- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Reasons That Vitamin D May Matter
Jane E. Brody : NY Times : March 12, 2012
At least once a week, someone, usually a woman over 50, asks me about vitamin D. Perhaps a routine checkup has revealed a deficiency, prompting the doctor to recommend an over-the-counter supplement or, in severe cases, large prescription doses to correct the problem.
Often, though, the concern is bone health. Without vitamin D, the body cannot properly absorb calcium, and bones become fragile. At the annual meeting of the American Academy of Orthopaedic Surgeons last month, researchers reported that among 889 adult patients treated for a fracture at a Missouri trauma center, blood levels of vitamin D were “insufficient” in 78 percent and “frankly deficient” in 39 percent. The study group excluded those with known risk factors for vitamin D deficiency.
A second report, by doctors in Seoul, South Korea, found vitamin D levels were “significantly lower” among 104 postmenopausal women who had broken a wrist than among 107 age-matched controls without a fracture.
But increasingly I receive inquiries regarding research suggesting that raising blood levels of vitamin D may protect against chronic or life-threatening diseases. Many studies in recent years have linked low levels to health risks like heart disease, high blood pressure, cancer, rheumatoid arthritis and other autoimmune diseases, prompting many health-conscious men and women to think that supplements of vitamin D are protective.
Alas, there are still no large-scale randomized controlled clinical trials — the gold standard of human research — to prove or disprove the value of vitamin D supplementation beyond its well-known benefits to bone health.
Nonetheless, Dr. Kevin A. Fiscella, a public health specialist and family physician at the University of Rochester, has decided to take 1,000 international units of vitamin D each day, based on data from his studies linking racial disparities in vitamin D levels to disease risk and his belief that “it can’t hurt and it may help.”
A Vitamin With Broad Influence
In an interview, Dr. Fiscella emphasized that his findings strongly suggest, but do not prove, that vitamin D deficiencies cause or contribute to diseases like colorectal cancer, high blood pressure and kidney and heart disease, which affect black Americans at higher rates than whites. The findings are bolstered by known biological effects of vitamin D and by the fact that widespread vitamin D deficiencies occur among blacks living in the Northern Hemisphere.
Nearly every body tissue has receptors for vitamin D, among them the intestines, brain, heart, skin, sex organs, breasts and lymphocytes, as well as the placenta. The vitamin, which acts as a hormone, is known to influence the expression of more than 200 genes.
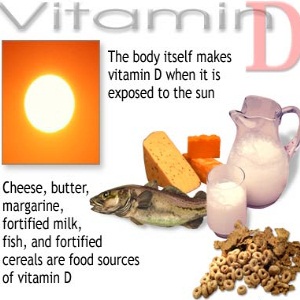
In laboratory studies, it has been shown to have anticancer activity, inhibiting the growth and spread of tumors. There is also suggestive but inconclusive evidence that vitamin D deficiency plays a role in asthma, Type 2 diabetes, autoimmune diseases like multiple sclerosis and rheumatoid arthritis, pre-eclampsia and low birth weight, and neuropsychological disorders like depression, autism and memory loss. Vitamin D is a fat-soluble essential nutrient that naturally enters the body primarily through the skin, where ultraviolet B radiation in sunlight stimulates production of previtamin D. This, in turn, is converted to the biologically active form, vitamin D hormone, in the kidneys.
Very few foods naturally contain meaningful levels of vitamin D; mostly they are fatty cold-water fish like salmon, mackerel, bluefish, anchovies, sardines and tuna, as well as cod liver oil. Some foods are fortified with the vitamin, especially milk, infant formula and, more recently, some brands of orange juice, yogurt, cheese and breakfast cereal.
Several factors work against achieving the levels of vitamin D known to prevent bone loss, let alone other diseases should a cause-and-effect ever be established.
One is skin color. Dark skin evolved in equatorial Africa, where the sun is intense year round and just a brief daily exposure to UVB (the sun’s burning rays) is sufficient to achieve adequate blood levels of vitamin D. But melanin in the skin acts as a natural sunblock, and among blacks living in the United States, where sun is less intense, less of the previtamin is produced.
Dr. Fiscella’s studies, based on thousands of adult participants in the National Health and Nutrition Examination Survey conducted from 2001 to 2006, revealed much higher rates of vitamin D deficiency among non-Hispanic blacks than non-Hispanic whites. Furthermore, in separate studies, lower levels of vitamin D among blacks across the country were associated with a greater incidence of colorectal cancer, high blood pressure, protein in urine (a precursor of kidney disease) and cardiovascular deaths.
Avoiding Deficiency
Warnings about the cosmetic and cancerous consequences of undue sun exposure have prompted millions of health-conscious Americans to protect themselves from UVB with protective clothing and liberal use of sunscreen on exposed skin. The latter can reduce previtamin D production in skin by more than 90 percent.
In addition, because vitamin D is stored in body fat, the dramatic increase in obesity in this country is placing more people, regardless of skin color, at risk of inadequate levels of D in blood serum.
Finally, consumption of milk has declined significantly, and most other popular dairy products are not fortified with D.
As a result, growing numbers of light-skinned Americans are finding that they, too, are not getting enough D to bring their serum levels to 20 nanograms per milliliter, the level deemed adequate by the Institute of Medicine, and even fewer reach 30 nanograms, the level many bone specialists and vitamin D researchers consider more desirable.
A placebo-controlled clinical trial called Vital, sponsored by the National Institutes of Health and due to be completed in 2016, is assessing the effect of a daily supplement of 2,000 I.U. of vitamin D on the risk of developing heart disease, cancer and stroke among 20,000 men over 50 and women over 55 with no prior history of these diseases.
Meanwhile, the Endocrine Society recommends that people at risk for vitamin D deficiency be screened to determine their serum levels, including those with bone disease, chronic kidney disease, liver failure, malabsorption syndromes (resulting from cystic fibrosis, irritable bowel disease, weight-reduction surgery or abdominal radiation), overactive parathyroid and granuloma-forming disorders. People taking drugs like anticonvulsants, glucocorticoids, antiretrovirals, antifungals and cholestyramine also should be tested, as well as older adults with a history of falls or nontraumatic fracture.
Certain groups at risk for a deficiency also warrant screening: blacks, obese children and adults, and pregnant or nursing women, Dr. Fiscella said.
Jane E. Brody : NY Times : March 12, 2012
At least once a week, someone, usually a woman over 50, asks me about vitamin D. Perhaps a routine checkup has revealed a deficiency, prompting the doctor to recommend an over-the-counter supplement or, in severe cases, large prescription doses to correct the problem.
Often, though, the concern is bone health. Without vitamin D, the body cannot properly absorb calcium, and bones become fragile. At the annual meeting of the American Academy of Orthopaedic Surgeons last month, researchers reported that among 889 adult patients treated for a fracture at a Missouri trauma center, blood levels of vitamin D were “insufficient” in 78 percent and “frankly deficient” in 39 percent. The study group excluded those with known risk factors for vitamin D deficiency.
A second report, by doctors in Seoul, South Korea, found vitamin D levels were “significantly lower” among 104 postmenopausal women who had broken a wrist than among 107 age-matched controls without a fracture.
But increasingly I receive inquiries regarding research suggesting that raising blood levels of vitamin D may protect against chronic or life-threatening diseases. Many studies in recent years have linked low levels to health risks like heart disease, high blood pressure, cancer, rheumatoid arthritis and other autoimmune diseases, prompting many health-conscious men and women to think that supplements of vitamin D are protective.
Alas, there are still no large-scale randomized controlled clinical trials — the gold standard of human research — to prove or disprove the value of vitamin D supplementation beyond its well-known benefits to bone health.
Nonetheless, Dr. Kevin A. Fiscella, a public health specialist and family physician at the University of Rochester, has decided to take 1,000 international units of vitamin D each day, based on data from his studies linking racial disparities in vitamin D levels to disease risk and his belief that “it can’t hurt and it may help.”
A Vitamin With Broad Influence
In an interview, Dr. Fiscella emphasized that his findings strongly suggest, but do not prove, that vitamin D deficiencies cause or contribute to diseases like colorectal cancer, high blood pressure and kidney and heart disease, which affect black Americans at higher rates than whites. The findings are bolstered by known biological effects of vitamin D and by the fact that widespread vitamin D deficiencies occur among blacks living in the Northern Hemisphere.
Nearly every body tissue has receptors for vitamin D, among them the intestines, brain, heart, skin, sex organs, breasts and lymphocytes, as well as the placenta. The vitamin, which acts as a hormone, is known to influence the expression of more than 200 genes.
In laboratory studies, it has been shown to have anticancer activity, inhibiting the growth and spread of tumors. There is also suggestive but inconclusive evidence that vitamin D deficiency plays a role in asthma, Type 2 diabetes, autoimmune diseases like multiple sclerosis and rheumatoid arthritis, pre-eclampsia and low birth weight, and neuropsychological disorders like depression, autism and memory loss. Vitamin D is a fat-soluble essential nutrient that naturally enters the body primarily through the skin, where ultraviolet B radiation in sunlight stimulates production of previtamin D. This, in turn, is converted to the biologically active form, vitamin D hormone, in the kidneys.
Very few foods naturally contain meaningful levels of vitamin D; mostly they are fatty cold-water fish like salmon, mackerel, bluefish, anchovies, sardines and tuna, as well as cod liver oil. Some foods are fortified with the vitamin, especially milk, infant formula and, more recently, some brands of orange juice, yogurt, cheese and breakfast cereal.
Several factors work against achieving the levels of vitamin D known to prevent bone loss, let alone other diseases should a cause-and-effect ever be established.
One is skin color. Dark skin evolved in equatorial Africa, where the sun is intense year round and just a brief daily exposure to UVB (the sun’s burning rays) is sufficient to achieve adequate blood levels of vitamin D. But melanin in the skin acts as a natural sunblock, and among blacks living in the United States, where sun is less intense, less of the previtamin is produced.
Dr. Fiscella’s studies, based on thousands of adult participants in the National Health and Nutrition Examination Survey conducted from 2001 to 2006, revealed much higher rates of vitamin D deficiency among non-Hispanic blacks than non-Hispanic whites. Furthermore, in separate studies, lower levels of vitamin D among blacks across the country were associated with a greater incidence of colorectal cancer, high blood pressure, protein in urine (a precursor of kidney disease) and cardiovascular deaths.
Avoiding Deficiency
Warnings about the cosmetic and cancerous consequences of undue sun exposure have prompted millions of health-conscious Americans to protect themselves from UVB with protective clothing and liberal use of sunscreen on exposed skin. The latter can reduce previtamin D production in skin by more than 90 percent.
In addition, because vitamin D is stored in body fat, the dramatic increase in obesity in this country is placing more people, regardless of skin color, at risk of inadequate levels of D in blood serum.
Finally, consumption of milk has declined significantly, and most other popular dairy products are not fortified with D.
As a result, growing numbers of light-skinned Americans are finding that they, too, are not getting enough D to bring their serum levels to 20 nanograms per milliliter, the level deemed adequate by the Institute of Medicine, and even fewer reach 30 nanograms, the level many bone specialists and vitamin D researchers consider more desirable.
A placebo-controlled clinical trial called Vital, sponsored by the National Institutes of Health and due to be completed in 2016, is assessing the effect of a daily supplement of 2,000 I.U. of vitamin D on the risk of developing heart disease, cancer and stroke among 20,000 men over 50 and women over 55 with no prior history of these diseases.
Meanwhile, the Endocrine Society recommends that people at risk for vitamin D deficiency be screened to determine their serum levels, including those with bone disease, chronic kidney disease, liver failure, malabsorption syndromes (resulting from cystic fibrosis, irritable bowel disease, weight-reduction surgery or abdominal radiation), overactive parathyroid and granuloma-forming disorders. People taking drugs like anticonvulsants, glucocorticoids, antiretrovirals, antifungals and cholestyramine also should be tested, as well as older adults with a history of falls or nontraumatic fracture.
Certain groups at risk for a deficiency also warrant screening: blacks, obese children and adults, and pregnant or nursing women, Dr. Fiscella said.
Triple That Vitamin D Intake, Panel Prescribes
Melinda Beck : WSJ : November 30, 2010
A long-awaited report from the Institute of Medicine to be released Tuesday triples the recommended amount of vitamin D most Americans should take every day to 600 international units from 200 IUs set in 1997.
That's far lower than many doctors and major medical groups have been advocating—and it could dampen some of the enthusiasm that's been building for the sunshine vitamin in recent years.
Many doctors have added blood tests of vitamin D levels to annual physicals, and sales of vitamin D supplements have soared to $425 million last year from $40 million in 2001, according to the Nutrition Business Journal.
The IOM panel also issued new recommendations for daily calcium intake, up to 1,200 milligrams for women 51 and older.
Who Needs Extra D?
Some people are at high risk for vitamin D deficiency, and experts believe they may benefit from more vitamin D than the new recommendations:
It's long been known that vitamin D is essential to maintaining strong bones. But hundreds of new studies have also linked low vitamin D levels to a higher risk of a slew of chronic health problems—heart disease, stroke, diabetes, prostate, breast and colon cancers, auto-immune diseases, infections, depression and cognitive decline. Studies have also suggested that many Americans are vitamin D deficient due to working and playing indoors and slathering on sunscreen.
The Institute of Medicine, an arm of the National Academy of Sciences that sets governmental nutrient levels, said there wasn't enough evidence to prove that low vitamin D causes such chronic diseases; it based its new recommendations on the levels needed to maintain strong bones alone.
"The evidence for bone health is compelling, consistent and gives strong evidence of cause and effect," said Patsy Brannon, a professor of nutritional sciences at Cornell University and member of the IOM panel. For the other health problems, she said, "there are relatively few randomized controlled trials, and even in the observational studies, the effects are inconsistent."
The new recommendations, which cover the U.S. and Canada, call for 600 IUs daily for infants through adults age 70 and 800 IUs after age 71. The IOM assumed that most people are getting minimal sun exposure, given rising concern over skin cancer and latitudes where the sun is too weak to create vitamin D on the skin much of the year. The panel also raised the acceptable upper limit of daily intake to 4,000 IUs for adults, from 2,000 previously.
Those levels do take into account vitamin D from food sources—but only a few, such as salmon and mackerel, contain much naturally. Milk fortified with vitamin D contains about 40 IUs per cup. Most Americans and Canadians need to get much of their vitamin D from supplements.
The IOM panel also issued new recommendations for daily calcium intake— ranging from 700 milligrams for children aged 1 to 3 up to 1,200 milligrams for women 51 and older. The main change from the 1997 recommendations was to lower the recommended level for men 50 to 70 to 1,000 from 1,200. The panel noted that teenage girls may not get enough calcium, and that postmenopausal women may get too much, running the risk of kidney stones.
The changes will impact the percentages of recommended daily allowances of vitamin D and calcium listed on food packages, as well as the composition of school-lunch menus and other federal nutrition programs
The panel dismissed concerns that many Americans and Canadians are vitamin D deficient, noting that there is no scientifically validated level that's considered optimum. Even so, the panel concluded that for 97% of the population, a blood level of 20 nanograms of vitamin D per milliliter is sufficient.
Some vitamin D advocates took particular issue with that assumption. Several major medical groups, including the Endocrine Society and the International Osteoporsis Foundation, have concluded that a level of 30 ng/ml is necessary for optimal bone health.
"Randomized clinical trials have shown that in men and women 60 and older, you see fewer falls and fractures at the 30 ng/ml level," said Bess Dawson-Hughes, endocrinologist and director of the Bone Metabolism Laboratory at Tufts University. She also noted that while healthy people may reach that level taking 800 IUs per day, those who don't go outside, who use sunscreen religiously, have very dark skin or are taking some medications will need more.
Studies have also shown that at levels below 30 ng/ml, the body seeks calcium for everyday needs by leaching it from bones.
Dr. Brannon said the panel found such a wide range of blood levels considered optimal in various studies that it could not settle on a single threshold level. "I think the confusion is understandable. The committee is very concerned about the lack of evidence-based consensus guidelines for interpreting blood levels for vitamin D," said Dr. Brannon. "We strongly recommend that these be developed."
The panel was also concerned about what she called "emerging evidence of concern" about possible ill effects of too much vitamin D. Besides a risk of kidney and heart damage noted with vitamin D levels of 10,000 IUs per day, Dr. Brannon said the panel had seen higher death rates from pancreatic cancer, prostate cancer and other causes in men whose blood levels were above 50 ng/ml. The link is still tentative and may never be proven, she noted: "The difficulty is, you can't design a trial to look at adverse effects."
Other vitamin D advocates had guarded praise for the recommendations. "At least they recognized that there was a need to raise the daily intake level. That's a very important message," said Michael Holick, a professor of medicine at Boston University School of Medicine who testified before the committee in April.
He said that despite the paucity of randomized-controlled trials, the long list of chronic diseases associated with vitamin D does make sense, given that it is actually a hormone that affects virtually every organ in the human body and regulates as many as 2,000 genes.
For his part, Dr. Holick recommends that adults take 2,000 to 3,000 IUs per day—and notes that he had done studies giving subjects 50,000 IUs twice a month for six years and seen no harmful effects. "There is no downside to increasing your vitamin D intake, and there are more studies coming out almost on a weekly basis," he said.
One in particular may help settle whether vitamin D has long-term benefits beyond bone health: The National Institutes of Health has begun recruiting 20,000 men and women over age 60 for a nationwide clinical trial to study whether taking 2,000 IUs of vitamin D, or omega-3 fatty acids from fish oil, is any better than a placebo at lowering the risk of heart disease, cancer than other diseases.
In the meantime, some doctors say the IOM recommendations will not change their belief in testing patients' vitamin D levels and supplementing them as needed.
"I supplement patients who are deficient and they feel better. They come in and say, 'I've been much less achy and stiff or my mood's been better since I've been taking the vitamin D,' said Alan Pocinki, an internist in Washington D.C. Most of his patients are office workers, and 75% of them are below the 30 ng/ml level he considers necessary.
"Do we have the data to prove this conclusively? No. We don't have evidence for much of what we do in medicine, but if you wait for the evidence, you may be depriving your patients of beneficial treatments," Dr. Pocinki said.
Melinda Beck : WSJ : November 30, 2010
A long-awaited report from the Institute of Medicine to be released Tuesday triples the recommended amount of vitamin D most Americans should take every day to 600 international units from 200 IUs set in 1997.
That's far lower than many doctors and major medical groups have been advocating—and it could dampen some of the enthusiasm that's been building for the sunshine vitamin in recent years.
Many doctors have added blood tests of vitamin D levels to annual physicals, and sales of vitamin D supplements have soared to $425 million last year from $40 million in 2001, according to the Nutrition Business Journal.
The IOM panel also issued new recommendations for daily calcium intake, up to 1,200 milligrams for women 51 and older.
Who Needs Extra D?
Some people are at high risk for vitamin D deficiency, and experts believe they may benefit from more vitamin D than the new recommendations:
- People age 50 and older: This group is at increased risk for Vitamin D insufficiency. As people age, their skin is less efficient in synthesizing the vitamin and the kidney is less able to convert it to its active hormone form.
- People with osteoporosis: Vitamin D is crucial for building and maintaining strong bones.
- People with limited sun exposure: This population includes the homebound, those living in northern latitudes and individuals who wear long robes and head coverings.
- People with dark skin: Greater amounts of the pigment melanin result in darker skin and reduce the skin's ability to produce vitamin D from sunlight. People who have immigrated from sunnier climates may find their levels dropping sharply in latitudes where the sun's rays aren't as strong much of the year.
- People with fat malabsorption: Vitamin D requires some dietary fat in the gut for absorption. Individuals who have a reduced ability to absorb dietary fat might require supplements. Fat malabsorption is associated with conditions including pancreatic enzyme deficiency, Crohn's disease, cystic fibrosis, celiac disease, surgical removal of part of the stomach or intestines and some forms of liver disease.
- People taking certain medications: Prednisone and anti-seizure drugs can cause vitamin D to be absorbed and metabolized more quickly, reducing available blood levels.
- People who are obese: Individuals with a body mass index equal to or greater than 30 typically have a low concentration of the vitamin in the blood.
It's long been known that vitamin D is essential to maintaining strong bones. But hundreds of new studies have also linked low vitamin D levels to a higher risk of a slew of chronic health problems—heart disease, stroke, diabetes, prostate, breast and colon cancers, auto-immune diseases, infections, depression and cognitive decline. Studies have also suggested that many Americans are vitamin D deficient due to working and playing indoors and slathering on sunscreen.
The Institute of Medicine, an arm of the National Academy of Sciences that sets governmental nutrient levels, said there wasn't enough evidence to prove that low vitamin D causes such chronic diseases; it based its new recommendations on the levels needed to maintain strong bones alone.
"The evidence for bone health is compelling, consistent and gives strong evidence of cause and effect," said Patsy Brannon, a professor of nutritional sciences at Cornell University and member of the IOM panel. For the other health problems, she said, "there are relatively few randomized controlled trials, and even in the observational studies, the effects are inconsistent."
The new recommendations, which cover the U.S. and Canada, call for 600 IUs daily for infants through adults age 70 and 800 IUs after age 71. The IOM assumed that most people are getting minimal sun exposure, given rising concern over skin cancer and latitudes where the sun is too weak to create vitamin D on the skin much of the year. The panel also raised the acceptable upper limit of daily intake to 4,000 IUs for adults, from 2,000 previously.
Those levels do take into account vitamin D from food sources—but only a few, such as salmon and mackerel, contain much naturally. Milk fortified with vitamin D contains about 40 IUs per cup. Most Americans and Canadians need to get much of their vitamin D from supplements.
The IOM panel also issued new recommendations for daily calcium intake— ranging from 700 milligrams for children aged 1 to 3 up to 1,200 milligrams for women 51 and older. The main change from the 1997 recommendations was to lower the recommended level for men 50 to 70 to 1,000 from 1,200. The panel noted that teenage girls may not get enough calcium, and that postmenopausal women may get too much, running the risk of kidney stones.
The changes will impact the percentages of recommended daily allowances of vitamin D and calcium listed on food packages, as well as the composition of school-lunch menus and other federal nutrition programs
The panel dismissed concerns that many Americans and Canadians are vitamin D deficient, noting that there is no scientifically validated level that's considered optimum. Even so, the panel concluded that for 97% of the population, a blood level of 20 nanograms of vitamin D per milliliter is sufficient.
Some vitamin D advocates took particular issue with that assumption. Several major medical groups, including the Endocrine Society and the International Osteoporsis Foundation, have concluded that a level of 30 ng/ml is necessary for optimal bone health.
"Randomized clinical trials have shown that in men and women 60 and older, you see fewer falls and fractures at the 30 ng/ml level," said Bess Dawson-Hughes, endocrinologist and director of the Bone Metabolism Laboratory at Tufts University. She also noted that while healthy people may reach that level taking 800 IUs per day, those who don't go outside, who use sunscreen religiously, have very dark skin or are taking some medications will need more.
Studies have also shown that at levels below 30 ng/ml, the body seeks calcium for everyday needs by leaching it from bones.
Dr. Brannon said the panel found such a wide range of blood levels considered optimal in various studies that it could not settle on a single threshold level. "I think the confusion is understandable. The committee is very concerned about the lack of evidence-based consensus guidelines for interpreting blood levels for vitamin D," said Dr. Brannon. "We strongly recommend that these be developed."
The panel was also concerned about what she called "emerging evidence of concern" about possible ill effects of too much vitamin D. Besides a risk of kidney and heart damage noted with vitamin D levels of 10,000 IUs per day, Dr. Brannon said the panel had seen higher death rates from pancreatic cancer, prostate cancer and other causes in men whose blood levels were above 50 ng/ml. The link is still tentative and may never be proven, she noted: "The difficulty is, you can't design a trial to look at adverse effects."
Other vitamin D advocates had guarded praise for the recommendations. "At least they recognized that there was a need to raise the daily intake level. That's a very important message," said Michael Holick, a professor of medicine at Boston University School of Medicine who testified before the committee in April.
He said that despite the paucity of randomized-controlled trials, the long list of chronic diseases associated with vitamin D does make sense, given that it is actually a hormone that affects virtually every organ in the human body and regulates as many as 2,000 genes.
For his part, Dr. Holick recommends that adults take 2,000 to 3,000 IUs per day—and notes that he had done studies giving subjects 50,000 IUs twice a month for six years and seen no harmful effects. "There is no downside to increasing your vitamin D intake, and there are more studies coming out almost on a weekly basis," he said.
One in particular may help settle whether vitamin D has long-term benefits beyond bone health: The National Institutes of Health has begun recruiting 20,000 men and women over age 60 for a nationwide clinical trial to study whether taking 2,000 IUs of vitamin D, or omega-3 fatty acids from fish oil, is any better than a placebo at lowering the risk of heart disease, cancer than other diseases.
In the meantime, some doctors say the IOM recommendations will not change their belief in testing patients' vitamin D levels and supplementing them as needed.
"I supplement patients who are deficient and they feel better. They come in and say, 'I've been much less achy and stiff or my mood's been better since I've been taking the vitamin D,' said Alan Pocinki, an internist in Washington D.C. Most of his patients are office workers, and 75% of them are below the 30 ng/ml level he considers necessary.
"Do we have the data to prove this conclusively? No. We don't have evidence for much of what we do in medicine, but if you wait for the evidence, you may be depriving your patients of beneficial treatments," Dr. Pocinki said.
Can Vitamin D Improve Your Athletic Performance?
Gretchen Reynolds : NY Times : September 23, 2009
When scientists at the Australian Institute of Sport recently decided to check the Vitamin D status of some of that country’s elite female gymnasts, their findings were fairly alarming. Of the 18 gymnasts tested, 15 had levels that were “below current recommended guidelines for optimal bone health,” the study’s authors report. Six of these had Vitamin D levels that would qualify as medically deficient. Unlike other nutrients, Vitamin D can be obtained by exposure to ultraviolet radiation from sunlight, as well as through foods or supplements. Of course, female gymnasts are a unique and specialized bunch, not known for the quality or quantity of their diets, or for getting outside much.
But in another study presented at a conference earlier this year, researchers found that many of a group of distance runners also had poor Vitamin D status. Forty percent of the runners, who trained outdoors in sunny Baton Rouge, Louisiana, had insufficient Vitamin D. “It was something of a surprise,” says D. Enette Larson-Meyer, an assistant professor in the Department of Family and Consumer Sciences at the University of Wyoming and one of the authors of the study.
Vitamin D is an often overlooked element in athletic achievement, a “sleeper nutrient,” says John Anderson, a professor emeritus of nutrition at the University of North Carolina and one of the authors of a review article published online in May about Vitamin D and athletic performance. Vitamin D once was thought to be primarily involved in bone development. But a growing body of research suggests that it’s vital in multiple different bodily functions, including allowing body cells to utilize calcium (which is essential for cell metabolism), muscle fibers to develop and grow normally, and the immune system to function properly. “Almost every cell in the body has receptors” for Vitamin D, Anderson says. “It can up-regulate and down-regulate hundreds, maybe even thousands of genes,” Larson-Meyer says. “We’re only at the start of understanding how important it is.”
But many of us, it seems, no matter how active and scrupulous we are about health, don’t get enough Vitamin D. Nowadays, “many people aren’t going outside very much,” Johnson says, and most of us
assiduously apply sunscreen and take other precautions when we do. The Baton Rouge runners, for instance, most likely “ran early in the morning or late in the day,” Larson-Meyer says, reducing their chances of heat stroke or sunburn, but also reducing their exposure to sunlight.
Meanwhile, dietary sources of Vitamin D are meager. Cod-liver oil provides a whopping dose. But a glass of fortified milk provides a fraction of what scientists now think we need per day. (A major study published online in the journal Pediatrics last month concluded that more than 60 percent of American children, or almost 51 million kids, have “insufficient” levels of Vitamin D and another 9 percent, or 7.6 million children, are clinically “deficient,” a serious condition. Cases of childhood rickets, a bone disease caused by lack of Vitamin D, have been rising in the U.S. in recent years.)
Although few studies have looked closely at the issue of Vitamin D and athletic performance, those that have are suggestive. A series of strange but evocative studies undertaken decades ago in Russia and Germany, for instance, hint that the Eastern Bloc nations may have depended in part on sunlamps and Vitamin D to produce their preternaturally well-muscled and world-beating athletes. In one of the studies, four Russian sprinters were doused with artificial, ultraviolet light. Another group wasn’t. Both trained identically for the 100-meter dash. The control group lowered their sprint times by 1.7 percent. The radiated runners, in comparison, improved by an impressive 7.4 percent.
More recently, when researchers tested the vertical jumping ability of a small group of adolescent athletes, Larson-Meyer says, “they found that those who had the lowest levels of Vitamin D tended not to jump as high,” intimating that too little of the nutrient may impair muscle power. Low levels might also contribute to sports injuries, in part because Vitamin D is so important for bone and muscle health. In a Creighton University study of female naval recruits, stress fractures were reduced significantly after the women started taking supplements of Vitamin D and calcium.
A number of recent studies also have shown that, among athletes who train outside year-round, maximal oxygen intake tends to be highest in late summer, Johnson says. The athletes, in other words, are fittest in August, when ultraviolet radiation from the sun is near its zenith. They often then experience an abrupt drop in maximal oxygen intake,
beginning as early as September, even thought they continue to train just as hard. This decline coincides with the autumnal lengthening of the angle of sunlight. Less ultraviolet radiation reaches the earth and, apparently, sports performance suffers.
Concerned now about your Vitamin D status? You can learn your status with a simple blood test. An at-home version is available through the Web site of the Vitamin D Council. (Use of the tests is restricted in some states, including New York. See the website for details.) Be sure that any test checks the level of 25(OH)D in your blood. This level “should generally be above 50 nanograms per milliliter,” Larson-Meyer says.
If your levels are low, talk to your doctor about the best response. Sunlight is one easy, if controversial, fix. “Most dermatologists will still tell you that no amount of sun exposure is safe,” Johnson says.
But Larson-Meyer and other Vitamin D researchers aren’t so sure. “There’s no good, scientific evidence that five to thirty minutes of sunlight a few times a week is harmful,” she says.
Or try supplements. “1,000 IU a day and much more for people who are deficient” is probably close to ideal, Larson-Meyer says. This, by the way, is about double the current recommended daily allowance. Most experts anticipate that this allowance will be revised upward soon. Consult with your doctor before beginning supplements. Overdoses of Vitamin D are rare, but can occur.
Finally, stay tuned. “In the next few years, we’re going to be learning much more” about the role of vitamin D in bodily function and sports performance, Larson-Meyer says.