes and cookies and restaurants serving gluten-free pastas, pizzas and beer, it has become far less difficult to stay on a gluten-free diet.
“It’s easy to go gluten-free,” Ms. Miller said. “I don’t miss it at all.”
By Carolyn Sayre : NY Times Article : December 16, 2009
It took three decades to figure out what was making Donna Sawka so sick. Her symptoms — bloating, chronic diarrhea and weight loss — began early in childhood, and they only became worse as she aged.
Nine years ago, after developing severe anemia, a specialist told Ms. Sawka that she had celiac disease. The digestive disorder causes damage to the small intestine when gluten, a protein found in wheat, barley and rye, is ingested. People with the disease need to follow a strict gluten-free diet for the rest of their lives to avoid serious complications like osteoporosis and lymphoma, an immune system cancer.
Ms. Sawka, 48, of Fairless Hills, Pa., said she “was overwhelmed” upon learning she had the disease.
“I kept thinking about everything I wouldn’t be able to eat,” she went on. “I couldn’t even receive communion at church.”
Ms. Sawka’s reaction is a familiar one at the support group she attends. It takes the average patient 10 years to receive a diagnosis. And according to specialists, they are the lucky ones. Studies show that 3 million Americans, or 1 in every 133 people, have celiac disease. But 95 percent of them have yet to learn they have it, according to the National Institutes of Health.
“The entire disease and all of its manifestations are incredibly underdiagnosed,” said Dr. Charles Bongiorno, the chief of the division of gastroenterology and hepatology at the University of Medicine and Dentistry of New Jersey. “Patients often have it for a decade or two before they are diagnosed.”
Celiac disease is often difficult to detect because the symptoms vary so widely from person to person. Ten years ago, the medical community thought it was a rare disorder that affected only 1 in every 10,000 people, primarily children who had digestive problems and failure to thrive.
But physicians now know that the disease is much more common. Most patients never experience the so-called classic symptoms: bloating, chronic diarrhea and stomach upset. Instead, the signs are often as nebulous as anemia, infertility and osteoporosis.
“It’s a problem,” said Dr. Ritu Verma, section chief of gastroenterology, hepatology and nutrition and director of the Children’s Celiac Center at the Children’s Hospital of Philadelphia. “The majority of patients do not have the traditional signs and symptoms. If someone’s only presenting symptom is anemia, physicians will think of a hundred other things before they think of celiac disease.”
As a result, the condition is also commonly mistaken for other ailments. Ms. Sawka, for one, was told she had everything from irritable bowel syndrome to lupus to an allergic reaction from a spider bite before celiac disease was confirmed.
Part of the problem is also a lack of education among physicians, particularly internists. According to Dr. Bongiorno, most primary care physicians are simply unaware of new research that shows the disease is common and can manifest itself in unusual ways.
“They think it is an exotic malady,” he explained. “That persistent fallacy causes a less-than-appropriate effort to order the right blood tests and refer to gastroenterologists for care.”
In 2006, the National Institutes of Health started a campaign to raise awareness of the disease among both the general public and physicians. A goal was to increase rates of diagnosis because, unlike many ailments, there is a definitive way to stop celiac disease from progressing once it is recognized.
“The vast majority of cases experience a complete remission from symptoms once they are diagnosed and go on a gluten-free diet,” said Dr. Stefano Guandalini, director of the University of Chicago Celiac Disease Center. “So essentially, you have no disease. That is what makes it all the more important to be diagnosed.”
And there is no better time to be on a gluten-free diet. In 2008, 832 gluten-free products entered the market, nearly 6 times the number that debuted in 2003. Last year, gluten-free even emerged as a fad diet in the general population.
“The quantity and quality of these products is amazing,” said Dr. Alessio Fasano, the medical director of the Center for Celiac Research at the University of Maryland Medical Center.
Dr. Fasano said gluten-free products used to taste like cardboard but had significantly improved in recent years. “The only problem,” he said, “is that they cost five or six times more than their normal counterparts.”
Researchers are also beginning to experiment with drugs that may be able to block the immune response to gluten, much like a lactate pill. If the clinical trials are successful, individuals with celiac disease may be someday able to ingest small amounts of gluten.
Until then, the gluten-free diet is working for patients like Ms. Sawka. “I am perfect now,” she said after 35 years of feeling sick. “Every system in my body was in an uproar, and then everything just quieted down.”
Expert Q & A
Effective Management of Celiac Disease
By Carolyn Sayre : New York Times Article : December 16, 2009
Dr. Ritu Verma is the section chief of gastroenterology, hepatology and nutrition and director of the Children’s Celiac Center at the Children’s Hospital of Philadelphia.
Q: You have two children with celiac disease. Did that inspire your work at the center?
A: No. I have been a gastroenterologist for much longer than that. I think it is one of the most fascinating diseases. I used to say to my patients, “If God ever said you have to have a disease, I would say give me celiacs.” There is an end point to it. If you change your diet, your intestines and body are as good as someone who does not have it. There is no other condition in medicine that you can cure — and you can call it a cure — just by changing your diet. There are no needles involved. If you think about it, it is probably the easiest disease to have.
Q: How do patients with celiac disease control their condition through diet?
A: They have to go on a gluten-free diet. That means a diet that does not have any wheat, barley or rye in it. You have to read labels for anything that goes in your mouth every time, because the manufacturer may switch ingredients on you. It is not just food — it is also medicine and cosmetics and, for little children, even Play-Doh and things like that. I had one patient who couldn’t figure out why her blood tests weren’t improving. Finally, she realized her shampoo had gluten in it, and she was ingesting it when she bit her nails.
Q: What can someone with celiac disease eat?
A: There is a lot that they can eat. They can eat any fruits, vegetables or meat; also corn, potatoes, beans, lentils, soymilk and eggs. Most people will eat a lot of Indian and Mediterranean food. Spanish food is also popular, because you can have the corn tortillas. Really, it is just the regular pasta, the bread and the cookies that you can’t have.
Q: Can people with celiac disease eat out at restaurants?
A: Many restaurants now have gluten-free menus. We have done a lot of education with restaurants through the National Foundation for Celiac Awareness and their Appetite for Awareness campaign.
Q: How big of a problem is cross-contamination for people trying to maintain a gluten-free diet?
A: Keeping the diet is easy as far as reading labels, but when you go out to eat you have to talk to the chef and make sure there is no cross-contamination. For example, if you went out to eat for breakfast you would probably think that eggs were safe, but some places use flour to make an omelet. You have to quiz the chef about every ingredient. It is overwhelming, especially when you are just diagnosed.
Q: The number of gluten-free products has increased significantly over the last five years. What has changed?
A: It is an increase in awareness. Five years ago, the National Institutes of Health had this whole session on celiac disease. From there, the North American Society for Pediatric Gastrointerology, Hepatology, and Nutrition started a series of lectures for physicians. Then came the legislation last year that foods would have to be labeled. Awareness has really been building.
Q: Gluten-free and wheat-free labels seem similar, but they mean very different things. Do patients often confuse the two?
A: Yes. That is where the recent labeling became a little dangerous. Foods would say “this does not contain wheat,” but it didn’t say anything about barley and rye. And then there is a whole controversy about oats. So a lot of people would say this is wheat-free, it must be gluten-free. A lot of education is needed about this. Gluten-free is wheat-free, but not the other way around.
Q: Is it important for newly diagnosed patients to work with a dietician?
A: Yes. Patients who are diagnosed and try to figure it out by themselves have a very difficult time and often give up. It is almost impossible to get the proper training yourself. It is also an extremely expensive diet. Going to the store and seeing a loaf of bread costs $8 is enough to make some people say “forget it” or go partially gluten-free, which can make themselves feel better. Dietitians and support groups are really the key to success for people with celiac disease. It is an overwhelming condition.
Q: What happens when patients stop eating gluten?
A: When you have celiac disease, there is damage to the lining of your small intestine. There is something called the villi, these finger-like projections that you look at under the microscope. In people who have celiac disease, the gluten damages the lining of the small intestine and the villi. Once you go on a gluten-free diet, these villi actually start healing and forming back again. If you do another biopsy on someone who has been on a gluten-free diet and is doing well, the small intestine and the villi will be back to normal.
Q: How strictly do patients need to follow the diet if the small intestine and villi will heal after a few months on a gluten-free diet?
A: When you start eating the gluten again, it affects your immune system. So your intestines will heal, but your immune system gets primed. It goes haywire and starts sending out these signals to the rest of your body. Your thyroid and other parts of your body can be affected, and those don’t heal. So it is not just a matter of healing your intestine; it is also a matter of healing your body and protesting this long-term risk of lymphoma that you can develop years down the line. The commitment has to be for life. So you can imagine how tough that is for patients, especially when they start feeling better. How many of us finish a course of antibiotics and when we start feeling better say, “O.K., I am done.”
Q: Physicians used to think celiac disease occurred mostly in childhood. Is any group particularly at risk?
A: A lot of people are diagnosed when they are older now. That is because they are not presenting with the traditional symptoms that young people had. It can really be in any ethnic background. It used to be someone who is Irish or French Canadian, but that is another myth taught in medical schools. It was thought that it was seen in boys more than girls, but that is still up in the air.
Q: Are there any other ways to control celiac disease?
A: Right now, it is only diet. But there are a lot of companies coming up with pills. One of them is actually almost in Phase III trials in adults, and it is thought that it will come out in the next few years. The idea is that people who take this pill would be covered if they went out and had cross contamination. The danger to this pill, of course, is people who would go out and eat regular pizza. We have to wait and see if it is safe enough for that. Right now it is only being tested to protect against the small amount of gluten that may be in someone’s diet.
Q: Are there any efforts to make a celiac vaccine?
A: There are some people who are working on a vaccine. The problem with a vaccine is that there are many different H.L.A. (human leukocyte antigens) types associated with celiac disease, so a vaccine will not be very easy. But I know the person who is looking at the vaccine is trying to develop one for the HLA-DQ2 type, because that is the more lethal one in terms of the long-term risks of cancer.
Questions for Your Doctor
What to Ask About Celiac Disease
By Carolyn Sayre : NY Times Article : December 16, 2009
Confronting a new diagnosis can be frightening — and because research changes so often, confusing. Here are some questions you may not think to ask your doctor, along with notes on why they’re important.
What is celiac disease?
Celiac disease is a digestive condition that causes an immune reaction in the small intestine when gluten, a protein found in wheat, barley and rye, is ingested. Gluten damages the tiny hairlike protrusions known as villi, which line the small intestine, and makes them unable to absorb nutrients from food like fat and protein. As a result, people with celiac disease typically become malnourished.
How common is celiac disease?
It has long been thought that celiac disease was a very rare condition that occurred only in childhood. Researchers now know that the disease is actually more common and affects both children and adults. Three million Americans, or 1 in every 133 people, have celiac disease, but only about 5 percent of them have been diagnosed, according to the National Institutes of Health.
What causes celiac disease?
Physicians are not sure why the disease occurs. But they do know that it is an inherited disorder. The incidence rises to 1 in 22 among people who have an immediate family member with celiac disease. Some researchers say the disease is activated in those who are genetically predisposed by extreme stressors like pregnancy, surgery or a viral infection. Patients with celiac disease also tend to have other autoimmune diseases, which cause the immune system to attack healthy cells and tissue, Like Type 1 diabetes, rheumatoid arthritis and Sjogren’s syndrome.
Does celiac disease always cause digestive problems?
No. Part of the reason why celiac disease is so often overlooked is because it manifests in many different ways. Classic symptoms like bloating, chronic diarrhea, stomach upset and weight loss do not always occur. Patients may instead have symptoms like anemia, bone or joint pain, fatigue, infertility, an itchy rash, osteoporosis or seizures.
Is it common for people with celiac disease to develop a rash?
Dermatitis herpetiformis, an itchy and blistering skin rash, which is commonly found on the elbows, knees or buttocks, occurs in some 15 percent to 25 percent of all patients. People with the rash usually do not have digestive symptoms.
How is celiac disease diagnosed?
Celiac disease is detected by a blood test that looks for elevated levels of autoantibodies proteins that damage the body’s healthy cells and tissues by mistake. It is important that patients continue to eat a regular diet containing gluten before the test; otherwise, the results may come back false positive. If the blood test is positive, most physicians will order an endoscopy, a procedure that lets the doctor look inside the stomach using a thin, flexible tube, to confirm the results. During the endoscopy, the physician will take samples — biopsies — of the intestinal tissue and examine the villi for damage.
Are tests for celiac disease accurate in infants and young children?
The blood test used to diagnose celiac disease is less reliable in children under age 2. If your physician suspects the condition after a negative test result, he or she will follow-up with an endoscopy.
Are there any treatments for celiac disease?
The only way to treat the disease is to follow a gluten-free diet, which eliminates foods and products containing barley, rye and wheat. Most patients’ symptoms will subside, and the damage to their small intestine will heal after just a few months on the diet. Researchers are working on drugs that may be able help people with celiac disease better tolerate gluten.
Which foods have gluten?
Gluten is a protein that is found in barley, rye and wheat. It is found in cereal, grains, pasta and most processed foods. Certain products like lip balms, medications and vitamins may also contain gluten. It is important that people with celiac disease read food and product labels carefully.
Will I ever be able to eat pasta and bread again?
People with celiac disease need to follow a gluten-free diet for the rest of their lives to avoid damaging the small intestine again. Many grocery stores carry special gluten-free bread and pasta products. In 2001, the gluten-free marketplace was a modest $210 million industry. Market researchers project it will reach $1.7 billion by the end of 2010, representing more than a sevenfold increase in just a decade.
What are the long-term complications of celiac disease?
Patients who follow a gluten-free diet rarely have problems. However, failure to adhere to a gluten-free lifestyle can cause serious consequences like anemia, infertility, lymphomas (cancers of the lymph glands) and osteoporosis.
Many people with celiac disease experience bone density loss. Are newly diagnosed patients screened routinely for osteoporosis or osteopenia?
It depends on your doctor. Some physicians will order a DEXA scan, which is a special type of X-ray that measures bone density, in adults and sometimes children, particularly those with a history of fractures. But it is not always standard practice. If you are concerned that you might have bone density loss, discuss taking the test with your physician.
Can supplements help celiac disease?
Sometimes. Patients with celiac disease may benefit from taking a multivitamin and supplements like calcium, iron and vitamin B12. The results of your blood tests and DEXA scan will help your physician determine if supplements are right for you. Supplements should never be used as a replacement for a gluten-free diet.
Should I be screened for celiac disease?
It is a personal decision. Most physicians will recommend that people who have an immediate family member with celiac disease be screened.
5 Things to Know
Hope for Patients With Celiac Disease
By Carolyn Sayre : NY Times Article : December 16, 2009
Dr. Charles Bongiorno is the chief of the division of gastroenterology and hepatology at the University of Medicine and Dentistry of New Jersey. “There is hope for patients,” Dr. Bongiorno said of the condition that can be overwhelming for the newly diagnosed. “There is not always going to be bad news.” Here are the five things he thinks everyone should know about the disease:
Celiac disease is underdiagnosed.
Researchers estimate that 1 in every 133 people have the digestive disorder. However, 95 percent of cases have not yet been diagnosed, according to the National Institutes of Health. It is difficult to detect the disease because the symptoms are so variable. Many physicians commonly misdiagnose the disease as other conditions like irritable bowel syndrome.
The classic symptoms are not very common.
It used to be thought that celiac disease always manifested itself in patients as digestive problems like bloating, chronic diarrhea, stomach pain and weight loss. But physicians now know that individuals with the disease have a host of less obvious symptoms including anemia, depression, infertility, osteoporosis and rashes.
Doctors often overlook celiac disease.
The condition is extremely underdiagnosed in patients. Many primary care physicians are unaware that the condition is so common and can manifest itself in unusual ways. If you are concerned that you may celiac disease, it is important that you talk with your physician about being tested. The earlier the disease is diagnosed, the better.
There is a treatment for celiac disease, and it has a very high success rate.
People with the disorder need to maintain a very restrictive gluten-free diet for the rest of their lives. The good news, however, is that the diet typically causes all of the symptoms of the disease to subside. It also repairs the damage that has been done to the intestines and helps avoid major complications that can develop like cancer and osteoporosis.
Those with celiac disease can have a good quality of life.
The diagnosis of celiac disease can be overwhelming for patients, because the diet is so restrictive. Yet a growing number of food manufacturers now make special gluten-free bread and pasta products. Many restaurants are also beginning to offer gluten-free menus. There are also support groups that patients can attend. Contact the National Foundation for Celiac Awareness, which includes advice and support.
Jury Is Still Out on Gluten, the Latest Dietary Villain
By Kate Murphy : NY Times Article : May 8, 2007
Brandi Walzer, a 29-year-old cartographer in Savannah, Ga., loves bread, not to mention pizza and beer. But she tries to avoid them, because they contain gluten — a substance she says upsets her stomach, aggravates her arthritis and touches off depression.
She is among a growing number of Americans who believe that gluten — a protein found in wheat, barley and rye — is responsible for a variety of ills, from skin eruptions to infertility to anxiety to gas. Though diagnostic tests have not indicated she has an allergy or sensitivity to gluten, she nonetheless says she is better off without it.
“I struggle with sticking to a gluten-free diet,” she said, “but when I do, I feel much better.”
There is no question that eating gluten aggravates celiac disease, an autoimmune disorder that damages the small intestine and interferes with absorption of nutrients. But doctors say it is unclear whether gluten can be blamed for other problems.
Nevertheless, it has become a popular dietary villain. Gluten-free foods are popping up on grocery-store shelves and restaurant menus, including those of national chains like P. F. Chang’s and Outback Steakhouse. Warnings of gluten’s evils are common on alternative medicine Web sites and message boards.
“A lot of alternative practitioners like chiropractors have picked up on it and are waving around magic silver balls, crystals and such, telling people they have gluten intolerance,” said Dr. Don W. Powell, a gastroenterologist at the University of Texas Medical Branch at Galveston.
Sloane Miller, a 35-year-old freelance editor in New York, went on a gluten-free diet six months ago on the advice of her acupuncturist, even though a blood test and a biopsy indicated that she did not have celiacdisease. Long plagued with gastrointestinal distress and believing that she might have an undetectable sensitivity to gluten, Ms. Miller said giving it up was “worth a try.”
Dr. Joseph A. Murray, a gastroenterologist at the Mayo Clinic in Rochester, Minn., who specializes in diagnosing and treating celiac disease, says such advice may be misguided. “There’s this ‘go blame gluten’ thing going on,” he said. “It’s difficult to sort out science from the belief.”
To be sure, whole wheat and other cereal grains that contain gluten can be hard to digest. The bran and germ components tend to pass through the alimentary canal intact, which is why they are often prescribed as a sort of natural broom to relieve constipation — and why they can also cause gas and diarrhea.
Processed and refined wheat products can cause a spike in blood sugar, followed by a drop, that can also make people feel ill. “If you stop eating the beloved Twinkie or fast foods because they contain wheat, then sure you’re going to feel better,” Dr. Murray said. Indeed, many people go on a gluten-free diet not to cure some ill but to lose weight by cutting down on carbohydrates.
Gluten is relatively new to the human diet, as wheat cultivation began only some 10,000 years ago. Now it is ubiquitous, not only in processed foods (including salad dressings, ice cream and peanut butter) but even in the adhesives on envelopes as well as in lipsticks and lotions. “It’s very hard to get away from gluten,” said Dr. Powell of the University of Texas.
Gluten is also making headlines now, because some Chinese suppliers are accused of slipping the industrial chemical melamine into wheat gluten that was added to American pet food, resulting in a product recall. But there is no indication that the contaminated gluten got into the human food supply.
While gluten allergies that provoke an immune response like hives or respiratory problems are rare, celiacdisease is more common than once thought. The prevalence in North America was previously estimated at about 1 in 3,000, but several studies published in the last three years indicate that it is closer to 1 in 100 — and 1 in 22 for those with risk factors like having an immediate relative with celiac disease.
Though no one knows for sure, the revised numbers can probably be attributed to increasing incidence as well as better screening tools. “Chances are now that people actually know someone who has it,” said Dr. Peter H. R. Green, director of the Celiac Disease Center at Columbia University College of Physicians and Surgeons.
With increased awareness, he said, more people have begun to suspect that they have celiac disease or some milder form of gluten intolerance and decide to eliminate wheat, barley and rye from their diet without proper diagnosis. Ms. Walzer, for example, gave up gluten a year and half ago upon learning she had symptoms similar to those of a co-worker with celiac disease.
Though no test for celiac disease is definitive, the most powerful indicator is a blood test widely used for three years that measures levels of antitissue transglutaminase, or anti-tTG, the antibodies to an enzyme the body secretes when gluten irritates or damages the small intestine.
People with celiac disease have high levels of anti-tTG, suggesting that the body is attacking its own secretions. This autoimmune response leads to destruction of the lining of the small intestine and consequent malabsorption of nutrients. (The test will not be accurate if someone has already stopped eating gluten.) The blood test is usually followed by a duodenal biopsy before a diagnosis of celiac disease is made. The final proof is reversal of symptoms on a gluten-free diet.
Earlier blood tests and a DNA test were far less predictive, and celiac disease has been difficult to identify, especially because its symptoms vary widely. Ann Austin McCormick, a 64-year-old retired elementary school principal in Crosslake, Minn., said she had chronic diarrhea and anemia before she got a diagnosis of celiac disease five years ago. Colin Leslie, a 15-year-old high school student in Rye, N.Y., said he suffered from severe joint pain and headaches before receiving a diagnosis in 2005.
Still others have no symptoms at all — merely a latent form of the disease that may become apparent only after a stressful physiological or psychological event like a serious illness or death of a spouse.
Researchers in the United States, Italy and Great Britain have hypothesized that the incidence of celiacdisease is on the rise worldwide because wheat has become so prevalent in the Western diet that humans are actually overdosing on it. While debatable, this view could also account for cases like those of Ms. Walzer and Ms. Miller, who believe they have subclinical gluten sensitivity.
Currently, the only treatment for celiac disease or a more subjective gluten sensitivity is to avoid eating anything containing gluten. Sensing an opportunity, several companies, including Alba Therapeutics and Alvine Pharmaceuticals Inc., are working to find drugs to inhibit the destructive autoimmune response to gluten that is characteristic of celiac disease.
And dietary supplement makers are in a race to develop enzyme formulations that will help people digest gluten, just as lactase pills and drops were developed in the 1980s to help people digest lactose in dairy products.
But with supermarkets brimming with gluten-free breads, cereals, cakes and cookies and restaurants serving gluten-free pastas, pizzas and beer, it has become far less difficult to stay on a gluten-free diet.
“It’s easy to go gluten-free,” Ms. Miller said. “I don’t miss it at all.”
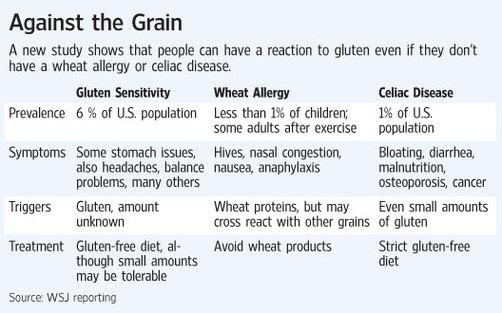
Clues to Gluten Sensitivity
By Melinda Beck : WSJ : March 14, 2011
Lisa Rayburn felt dizzy, bloated and exhausted. Wynn Avocette suffered migraines and body aches. Stephanie Meade's 4-year-old daughter had constipation and threw temper tantrums.
Some people claim that eating gluten products can cause health problems like body aches and chronic fatigue -- and even some behavioral problems in children. WSJ's Melinda Beck talks with Kelsey Hubbard about a new study that sheds light on what may be going on.
All three tested negative for celiac disease, a severe intolerance to gluten, a protein found in wheat and other grains. But after their doctors ruled out other causes, all three adults did their own research and cut gluten—and saw the symptoms subside.
A new study in the journal BMC Medicine may shed some light on why. It shows gluten can set off a distinct reaction in the intestines and the immune system, even in people who don't have celiac disease.
"For the first time, we have scientific evidence that indeed, gluten sensitivity not only exists, but is very different from celiac disease," says lead author Alessio Fasano, medical director of the University of Maryland's Center for Celiac Research.
The news will be welcome to people who have suspected a broad range of ailments may be linked to their gluten intake, but have failed to find doctors who agree.
"Patients have been told if it wasn't celiac disease, it wasn't anything. It was all in their heads," says Cynthia Kupper, executive director of the nonprofit Gluten Intolerance Group of North America.
The growing market for gluten-free foods, with sales estimated at $2.6 billion last year, has made it even harder to distinguish a medical insight from a fad.
Although much remains unknown, it is clear that gluten—a staple of human diets for 10,000 years—triggers an immune response like an enemy invader in some modern humans.
The most basic negative response is an allergic reaction to wheat that quickly brings on hives, congestion, nausea or potentially fatal anaphylaxis. Less than 1% of children have the allergy and most outgrow it by age five. A small number of adults have similar symptoms if they exercise shortly after eating wheat.
At the other extreme is celiac disease, which causes the immune system to mistakenly attack the body's own tissue. Antibodies triggered by gluten flatten the villi, the tiny fingers in the intestines needed to soak up nutrients from food. The initial symptoms are cramping, bloating and diarrhea, similar to irritable bowel syndrome, or IBS, but celiac disease can lead to malnutrition, osteoporosis and other more serious health problems that can result in early death. It can be diagnosed with a blood test, but an intestinal biopsy is needed to be sure.
The incidence of celiac disease is rising sharply—and not just due to greater awareness. Tests comparing old blood samples to recent ones show the rate has increased four-fold in the last 50 years, to at least 1 in 133 Americans. It's also being diagnosed in people as old as 70 who have eaten gluten safely all their lives.
"People aren't born with this. Something triggers it and with this dramatic rise in all ages, it must be something pervasive in the environment," says Joseph A. Murray, a gastroenterologist at the Mayo Clinic in Rochester, Minn. One possible culprit: agricultural changes to wheat that have boosted its protein content.
Gluten sensitivity, also known as gluten intolerance, is much more vague.
Some experts think as many as 1 in 20 Americans may have some form of it, but there is no test or defined set of symptoms. The most common are IBS-like stomach problems, headaches, fatigue, numbness and depression, but more than 100 symptoms have been loosely linked to gluten intake, which is why it has been so difficult to study. Peter Green, director of the Celiac Disease Center says that research into gluten sensitivity today is roughly where celiac disease was 30 years ago.
In the new study, researchers compared blood samples and intestinal biopsies from 42 subjects with confirmed celiac disease, 26 with suspected gluten sensitivity and 39 healthy controls. Those with gluten sensitivity didn't have the flattened villi, or the "leaky" intestinal walls seen in the subjects with celiac disease.
Their immune reactions were different, too. In the gluten-sensitive group, the response came from innate immunity, a primitive system with which the body sets up barriers to repel invaders. The subjects with celiac disease rallied adaptive immunity, a more sophisticated system that develops specific cells to fight foreign bodies.
The findings still need to be replicated. How a reaction to gluten could cause such a wide range of symptoms also remains unproven. Dr. Fasano and other experts speculate that once immune cells are mistakenly primed to attack gluten, they can migrate and spread inflammation, even to the brain.
Indeed, Marios Hadjivassiliou, a neurologist in Sheffield, England, says he found deposits of antibodies to gluten in autopsies and brain scans of some patients with ataxia, a condition of impaired balance.
Could such findings help explain why some parents of autistic children say their symptoms have improved—sometimes dramatically—when gluten was eliminated from their diets? To date, no scientific studies have emerged to back up such reports.
Dr. Fasano hopes to eventually discover a biomarker specifically for gluten sensitivity. In the meantime, he and other experts recommend that anyone who thinks they have it be tested for celiac disease first.
For now, a gluten-free diet is the only treatment recommended for gluten sensitivity, though some may be able to tolerate small amounts, says Ms. Kupper.
"There's a lot more that needs to be done for people with gluten sensitivity," she says. "But at least we now recognize that it's real and that these people aren't crazy."
By Melinda Beck : WSJ : March 14, 2011
Lisa Rayburn felt dizzy, bloated and exhausted. Wynn Avocette suffered migraines and body aches. Stephanie Meade's 4-year-old daughter had constipation and threw temper tantrums.
Some people claim that eating gluten products can cause health problems like body aches and chronic fatigue -- and even some behavioral problems in children. WSJ's Melinda Beck talks with Kelsey Hubbard about a new study that sheds light on what may be going on.
All three tested negative for celiac disease, a severe intolerance to gluten, a protein found in wheat and other grains. But after their doctors ruled out other causes, all three adults did their own research and cut gluten—and saw the symptoms subside.
A new study in the journal BMC Medicine may shed some light on why. It shows gluten can set off a distinct reaction in the intestines and the immune system, even in people who don't have celiac disease.
"For the first time, we have scientific evidence that indeed, gluten sensitivity not only exists, but is very different from celiac disease," says lead author Alessio Fasano, medical director of the University of Maryland's Center for Celiac Research.
The news will be welcome to people who have suspected a broad range of ailments may be linked to their gluten intake, but have failed to find doctors who agree.
"Patients have been told if it wasn't celiac disease, it wasn't anything. It was all in their heads," says Cynthia Kupper, executive director of the nonprofit Gluten Intolerance Group of North America.
The growing market for gluten-free foods, with sales estimated at $2.6 billion last year, has made it even harder to distinguish a medical insight from a fad.
Although much remains unknown, it is clear that gluten—a staple of human diets for 10,000 years—triggers an immune response like an enemy invader in some modern humans.
The most basic negative response is an allergic reaction to wheat that quickly brings on hives, congestion, nausea or potentially fatal anaphylaxis. Less than 1% of children have the allergy and most outgrow it by age five. A small number of adults have similar symptoms if they exercise shortly after eating wheat.
At the other extreme is celiac disease, which causes the immune system to mistakenly attack the body's own tissue. Antibodies triggered by gluten flatten the villi, the tiny fingers in the intestines needed to soak up nutrients from food. The initial symptoms are cramping, bloating and diarrhea, similar to irritable bowel syndrome, or IBS, but celiac disease can lead to malnutrition, osteoporosis and other more serious health problems that can result in early death. It can be diagnosed with a blood test, but an intestinal biopsy is needed to be sure.
The incidence of celiac disease is rising sharply—and not just due to greater awareness. Tests comparing old blood samples to recent ones show the rate has increased four-fold in the last 50 years, to at least 1 in 133 Americans. It's also being diagnosed in people as old as 70 who have eaten gluten safely all their lives.
"People aren't born with this. Something triggers it and with this dramatic rise in all ages, it must be something pervasive in the environment," says Joseph A. Murray, a gastroenterologist at the Mayo Clinic in Rochester, Minn. One possible culprit: agricultural changes to wheat that have boosted its protein content.
Gluten sensitivity, also known as gluten intolerance, is much more vague.
Some experts think as many as 1 in 20 Americans may have some form of it, but there is no test or defined set of symptoms. The most common are IBS-like stomach problems, headaches, fatigue, numbness and depression, but more than 100 symptoms have been loosely linked to gluten intake, which is why it has been so difficult to study. Peter Green, director of the Celiac Disease Center says that research into gluten sensitivity today is roughly where celiac disease was 30 years ago.
In the new study, researchers compared blood samples and intestinal biopsies from 42 subjects with confirmed celiac disease, 26 with suspected gluten sensitivity and 39 healthy controls. Those with gluten sensitivity didn't have the flattened villi, or the "leaky" intestinal walls seen in the subjects with celiac disease.
Their immune reactions were different, too. In the gluten-sensitive group, the response came from innate immunity, a primitive system with which the body sets up barriers to repel invaders. The subjects with celiac disease rallied adaptive immunity, a more sophisticated system that develops specific cells to fight foreign bodies.
The findings still need to be replicated. How a reaction to gluten could cause such a wide range of symptoms also remains unproven. Dr. Fasano and other experts speculate that once immune cells are mistakenly primed to attack gluten, they can migrate and spread inflammation, even to the brain.
Indeed, Marios Hadjivassiliou, a neurologist in Sheffield, England, says he found deposits of antibodies to gluten in autopsies and brain scans of some patients with ataxia, a condition of impaired balance.
Could such findings help explain why some parents of autistic children say their symptoms have improved—sometimes dramatically—when gluten was eliminated from their diets? To date, no scientific studies have emerged to back up such reports.
Dr. Fasano hopes to eventually discover a biomarker specifically for gluten sensitivity. In the meantime, he and other experts recommend that anyone who thinks they have it be tested for celiac disease first.
For now, a gluten-free diet is the only treatment recommended for gluten sensitivity, though some may be able to tolerate small amounts, says Ms. Kupper.
"There's a lot more that needs to be done for people with gluten sensitivity," she says. "But at least we now recognize that it's real and that these people aren't crazy."
Classifying the Symptoms
Gluten-related disorders are rising around the world. One group of international experts has proposed classifying them based on the kind of defenses the body mounts.
Wheat allergy
Can affect skin, gastrointestinal tract or respiratory tract
Symptoms: Hives, nasal and chest congestion, nausea, vomiting, anaphylaxis
Prevalence: Less than 1% of children, most outgrow it
Diagnosis: Blood and skin prick reveal IgE antibodies; food challenge
Treatment: Avoid wheat products
Celiac disease
Antibodies to gluten damage intestinal villi needed to absorb food
Symptoms: Abdominal pain, bloating, diarrhea, fatigue, osteoporosis, cancer; can also be asymptomatic
Prevalence: 1% of adults of European descent, up fourfold in 50 years
Diagnosis: Gene tests show HLA-DQ2 or HLA-DQ8 variations; blood tests reveal tTGA or EMA antibodies; biopsy shows villi damage
Treatment: Strict gluten-free diet can reverse symptoms
Gluten ataxia
Antibodies to gluten attack cerebellum
Symptoms: Loss of balance and coordination; few GI symptoms
Prevalence: Gluten may be the cause of ataxia in a fifth of all sufferers of the ailment
Diagnosis: Blood tests show tTG6 and AGA antibodies; brain images are abnormal
Treatment: Gluten-free diet may stabilize ataxia but some damage may be irreversible
Gluten Sensitivity
Gluten may trigger a primitive immune defense
Symptoms: similar to celiac disease without villi damage; foggy thinking, mood swings
Prevalence: Unknown
Diagnosis: Rule out celiac disease and wheat allergies; possible AGA antibodies in blood; symptoms ease when avoiding gluten
Treatment: Avoiding gluten, though small amounts on occasion may not cause problems
New Guide to Who Really Shouldn't Eat Gluten
Melinda Beck : WSJ : February 8, 2012
You've got abdominal pains, bloating, fatigue and foggy thinking. You feel worse after eating wheat or other foods with gluten, and better when you avoid them.
Other autoimmune forms include dermatitis herpetiformis, which causes itchy skin lesions, and gluten ataxia, which affects brain tissue, resulting in unsteady gait and lack of motor control.
The experts also propose a third category for "gluten sensitivity," in which patients report the same symptoms as celiac disease but test negative for telltale antibodies. Some doctors have dismissed such complaints as imaginary, or fueled by the boom in gluten-free foods.
U.S. sales of gluten-free foods grew to $2.3 billion in 2010, more than doubling from 2006, according to Packaged Facts. The market-research firm surveyed 277 consumers of gluten-free products in 2010, and nearly half said they perceived them as "generally healthier."
"Confusion about gluten sensitivity has been rampant," says Alessio Fasano, director of the University of Maryland's Center for Celiac Research and a co-author of the proposal, published this week in the journal BMC Medicine. "That prompted a few of us to say, 'Let's put some facts on the table to assess what's known and what's not known.' "
The proposal—partly supported by a maker of gluten-free products, Italy's Dr. Schär AG—also spells out diagnostic criteria to help physicians determine which, if any, disorder a patient suffers from. "It is well possible that many individuals are on a gluten-free diet for no sound medical reasons," the authors note.
The American Gastroenterological Association says that much more needs to be known about gluten sensitivity before official guidelines can be devised—including how many people suffer from it and to what degree.
About 1% of people in the U.S. have celiac disease, a fourfold increase over the past 50 years. Some gastroenterologists say that for every patient with celiac disease, they see six to eight who have the same symptoms, but without the tell-tale antibodies or intestinal damage needed to confirm celiac.
Evidence is mounting that gluten sensitivity does exist. Dr. Fasano and colleagues last year compared blood samples and intestinal biopsies from people with suspected gluten sensitivity to those with confirmed celiac disease and healthy controls, and found distinct differences in each.
And in a study published last year, researchers in Australia showed in a double-blind, placebo-controlled trial that subjects with suspected gluten sensitivity had substantially fewer symptoms on a gluten-free diet than control subjects who unknowingly ingested gluten.
"Many physicians would roll their eyes and say, 'God, another crazy person with food sensitivities,' " says Peter Green, director of the Celiac Disease Center at Columbia University and a co-author of the proposal. "It's only now that studies are coming out showing that there's something real about gluten sensitivity." In fact, he notes that patients with gluten sensitivity often have even more severe symptoms than those with celiac disease, which is frequently "silent" or asymptomatic, even though antibodies to gluten are slowly damaging their intestinal tracts. That's partly why celiac disease is underdiagnosed, he says.
Confusing the picture further are private labs that offer tests of stool or saliva that they say can definitively diagnose gluten sensitivity. Experts say that such tests haven't been validated and shouldn't be relied on for a diagnosis. "If anyone claims they have a test that is specifically for gluten sensitivity, there is no such thing, though I'm not ruling it out in the future," says Dr. Fasano.
He and other researchers are hoping to find a biomarker that can officially diagnose gluten sensitivity. But for now, the proposal notes, it can only be diagnosed by ruling out the other disorders. Specifically, it says that physicians should suspect gluten sensitivity when patients complain of abdominal pain, bloating, diarrhea, constipation, anemia and other celiac symptoms, but don't have wheat allergies or the antibodies seen with celiac disease. If a biopsy is done, it generally won't show damage to the intestinal villi.
Only about half of people with gluten sensitivity have one of the two gene variations seen in virtually all celiac patients, so gene tests can rule out celiac, but not diagnose gluten sensitivity conclusively. (The blood tests cost about $100; the gene test about $300, and the biopsy $600 or more.)
Ultimately, the best test for gluten sensitivity is to see whether symptoms improve on a gluten-free diet. To avoid the power of suggestion, some doctors give patients blind tests with foods that may or may not contain hidden gluten.
Experts urge people who suspect they have problems with gluten to be tested for celiac disease before going gluten-free on their own. Otherwise, with no gluten to react to, their blood tests will show false negatives.
"This is the single biggest problem I see, and I see it every day in practice," says Joseph Murray, a celiac expert at the Mayo Clinic in Rochester, Minn.
Convincing patients who feel better to go back on gluten for testing purposes may be a hard sell. But getting a firm diagnosis is crucial, experts say, because those with celiac disease need to be on a strict gluten-free diet for the rest of their lives, or risk long-term complications including osteoporosis, infertility and some cancers. Those with gluten sensitivity may be able to eat small quantities occasionally without problems.
Cynthia Kupper, executive director of the nonprofit Gluten Intolerance Group, suggests that rather than going gluten-free on their own, people who suspect they have a gluten disorder should first keep a food diary to see if their symptoms occur shortly after consuming it. She also notes that a gluten-free diet isn't necessarily healthier, with many gluten-free products having more fat and calories than the foods they replace.
She welcomes the new classification system—in part because she sees the range of gluten disorders in her own family: She has celiac disease. Her daughter shows no signs of it, but her granddaughter has severe symptoms whenever she eats anything with gluten in it, even though tests for celiac are negative.
"When you take her off gluten, she becomes a happy child again. She's not popping Pepto-Bismol like it's candy," Ms. Kupper says.
Gluten-related disorders are rising around the world. One group of international experts has proposed classifying them based on the kind of defenses the body mounts.
Wheat allergy
Can affect skin, gastrointestinal tract or respiratory tract
Symptoms: Hives, nasal and chest congestion, nausea, vomiting, anaphylaxis
Prevalence: Less than 1% of children, most outgrow it
Diagnosis: Blood and skin prick reveal IgE antibodies; food challenge
Treatment: Avoid wheat products
Celiac disease
Antibodies to gluten damage intestinal villi needed to absorb food
Symptoms: Abdominal pain, bloating, diarrhea, fatigue, osteoporosis, cancer; can also be asymptomatic
Prevalence: 1% of adults of European descent, up fourfold in 50 years
Diagnosis: Gene tests show HLA-DQ2 or HLA-DQ8 variations; blood tests reveal tTGA or EMA antibodies; biopsy shows villi damage
Treatment: Strict gluten-free diet can reverse symptoms
Gluten ataxia
Antibodies to gluten attack cerebellum
Symptoms: Loss of balance and coordination; few GI symptoms
Prevalence: Gluten may be the cause of ataxia in a fifth of all sufferers of the ailment
Diagnosis: Blood tests show tTG6 and AGA antibodies; brain images are abnormal
Treatment: Gluten-free diet may stabilize ataxia but some damage may be irreversible
Gluten Sensitivity
Gluten may trigger a primitive immune defense
Symptoms: similar to celiac disease without villi damage; foggy thinking, mood swings
Prevalence: Unknown
Diagnosis: Rule out celiac disease and wheat allergies; possible AGA antibodies in blood; symptoms ease when avoiding gluten
Treatment: Avoiding gluten, though small amounts on occasion may not cause problems
New Guide to Who Really Shouldn't Eat Gluten
Melinda Beck : WSJ : February 8, 2012
You've got abdominal pains, bloating, fatigue and foggy thinking. You feel worse after eating wheat or other foods with gluten, and better when you avoid them.
Other autoimmune forms include dermatitis herpetiformis, which causes itchy skin lesions, and gluten ataxia, which affects brain tissue, resulting in unsteady gait and lack of motor control.
The experts also propose a third category for "gluten sensitivity," in which patients report the same symptoms as celiac disease but test negative for telltale antibodies. Some doctors have dismissed such complaints as imaginary, or fueled by the boom in gluten-free foods.
U.S. sales of gluten-free foods grew to $2.3 billion in 2010, more than doubling from 2006, according to Packaged Facts. The market-research firm surveyed 277 consumers of gluten-free products in 2010, and nearly half said they perceived them as "generally healthier."
"Confusion about gluten sensitivity has been rampant," says Alessio Fasano, director of the University of Maryland's Center for Celiac Research and a co-author of the proposal, published this week in the journal BMC Medicine. "That prompted a few of us to say, 'Let's put some facts on the table to assess what's known and what's not known.' "
The proposal—partly supported by a maker of gluten-free products, Italy's Dr. Schär AG—also spells out diagnostic criteria to help physicians determine which, if any, disorder a patient suffers from. "It is well possible that many individuals are on a gluten-free diet for no sound medical reasons," the authors note.
The American Gastroenterological Association says that much more needs to be known about gluten sensitivity before official guidelines can be devised—including how many people suffer from it and to what degree.
About 1% of people in the U.S. have celiac disease, a fourfold increase over the past 50 years. Some gastroenterologists say that for every patient with celiac disease, they see six to eight who have the same symptoms, but without the tell-tale antibodies or intestinal damage needed to confirm celiac.
Evidence is mounting that gluten sensitivity does exist. Dr. Fasano and colleagues last year compared blood samples and intestinal biopsies from people with suspected gluten sensitivity to those with confirmed celiac disease and healthy controls, and found distinct differences in each.
And in a study published last year, researchers in Australia showed in a double-blind, placebo-controlled trial that subjects with suspected gluten sensitivity had substantially fewer symptoms on a gluten-free diet than control subjects who unknowingly ingested gluten.
"Many physicians would roll their eyes and say, 'God, another crazy person with food sensitivities,' " says Peter Green, director of the Celiac Disease Center at Columbia University and a co-author of the proposal. "It's only now that studies are coming out showing that there's something real about gluten sensitivity." In fact, he notes that patients with gluten sensitivity often have even more severe symptoms than those with celiac disease, which is frequently "silent" or asymptomatic, even though antibodies to gluten are slowly damaging their intestinal tracts. That's partly why celiac disease is underdiagnosed, he says.
Confusing the picture further are private labs that offer tests of stool or saliva that they say can definitively diagnose gluten sensitivity. Experts say that such tests haven't been validated and shouldn't be relied on for a diagnosis. "If anyone claims they have a test that is specifically for gluten sensitivity, there is no such thing, though I'm not ruling it out in the future," says Dr. Fasano.
He and other researchers are hoping to find a biomarker that can officially diagnose gluten sensitivity. But for now, the proposal notes, it can only be diagnosed by ruling out the other disorders. Specifically, it says that physicians should suspect gluten sensitivity when patients complain of abdominal pain, bloating, diarrhea, constipation, anemia and other celiac symptoms, but don't have wheat allergies or the antibodies seen with celiac disease. If a biopsy is done, it generally won't show damage to the intestinal villi.
Only about half of people with gluten sensitivity have one of the two gene variations seen in virtually all celiac patients, so gene tests can rule out celiac, but not diagnose gluten sensitivity conclusively. (The blood tests cost about $100; the gene test about $300, and the biopsy $600 or more.)
Ultimately, the best test for gluten sensitivity is to see whether symptoms improve on a gluten-free diet. To avoid the power of suggestion, some doctors give patients blind tests with foods that may or may not contain hidden gluten.
Experts urge people who suspect they have problems with gluten to be tested for celiac disease before going gluten-free on their own. Otherwise, with no gluten to react to, their blood tests will show false negatives.
"This is the single biggest problem I see, and I see it every day in practice," says Joseph Murray, a celiac expert at the Mayo Clinic in Rochester, Minn.
Convincing patients who feel better to go back on gluten for testing purposes may be a hard sell. But getting a firm diagnosis is crucial, experts say, because those with celiac disease need to be on a strict gluten-free diet for the rest of their lives, or risk long-term complications including osteoporosis, infertility and some cancers. Those with gluten sensitivity may be able to eat small quantities occasionally without problems.
Cynthia Kupper, executive director of the nonprofit Gluten Intolerance Group, suggests that rather than going gluten-free on their own, people who suspect they have a gluten disorder should first keep a food diary to see if their symptoms occur shortly after consuming it. She also notes that a gluten-free diet isn't necessarily healthier, with many gluten-free products having more fat and calories than the foods they replace.
She welcomes the new classification system—in part because she sees the range of gluten disorders in her own family: She has celiac disease. Her daughter shows no signs of it, but her granddaughter has severe symptoms whenever she eats anything with gluten in it, even though tests for celiac are negative.
"When you take her off gluten, she becomes a happy child again. She's not popping Pepto-Bismol like it's candy," Ms. Kupper says.
Gluten-Free, Whether You Need It or Not
By Kenneth Chang : NY Times : February 4, 2013
Eat no wheat.
That is the core, draconian commandment of a gluten-free diet, a prohibition that excises wide swaths of American cuisine - cupcakes, pizza, bread and macaroni and cheese, to name a few things.
For the approximately one-in-a-hundred Americans who have a serious condition called celiac disease, that is an indisputably wise medical directive.
Now medical experts largely agree that there is a condition related to gluten other than celiac. In 2011 a panel of celiac experts convened in Oslo and settled on a medical term for this malady: non-celiac gluten sensitivity.
What they still do not know: how many people have gluten sensitivity, what its long-term effects are, or even how to reliably identify it. Indeed, they do not really know what the illness is.
The definition is less a diagnosis than a description - someone who does not have celiac, but whose health improves on a gluten-free diet and worsens again if gluten is eaten. It could even be more than one illness.
"We have absolutely no clue at this point," said Dr. Stefano Guandalini, medical director of the University of Chicago's Celiac Disease Center.
Kristen Golden Testa could be one of the gluten-sensitive. Although she does not have celiac, she adopted a gluten-free diet last year. She says she has lost weight and her allergies have gone away. "It's just so marked," said Ms. Golden Testa, who is health program director in California for the Children's Partnership, a national nonprofit advocacy group.
She did not consult a doctor before making the change, and she also does not know whether avoiding gluten has helped at all. "This is my speculation," she said. She also gave up sugar at the same time and made an effort to eat more vegetables and nuts.
Many advocates of gluten-free diets warn that non-celiac gluten sensitivity is a wide, unseen epidemic undermining the health of millions of people. They believe that avoiding gluten - a composite of starch and proteins found in certain grassy grains like wheat, barley and rye - gives them added energy and alleviates chronic ills. Oats, while gluten-free, are also avoided, because they are often contaminated with gluten-containing grains.
Others see the popularity of gluten-free foods as just the latest fad, destined to fade like the Atkins diet and avoidance of carbohydrates a decade ago.
Indeed, Americans are buying billions of dollars of food labeled gluten-free each year. And celebrities like Miley Cyrus, the actress and singer, have urged fans to give up gluten. "The change in your skin, physical and mental health is amazing!" she posted on Twitter in April.
For celiac experts, the anti-gluten zeal is a dramatic turnaround; not many years ago, they were struggling to raise awareness among doctors that bread and pasta can make some people very sick. Now they are voicing caution, tamping down the wilder claims about gluten-free diets.
"It is not a healthier diet for those who don't need it," Dr. Guandalini said. These people "are following a fad, essentially." He added, "And that's my biased opinion."
Nonetheless, Dr. Guandalini agrees that some people who do not have celiac receive a genuine health boost from a gluten-free diet. He just cannot say how many.
As with most nutrition controversies, most everyone agrees on the underlying facts. Wheat entered the human diet only about 10,000 years ago, with the advent of agriculture.
"For the previous 250,000 years, man had evolved without having this very strange protein in his gut," Dr. Guandalini said. "And as a result, this is a really strange, different protein which the human intestine cannot fully digest. Many people did not adapt to these great environmental changes, so some adverse effects related to gluten ingestion developed around that time."
The primary proteins in wheat gluten are glutenin and gliadin, and gliadin contains repeating patterns of amino acids that the human digestive system cannot break down. (Gluten is the only substance that contains these proteins.) People with celiac have one or two genetic mutations that somehow, when pieces of gliadin course through the gut, cause the immune system to attack the walls of the intestine in a case of mistaken identity. That, in turn, causes fingerlike structures called villi that absorb nutrients on the inside of the intestines to atrophy, and the intestines can become leaky, wreaking havoc. Symptoms, which vary widely among people with the disease, can include vomiting, chronic diarrhea or constipation and diminished growth rates in children.
The vast majority of people who have celiac do not know it. And not everyone who has the genetic mutations develops celiac.
What worries doctors is that the problem seems to be growing. After testing blood samples from a century ago, researchers discovered that the rate of celiac appears to be increasing. Why is another mystery. Some blame the wheat, as some varieties now grown contain higher levels of gluten, because gluten helps provide the springy inside and crusty outside desirable in bread. (Blame the artisanal bakers.)
There are also people who are allergic to wheat (not necessarily gluten), but until recently, most experts had thought that celiac and wheat allergy were the only problems caused by eating the grain.
For 99 out of 100 people who don't have celiac - and those who don't have a wheat allergy - the undigested gliadin fragments usually pass harmlessly through the gut, and the possible benefits of a gluten-free diet are nebulous, perhaps nonexistent for most. But not all.
Anecdotally, people like Ms. Golden Testa say that gluten-free diets have improved their health. Some people with diseases like irritable bowel syndrome and arthritis also report alleviation of their symptoms, and others are grasping at gluten as a source of a host of other conditions, though there is no scientific evidence to back most of the claims. Experts have been skeptical. It does not make obvious sense, for example, that someone would lose weight on a gluten-free diet. In fact, the opposite often happens for celiac patients as their malfunctioning intestines recover.
They also worried that people could end up eating less healthfully. A gluten-free muffin generally contains less fiber than a wheat-based one and still offers the same nutritional dangers - fat and sugar. Gluten-free foods are also less likely to be fortified with vitamins.
But those views have changed. Crucial in the evolving understanding of gluten were the findings, published in 2011, in The American Journal of Gastroenterology, of an experiment in Australia. In the double-blind study, people who suffered from irritable bowel syndrome, did not have celiac and were on a gluten-free diet were given bread and muffins to eat for up to six weeks. Some of them were given gluten-free baked goods; the others got muffins and bread with gluten. Thirty-four patients completed the study. Those who ate gluten reported they felt significantly worse.
That influenced many experts to acknowledge that the disease was not just in the heads of patients. "It's not just a placebo effect," said Dr. Marios Hadjivassiliou, a neurologist and celiac expert at the University of Sheffield in England.
Even though there was now convincing evidence that gluten sensitivity exists, that has not helped to establish what causes gluten sensitivity. The researchers of the Australian experiment noted, "No clues to the mechanism were elucidated."
What is known is that gluten sensitivity does not correlate with the genetic mutations of celiac, so it appears to be something distinct from celiac.
How widespread gluten sensitivity may be is another point of controversy.
Dr. Thomas O'Bryan, a chiropractor turned anti-gluten crusader, said that when he tested his patients, 30 percent of them had antibodies targeting gliadin fragments in their blood. "If a person has a choice between eating wheat or not eating wheat," he said, "then for most people, avoiding wheat would be ideal."
Dr. O'Bryan has given himself a diagnosis of gluten sensitivity. "I had these blood sugar abnormalities and didn't have a handle where they were coming from," he said. He said a blood test showed gliadin antibodies, and he started avoiding gluten. "It took me a number of years to get completely gluten-free," he said. "I'd still have a piece of pie once in a while. And I'd notice afterwards that I didn't feel as good the next day or for two days. Subtle, nothing major, but I'd notice that."
But Suzy Badaracco, president of Culinary Tides, Inc., a consulting firm, said fewer people these days were citing the benefits of gluten-free diets. She said a recent survey of people who bought gluten-free foods found that 35 percent said they thought gluten-free products were generally healthier, down from 46 percent in 2010. She predicted that the use of gluten-free products would decline.
Dr. Guandalini said finding out whether you are gluten sensitive is not as simple as Dr. O'Bryan's antibody tests, because the tests only indicate the presence of the fragments in the blood, which can occur for a variety of reasons and do not necessarily indicate a chronic illness. For diagnosing gluten sensitivity, "There is no testing of the blood that can be helpful," he said.
He also doubts that the occurrence of gluten sensitivity is nearly as high as Dr. O'Bryan asserts. "No more than 1 percent," Dr. Guandalini said, although he agreed that at present all numbers were speculative.
He said his research group was working to identify biological tests that could determine gluten sensitivity. Some of the results are promising, he said, but they are too preliminary to discuss. Celiac experts urge people to not do what Ms. Golden Testa did - self-diagnose. Should they actually have celiac, tests to diagnose it become unreliable if one is not eating gluten. They also recommend visiting a doctor before starting on a gluten-free diet.
Can Celiac Disease Affect the Brain?
By Moises Velasquez-Manoff : NY Times : October 11, 2014
When Andre H. Lagrange, a neurologist at Vanderbilt University in Nashville, saw the ominous white spots on the patient’s brain scan, he considered infection or lymphoma, a type of cancer. But tests ruled out both. Meanwhile, anti-epilepsy drugs failed to halt the man’s seizures. Stumped, Dr. Lagrange turned to something the mother of the 30-year-old man kept repeating. The fits coincided, she insisted, with spells of constipation and diarrhea.
That, along with an odd rash, prompted Dr. Lagrange to think beyond the brain. Antibody tests, followed by an intestinal biopsy, indicated celiac disease, an autoimmune disorder of the gut triggered by the gluten proteins in wheat and other grains. Once on a gluten-free diet, the man’s seizures stopped; those brain lesions gradually disappeared. He made a “nearly complete recovery,” Dr. Lagrange told me.
I began encountering case descriptions like this some years ago as I researched autoimmune disease. The first few seemed like random noise in an already nebulous field. But as I amassed more — describing seizures, hallucinations, psychotic breaks and even, in one published case, what looked like regressive autism, all ultimately associated with celiac disease — they began to seem less like anomalies, and more like a frontier in celiac research.
They tended to follow a similar plot. What looked like neurological or psychiatric symptoms appeared suddenly. The physician ran through a diagnostic checklist without success. Drugs directed at the brain failed. Some clue suggestive of celiac disease was observed. The diagnosis was made. And the patient recovered on a gluten-free diet.
The cases highlighted, in an unusually concrete fashion, the so-called gut-brain axis. The supposed link between the intestinal tract and the central nervous system is much discussed in science journals, often in the context of the microbial community inhabiting the gut. But it’s unclear how, really, we can leverage the link to improve health.
Here, though, was a rather spectacular example: Treating an autoimmune disease of the gut (by avoiding gluten) resolved what looked like a debilitating disorder of the brain. The broader takeaway was that, in some subset of patients, apparent neurological symptoms could signal undiagnosed celiac disease.
These are individual cases, but Celiac disease has long been associated with symptoms beyond the gut, including blistering rashes, burning nerve pain, and a loss of muscle control called ataxia. Historically, scientists often attributed these problems to nutrient deficiencies, which undoubtedly occur in some cases. Gut inflammation can hinder the absorption of critical nutrients, such as copper or B vitamins, prompting neurological dysfunction.
But as antibodies specific to tissues beyond the gut have come to light, some now suspect that the autoimmune firestorm ignited in the gut may descend on other organs, including the brain. This idea, which remains hypothetical, has gained traction during a time of progress in understanding autoimmune diseases of the central nervous system.
At the Mayo Clinic in Rochester, Minn., a center of research on neurological autoimmunity, patients with autoimmune epilepsy, dementia and other recently described autoimmune disorders are frequently “cured” with immunotherapy. That usually involves some combination of steroidal immune-suppressants, intravenous immunoglobulin-G, which consists of antibodies from donors, and plasmapheresis, a procedure that removes antibodies from the blood.
THE Mayo Clinic is on track to run 140,000 tests this year for autoimmune disorders of the brain, about a 20 percent increase over last year. One-tenth of samples usually come back positive for the self-directed antibodies indicative of autoimmunity, said Sean J. Pittock, a neurologist there. Many of these patients have cancers, which can trigger an attack. But a fraction have an autoimmune disease of the brain.
“There are people out there who are very ill and in nursing homes, and their condition is treatable and reversible,” he said. “And they’re being missed.” It’s rare, but he estimates these patients to number in the many thousands.
One such story comes from the journalist Susannah Cahalan whose memoir “Brain on Fire” details her bout with autoimmune encephalitis. Her sudden descent into “madness” resembled a psychotic break. And just a few years earlier, before the condition was understood to be autoimmune, she might have been considered lost to psychosis and institutionalized. But in 2009, Ms. Cahalan, the 217th patient to get the diagnosis of what’s called anti-NMDA receptor encephalitis, was treated for her autoimmune disorder and recovered.
Celiac disease differs from most other autoimmune diseases in one critical respect: The trigger, gluten, is known. And in most cases, removing gluten will turn off the autoimmune destruction in the gut. Around 10 percent of people with celiac disease, and possibly more, are thought to suffer neurological symptoms, ranging from headache and nerve pain, to ataxia and to epilepsy.
When I called Alessio Fasano, director of the Center for Celiac Research at Massachusetts General Hospital in Boston, he spoke of his own celiac-related miracle stories. In one, a boy with autism-like symptoms actually had undiagnosed celiac disease, and recovered on a gluten-free diet. Dr. Fasano told me he had seen a few similar cases in his native Italy.
In another, a former professor diagnosed with dementia and institutionalized, recovered on a gluten-free diet. Her doctors knew she had celiac disease, but thought it irrelevant to her degenerative brain disorder.
Some researchers have proposed autoimmune mechanisms to explain these phenomena. The presence of antibodies that bind to an enzyme called transglutaminase 2 is used to help diagnose celiac disease. Among other functions, transglutaminases help seal barriers in the body. Scientists at the Royal Hallamshire Hospital in Sheffield, Britain, have identified an antibody that binds to a version of transglutaminase, called TG6, which occurs primarily in the brain.
This antibody, they argue, may identify celiac patients at risk for neurological complications. When celiac patients with ataxia adopt a gluten-free diet, they showed last year, those brain-directed antibodies decline and their symptoms improved. And injecting the antibodies into the brains of mice prompts ataxia-like symptoms, suggesting that they can cause (rather than result from) disease.
Rather than celiac disease driving autoimmune brain problems, he thinks, distinct autoimmune diseases are likely to cluster in the same individual. Avoiding gluten won’t entirely mend these patients.
The even more controversial idea is that a subset of patients mounts an immune response to gluten without obvious intestinal inflammation, and develops neurological symptoms. Marios Hadjivassiliou, a neurologist at the Royal Hallamshire Hospital, calls one variant of this entity “gluten ataxia”: a gluten-triggered disease whose primary symptoms occur in the brain.
Although the idea remains debated, physicians I queried weren’t ready to dismiss it. That’s partly because some years ago, Armin Alaedini, an immunologist now at Columbia University, found that antibodies directed at gliadin, a gluten protein, could cross-react with proteins in the brain. The finding suggests that, by some coincidence, certain proteins on neurons structurally resemble proteins in wheat. Meaning that, if your immune system attacks gluten, it might also inadvertently pursue brain tissue.
This discovery has helped revive an old idea about schizophrenia. Might an immune reaction to wheat contribute in some cases? In 2011, Johns Hopkins University scientists found that nearly one-quarter of serum samples from some 1,400 schizophrenia patients had anti-gliadin antibodies, compared with just 3 percent of healthy controls. Of the subset with those antibodies, one-fifth also had those antibodies to transglutaminase 6 linked with neurological dysfunction, compared with 6 percent of healthy controls.
It’s unclear if these antibodies contribute to schizophrenia, result from it, or are irrelevant to it. Dr. McKeon considers some of the antibody tests to be poor diagnostic tools. And Dr. Alaedini suspects that, rather than causing problems, they may indicate systemic inflammation and a defect in the intestinal barrier. Numerous immune abnormalities have been described in schizophrenia.
But in a pilot study on two patients with those antibodies, Deanna L. Kelly, a researcher at the University of Maryland in Baltimore, found that a gluten-free diet alleviated some symptoms. Now Dr. Kelly is beginning a larger, gluten-free intervention on that subgroup.
By one recent estimate, meanwhile, one in three Americans dabbles in a gluten-free diet. That vastly outnumbers those thought to have celiac disease — about 1 percent — or the (still unmeasurable) percentage of people with gluten sensitivity, estimated at slightly higher. And yet, the prevalence of celiac disease is indeed rising. Symptoms are increasingly understood to manifest beyond the gut, including occasionally in the brain. Gluten sensitivity may yet prove to be real and measurable.
No one I spoke to recommends going on a gluten-free diet proactively. But when sudden and inexplicable neurological problems arise, it’s not completely far-fetched to raise the gluten question with your doctor. It just might provide an answer.
Moises Velasquez-Manoff is a science writer and the author of “An Epidemic of Absence.”
By Moises Velasquez-Manoff : NY Times : October 11, 2014
When Andre H. Lagrange, a neurologist at Vanderbilt University in Nashville, saw the ominous white spots on the patient’s brain scan, he considered infection or lymphoma, a type of cancer. But tests ruled out both. Meanwhile, anti-epilepsy drugs failed to halt the man’s seizures. Stumped, Dr. Lagrange turned to something the mother of the 30-year-old man kept repeating. The fits coincided, she insisted, with spells of constipation and diarrhea.
That, along with an odd rash, prompted Dr. Lagrange to think beyond the brain. Antibody tests, followed by an intestinal biopsy, indicated celiac disease, an autoimmune disorder of the gut triggered by the gluten proteins in wheat and other grains. Once on a gluten-free diet, the man’s seizures stopped; those brain lesions gradually disappeared. He made a “nearly complete recovery,” Dr. Lagrange told me.
I began encountering case descriptions like this some years ago as I researched autoimmune disease. The first few seemed like random noise in an already nebulous field. But as I amassed more — describing seizures, hallucinations, psychotic breaks and even, in one published case, what looked like regressive autism, all ultimately associated with celiac disease — they began to seem less like anomalies, and more like a frontier in celiac research.
They tended to follow a similar plot. What looked like neurological or psychiatric symptoms appeared suddenly. The physician ran through a diagnostic checklist without success. Drugs directed at the brain failed. Some clue suggestive of celiac disease was observed. The diagnosis was made. And the patient recovered on a gluten-free diet.
The cases highlighted, in an unusually concrete fashion, the so-called gut-brain axis. The supposed link between the intestinal tract and the central nervous system is much discussed in science journals, often in the context of the microbial community inhabiting the gut. But it’s unclear how, really, we can leverage the link to improve health.
Here, though, was a rather spectacular example: Treating an autoimmune disease of the gut (by avoiding gluten) resolved what looked like a debilitating disorder of the brain. The broader takeaway was that, in some subset of patients, apparent neurological symptoms could signal undiagnosed celiac disease.
These are individual cases, but Celiac disease has long been associated with symptoms beyond the gut, including blistering rashes, burning nerve pain, and a loss of muscle control called ataxia. Historically, scientists often attributed these problems to nutrient deficiencies, which undoubtedly occur in some cases. Gut inflammation can hinder the absorption of critical nutrients, such as copper or B vitamins, prompting neurological dysfunction.
But as antibodies specific to tissues beyond the gut have come to light, some now suspect that the autoimmune firestorm ignited in the gut may descend on other organs, including the brain. This idea, which remains hypothetical, has gained traction during a time of progress in understanding autoimmune diseases of the central nervous system.
At the Mayo Clinic in Rochester, Minn., a center of research on neurological autoimmunity, patients with autoimmune epilepsy, dementia and other recently described autoimmune disorders are frequently “cured” with immunotherapy. That usually involves some combination of steroidal immune-suppressants, intravenous immunoglobulin-G, which consists of antibodies from donors, and plasmapheresis, a procedure that removes antibodies from the blood.
THE Mayo Clinic is on track to run 140,000 tests this year for autoimmune disorders of the brain, about a 20 percent increase over last year. One-tenth of samples usually come back positive for the self-directed antibodies indicative of autoimmunity, said Sean J. Pittock, a neurologist there. Many of these patients have cancers, which can trigger an attack. But a fraction have an autoimmune disease of the brain.
“There are people out there who are very ill and in nursing homes, and their condition is treatable and reversible,” he said. “And they’re being missed.” It’s rare, but he estimates these patients to number in the many thousands.
One such story comes from the journalist Susannah Cahalan whose memoir “Brain on Fire” details her bout with autoimmune encephalitis. Her sudden descent into “madness” resembled a psychotic break. And just a few years earlier, before the condition was understood to be autoimmune, she might have been considered lost to psychosis and institutionalized. But in 2009, Ms. Cahalan, the 217th patient to get the diagnosis of what’s called anti-NMDA receptor encephalitis, was treated for her autoimmune disorder and recovered.
Celiac disease differs from most other autoimmune diseases in one critical respect: The trigger, gluten, is known. And in most cases, removing gluten will turn off the autoimmune destruction in the gut. Around 10 percent of people with celiac disease, and possibly more, are thought to suffer neurological symptoms, ranging from headache and nerve pain, to ataxia and to epilepsy.
When I called Alessio Fasano, director of the Center for Celiac Research at Massachusetts General Hospital in Boston, he spoke of his own celiac-related miracle stories. In one, a boy with autism-like symptoms actually had undiagnosed celiac disease, and recovered on a gluten-free diet. Dr. Fasano told me he had seen a few similar cases in his native Italy.
In another, a former professor diagnosed with dementia and institutionalized, recovered on a gluten-free diet. Her doctors knew she had celiac disease, but thought it irrelevant to her degenerative brain disorder.
Some researchers have proposed autoimmune mechanisms to explain these phenomena. The presence of antibodies that bind to an enzyme called transglutaminase 2 is used to help diagnose celiac disease. Among other functions, transglutaminases help seal barriers in the body. Scientists at the Royal Hallamshire Hospital in Sheffield, Britain, have identified an antibody that binds to a version of transglutaminase, called TG6, which occurs primarily in the brain.
This antibody, they argue, may identify celiac patients at risk for neurological complications. When celiac patients with ataxia adopt a gluten-free diet, they showed last year, those brain-directed antibodies decline and their symptoms improved. And injecting the antibodies into the brains of mice prompts ataxia-like symptoms, suggesting that they can cause (rather than result from) disease.
Rather than celiac disease driving autoimmune brain problems, he thinks, distinct autoimmune diseases are likely to cluster in the same individual. Avoiding gluten won’t entirely mend these patients.
The even more controversial idea is that a subset of patients mounts an immune response to gluten without obvious intestinal inflammation, and develops neurological symptoms. Marios Hadjivassiliou, a neurologist at the Royal Hallamshire Hospital, calls one variant of this entity “gluten ataxia”: a gluten-triggered disease whose primary symptoms occur in the brain.
Although the idea remains debated, physicians I queried weren’t ready to dismiss it. That’s partly because some years ago, Armin Alaedini, an immunologist now at Columbia University, found that antibodies directed at gliadin, a gluten protein, could cross-react with proteins in the brain. The finding suggests that, by some coincidence, certain proteins on neurons structurally resemble proteins in wheat. Meaning that, if your immune system attacks gluten, it might also inadvertently pursue brain tissue.
This discovery has helped revive an old idea about schizophrenia. Might an immune reaction to wheat contribute in some cases? In 2011, Johns Hopkins University scientists found that nearly one-quarter of serum samples from some 1,400 schizophrenia patients had anti-gliadin antibodies, compared with just 3 percent of healthy controls. Of the subset with those antibodies, one-fifth also had those antibodies to transglutaminase 6 linked with neurological dysfunction, compared with 6 percent of healthy controls.
It’s unclear if these antibodies contribute to schizophrenia, result from it, or are irrelevant to it. Dr. McKeon considers some of the antibody tests to be poor diagnostic tools. And Dr. Alaedini suspects that, rather than causing problems, they may indicate systemic inflammation and a defect in the intestinal barrier. Numerous immune abnormalities have been described in schizophrenia.
But in a pilot study on two patients with those antibodies, Deanna L. Kelly, a researcher at the University of Maryland in Baltimore, found that a gluten-free diet alleviated some symptoms. Now Dr. Kelly is beginning a larger, gluten-free intervention on that subgroup.
By one recent estimate, meanwhile, one in three Americans dabbles in a gluten-free diet. That vastly outnumbers those thought to have celiac disease — about 1 percent — or the (still unmeasurable) percentage of people with gluten sensitivity, estimated at slightly higher. And yet, the prevalence of celiac disease is indeed rising. Symptoms are increasingly understood to manifest beyond the gut, including occasionally in the brain. Gluten sensitivity may yet prove to be real and measurable.
No one I spoke to recommends going on a gluten-free diet proactively. But when sudden and inexplicable neurological problems arise, it’s not completely far-fetched to raise the gluten question with your doctor. It just might provide an answer.
Moises Velasquez-Manoff is a science writer and the author of “An Epidemic of Absence.”