- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
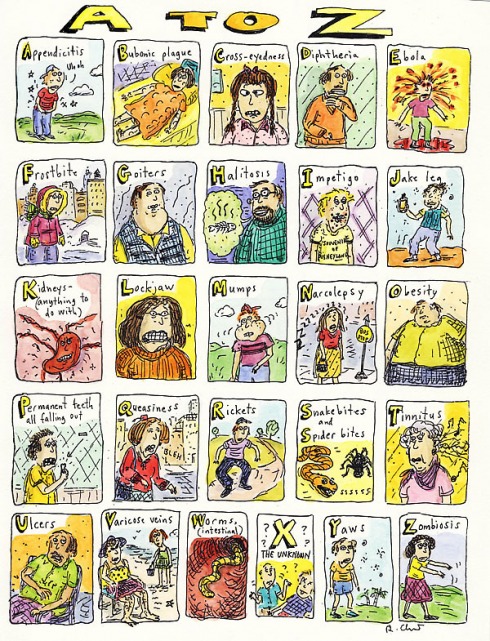
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Sleep
To Rest Easy, Forget the Sheep
Scientists know that many people inadvertently undermine their ability to fall asleep and stay asleep for a full night. Here are some frequent suggestions:
1. Establish a regular sleep schedule and try to stick to it, even on weekends.
2. If you nap during the day, limit it to 20 or 30 minutes, preferably early in the afternoon.
3. Avoid alcohol in the evening, as it can disrupt sleep.
4. Don’t eat a big meal just before bedtime, but don’t go to bed hungry, either. Eat a light snack before bed, if needed, preferably one high in carbohydrates.
5. If you use medications that are stimulants, take them in the morning, or ask your doctor if you can switch to a nonstimulating alternative. If you use drugs that cause drowsiness, take them in the evening.
6. Get regular exercise during the day, but avoid vigorous exercise within three hours of bedtime.
7. If pressing thoughts interfere with falling asleep, write them down (keep a pad and pen next to the bed) and try to forget about them until morning.
8. If you are frequently awakened by a need to use the bathroom, cut down on how much you drink late in the day.
9. If you smoke, quit. Among other hazards, nicotine is a stimulant and can cause nightmares.
10. Avoid beverages and foods containing caffeine after 3 p.m. Even decaf versions have some caffeine, which can bother some people.
Cheating Ourselves of Sleep
By Jane E. Brody : NY Times : June 17, 2013
Think you do just fine on five or six hours of shut-eye? Chances are, you are among the many millions who unwittingly shortchange themselves on sleep.
Research shows that most people require seven or eight hours of sleep to function optimally. Failing to get enough sleep night after night can compromise your health and may even shorten your life. From infancy to old age, the effects of inadequate sleep can profoundly affect memory, learning, creativity, productivity and emotional stability, as well as your physical health.
According to sleep specialists at the University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic, among others, a number of bodily systems are negatively affected by inadequate sleep: the heart, lungs and kidneys; appetite, metabolism and weight control; immune function and disease resistance; sensitivity to pain; reaction time; mood; and brain function.
Poor sleep is also a risk factor for depression and substance abuse, especially among people with post-traumatic stress disorder, according to Anne Germain, associate professor of psychiatry at the University of Pittsburgh. People with PTSD tend to relive their trauma when they try to sleep, which keeps their brains in a heightened state of alertness.
Dr. Germain is studying what happens in the brains of sleeping veterans with PTSD in hopes of developing more effective treatments for them and for people with lesser degrees of stress that interfere with a good night’s sleep.
The elderly are especially vulnerable. Timothy H. Monk, who directs the Human Chronobiology Research Program at Western Psychiatric, heads a five-year federally funded study of circadian rhythms, sleep strength, stress reactivity, brain function and genetics among the elderly. “The circadian signal isn’t as strong as people get older,” he said.
He is finding that many are helped by standard behavioral treatments for insomnia, like maintaining a regular sleep schedule, avoiding late-in-day naps and caffeine, and reducing distractions from light, noise and pets.
It should come as no surprise that myriad bodily systems can be harmed by chronically shortened nights. “Sleep affects almost every tissue in our bodies,” said Dr. Michael J. Twery, a sleep specialist at the National Institutes of Health.
Several studies have linked insufficient sleep to weight gain. Not only do night owls with shortchanged sleep have more time to eat, drink and snack, but levels of the hormone leptin, which tells the brain enough food has been consumed, are lower in the sleep-deprived while levels of ghrelin, which stimulates appetite, are higher.
In addition, metabolism slows when one’s circadian rhythm and sleep are disrupted; if not counteracted by increased exercise or reduced caloric intake, this slowdown could add up to 10 extra pounds in a year.
The body’s ability to process glucose is also adversely affected, which may ultimately result in Type 2 diabetes. In one study, healthy young men prevented from sleeping more than four hours a night for six nights in a row ended up with insulin and blood sugar levels like those of people deemed prediabetic. The risks of cardiovascular diseases and stroke are higher in people who sleep less than six hours a night. Even a single night of inadequate sleep can cause daylong elevations in blood pressure in people with hypertension. Inadequate sleep is also associated with calcification of coronary arteries and raised levels of inflammatory factors linked to heart disease. (In terms of cardiovascular disease, sleeping too much may also be risky. Higher rates of heart disease have been found among women who sleep more than nine hours nightly.)
The risk of cancer may also be elevated in people who fail to get enough sleep. A Japanese study of nearly 24,000 women ages 40 to 79 found that those who slept less than six hours a night were more likely to develop breast cancer than women who slept longer. The increased risk may result from diminished secretion of the sleep hormone melatonin. Among participants in the Nurses Health Study, Eva S. Schernhammer of Harvard Medical School found a link between low melatonin levels and an increased risk of breast cancer.
A study of 1,240 people by researchers at Case Western Reserve University in Cleveland found an increased risk of potentially cancerous colorectal polyps in those who slept fewer than six hours nightly.
Children can also experience hormonal disruptions from inadequate sleep. Growth hormone is released during deep sleep; it not only stimulates growth in children, but also boosts muscle mass and repairs damaged cells and tissues in both children and adults.
Dr. Vatsal G. Thakkar, a psychiatrist affiliated with New York University, recently described evidence associating inadequate sleep with an erroneous diagnosis of attention deficit hyperactivity disorder in children. In one study, 28 percent of children with sleep problems had symptoms of the disorder, but not the disorder.
During sleep, the body produces cytokines, cellular hormones that help fight infections. Thus, short sleepers may be more susceptible to everyday infections like colds and flu. In a study of 153 healthy men and women, Sheldon Cohen and colleagues at Carnegie Mellon University found that those who slept less than seven hours a night were three times as likely to develop cold symptoms when exposed to a cold-causing virus than were people who slept eight or more hours.
Some of the most insidious effects of too little sleep involve mental processes like learning, memory, judgment and problem-solving. During sleep, new learning and memory pathways become encoded in the brain, and adequate sleep is necessary for those pathways to work optimally. People who are well rested are better able to learn a task and more likely to remember what they learned. The cognitive decline that so often accompanies aging may in part result from chronically poor sleep.
With insufficient sleep, thinking slows, it is harder to focus and pay attention, and people are more likely to make poor decisions and take undue risks. As you might guess, these effects can be disastrous when operating a motor vehicle or dangerous machine.
In driving tests, sleep-deprived people perform as if drunk, and no amount of caffeine or cold air can negate the ill effects.
At your next health checkup, tell your doctor how long and how well you sleep. Be honest: Sleep duration and quality can be as important to your health as your blood pressure and cholesterol level.
This is the first of two columns on inadequate sleep.
Why We Need Our Sleep
By Robert Lee Hotz : WSJ Article : January 18, 2008
People have been trying to figure out why we sleep for almost as long as we have been conscious of being awake, tossing and turning in the dark.
After a few restless nights, most of us can't even think straight. We are less able to make sense of problems, make competent moral judgments or retain what we learn, even though studies show our brain cells fire more frenetically to overcome the lack of sleep. Lose too much sleep and we become reckless, emotionally fragile and more vulnerable to infections as well as diabetes, heart disease and obesity, recent research suggests.
Yet scientists probing the purpose of sleep are still largely in the dark. "Why we sleep at all is a strange bastion of the unknown," said sleep psychologist Matthew Walker at the University of California in Berkeley.
One vital function of sleep, researchers argue, may be to help our brains sort, store and consolidate new memories, etching experiences more indelibly into the brain's biochemical archives.
.
Even a 90-minute nap can significantly improve our ability to master new motor skills and strengthen our memories of what we learn, researchers at the University of Haifa in Israel reported last month in Nature Neuroscience. "Napping is as effective as a night's sleep," said psychologist Sara Mednick at the University of California in San Diego.
Moreover, slumber seems to boost our ability to make sense of new knowledge by allowing the brain to detect connections between things we learn.
In research published in April in the Proceedings of the National Academy of Sciences, Dr. Walker and his collaborators at the Harvard Medical School tested 56 college students and found that their ability to discern the big picture in disparate pieces of information improved measurably after the brain could, during a night's sleep, mull things over.
It is these patterns of meaning -- the distilled essence of knowledge -- that we remember so well. "Sleep helps stabilize memory," said neurologist Jeffrey Ellenbogen, director of the sleep-medicine program at Massachusetts General Hospital.
The erratic biorhythms of sleep and behavior are intertwined everywhere in nature. Socially active fruit flies need more sleep than loner flies, and even zebra fish can get insomnia.
Sleep is controlled partly by our genes. The difference between those of us who naturally wake at dawn and night owls who are wide-eyed at midnight may be partly due to variations in a gene, named Period3, that affects our biological clock. Variations in that gene also make some people especially sensitive to sleep deprivation, scientists at the U.K.'s University of Surrey recently reported.
For many of us, though, sleeplessness is a self-inflicted epidemic in which lifestyle overrides basic biology. "In this odd, Western 24-hour-MTV-fast-food generation we have created, we all feel the need to achieve more and more. The one thing that takes a hit is sleep," Dr. Walker said. On average, most people sleep 75 minutes less each night than people did a century ago, sleep surveys record.
Yet, rarely have so many millions of drowsy people been trying so hard to secure some shut-eye, spending billions on sleep aids. By one estimate, in the U.S. alone, pharmacists filled 49 million prescriptions for sleep drugs last year. Even so, we think we sleep more than we actually do, according to Arizona State University scientists. They recorded how long 2,100 volunteers actually slept each night and compared that to how long the people reported they had slept. Most people overestimated their sleep by about 18 minutes, the scientists found.
The consequences of too little sleep can be dire. Almost half of all heavy-truck accidents in the U.S. can be traced to driver fatigue, while decisions leading to the Challenger space-shuttle disaster, the Chernobyl nuclear-reactor meltdown and the Exxon Valdez oil spill can be partly linked to people drained of rest by round-the-clock work schedules. Weary doctors make more serious medical errors, while sleepy airport baggage screeners make more security mistakes, researchers reported at the Associated Professional Sleep Societies.
All told, the frayed tempers, short attention spans and fuzzy thinking caused by sleep deprivation may cost $15 billion a year in reduced productivity, the National Commission on Sleep Disorders Research estimated.
The expectation of a nap, however, is by itself enough to measurably lower our blood pressure, researchers at the Liverpool John Moores University in England reported in October in the Journal of Applied Physiology.
Indeed, regular nappers -- working men who took a siesta for 30 minutes or more at least three times a week -- had a 64% lower risk of heart-related death, researchers at the University of Athens reported last February in the Archives of Internal Medicine.
"All of the things we are proving about sleep and the brain are things that your mother already knew decades ago," Dr. Walker said. "We are putting the science and the hard facts behind it."
A Good Night’s Sleep Isn’t a Luxury; It’s a Necessity
By Jane E. Brody : NY Times : May 30, 2011
In my younger years, I regarded sleep as a necessary evil, nature’s way of thwarting my desire to cram as many activities into a 24-hour day as possible. I frequently flew the red-eye from California, for instance, sailing (or so I thought) through the next day on less than four hours of uncomfortable sleep.
But my neglect was costing me in ways that I did not fully appreciate. My husband called our nights at the ballet and theater “Jane’s most expensive naps.” Eventually we relinquished our subscriptions. Driving, too, was dicey: twice I fell asleep at the wheel, narrowly avoiding disaster. I realize now that I was living in a state of chronic sleep deprivation.
I don’t want to nod off during cultural events, and I no longer have my husband to spell me at the wheel. I also don’t want to compromise my ability to think and react. As research cited recently in this newspaper’s magazine found, “The sleep-deprived among us are lousy judges of our own sleep needs. We are not nearly as sharp as we think we are.”
Studies have shown that people function best after seven to eight hours of sleep, so I now aim for a solid seven hours, the amount associated with the lowest mortality rate. Yet on most nights something seems to interfere, keeping me up later than my intended lights-out at 10 p.m. — an essential household task, an e-mail requiring an urgent and thoughtful response, a condolence letter I never found time to write during the day, a long article that I must read.
It’s always something.
What’s Keeping Us Up?
I know I’m hardly alone. Between 1960 and 2010, the average night’s sleep for adults in the United States dropped to six and a half hours from more than eight. Some experts predict a continuing decline, thanks to distractions like e-mail, instant and text messaging, and online shopping.
Age can have a detrimental effect on sleep. In a 2005 national telephone survey of 1,003 adults ages 50 and older, the Gallup Organization found that a mere third of older adults got a good night’s sleep every day, fewer than half slept more than seven hours, and one-fifth slept less than six hours a night.
With advancing age, natural changes in sleep quality occur. People may take longer to fall asleep, and they tend to get sleepy earlier in the evening and to awaken earlier in the morning. More time is spent in the lighter stages of sleep and less in restorative deep sleep. R.E.M. sleep, during which the mind processes emotions and memories and relieves stress, also declines with age.
Habits that ruin sleep often accompany aging: less physical activity, less time spent outdoors (sunlight is the body’s main regulator of sleepiness and wakefulness), poorer attention to diet, taking medications that can disrupt sleep, caring for a chronically ill spouse, having a partner who snores. Some use alcohol in hopes of inducing sleep; in fact, it disrupts sleep.
Add to this list a host of sleep-robbing health issues, like painful arthritis, diabetes, depression, anxiety, sleep apnea, hot flashes in women and prostate enlargement in men. In the last years of his life, my husband was plagued with restless leg syndrome, forcing him to get up and walk around in the middle of the night until the symptoms subsided. During a recent night, I was awake for hours with leg cramps that simply wouldn’t quit.
Beauty Rest and Beyond
A good night’s sleep is much more than a luxury. Its benefits include improvements in concentration, short-term memory, productivity, mood, sensitivity to pain and immune function.
If you care about how you look, more sleep can even make you appear more attractive. In a study published online in December in the journal BMJ, researchers in Sweden and the Netherlands reported that 23 sleep-deprived adults seemed to untrained observers to be less healthy, more tired and less attractive than they appeared to be after a full night’s sleep.
Perhaps more important, losing sleep may make you fat — or at least, fatter than you would otherwise be. In a study by Harvard researchers involving 68,000 middle-aged women followed for 16 years, those who slept five hours or less each night were found to weigh 5.4 pounds more — and were 15 percent more likely to become obese — than the women who slept seven hours nightly.
Michael Breus, a clinical psychologist and sleep specialist in Scottsdale, Ariz., and author of “The Sleep Doctor’s Diet Plan,” points out that as the average length of sleep has declined in the United States, the average weight of Americans has increased.
There are plausible reasons to think this is a cause-and-effect relationship. At least two factors may be involved: more waking hours in homes brimming with food and snacks; and possible changes in the hormones leptin and ghrelin, which regulate appetite.
In a study published in 2009 in The American Journal of Clinical Nutrition, Dr. Plamen D. Penev, an endocrinologist at the University of Chicago, and co-authors explored calorie consumption and expenditure by 11 healthy volunteers who spent two 14-day stays in a sleep laboratory. Both sessions offered unlimited access to tasty foods. During one stay, the volunteers — five women and six men — were limited to 5.5 hours of sleep a night, and during the other they got 8.5 hours of sleep.
Although the subjects ate the same amount of food at meals, during the shortened nights they consumed an average of 221 more calories from snacks than they did when they were getting more sleep. The snacks they ate tended to be high in carbohydrates, and the subjects expended no more energy than they did on the longer nights. In just two weeks, the extra nighttime snacking could add nearly a pound to body weight, the scientists concluded.
These researchers found no significant changes in the participants’ blood levels of the hormones leptin and ghrelin, but others have found that short sleepers have lower levels of appetite-suppressing leptin and higher levels of ghrelin, which prompts an increase in calorie intake.
Sleep loss may also affect the function of a group of neurons in the hypothalamus of the brain, where another hormone, orexin, is involved in the regulation of feeding behavior.
The bottom line: Resist the temptation to squeeze one more thing into the end of your day. If health problems disrupt your sleep, seek treatment that can lessen their effect. If you have trouble falling asleep or often awaken during the night and can’t get back to sleep, you could try taking supplements of melatonin, the body’s natural sleep inducer. I keep it at my bedside.
If you have trouble sleeping, the tips accompanying this article may help. And if all else fails, try to take a nap during the day. Naps can enhance brain function, energy, mood and productivity.
Brain Basics:
Understanding Sleep
Do you ever feel sleepy or "zone out" during the day? Do you find it hard to wake up on Monday mornings? If so, you are familiar with the powerful need for sleep. However, you may not realize that sleep is as essential for your well-being as food and water.
Until the 1950s, most people thought of sleep as a passive, dormant part of our daily lives. We now know that our brains are very active during sleep. Moreover, sleep affects our daily functioning and our physical and mental health in many ways that we are just beginning to understand.
Nerve-signaling chemicals called neurotransmitters control whether we are asleep or awake by acting on different groups of nerve cells, or neurons, in the brain. Neurons in the brainstem, which connects the brain with the spinal cord, produce neurotransmitters such as serotonin and norepinephrine that keep some parts of the brain active while we are awake. Other neurons at the base of the brain begin signaling when we fall asleep. These neurons appear to "switch off" the signals that keep us awake. Research also suggests that a chemical called adenosine builds up in our blood while we are awake and causes drowsiness. This chemical gradually breaks down while we sleep.
During sleep, we usually pass through five phases of sleep: stages 1, 2, 3, 4, and REM (rapid eye movement) sleep. These stages progress in a cycle from stage 1 to REM sleep, then the cycle starts over again with stage 1 (see figure 1 ). We spend almost 50 percent of our total sleep time in stage 2 sleep, about 20 percent in REM sleep, and the remaining 30 percent in the other stages. Infants, by contrast, spend about half of their sleep time in REM sleep.
During stage 1, which is light sleep, we drift in and out of sleep and can be awakened easily. Our eyes move very slowly and muscle activity slows. People awakened from stage 1 sleep often remember fragmented visual images. Many also experience sudden muscle contractions called hypnic myoclonia, often preceded by a sensation of starting to fall. These sudden movements are similar to the "jump" we make when startled. When we enter stage 2 sleep, our eye movements stop and our brain waves (fluctuations of electrical activity that can be measured by electrodes) become slower, with occasional bursts of rapid waves called sleep spindles. In stage 3, extremely slow brain waves called delta waves begin to appear, interspersed with smaller, faster waves. By stage 4, the brain produces delta waves almost exclusively. It is very difficult to wake someone during stages 3 and 4, which together are called deep sleep. There is no eye movement or muscle activity. People awakened during deep sleep do not adjust immediately and often feel groggy and disoriented for several minutes after they wake up. Some children experience bedwetting, night terrors, or sleepwalking during deep sleep.
When we switch into REM sleep, our breathing becomes more rapid, irregular, and shallow, our eyes jerk rapidly in various directions, and our limb muscles become temporarily paralyzed. Our heart rate increases, our blood pressure rises, and males develop penile erections. When people awaken during REM sleep, they often describe bizarre and illogical tales – dreams.
The first REM sleep period usually occurs about 70 to 90 minutes after we fall asleep. A complete sleep cycle takes 90 to 110 minutes on average. The first sleep cycles each night contain relatively short REM periods and long periods of deep sleep. As the night progresses, REM sleep periods increase in length while deep sleep decreases. By morning, people spend nearly all their sleep time in stages 1, 2, and REM.
People awakened after sleeping more than a few minutes are usually unable to recall the last few minutes before they fell asleep. This sleep-related form of amnesia is the reason people often forget telephone calls or conversations they've had in the middle of the night. It also explains why we often do not remember our alarms ringing in the morning if we go right back to sleep after turning them off.
Since sleep and wakefulness are influenced by different neurotransmitter signals in the brain, foods and medicines that change the balance of these signals affect whether we feel alert or drowsy and how well we sleep. Caffeinated drinks such as coffee and drugs such as diet pills and decongestants stimulate some parts of the brain and can cause insomnia, or an inability to sleep. Many antidepressants suppress REM sleep. Heavy smokers often sleep very lightly and have reduced amounts of REM sleep. They also tend to wake up after 3 or 4 hours of sleep due to nicotine withdrawal. Many people who suffer from insomnia try to solve the problem with alcohol – the so-called night cap. While alcohol does help people fall into light sleep, it also robs them of REM and the deeper, more restorative stages of sleep. Instead, it keeps them in the lighter stages of sleep, from which they can be awakened easily.
People lose some of the ability to regulate their body temperature during REM, so abnormally hot or cold temperatures in the environment can disrupt this stage of sleep. If our REM sleep is disrupted one night, our bodies don't follow the normal sleep cycle progression the next time we doze off. Instead, we often slip directly into REM sleep and go through extended periods of REM until we "catch up" on this stage of sleep.
People who are under anesthesia or in a coma are often said to be asleep. However, people in these conditions cannot be awakened and do not produce the complex, active brain wave patterns seen in normal sleep. Instead, their brain waves are very slow and weak, sometimes all but undetectable.
How Much Sleep Do We Need?
The amount of sleep each person needs depends on many factors, including age. Infants generally require about 16 hours a day, while teenagers need about 9 hours on average. For most adults, 7 to 8 hours a night appears to be the best amount of sleep, although some people may need as few as 5 hours or as many as 10 hours of sleep each day. Women in the first 3 months of pregnancy often need several more hours of sleep than usual. The amount of sleep a person needs also increases if he or she has been deprived of sleep in previous days. Getting too little sleep creates a "sleep debt," which is much like being overdrawn at a bank. Eventually, your body will demand that the debt be repaid. We don't seem to adapt to getting less sleep than we need; while we may get used to a sleep-depriving schedule, our judgment, reaction time, and other functions are still impaired.
People tend to sleep more lightly and for shorter time spans as they get older, although they generally need about the same amount of sleep as they needed in early adulthood. About half of all people over 65 have frequent sleeping problems, such as insomnia, and deep sleep stages in many elderly people often become very short or stop completely. This change may be a normal part of aging, or it may result from medical problems that are common in elderly people and from the medications and other treatments for those problems.
Experts say that if you feel drowsy during the day, even during boring activities, you haven't had enough sleep. If you routinely fall asleep within 5 minutes of lying down, you probably have severe sleep deprivation, possibly even a sleep disorder. Microsleeps, or very brief episodes of sleep in an otherwise awake person, are another mark of sleep deprivation. In many cases, people are not aware that they are experiencing microsleeps. The widespread practice of "burning the candle at both ends" in western industrialized societies has created so much sleep deprivation that what is really abnormal sleepiness is now almost the norm.
Many studies make it clear that sleep deprivation is dangerous. Sleep-deprived people who are tested by using a driving simulator or by performing a hand-eye coordination task perform as badly as or worse than those who are intoxicated. Sleep deprivation also magnifies alcohol's effects on the body, so a fatigued person who drinks will become much more impaired than someone who is well-rested. Driver fatigue is responsible for an estimated 100,000 motor vehicle accidents and 1500 deaths each year, according to the National Highway Traffic Safety Administration. Since drowsiness is the brain's last step before falling asleep, driving while drowsy can – and often does – lead to disaster. Caffeine and other stimulants cannot overcome the effects of severe sleep deprivation. The National Sleep Foundation says that if you have trouble keeping your eyes focused, if you can't stop yawning, or if you can't remember driving the last few miles, you are probably too drowsy to drive safely.
What Does Sleep Do For Us?
Although scientists are still trying to learn exactly why people need sleep, animal studies show that sleep is necessary for survival. For example, while rats normally live for two to three years, those deprived of REM sleep survive only about 5 weeks on average, and rats deprived of all sleep stages live only about 3 weeks. Sleep-deprived rats also develop abnormally low body temperatures and sores on their tail and paws. The sores may develop because the rats' immune systems become impaired. Some studies suggest that sleep deprivation affects the immune system in detrimental ways.
Sleep appears necessary for our nervous systems to work properly. Too little sleep leaves us drowsy and unable to concentrate the next day. It also leads to impaired memory and physical performance and reduced ability to carry out math calculations. If sleep deprivation continues, hallucinations and mood swings may develop. Some experts believe sleep gives neurons used while we are awake a chance to shut down and repair themselves. Without sleep, neurons may become so depleted in energy or so polluted with byproducts of normal cellular activities that they begin to malfunction. Sleep also may give the brain a chance to exercise important neuronal connections that might otherwise deteriorate from lack of activity.
Deep sleep coincides with the release of growth hormone in children and young adults. Many of the body's cells also show increased production and reduced breakdown of proteins during deep sleep. Since proteins are the building blocks needed for cell growth and for repair of damage from factors like stress and ultraviolet rays, deep sleep may truly be "beauty sleep." Activity in parts of the brain that control emotions, decision-making processes, and social interactions is drastically reduced during deep sleep, suggesting that this type of sleep may help people maintain optimal emotional and social functioning while they are awake. A study in rats also showed that certain nerve-signaling patterns which the rats generated during the day were repeated during deep sleep. This pattern repetition may help encode memories and improve learning.
Dreaming and REM Sleep
We typically spend more than 2 hours each night dreaming. Scientists do not know much about how or why we dream. Sigmund Freud, who greatly influenced the field of psychology, believed dreaming was a "safety valve" for unconscious desires. Only after 1953, when researchers first described REM in sleeping infants, did scientists begin to carefully study sleep and dreaming. They soon realized that the strange, illogical experiences we call dreams almost always occur during REM sleep. While most mammals and birds show signs of REM sleep, reptiles and other cold-blooded animals do not.
REM sleep begins with signals from an area at the base of the brain called the pons (see figure 2 ). These signals travel to a brain region called the thalamus, which relays them to the cerebral cortex – the outer layer of the brain that is responsible for learning, thinking, and organizing information. The pons also sends signals that shut off neurons in the spinal cord, causing temporary paralysis of the limb muscles. If something interferes with this paralysis, people will begin to physically "act out" their dreams – a rare, dangerous problem called REM sleep behavior disorder. A person dreaming about a ball game, for example, may run headlong into furniture or blindly strike someone sleeping nearby while trying to catch a ball in the dream.
REM sleep stimulates the brain regions used in learning. This may be important for normal brain development during infancy, which would explain why infants spend much more time in REM sleep than adults (see Sleep: A Dynamic Activity ). Like deep sleep, REM sleep is associated with increased production of proteins. One study found that REM sleep affects learning of certain mental skills. People taught a skill and then deprived of non-REM sleep could recall what they had learned after sleeping, while people deprived of REM sleep could not.
Some scientists believe dreams are the cortex's attempt to find meaning in the random signals that it receives during REM sleep. The cortex is the part of the brain that interprets and organizes information from the environment during consciousness. It may be that, given random signals from the pons during REM sleep, the cortex tries to interpret these signals as well, creating a "story" out of fragmented brain activity.
Sleep and Circadian Rhythms
Circadian rhythms are regular changes in mental and physical characteristics that occur in the course of a day (circadian is Latin for "around a day"). Most circadian rhythms are controlled by the body's biological "clock." This clock, called the suprachiasmatic nucleus or SCN (see figure 2 ), is actually a pair of pinhead-sized brain structures that together contain about 20,000 neurons. The SCN rests in a part of the brain called the hypothalamus, just above the point where the optic nerves cross. Light that reaches photoreceptors in the retina (a tissue at the back of the eye) creates signals that travel along the optic nerve to the SCN.
Signals from the SCN travel to several brain regions, including the pineal gland, which responds to light-induced signals by switching off production of the hormone melatonin. The body's level of melatonin normally increases after darkness falls, making people feel drowsy. The SCN also governs functions that are synchronized with the sleep/wake cycle, including body temperature, hormone secretion, urine production, and changes in blood pressure.
By depriving people of light and other external time cues, scientists have learned that most people's biological clocks work on a 25-hour cycle rather than a 24-hour one. But because sunlight or other bright lights can reset the SCN, our biological cycles normally follow the 24-hour cycle of the sun, rather than our innate cycle. Circadian rhythms can be affected to some degree by almost any kind of external time cue, such as the beeping of your alarm clock, the clatter of a garbage truck, or the timing of your meals. Scientists call external time cues zeitgebers (German for "time givers").
When travelers pass from one time zone to another, they suffer from disrupted circadian rhythms, an uncomfortable feeling known as jet lag. For instance, if you travel from California to New York, you "lose" 3 hours according to your body's clock. You will feel tired when the alarm rings at 8 a.m. the next morning because, according to your body's clock, it is still 5 a.m. It usually takes several days for your body's cycles to adjust to the new time.
To reduce the effects of jet lag, some doctors try to manipulate the biological clock with a technique called light therapy. They expose people to special lights, many times brighter than ordinary household light, for several hours near the time the subjects want to wake up. This helps them reset their biological clocks and adjust to a new time zone.
Symptoms much like jet lag are common in people who work nights or who perform shift work. Because these people's work schedules are at odds with powerful sleep-regulating cues like sunlight, they often become uncontrollably drowsy during work, and they may suffer insomnia or other problems when they try to sleep. Shift workers have an increased risk of heart problems, digestive disturbances, and emotional and mental problems, all of which may be related to their sleeping problems. The number and severity of workplace accidents also tend to increase during the night shift. Major industrial accidents attributed partly to errors made by fatigued night-shift workers include the Exxon Valdez oil spill and the Three Mile Island and Chernobyl nuclear power plant accidents. One study also found that medical interns working on the night shift are twice as likely as others to misinterpret hospital test records, which could endanger their patients. It may be possible to reduce shift-related fatigue by using bright lights in the workplace, minimizing shift changes, and taking scheduled naps.
Many people with total blindness experience life-long sleeping problems because their retinas are unable to detect light. These people have a kind of permanent jet lag and periodic insomnia because their circadian rhythms follow their innate cycle rather than a 24-hour one. Daily supplements of melatonin may improve night-time sleep for such patients. However, since the high doses of melatonin found in most supplements can build up in the body, long-term use of this substance may create new problems. Because the potential side effects of melatonin supplements are still largely unknown, most experts discourage melatonin use by the general public.
Sleep and Disease
Sleep and sleep-related problems play a role in a large number of human disorders and affect almost every field of medicine. For example, problems like stroke and asthma attacks tend to occur more frequently during the night and early morning, perhaps due to changes in hormones, heart rate, and other characteristics associated with sleep. Sleep also affects some kinds of epilepsy in complex ways. REM sleep seems to help prevent seizures that begin in one part of the brain from spreading to other brain regions, while deep sleep may promote the spread of these seizures. Sleep deprivation also triggers seizures in people with some types of epilepsy.
Neurons that control sleep interact closely with the immune system. As anyone who has had the flu knows, infectious diseases tend to make us feel sleepy. This probably happens because cytokines, chemicals our immune systems produce while fighting an infection, are powerful sleep-inducing chemicals. Sleep may help the body conserve energy and other resources that the immune system needs to mount an attack.
Sleeping problems occur in almost all people with mental disorders, including those with depression and schizophrenia. People with depression, for example, often awaken in the early hours of the morning and find themselves unable to get back to sleep. The amount of sleep a person gets also strongly influences the symptoms of mental disorders. Sleep deprivation is an effective therapy for people with certain types of depression, while it can actually cause depression in other people. Extreme sleep deprivation can lead to a seemingly psychotic state of paranoia and hallucinations in otherwise healthy people, and disrupted sleep can trigger episodes of mania (agitation and hyperactivity) in people with manic depression.
Sleeping problems are common in many other disorders as well, including Alzheimer's disease, stroke, cancer, and head injury. These sleeping problems may arise from changes in the brain regions and neurotransmitters that control sleep, or from the drugs used to control symptoms of other disorders. In patients who are hospitalized or who receive round-the-clock care, treatment schedules or hospital routines also may disrupt sleep. The old joke about a patient being awakened by a nurse so he could take a sleeping pill contains a grain of truth. Once sleeping problems develop, they can add to a person's impairment and cause confusion, frustration, or depression. Patients who are unable to sleep also notice pain more and may increase their requests for pain medication. Better management of sleeping problems in people who have other disorders could improve these patients' health and quality of life.
Sleep Disorders
At least 40 million Americans each year suffer from chronic, long-term sleep disorders each year, and an additional 20 million experience occasional sleeping problems. These disorders and the resulting sleep deprivation interfere with work, driving, and social activities. They also account for an estimated $16 billion in medical costs each year, while the indirect costs due to lost productivity and other factors are probably much greater. Doctors have described more than 70 sleep disorders, most of which can be managed effectively once they are correctly diagnosed. The most common sleep disorders include insomnia, sleep apnea, restless legs syndrome, and narcolepsy.
Insomnia
Almost everyone occasionally suffers from short-term insomnia. This problem can result from stress, jet lag, diet, or many other factors. Insomnia almost always affects job performance and well-being the next day. About 60 million Americans a year have insomnia frequently or for extended periods of time, which leads to even more serious sleep deficits. Insomnia tends to increase with age and affects about 40 percent of women and 30 percent of men. It is often the major disabling symptom of an underlying medical disorder.
For short-term insomnia, doctors may prescribe sleeping pills. Most sleeping pills stop working after several weeks of nightly use, however, and long-term use can actually interfere with good sleep. Mild insomnia often can be prevented or cured by practicing good sleep habits (see "Tips for a Good Night's Sleep"). For more serious cases of insomnia, researchers are experimenting with light therapy and other ways to alter circadian cycles.
Sleep Apnea
Sleep apnea is a disorder of interrupted breathing during sleep. It usually occurs in association with fat buildup or loss of muscle tone with aging. These changes allow the windpipe to collapse during breathing when muscles relax during sleep (see figure 3 ). This problem, called obstructive sleep apnea, is usually associated with loud snoring (though not everyone who snores has this disorder). Sleep apnea also can occur if the neurons that control breathing malfunction during sleep.
During an episode of obstructive apnea, the person's effort to inhale air creates suction that collapses the windpipe. This blocks the air flow for 10 seconds to a minute while the sleeping person struggles to breathe. When the person's blood oxygen level falls, the brain responds by awakening the person enough to tighten the upper airway muscles and open the windpipe. The person may snort or gasp, then resume snoring. This cycle may be repeated hundreds of times a night. The frequent awakenings that sleep apnea patients experience leave them continually sleepy and may lead to personality changes such as irritability or depression. Sleep apnea also deprives the person of oxygen, which can lead to morning headaches, a loss of interest in sex, or a decline in mental functioning. It also is linked to high blood pressure, irregular heartbeats, and an increased risk of heart attacks and stroke. Patients with severe, untreated sleep apnea are two to three times more likely to have automobile accidents than the general population. In some high-risk individuals, sleep apnea may even lead to sudden death from respiratory arrest during sleep.
An estimated 18 million Americans have sleep apnea. However, few of them have had the problem diagnosed. Patients with the typical features of sleep apnea, such as loud snoring, obesity, and excessive daytime sleepiness, should be referred to a specialized sleep center that can perform a test called polysomnography. This test records the patient's brain waves, heartbeat, and breathing during an entire night. If sleep apnea is diagnosed, several treatments are available. Mild sleep apnea frequently can be overcome through weight loss or by preventing the person from sleeping on his or her back. Other people may need special devices or surgery to correct the obstruction. People with sleep apnea should never take sedatives or sleeping pills, which can prevent them from awakening enough to breathe.
Restless Legs Syndrome
Restless legs syndrome (RLS), a familial disorder causing unpleasant crawling, prickling, or tingling sensations in the legs and feet and an urge to move them for relief, is emerging as one of the most common sleep disorders, especially among older people. This disorder, which affects as many as 12 million Americans, leads to constant leg movement during the day and insomnia at night. Severe RLS is most common in elderly people, though symptoms may develop at any age. In some cases, it may be linked to other conditions such as anemia, pregnancy, or diabetes.
Many RLS patients also have a disorder known as periodic limb movement disorder or PLMD, which causes repetitive jerking movements of the limbs, especially the legs. These movements occur every 20 to 40 seconds and cause repeated awakening and severely fragmented sleep. In one study, RLS and PLMD accounted for a third of the insomnia seen in patients older than age 60.
RLS and PLMD often can be relieved by drugs that affect the neurotransmitter dopamine, suggesting that dopamine abnormalities underlie these disorders' symptoms. Learning how these disorders occur may lead to better therapies in the future.
Narcolepsy
Narcolepsy affects an estimated 250,000 Americans. People with narcolepsy have frequent "sleep attacks" at various times of the day, even if they have had a normal amount of night-time sleep. These attacks last from several seconds to more than 30 minutes. People with narcolepsy also may experience cataplexy (loss of muscle control during emotional situations), hallucinations, temporary paralysis when they awaken, and disrupted night-time sleep. These symptoms seem to be features of REM sleep that appear during waking, which suggests that narcolepsy is a disorder of sleep regulation. The symptoms of narcolepsy typically appear during adolescence, though it often takes years to obtain a correct diagnosis. The disorder (or at least a predisposition to it) is usually hereditary, but it occasionally is linked to brain damage from a head injury or neurological disease.
Once narcolepsy is diagnosed, stimulants, antidepressants, or other drugs can help control the symptoms and prevent the embarrassing and dangerous effects of falling asleep at improper times. Naps at certain times of the day also may reduce the excessive daytime sleepiness.
In 1999, a research team working with canine models identified a gene that causes narcolepsy–a breakthrough that brings a cure for this disabling condition within reach. The gene, hypocretin receptor 2, codes for a protein that allows brain cells to receive instructions from other cells. The defective versions of the gene encode proteins that cannot recognize these messages, perhaps cutting the cells off from messages that promote wakefulness. The researchers know that the same gene exists in humans, and they are currently searching for defective versions in people with narcolepsy.
The Future
Sleep research is expanding and attracting more and more attention from scientists. Researchers now know that sleep is an active and dynamic state that greatly influences our waking hours, and they realize that we must understand sleep to fully understand the brain. Innovative techniques, such as brain imaging, can now help researchers understand how different brain regions function during sleep and how different activities and disorders affect sleep. Understanding the factors that affect sleep in health and disease also may lead to revolutionary new therapies for sleep disorders and to ways of overcoming jet lag and the problems associated with shift work. We can expect these and many other benefits from research that will allow us to truly understand sleep's impact on our lives.
Choosing the Right Sleep Medicines, or None at All
By Peter Jaret : NY Times Article : August 7, 2008
In Brief:
The safety of insomnia drugs has improved steadily over the past 30 years.
Choosing the right sleep medication is important; some are best at helping people fall asleep, while others help people stay asleep through the night.
Although medications are often recommended for acute insomnia, the first line of treatment for chronic insomnia is behavioral therapy.
Insomniacs know all too well what it’s like to lie awake in a tangle of sheets, the day’s worries parading through the brain as the minutes tick past with agonizing slowness. With studies linking troubled sleep to a variety of health problems including heart attacks and obesity, it’s enough to keep anyone awake at night.
An estimated 30 million Americans wrestle with chronic insomnia. Many suffer in silence. A 2005 National Sleep Foundation survey found that only one-third of patients with insomnia were asked by their primary care physicians about the quality of their sleep. Insomnia sufferers are equally unlikely to raise the issue with their doctors, studies show. And that’s too bad, experts say.
More and safer medications for sleep problems are available. And with a growing list to choose from, doctors can target prescriptions more precisely to specific complaints: trouble falling asleep, for instance, versus trouble staying asleep.
Remedies to help people fall asleep have been around for centuries, from laudanum in the 1800s to barbiturates more recently. “Unfortunately, most of them were addictive and potentially deadly,” said Dr. David Neubauer, associate director of the Sleep Disorders Center at Johns Hopkins University School of Medicine in Baltimore. “The history of sleep medications is really a tale of improving safety.”
A big advance came in the 1970s with the introduction of benzodiazepine drugs like Halcion, Xanax and Restoril. Although far safer than barbiturates, these sleep medications can still cause dependence and withdrawal symptoms like rebound insomnia. That prompted the Food and Drug Administration to approve them only for short-term use, usually no more than two weeks.
The same restrictions remained in place when a new generation of hypnotic drugs, known as nonbenzodiazepines or “Z” drugs, hit the market, starting with Ambien in the early 1990s.
“But it soon became evident that Ambien was really quite different, that it didn’t have the same withdrawal effects or dependency,” said Dr. Michael Thorpy, director of the Sleep-Wake Disorders Center at Montefiore Medical Center in the Bronx.
In one recent study, researchers at Duke University Medical Center pitted Ambien-CR, a controlled-release formulation, against a placebo. After taking the drug for six months, volunteers reported no rebound insomnia when they stopped. Almost 90 percent said the drug helped them sleep, compared with just under 60 percent of the placebo group. Those on the active drug also reported less morning sleepiness and greater ability to concentrate during the day.
Newer nonbenzodiazepines like Lunesta and Sonata have no restrictions on how long they can be used. Even so, they remain on the federal list of controlled substances because of their potential for abuse.
The latest sleeping pill to win F.D.A. approval, called Rozerem, is the first sleeping pill not on that list, because there appears to be little chance it will be abused. The drug, which targets receptors in the brain for the sleep hormone melatonin, represents the first new class of sleep medication in several decades.
Safer sleep medicines are particularly welcome for people whose insomnia is caused by chronic pain or other persistent medical conditions, Dr. Thorpy said. “These are people who are never going to get a good night’s sleep without medication, and who may need hypnotics for the rest of their lives,” he said.
But those people are the exceptions — most insomniacs will not require pills indefinitely. Indeed, medications are generally considered the first-line treatment not for chronic sleep problems but for acute, short-term insomnia brought on by, say, unusual stress at work or the aftermath of surgery.
“Medications can help nip insomnia in the bud, and may prevent it from becoming a chronic problem,” said Wilfred Pigeon, assistant professor of psychiatry at the Sleep and Neurophysiology Research Laboratory at the University of Rochester.
Doctors are increasingly exploiting the differences among nonbenzodiazepines to tailor their prescription to particular sleep complaints.
Chief among these differences is a drug’s half-life, a measure of how long the active ingredients remain in the body, which can range from one to seven hours for the top sleep aids. If the problem is falling asleep, a drug with a short half-life, like Sonata or Rozerem, may be the best choice. If a patient complains about waking in the middle of the night, a medicine with a longer half-life, like Ambien-CR or Lunesta, may work best.
Although the F.D.A. has not yet approved sleeping pills specifically to be taken when people find themselves wide awake in the middle of the night, “many people take Sonata that way, because it has a very short half-life,” Dr. Thorpy said.
A 2006 study by researchers at the Clinilabs Sleep Disorders Institute at St. Luke’s-Roosevelt Hospital Center in New York found that Sonata taken in the middle of the night caused less next-day sleepiness than Ambien, a drug with a longer half-life.
But even the newer sleep medicines have side effects, including reports of people having no memory of raiding the refrigerator or getting behind the wheel the night before. And because sleep medications address only the symptoms of insomnia and not the causes, many experts agree that the best approach when sleep problems persist is cognitive-behavioral therapy, which teaches strategies like better sleep habits and restricting the amount of time spent awake in bed.
“Drugs can help relieve people’s acute anxiety about being able to fall asleep or stay asleep,” Dr. Pigeon said. Behavioral approaches, which in practice are often combined with sleep drugs, “help make lasting changes in the quality of people’s sleep,” he said.
But changing sleep habits takes time, and a shortage of therapists trained in behavioral sleep medicine means that option is not available to everyone who might benefit. Harried physicians often find it easier to write out a prescription than to discuss sleep hygiene with patients, who likewise often seek the quick relief offered by pills.
Small wonder that pharmaceutical researchers are continually in search of novel insomnia drugs. One drug under development, for example, works in a new way to enhance slow-wave sleep, the deepest stage of slumber, with a goal of making people feel more refreshed in the morning.
“People come in complaining about their sleep,” Dr. Neubauer said. “But of course what we’re really looking for is better wakefulness.”
Tips for a Good Night's Sleep:
Adapted from "When You Can't Sleep: The ABCs of ZZZs," by the National Sleep Foundation.
Sleep Apnea ........An Overview
Obstructive sleep apnea is a condition in which a person has episodes of stopped breathing during sleep.
See also:
Alternative Names Sleep apnea - obstructive; Apnea - obstructive sleep apnea syndrome
Causes » Normally, the muscles of the upper part of the throat help keep the airway open and allow air to flow into the lungs. Even though these muscles usually relax during sleep, the upper throat remains open enough to let air pass by.
However, some people have a narrower throat area, and, during sleep, relaxation of the muscles causes the passage to completely close. This prevents air from getting into the lungs. Loud snoring and labored breathing occur. During deep sleep, breathing can stop for a short period of time (often more than 10 seconds). This is called apnea.
An apnea episode is followed by a sudden attempt to breathe, and a change to a lighter stage of sleep. The result is fragmented sleep that is not restful, leading to excessive daytime drowsiness.
Older obese men seem to be at higher risk, although as many as 40% of people with obstructive sleep apnea are not obese. The following factors may also increase your risk for obstructive sleep apnea:
In-Depth Causes »
Symptoms » It is important to emphasize that, often, the person who has obstructive sleep apnea does not remember the episodes of apnea during the night. The main symptoms are usually associated with excessive daytime sleepiness due to poor sleep during the night. Often, family members, especially spouses, witness the periods of no breathing.
A person with obstructive sleep apnea usually snores heavily soon after falling asleep. The snoring continues at a regular pace for a period of time, often becoming louder, but is then interrupted by a long silent period during which there is no breathing. This is followed by a loud snort and gasp, and the snoring returns. This pattern repeats frequently throughout the night.
Symptoms that may be observed include:
Exams and Tests » The health care provider will perform a physical exam. This will involve carefully checking your mouth, neck, and throat. You will be asked about your medical history. Often, a survey that asks a series of questions about daytime sleepiness, sleep quality, and bedtime habits is given.
A sleep study (polysomnogram) is used to confirm obstructive sleep apnea.
Other tests that may be performed include:
Treatment » The goal is to keep the airway open so that breathing does not stop during sleep.
The following may relieve symptoms of sleep apnea in some individuals:
Surgery may be an option in some cases. This may involve:
In-Depth Treatment »
Outlook (Prognosis) When treated correctly, obstructive sleep apnea may be controlled. However, many patients are unable or unwilling to tolerate CPAP therapy.
Possible Complications During the nonbreathing episodes, blood oxygen levels falls. Persistent low levels of oxygen (hypoxia) may cause many of the daytime symptoms. If the condition is severe enough, pulmonary hypertension may develop, leading to right-sided heart failure or cor pulmonale.
Other complications include:
Scientists know that many people inadvertently undermine their ability to fall asleep and stay asleep for a full night. Here are some frequent suggestions:
1. Establish a regular sleep schedule and try to stick to it, even on weekends.
2. If you nap during the day, limit it to 20 or 30 minutes, preferably early in the afternoon.
3. Avoid alcohol in the evening, as it can disrupt sleep.
4. Don’t eat a big meal just before bedtime, but don’t go to bed hungry, either. Eat a light snack before bed, if needed, preferably one high in carbohydrates.
5. If you use medications that are stimulants, take them in the morning, or ask your doctor if you can switch to a nonstimulating alternative. If you use drugs that cause drowsiness, take them in the evening.
6. Get regular exercise during the day, but avoid vigorous exercise within three hours of bedtime.
7. If pressing thoughts interfere with falling asleep, write them down (keep a pad and pen next to the bed) and try to forget about them until morning.
8. If you are frequently awakened by a need to use the bathroom, cut down on how much you drink late in the day.
9. If you smoke, quit. Among other hazards, nicotine is a stimulant and can cause nightmares.
10. Avoid beverages and foods containing caffeine after 3 p.m. Even decaf versions have some caffeine, which can bother some people.
Cheating Ourselves of Sleep
By Jane E. Brody : NY Times : June 17, 2013
Think you do just fine on five or six hours of shut-eye? Chances are, you are among the many millions who unwittingly shortchange themselves on sleep.
Research shows that most people require seven or eight hours of sleep to function optimally. Failing to get enough sleep night after night can compromise your health and may even shorten your life. From infancy to old age, the effects of inadequate sleep can profoundly affect memory, learning, creativity, productivity and emotional stability, as well as your physical health.
According to sleep specialists at the University of Pittsburgh School of Medicine and Western Psychiatric Institute and Clinic, among others, a number of bodily systems are negatively affected by inadequate sleep: the heart, lungs and kidneys; appetite, metabolism and weight control; immune function and disease resistance; sensitivity to pain; reaction time; mood; and brain function.
Poor sleep is also a risk factor for depression and substance abuse, especially among people with post-traumatic stress disorder, according to Anne Germain, associate professor of psychiatry at the University of Pittsburgh. People with PTSD tend to relive their trauma when they try to sleep, which keeps their brains in a heightened state of alertness.
Dr. Germain is studying what happens in the brains of sleeping veterans with PTSD in hopes of developing more effective treatments for them and for people with lesser degrees of stress that interfere with a good night’s sleep.
The elderly are especially vulnerable. Timothy H. Monk, who directs the Human Chronobiology Research Program at Western Psychiatric, heads a five-year federally funded study of circadian rhythms, sleep strength, stress reactivity, brain function and genetics among the elderly. “The circadian signal isn’t as strong as people get older,” he said.
He is finding that many are helped by standard behavioral treatments for insomnia, like maintaining a regular sleep schedule, avoiding late-in-day naps and caffeine, and reducing distractions from light, noise and pets.
It should come as no surprise that myriad bodily systems can be harmed by chronically shortened nights. “Sleep affects almost every tissue in our bodies,” said Dr. Michael J. Twery, a sleep specialist at the National Institutes of Health.
Several studies have linked insufficient sleep to weight gain. Not only do night owls with shortchanged sleep have more time to eat, drink and snack, but levels of the hormone leptin, which tells the brain enough food has been consumed, are lower in the sleep-deprived while levels of ghrelin, which stimulates appetite, are higher.
In addition, metabolism slows when one’s circadian rhythm and sleep are disrupted; if not counteracted by increased exercise or reduced caloric intake, this slowdown could add up to 10 extra pounds in a year.
The body’s ability to process glucose is also adversely affected, which may ultimately result in Type 2 diabetes. In one study, healthy young men prevented from sleeping more than four hours a night for six nights in a row ended up with insulin and blood sugar levels like those of people deemed prediabetic. The risks of cardiovascular diseases and stroke are higher in people who sleep less than six hours a night. Even a single night of inadequate sleep can cause daylong elevations in blood pressure in people with hypertension. Inadequate sleep is also associated with calcification of coronary arteries and raised levels of inflammatory factors linked to heart disease. (In terms of cardiovascular disease, sleeping too much may also be risky. Higher rates of heart disease have been found among women who sleep more than nine hours nightly.)
The risk of cancer may also be elevated in people who fail to get enough sleep. A Japanese study of nearly 24,000 women ages 40 to 79 found that those who slept less than six hours a night were more likely to develop breast cancer than women who slept longer. The increased risk may result from diminished secretion of the sleep hormone melatonin. Among participants in the Nurses Health Study, Eva S. Schernhammer of Harvard Medical School found a link between low melatonin levels and an increased risk of breast cancer.
A study of 1,240 people by researchers at Case Western Reserve University in Cleveland found an increased risk of potentially cancerous colorectal polyps in those who slept fewer than six hours nightly.
Children can also experience hormonal disruptions from inadequate sleep. Growth hormone is released during deep sleep; it not only stimulates growth in children, but also boosts muscle mass and repairs damaged cells and tissues in both children and adults.
Dr. Vatsal G. Thakkar, a psychiatrist affiliated with New York University, recently described evidence associating inadequate sleep with an erroneous diagnosis of attention deficit hyperactivity disorder in children. In one study, 28 percent of children with sleep problems had symptoms of the disorder, but not the disorder.
During sleep, the body produces cytokines, cellular hormones that help fight infections. Thus, short sleepers may be more susceptible to everyday infections like colds and flu. In a study of 153 healthy men and women, Sheldon Cohen and colleagues at Carnegie Mellon University found that those who slept less than seven hours a night were three times as likely to develop cold symptoms when exposed to a cold-causing virus than were people who slept eight or more hours.
Some of the most insidious effects of too little sleep involve mental processes like learning, memory, judgment and problem-solving. During sleep, new learning and memory pathways become encoded in the brain, and adequate sleep is necessary for those pathways to work optimally. People who are well rested are better able to learn a task and more likely to remember what they learned. The cognitive decline that so often accompanies aging may in part result from chronically poor sleep.
With insufficient sleep, thinking slows, it is harder to focus and pay attention, and people are more likely to make poor decisions and take undue risks. As you might guess, these effects can be disastrous when operating a motor vehicle or dangerous machine.
In driving tests, sleep-deprived people perform as if drunk, and no amount of caffeine or cold air can negate the ill effects.
At your next health checkup, tell your doctor how long and how well you sleep. Be honest: Sleep duration and quality can be as important to your health as your blood pressure and cholesterol level.
This is the first of two columns on inadequate sleep.
Why We Need Our Sleep
By Robert Lee Hotz : WSJ Article : January 18, 2008
People have been trying to figure out why we sleep for almost as long as we have been conscious of being awake, tossing and turning in the dark.
After a few restless nights, most of us can't even think straight. We are less able to make sense of problems, make competent moral judgments or retain what we learn, even though studies show our brain cells fire more frenetically to overcome the lack of sleep. Lose too much sleep and we become reckless, emotionally fragile and more vulnerable to infections as well as diabetes, heart disease and obesity, recent research suggests.
Yet scientists probing the purpose of sleep are still largely in the dark. "Why we sleep at all is a strange bastion of the unknown," said sleep psychologist Matthew Walker at the University of California in Berkeley.
One vital function of sleep, researchers argue, may be to help our brains sort, store and consolidate new memories, etching experiences more indelibly into the brain's biochemical archives.
.
Even a 90-minute nap can significantly improve our ability to master new motor skills and strengthen our memories of what we learn, researchers at the University of Haifa in Israel reported last month in Nature Neuroscience. "Napping is as effective as a night's sleep," said psychologist Sara Mednick at the University of California in San Diego.
Moreover, slumber seems to boost our ability to make sense of new knowledge by allowing the brain to detect connections between things we learn.
In research published in April in the Proceedings of the National Academy of Sciences, Dr. Walker and his collaborators at the Harvard Medical School tested 56 college students and found that their ability to discern the big picture in disparate pieces of information improved measurably after the brain could, during a night's sleep, mull things over.
It is these patterns of meaning -- the distilled essence of knowledge -- that we remember so well. "Sleep helps stabilize memory," said neurologist Jeffrey Ellenbogen, director of the sleep-medicine program at Massachusetts General Hospital.
The erratic biorhythms of sleep and behavior are intertwined everywhere in nature. Socially active fruit flies need more sleep than loner flies, and even zebra fish can get insomnia.
Sleep is controlled partly by our genes. The difference between those of us who naturally wake at dawn and night owls who are wide-eyed at midnight may be partly due to variations in a gene, named Period3, that affects our biological clock. Variations in that gene also make some people especially sensitive to sleep deprivation, scientists at the U.K.'s University of Surrey recently reported.
For many of us, though, sleeplessness is a self-inflicted epidemic in which lifestyle overrides basic biology. "In this odd, Western 24-hour-MTV-fast-food generation we have created, we all feel the need to achieve more and more. The one thing that takes a hit is sleep," Dr. Walker said. On average, most people sleep 75 minutes less each night than people did a century ago, sleep surveys record.
Yet, rarely have so many millions of drowsy people been trying so hard to secure some shut-eye, spending billions on sleep aids. By one estimate, in the U.S. alone, pharmacists filled 49 million prescriptions for sleep drugs last year. Even so, we think we sleep more than we actually do, according to Arizona State University scientists. They recorded how long 2,100 volunteers actually slept each night and compared that to how long the people reported they had slept. Most people overestimated their sleep by about 18 minutes, the scientists found.
The consequences of too little sleep can be dire. Almost half of all heavy-truck accidents in the U.S. can be traced to driver fatigue, while decisions leading to the Challenger space-shuttle disaster, the Chernobyl nuclear-reactor meltdown and the Exxon Valdez oil spill can be partly linked to people drained of rest by round-the-clock work schedules. Weary doctors make more serious medical errors, while sleepy airport baggage screeners make more security mistakes, researchers reported at the Associated Professional Sleep Societies.
All told, the frayed tempers, short attention spans and fuzzy thinking caused by sleep deprivation may cost $15 billion a year in reduced productivity, the National Commission on Sleep Disorders Research estimated.
The expectation of a nap, however, is by itself enough to measurably lower our blood pressure, researchers at the Liverpool John Moores University in England reported in October in the Journal of Applied Physiology.
Indeed, regular nappers -- working men who took a siesta for 30 minutes or more at least three times a week -- had a 64% lower risk of heart-related death, researchers at the University of Athens reported last February in the Archives of Internal Medicine.
"All of the things we are proving about sleep and the brain are things that your mother already knew decades ago," Dr. Walker said. "We are putting the science and the hard facts behind it."
A Good Night’s Sleep Isn’t a Luxury; It’s a Necessity
By Jane E. Brody : NY Times : May 30, 2011
In my younger years, I regarded sleep as a necessary evil, nature’s way of thwarting my desire to cram as many activities into a 24-hour day as possible. I frequently flew the red-eye from California, for instance, sailing (or so I thought) through the next day on less than four hours of uncomfortable sleep.
But my neglect was costing me in ways that I did not fully appreciate. My husband called our nights at the ballet and theater “Jane’s most expensive naps.” Eventually we relinquished our subscriptions. Driving, too, was dicey: twice I fell asleep at the wheel, narrowly avoiding disaster. I realize now that I was living in a state of chronic sleep deprivation.
I don’t want to nod off during cultural events, and I no longer have my husband to spell me at the wheel. I also don’t want to compromise my ability to think and react. As research cited recently in this newspaper’s magazine found, “The sleep-deprived among us are lousy judges of our own sleep needs. We are not nearly as sharp as we think we are.”
Studies have shown that people function best after seven to eight hours of sleep, so I now aim for a solid seven hours, the amount associated with the lowest mortality rate. Yet on most nights something seems to interfere, keeping me up later than my intended lights-out at 10 p.m. — an essential household task, an e-mail requiring an urgent and thoughtful response, a condolence letter I never found time to write during the day, a long article that I must read.
It’s always something.
What’s Keeping Us Up?
I know I’m hardly alone. Between 1960 and 2010, the average night’s sleep for adults in the United States dropped to six and a half hours from more than eight. Some experts predict a continuing decline, thanks to distractions like e-mail, instant and text messaging, and online shopping.
Age can have a detrimental effect on sleep. In a 2005 national telephone survey of 1,003 adults ages 50 and older, the Gallup Organization found that a mere third of older adults got a good night’s sleep every day, fewer than half slept more than seven hours, and one-fifth slept less than six hours a night.
With advancing age, natural changes in sleep quality occur. People may take longer to fall asleep, and they tend to get sleepy earlier in the evening and to awaken earlier in the morning. More time is spent in the lighter stages of sleep and less in restorative deep sleep. R.E.M. sleep, during which the mind processes emotions and memories and relieves stress, also declines with age.
Habits that ruin sleep often accompany aging: less physical activity, less time spent outdoors (sunlight is the body’s main regulator of sleepiness and wakefulness), poorer attention to diet, taking medications that can disrupt sleep, caring for a chronically ill spouse, having a partner who snores. Some use alcohol in hopes of inducing sleep; in fact, it disrupts sleep.
Add to this list a host of sleep-robbing health issues, like painful arthritis, diabetes, depression, anxiety, sleep apnea, hot flashes in women and prostate enlargement in men. In the last years of his life, my husband was plagued with restless leg syndrome, forcing him to get up and walk around in the middle of the night until the symptoms subsided. During a recent night, I was awake for hours with leg cramps that simply wouldn’t quit.
Beauty Rest and Beyond
A good night’s sleep is much more than a luxury. Its benefits include improvements in concentration, short-term memory, productivity, mood, sensitivity to pain and immune function.
If you care about how you look, more sleep can even make you appear more attractive. In a study published online in December in the journal BMJ, researchers in Sweden and the Netherlands reported that 23 sleep-deprived adults seemed to untrained observers to be less healthy, more tired and less attractive than they appeared to be after a full night’s sleep.
Perhaps more important, losing sleep may make you fat — or at least, fatter than you would otherwise be. In a study by Harvard researchers involving 68,000 middle-aged women followed for 16 years, those who slept five hours or less each night were found to weigh 5.4 pounds more — and were 15 percent more likely to become obese — than the women who slept seven hours nightly.
Michael Breus, a clinical psychologist and sleep specialist in Scottsdale, Ariz., and author of “The Sleep Doctor’s Diet Plan,” points out that as the average length of sleep has declined in the United States, the average weight of Americans has increased.
There are plausible reasons to think this is a cause-and-effect relationship. At least two factors may be involved: more waking hours in homes brimming with food and snacks; and possible changes in the hormones leptin and ghrelin, which regulate appetite.
In a study published in 2009 in The American Journal of Clinical Nutrition, Dr. Plamen D. Penev, an endocrinologist at the University of Chicago, and co-authors explored calorie consumption and expenditure by 11 healthy volunteers who spent two 14-day stays in a sleep laboratory. Both sessions offered unlimited access to tasty foods. During one stay, the volunteers — five women and six men — were limited to 5.5 hours of sleep a night, and during the other they got 8.5 hours of sleep.
Although the subjects ate the same amount of food at meals, during the shortened nights they consumed an average of 221 more calories from snacks than they did when they were getting more sleep. The snacks they ate tended to be high in carbohydrates, and the subjects expended no more energy than they did on the longer nights. In just two weeks, the extra nighttime snacking could add nearly a pound to body weight, the scientists concluded.
These researchers found no significant changes in the participants’ blood levels of the hormones leptin and ghrelin, but others have found that short sleepers have lower levels of appetite-suppressing leptin and higher levels of ghrelin, which prompts an increase in calorie intake.
Sleep loss may also affect the function of a group of neurons in the hypothalamus of the brain, where another hormone, orexin, is involved in the regulation of feeding behavior.
The bottom line: Resist the temptation to squeeze one more thing into the end of your day. If health problems disrupt your sleep, seek treatment that can lessen their effect. If you have trouble falling asleep or often awaken during the night and can’t get back to sleep, you could try taking supplements of melatonin, the body’s natural sleep inducer. I keep it at my bedside.
If you have trouble sleeping, the tips accompanying this article may help. And if all else fails, try to take a nap during the day. Naps can enhance brain function, energy, mood and productivity.
Brain Basics:
Understanding Sleep
Do you ever feel sleepy or "zone out" during the day? Do you find it hard to wake up on Monday mornings? If so, you are familiar with the powerful need for sleep. However, you may not realize that sleep is as essential for your well-being as food and water.
- Sleep: A Dynamic Activity
- How Much Sleep Do We Need?
- What Does Sleep Do For Us?
- Dreaming and REM Sleep
- Sleep and Circadian Rhythms
- Sleep and Disease
- Sleep Disorders
- The Future
- Tips for a Good Night's Sleep
Until the 1950s, most people thought of sleep as a passive, dormant part of our daily lives. We now know that our brains are very active during sleep. Moreover, sleep affects our daily functioning and our physical and mental health in many ways that we are just beginning to understand.
Nerve-signaling chemicals called neurotransmitters control whether we are asleep or awake by acting on different groups of nerve cells, or neurons, in the brain. Neurons in the brainstem, which connects the brain with the spinal cord, produce neurotransmitters such as serotonin and norepinephrine that keep some parts of the brain active while we are awake. Other neurons at the base of the brain begin signaling when we fall asleep. These neurons appear to "switch off" the signals that keep us awake. Research also suggests that a chemical called adenosine builds up in our blood while we are awake and causes drowsiness. This chemical gradually breaks down while we sleep.
During sleep, we usually pass through five phases of sleep: stages 1, 2, 3, 4, and REM (rapid eye movement) sleep. These stages progress in a cycle from stage 1 to REM sleep, then the cycle starts over again with stage 1 (see figure 1 ). We spend almost 50 percent of our total sleep time in stage 2 sleep, about 20 percent in REM sleep, and the remaining 30 percent in the other stages. Infants, by contrast, spend about half of their sleep time in REM sleep.
During stage 1, which is light sleep, we drift in and out of sleep and can be awakened easily. Our eyes move very slowly and muscle activity slows. People awakened from stage 1 sleep often remember fragmented visual images. Many also experience sudden muscle contractions called hypnic myoclonia, often preceded by a sensation of starting to fall. These sudden movements are similar to the "jump" we make when startled. When we enter stage 2 sleep, our eye movements stop and our brain waves (fluctuations of electrical activity that can be measured by electrodes) become slower, with occasional bursts of rapid waves called sleep spindles. In stage 3, extremely slow brain waves called delta waves begin to appear, interspersed with smaller, faster waves. By stage 4, the brain produces delta waves almost exclusively. It is very difficult to wake someone during stages 3 and 4, which together are called deep sleep. There is no eye movement or muscle activity. People awakened during deep sleep do not adjust immediately and often feel groggy and disoriented for several minutes after they wake up. Some children experience bedwetting, night terrors, or sleepwalking during deep sleep.
When we switch into REM sleep, our breathing becomes more rapid, irregular, and shallow, our eyes jerk rapidly in various directions, and our limb muscles become temporarily paralyzed. Our heart rate increases, our blood pressure rises, and males develop penile erections. When people awaken during REM sleep, they often describe bizarre and illogical tales – dreams.
The first REM sleep period usually occurs about 70 to 90 minutes after we fall asleep. A complete sleep cycle takes 90 to 110 minutes on average. The first sleep cycles each night contain relatively short REM periods and long periods of deep sleep. As the night progresses, REM sleep periods increase in length while deep sleep decreases. By morning, people spend nearly all their sleep time in stages 1, 2, and REM.
People awakened after sleeping more than a few minutes are usually unable to recall the last few minutes before they fell asleep. This sleep-related form of amnesia is the reason people often forget telephone calls or conversations they've had in the middle of the night. It also explains why we often do not remember our alarms ringing in the morning if we go right back to sleep after turning them off.
Since sleep and wakefulness are influenced by different neurotransmitter signals in the brain, foods and medicines that change the balance of these signals affect whether we feel alert or drowsy and how well we sleep. Caffeinated drinks such as coffee and drugs such as diet pills and decongestants stimulate some parts of the brain and can cause insomnia, or an inability to sleep. Many antidepressants suppress REM sleep. Heavy smokers often sleep very lightly and have reduced amounts of REM sleep. They also tend to wake up after 3 or 4 hours of sleep due to nicotine withdrawal. Many people who suffer from insomnia try to solve the problem with alcohol – the so-called night cap. While alcohol does help people fall into light sleep, it also robs them of REM and the deeper, more restorative stages of sleep. Instead, it keeps them in the lighter stages of sleep, from which they can be awakened easily.
People lose some of the ability to regulate their body temperature during REM, so abnormally hot or cold temperatures in the environment can disrupt this stage of sleep. If our REM sleep is disrupted one night, our bodies don't follow the normal sleep cycle progression the next time we doze off. Instead, we often slip directly into REM sleep and go through extended periods of REM until we "catch up" on this stage of sleep.
People who are under anesthesia or in a coma are often said to be asleep. However, people in these conditions cannot be awakened and do not produce the complex, active brain wave patterns seen in normal sleep. Instead, their brain waves are very slow and weak, sometimes all but undetectable.
How Much Sleep Do We Need?
The amount of sleep each person needs depends on many factors, including age. Infants generally require about 16 hours a day, while teenagers need about 9 hours on average. For most adults, 7 to 8 hours a night appears to be the best amount of sleep, although some people may need as few as 5 hours or as many as 10 hours of sleep each day. Women in the first 3 months of pregnancy often need several more hours of sleep than usual. The amount of sleep a person needs also increases if he or she has been deprived of sleep in previous days. Getting too little sleep creates a "sleep debt," which is much like being overdrawn at a bank. Eventually, your body will demand that the debt be repaid. We don't seem to adapt to getting less sleep than we need; while we may get used to a sleep-depriving schedule, our judgment, reaction time, and other functions are still impaired.
People tend to sleep more lightly and for shorter time spans as they get older, although they generally need about the same amount of sleep as they needed in early adulthood. About half of all people over 65 have frequent sleeping problems, such as insomnia, and deep sleep stages in many elderly people often become very short or stop completely. This change may be a normal part of aging, or it may result from medical problems that are common in elderly people and from the medications and other treatments for those problems.
Experts say that if you feel drowsy during the day, even during boring activities, you haven't had enough sleep. If you routinely fall asleep within 5 minutes of lying down, you probably have severe sleep deprivation, possibly even a sleep disorder. Microsleeps, or very brief episodes of sleep in an otherwise awake person, are another mark of sleep deprivation. In many cases, people are not aware that they are experiencing microsleeps. The widespread practice of "burning the candle at both ends" in western industrialized societies has created so much sleep deprivation that what is really abnormal sleepiness is now almost the norm.
Many studies make it clear that sleep deprivation is dangerous. Sleep-deprived people who are tested by using a driving simulator or by performing a hand-eye coordination task perform as badly as or worse than those who are intoxicated. Sleep deprivation also magnifies alcohol's effects on the body, so a fatigued person who drinks will become much more impaired than someone who is well-rested. Driver fatigue is responsible for an estimated 100,000 motor vehicle accidents and 1500 deaths each year, according to the National Highway Traffic Safety Administration. Since drowsiness is the brain's last step before falling asleep, driving while drowsy can – and often does – lead to disaster. Caffeine and other stimulants cannot overcome the effects of severe sleep deprivation. The National Sleep Foundation says that if you have trouble keeping your eyes focused, if you can't stop yawning, or if you can't remember driving the last few miles, you are probably too drowsy to drive safely.
What Does Sleep Do For Us?
Although scientists are still trying to learn exactly why people need sleep, animal studies show that sleep is necessary for survival. For example, while rats normally live for two to three years, those deprived of REM sleep survive only about 5 weeks on average, and rats deprived of all sleep stages live only about 3 weeks. Sleep-deprived rats also develop abnormally low body temperatures and sores on their tail and paws. The sores may develop because the rats' immune systems become impaired. Some studies suggest that sleep deprivation affects the immune system in detrimental ways.
Sleep appears necessary for our nervous systems to work properly. Too little sleep leaves us drowsy and unable to concentrate the next day. It also leads to impaired memory and physical performance and reduced ability to carry out math calculations. If sleep deprivation continues, hallucinations and mood swings may develop. Some experts believe sleep gives neurons used while we are awake a chance to shut down and repair themselves. Without sleep, neurons may become so depleted in energy or so polluted with byproducts of normal cellular activities that they begin to malfunction. Sleep also may give the brain a chance to exercise important neuronal connections that might otherwise deteriorate from lack of activity.
Deep sleep coincides with the release of growth hormone in children and young adults. Many of the body's cells also show increased production and reduced breakdown of proteins during deep sleep. Since proteins are the building blocks needed for cell growth and for repair of damage from factors like stress and ultraviolet rays, deep sleep may truly be "beauty sleep." Activity in parts of the brain that control emotions, decision-making processes, and social interactions is drastically reduced during deep sleep, suggesting that this type of sleep may help people maintain optimal emotional and social functioning while they are awake. A study in rats also showed that certain nerve-signaling patterns which the rats generated during the day were repeated during deep sleep. This pattern repetition may help encode memories and improve learning.
Dreaming and REM Sleep
We typically spend more than 2 hours each night dreaming. Scientists do not know much about how or why we dream. Sigmund Freud, who greatly influenced the field of psychology, believed dreaming was a "safety valve" for unconscious desires. Only after 1953, when researchers first described REM in sleeping infants, did scientists begin to carefully study sleep and dreaming. They soon realized that the strange, illogical experiences we call dreams almost always occur during REM sleep. While most mammals and birds show signs of REM sleep, reptiles and other cold-blooded animals do not.
REM sleep begins with signals from an area at the base of the brain called the pons (see figure 2 ). These signals travel to a brain region called the thalamus, which relays them to the cerebral cortex – the outer layer of the brain that is responsible for learning, thinking, and organizing information. The pons also sends signals that shut off neurons in the spinal cord, causing temporary paralysis of the limb muscles. If something interferes with this paralysis, people will begin to physically "act out" their dreams – a rare, dangerous problem called REM sleep behavior disorder. A person dreaming about a ball game, for example, may run headlong into furniture or blindly strike someone sleeping nearby while trying to catch a ball in the dream.
REM sleep stimulates the brain regions used in learning. This may be important for normal brain development during infancy, which would explain why infants spend much more time in REM sleep than adults (see Sleep: A Dynamic Activity ). Like deep sleep, REM sleep is associated with increased production of proteins. One study found that REM sleep affects learning of certain mental skills. People taught a skill and then deprived of non-REM sleep could recall what they had learned after sleeping, while people deprived of REM sleep could not.
Some scientists believe dreams are the cortex's attempt to find meaning in the random signals that it receives during REM sleep. The cortex is the part of the brain that interprets and organizes information from the environment during consciousness. It may be that, given random signals from the pons during REM sleep, the cortex tries to interpret these signals as well, creating a "story" out of fragmented brain activity.
Sleep and Circadian Rhythms
Circadian rhythms are regular changes in mental and physical characteristics that occur in the course of a day (circadian is Latin for "around a day"). Most circadian rhythms are controlled by the body's biological "clock." This clock, called the suprachiasmatic nucleus or SCN (see figure 2 ), is actually a pair of pinhead-sized brain structures that together contain about 20,000 neurons. The SCN rests in a part of the brain called the hypothalamus, just above the point where the optic nerves cross. Light that reaches photoreceptors in the retina (a tissue at the back of the eye) creates signals that travel along the optic nerve to the SCN.
Signals from the SCN travel to several brain regions, including the pineal gland, which responds to light-induced signals by switching off production of the hormone melatonin. The body's level of melatonin normally increases after darkness falls, making people feel drowsy. The SCN also governs functions that are synchronized with the sleep/wake cycle, including body temperature, hormone secretion, urine production, and changes in blood pressure.
By depriving people of light and other external time cues, scientists have learned that most people's biological clocks work on a 25-hour cycle rather than a 24-hour one. But because sunlight or other bright lights can reset the SCN, our biological cycles normally follow the 24-hour cycle of the sun, rather than our innate cycle. Circadian rhythms can be affected to some degree by almost any kind of external time cue, such as the beeping of your alarm clock, the clatter of a garbage truck, or the timing of your meals. Scientists call external time cues zeitgebers (German for "time givers").
When travelers pass from one time zone to another, they suffer from disrupted circadian rhythms, an uncomfortable feeling known as jet lag. For instance, if you travel from California to New York, you "lose" 3 hours according to your body's clock. You will feel tired when the alarm rings at 8 a.m. the next morning because, according to your body's clock, it is still 5 a.m. It usually takes several days for your body's cycles to adjust to the new time.
To reduce the effects of jet lag, some doctors try to manipulate the biological clock with a technique called light therapy. They expose people to special lights, many times brighter than ordinary household light, for several hours near the time the subjects want to wake up. This helps them reset their biological clocks and adjust to a new time zone.
Symptoms much like jet lag are common in people who work nights or who perform shift work. Because these people's work schedules are at odds with powerful sleep-regulating cues like sunlight, they often become uncontrollably drowsy during work, and they may suffer insomnia or other problems when they try to sleep. Shift workers have an increased risk of heart problems, digestive disturbances, and emotional and mental problems, all of which may be related to their sleeping problems. The number and severity of workplace accidents also tend to increase during the night shift. Major industrial accidents attributed partly to errors made by fatigued night-shift workers include the Exxon Valdez oil spill and the Three Mile Island and Chernobyl nuclear power plant accidents. One study also found that medical interns working on the night shift are twice as likely as others to misinterpret hospital test records, which could endanger their patients. It may be possible to reduce shift-related fatigue by using bright lights in the workplace, minimizing shift changes, and taking scheduled naps.
Many people with total blindness experience life-long sleeping problems because their retinas are unable to detect light. These people have a kind of permanent jet lag and periodic insomnia because their circadian rhythms follow their innate cycle rather than a 24-hour one. Daily supplements of melatonin may improve night-time sleep for such patients. However, since the high doses of melatonin found in most supplements can build up in the body, long-term use of this substance may create new problems. Because the potential side effects of melatonin supplements are still largely unknown, most experts discourage melatonin use by the general public.
Sleep and Disease
Sleep and sleep-related problems play a role in a large number of human disorders and affect almost every field of medicine. For example, problems like stroke and asthma attacks tend to occur more frequently during the night and early morning, perhaps due to changes in hormones, heart rate, and other characteristics associated with sleep. Sleep also affects some kinds of epilepsy in complex ways. REM sleep seems to help prevent seizures that begin in one part of the brain from spreading to other brain regions, while deep sleep may promote the spread of these seizures. Sleep deprivation also triggers seizures in people with some types of epilepsy.
Neurons that control sleep interact closely with the immune system. As anyone who has had the flu knows, infectious diseases tend to make us feel sleepy. This probably happens because cytokines, chemicals our immune systems produce while fighting an infection, are powerful sleep-inducing chemicals. Sleep may help the body conserve energy and other resources that the immune system needs to mount an attack.
Sleeping problems occur in almost all people with mental disorders, including those with depression and schizophrenia. People with depression, for example, often awaken in the early hours of the morning and find themselves unable to get back to sleep. The amount of sleep a person gets also strongly influences the symptoms of mental disorders. Sleep deprivation is an effective therapy for people with certain types of depression, while it can actually cause depression in other people. Extreme sleep deprivation can lead to a seemingly psychotic state of paranoia and hallucinations in otherwise healthy people, and disrupted sleep can trigger episodes of mania (agitation and hyperactivity) in people with manic depression.
Sleeping problems are common in many other disorders as well, including Alzheimer's disease, stroke, cancer, and head injury. These sleeping problems may arise from changes in the brain regions and neurotransmitters that control sleep, or from the drugs used to control symptoms of other disorders. In patients who are hospitalized or who receive round-the-clock care, treatment schedules or hospital routines also may disrupt sleep. The old joke about a patient being awakened by a nurse so he could take a sleeping pill contains a grain of truth. Once sleeping problems develop, they can add to a person's impairment and cause confusion, frustration, or depression. Patients who are unable to sleep also notice pain more and may increase their requests for pain medication. Better management of sleeping problems in people who have other disorders could improve these patients' health and quality of life.
Sleep Disorders
At least 40 million Americans each year suffer from chronic, long-term sleep disorders each year, and an additional 20 million experience occasional sleeping problems. These disorders and the resulting sleep deprivation interfere with work, driving, and social activities. They also account for an estimated $16 billion in medical costs each year, while the indirect costs due to lost productivity and other factors are probably much greater. Doctors have described more than 70 sleep disorders, most of which can be managed effectively once they are correctly diagnosed. The most common sleep disorders include insomnia, sleep apnea, restless legs syndrome, and narcolepsy.
Insomnia
Almost everyone occasionally suffers from short-term insomnia. This problem can result from stress, jet lag, diet, or many other factors. Insomnia almost always affects job performance and well-being the next day. About 60 million Americans a year have insomnia frequently or for extended periods of time, which leads to even more serious sleep deficits. Insomnia tends to increase with age and affects about 40 percent of women and 30 percent of men. It is often the major disabling symptom of an underlying medical disorder.
For short-term insomnia, doctors may prescribe sleeping pills. Most sleeping pills stop working after several weeks of nightly use, however, and long-term use can actually interfere with good sleep. Mild insomnia often can be prevented or cured by practicing good sleep habits (see "Tips for a Good Night's Sleep"). For more serious cases of insomnia, researchers are experimenting with light therapy and other ways to alter circadian cycles.
Sleep Apnea
Sleep apnea is a disorder of interrupted breathing during sleep. It usually occurs in association with fat buildup or loss of muscle tone with aging. These changes allow the windpipe to collapse during breathing when muscles relax during sleep (see figure 3 ). This problem, called obstructive sleep apnea, is usually associated with loud snoring (though not everyone who snores has this disorder). Sleep apnea also can occur if the neurons that control breathing malfunction during sleep.
During an episode of obstructive apnea, the person's effort to inhale air creates suction that collapses the windpipe. This blocks the air flow for 10 seconds to a minute while the sleeping person struggles to breathe. When the person's blood oxygen level falls, the brain responds by awakening the person enough to tighten the upper airway muscles and open the windpipe. The person may snort or gasp, then resume snoring. This cycle may be repeated hundreds of times a night. The frequent awakenings that sleep apnea patients experience leave them continually sleepy and may lead to personality changes such as irritability or depression. Sleep apnea also deprives the person of oxygen, which can lead to morning headaches, a loss of interest in sex, or a decline in mental functioning. It also is linked to high blood pressure, irregular heartbeats, and an increased risk of heart attacks and stroke. Patients with severe, untreated sleep apnea are two to three times more likely to have automobile accidents than the general population. In some high-risk individuals, sleep apnea may even lead to sudden death from respiratory arrest during sleep.
An estimated 18 million Americans have sleep apnea. However, few of them have had the problem diagnosed. Patients with the typical features of sleep apnea, such as loud snoring, obesity, and excessive daytime sleepiness, should be referred to a specialized sleep center that can perform a test called polysomnography. This test records the patient's brain waves, heartbeat, and breathing during an entire night. If sleep apnea is diagnosed, several treatments are available. Mild sleep apnea frequently can be overcome through weight loss or by preventing the person from sleeping on his or her back. Other people may need special devices or surgery to correct the obstruction. People with sleep apnea should never take sedatives or sleeping pills, which can prevent them from awakening enough to breathe.
Restless Legs Syndrome
Restless legs syndrome (RLS), a familial disorder causing unpleasant crawling, prickling, or tingling sensations in the legs and feet and an urge to move them for relief, is emerging as one of the most common sleep disorders, especially among older people. This disorder, which affects as many as 12 million Americans, leads to constant leg movement during the day and insomnia at night. Severe RLS is most common in elderly people, though symptoms may develop at any age. In some cases, it may be linked to other conditions such as anemia, pregnancy, or diabetes.
Many RLS patients also have a disorder known as periodic limb movement disorder or PLMD, which causes repetitive jerking movements of the limbs, especially the legs. These movements occur every 20 to 40 seconds and cause repeated awakening and severely fragmented sleep. In one study, RLS and PLMD accounted for a third of the insomnia seen in patients older than age 60.
RLS and PLMD often can be relieved by drugs that affect the neurotransmitter dopamine, suggesting that dopamine abnormalities underlie these disorders' symptoms. Learning how these disorders occur may lead to better therapies in the future.
Narcolepsy
Narcolepsy affects an estimated 250,000 Americans. People with narcolepsy have frequent "sleep attacks" at various times of the day, even if they have had a normal amount of night-time sleep. These attacks last from several seconds to more than 30 minutes. People with narcolepsy also may experience cataplexy (loss of muscle control during emotional situations), hallucinations, temporary paralysis when they awaken, and disrupted night-time sleep. These symptoms seem to be features of REM sleep that appear during waking, which suggests that narcolepsy is a disorder of sleep regulation. The symptoms of narcolepsy typically appear during adolescence, though it often takes years to obtain a correct diagnosis. The disorder (or at least a predisposition to it) is usually hereditary, but it occasionally is linked to brain damage from a head injury or neurological disease.
Once narcolepsy is diagnosed, stimulants, antidepressants, or other drugs can help control the symptoms and prevent the embarrassing and dangerous effects of falling asleep at improper times. Naps at certain times of the day also may reduce the excessive daytime sleepiness.
In 1999, a research team working with canine models identified a gene that causes narcolepsy–a breakthrough that brings a cure for this disabling condition within reach. The gene, hypocretin receptor 2, codes for a protein that allows brain cells to receive instructions from other cells. The defective versions of the gene encode proteins that cannot recognize these messages, perhaps cutting the cells off from messages that promote wakefulness. The researchers know that the same gene exists in humans, and they are currently searching for defective versions in people with narcolepsy.
The Future
Sleep research is expanding and attracting more and more attention from scientists. Researchers now know that sleep is an active and dynamic state that greatly influences our waking hours, and they realize that we must understand sleep to fully understand the brain. Innovative techniques, such as brain imaging, can now help researchers understand how different brain regions function during sleep and how different activities and disorders affect sleep. Understanding the factors that affect sleep in health and disease also may lead to revolutionary new therapies for sleep disorders and to ways of overcoming jet lag and the problems associated with shift work. We can expect these and many other benefits from research that will allow us to truly understand sleep's impact on our lives.
Choosing the Right Sleep Medicines, or None at All
By Peter Jaret : NY Times Article : August 7, 2008
In Brief:
The safety of insomnia drugs has improved steadily over the past 30 years.
Choosing the right sleep medication is important; some are best at helping people fall asleep, while others help people stay asleep through the night.
Although medications are often recommended for acute insomnia, the first line of treatment for chronic insomnia is behavioral therapy.
Insomniacs know all too well what it’s like to lie awake in a tangle of sheets, the day’s worries parading through the brain as the minutes tick past with agonizing slowness. With studies linking troubled sleep to a variety of health problems including heart attacks and obesity, it’s enough to keep anyone awake at night.
An estimated 30 million Americans wrestle with chronic insomnia. Many suffer in silence. A 2005 National Sleep Foundation survey found that only one-third of patients with insomnia were asked by their primary care physicians about the quality of their sleep. Insomnia sufferers are equally unlikely to raise the issue with their doctors, studies show. And that’s too bad, experts say.
More and safer medications for sleep problems are available. And with a growing list to choose from, doctors can target prescriptions more precisely to specific complaints: trouble falling asleep, for instance, versus trouble staying asleep.
Remedies to help people fall asleep have been around for centuries, from laudanum in the 1800s to barbiturates more recently. “Unfortunately, most of them were addictive and potentially deadly,” said Dr. David Neubauer, associate director of the Sleep Disorders Center at Johns Hopkins University School of Medicine in Baltimore. “The history of sleep medications is really a tale of improving safety.”
A big advance came in the 1970s with the introduction of benzodiazepine drugs like Halcion, Xanax and Restoril. Although far safer than barbiturates, these sleep medications can still cause dependence and withdrawal symptoms like rebound insomnia. That prompted the Food and Drug Administration to approve them only for short-term use, usually no more than two weeks.
The same restrictions remained in place when a new generation of hypnotic drugs, known as nonbenzodiazepines or “Z” drugs, hit the market, starting with Ambien in the early 1990s.
“But it soon became evident that Ambien was really quite different, that it didn’t have the same withdrawal effects or dependency,” said Dr. Michael Thorpy, director of the Sleep-Wake Disorders Center at Montefiore Medical Center in the Bronx.
In one recent study, researchers at Duke University Medical Center pitted Ambien-CR, a controlled-release formulation, against a placebo. After taking the drug for six months, volunteers reported no rebound insomnia when they stopped. Almost 90 percent said the drug helped them sleep, compared with just under 60 percent of the placebo group. Those on the active drug also reported less morning sleepiness and greater ability to concentrate during the day.
Newer nonbenzodiazepines like Lunesta and Sonata have no restrictions on how long they can be used. Even so, they remain on the federal list of controlled substances because of their potential for abuse.
The latest sleeping pill to win F.D.A. approval, called Rozerem, is the first sleeping pill not on that list, because there appears to be little chance it will be abused. The drug, which targets receptors in the brain for the sleep hormone melatonin, represents the first new class of sleep medication in several decades.
Safer sleep medicines are particularly welcome for people whose insomnia is caused by chronic pain or other persistent medical conditions, Dr. Thorpy said. “These are people who are never going to get a good night’s sleep without medication, and who may need hypnotics for the rest of their lives,” he said.
But those people are the exceptions — most insomniacs will not require pills indefinitely. Indeed, medications are generally considered the first-line treatment not for chronic sleep problems but for acute, short-term insomnia brought on by, say, unusual stress at work or the aftermath of surgery.
“Medications can help nip insomnia in the bud, and may prevent it from becoming a chronic problem,” said Wilfred Pigeon, assistant professor of psychiatry at the Sleep and Neurophysiology Research Laboratory at the University of Rochester.
Doctors are increasingly exploiting the differences among nonbenzodiazepines to tailor their prescription to particular sleep complaints.
Chief among these differences is a drug’s half-life, a measure of how long the active ingredients remain in the body, which can range from one to seven hours for the top sleep aids. If the problem is falling asleep, a drug with a short half-life, like Sonata or Rozerem, may be the best choice. If a patient complains about waking in the middle of the night, a medicine with a longer half-life, like Ambien-CR or Lunesta, may work best.
Although the F.D.A. has not yet approved sleeping pills specifically to be taken when people find themselves wide awake in the middle of the night, “many people take Sonata that way, because it has a very short half-life,” Dr. Thorpy said.
A 2006 study by researchers at the Clinilabs Sleep Disorders Institute at St. Luke’s-Roosevelt Hospital Center in New York found that Sonata taken in the middle of the night caused less next-day sleepiness than Ambien, a drug with a longer half-life.
But even the newer sleep medicines have side effects, including reports of people having no memory of raiding the refrigerator or getting behind the wheel the night before. And because sleep medications address only the symptoms of insomnia and not the causes, many experts agree that the best approach when sleep problems persist is cognitive-behavioral therapy, which teaches strategies like better sleep habits and restricting the amount of time spent awake in bed.
“Drugs can help relieve people’s acute anxiety about being able to fall asleep or stay asleep,” Dr. Pigeon said. Behavioral approaches, which in practice are often combined with sleep drugs, “help make lasting changes in the quality of people’s sleep,” he said.
But changing sleep habits takes time, and a shortage of therapists trained in behavioral sleep medicine means that option is not available to everyone who might benefit. Harried physicians often find it easier to write out a prescription than to discuss sleep hygiene with patients, who likewise often seek the quick relief offered by pills.
Small wonder that pharmaceutical researchers are continually in search of novel insomnia drugs. One drug under development, for example, works in a new way to enhance slow-wave sleep, the deepest stage of slumber, with a goal of making people feel more refreshed in the morning.
“People come in complaining about their sleep,” Dr. Neubauer said. “But of course what we’re really looking for is better wakefulness.”
Tips for a Good Night's Sleep:
Adapted from "When You Can't Sleep: The ABCs of ZZZs," by the National Sleep Foundation.
- Set a schedule:
- Exercise:
- Avoid caffeine, nicotine, and alcohol:
- Relax before bed:
- Sleep until sunlight:
- Don't lie in bed awake:
- Control your room temperature:
- See a doctor if your sleeping problem continues:
Sleep Apnea ........An Overview
Obstructive sleep apnea is a condition in which a person has episodes of stopped breathing during sleep.
See also:
Alternative Names Sleep apnea - obstructive; Apnea - obstructive sleep apnea syndrome
Causes » Normally, the muscles of the upper part of the throat help keep the airway open and allow air to flow into the lungs. Even though these muscles usually relax during sleep, the upper throat remains open enough to let air pass by.
However, some people have a narrower throat area, and, during sleep, relaxation of the muscles causes the passage to completely close. This prevents air from getting into the lungs. Loud snoring and labored breathing occur. During deep sleep, breathing can stop for a short period of time (often more than 10 seconds). This is called apnea.
An apnea episode is followed by a sudden attempt to breathe, and a change to a lighter stage of sleep. The result is fragmented sleep that is not restful, leading to excessive daytime drowsiness.
Older obese men seem to be at higher risk, although as many as 40% of people with obstructive sleep apnea are not obese. The following factors may also increase your risk for obstructive sleep apnea:
- Certain shapes of the palate and jaw
- Large tonsils and adenoids in children
- Large neck or collar size
- Large tongue
- Narrow airway
- Nasal obstruction
- Recent weight gain
In-Depth Causes »
Symptoms » It is important to emphasize that, often, the person who has obstructive sleep apnea does not remember the episodes of apnea during the night. The main symptoms are usually associated with excessive daytime sleepiness due to poor sleep during the night. Often, family members, especially spouses, witness the periods of no breathing.
A person with obstructive sleep apnea usually snores heavily soon after falling asleep. The snoring continues at a regular pace for a period of time, often becoming louder, but is then interrupted by a long silent period during which there is no breathing. This is followed by a loud snort and gasp, and the snoring returns. This pattern repeats frequently throughout the night.
Symptoms that may be observed include:
- Abnormal daytime sleepiness, including falling asleep at inappropriate times
- Awakening unrefreshed in the morning
- Depression (possibly)
- Episodes of no breathing (apnea)
- Lethargy
- Loud snoring
- Memory difficulties
- Morning headaches
- Personality changes
- Poor concentration
- Restless sleep
- Hyperactive behavior, especially in children
- Leg swelling (if severe)
Exams and Tests » The health care provider will perform a physical exam. This will involve carefully checking your mouth, neck, and throat. You will be asked about your medical history. Often, a survey that asks a series of questions about daytime sleepiness, sleep quality, and bedtime habits is given.
A sleep study (polysomnogram) is used to confirm obstructive sleep apnea.
Other tests that may be performed include:
- Arterial blood gases
- Electrocardiogram (ECG)
- Echocardiogram
- Thyroid function studies
Treatment » The goal is to keep the airway open so that breathing does not stop during sleep.
The following may relieve symptoms of sleep apnea in some individuals:
- Avoiding alcohol or sedatives at bedtime
- Dental devices inserted into the mouth at night to keep the jaw forward
- Weight management or weight loss
Surgery may be an option in some cases. This may involve:
- Uvulopalatopharyngoplasty (UPPP) to removing excess tissue at the back of the throat
- Tracheostomy to create an opening in the windpipe to bypass the blocked airway if anatomical causes are present (rarely done)
In-Depth Treatment »
Outlook (Prognosis) When treated correctly, obstructive sleep apnea may be controlled. However, many patients are unable or unwilling to tolerate CPAP therapy.
Possible Complications During the nonbreathing episodes, blood oxygen levels falls. Persistent low levels of oxygen (hypoxia) may cause many of the daytime symptoms. If the condition is severe enough, pulmonary hypertension may develop, leading to right-sided heart failure or cor pulmonale.
Other complications include:
- Abnormal heart rhythm (arrhythmia)
- Excessive carbon dioxide levels in the blood
- Heart disease
- High blood pressure
- Sleep deprivation
Snoring:
What to Do When a Punch in the Shoulder Fails
By Walecia Konrad : NY Times article : December 10, 2010
Dr. Elizabeth Walton, a 43-year-old internist in Atlanta and the mother of twin 4-year-old boys, has a common, if sometimes embarrassing, health problem. She snores — loudly. And she has tried to fix it with a variety of things, including a machine that blows air down her throat and an oral appliance that looks something like a mouthguard worn by a hockey player.
The appliance works, and Dr. Walton is finally sleeping more easily. (So is her partner.) And because she was told she had obstructive sleep apnea, a more serious disorder than simple snoring, her treatments have been mostly covered by insurance.
Still, she estimates she has spent hundreds of dollars in deductibles, co-payments and fees.
Dr. Walton would have preferred not to go through so much expensive trial and error: “Unfortunately, it’s the nature of this condition.”
Almost half of the adult population snores at least occasionally. Snoring occurs when air flows past relaxed tissues in the throat, causing them to vibrate. Nasal congestion can also contribute to the racket.
“We laugh and joke about snoring,” said Dr. Nancy A. Collop, president elect of the American Academy of Sleep Medicine, “but it can be pretty annoying and disruptive to couples.”
What’s more, while ordinary snoring in itself does not present health problems, it may be a sign of a sleep apnea, as it was in Dr. Walton’s case. Patients suffering from sleep apnea have airways that are so obstructed they stop or nearly stop breathing during sleep.
The lack of oxygen wakens them, usually with a gasp, frequently during the night. “All people with sleep apnea snore,” said Dr. Collop, “but not all people who snore have sleep apnea.”
If you find you suffer from plain old snoring and not sleep apnea, do not expect insurance to cover your treatments. How far you decide to go will depend on a combination of what you and your spouse are comfortable with, what works for you and what you can afford.
Here are a few ways to determine which treatment is right for you or the loud sleeper in your family:
THE GIMMICKS
Search for snoring remedies on the Web and you will find dozens of products, including special pillows, mouth and nose devices, special throat exercises and even advice on learning to play the didgeridoo, a wind instrument, to strengthen throat muscles and tissues. By and large, these products are marketed without much evidence of results.
“For the most part, you can save your money,” said Dr. Collop. Instead, she and other sleep experts recommend that most patients start with lifestyle changes that may reduce or eliminate snoring. All are free or low-cost.
¶Lose weight.
Extra weight can restrict throat tissue and cause snoring, so losing weight is often advised for overweight snorers.
¶Sleep on your side.
When you lie on your back, the base of your tongue and soft palate fall to the back wall of your throat, often causing snoring.
¶Avoid alcohol before bed.
Alcohol or sedatives can relax throat muscles and make snoring worse. Avoiding alcohol three or four hours before going to sleep can help, said Dr. Collop.
¶Clear nasal passages.
This is relevant only for people whose snoring starts in their noses. Take a hot shower before bed, or use a saline solution to help clear nasal passages. Check for allergens and dust mites in your bedroom, especially if you are congested only at night. Over-the-counter nasal strips that you put on the outside of your nose before bed may also help. They cost $10 to $12 for a pack of 30.
If none of this eases your snoring, you will need to see a doctor to be evaluated for sleep apnea. About 50 percent of people who snore loudly have the condition. Other symptoms include daytime sleepiness and extensive fatigue.
A SLEEP STUDY
To find out if you have sleep apnea, you will most likely need to spend the night in a sleep clinic, where specialists will track your blood oxygen levels, breathing and other movements to see if you are waking frequently at night.
These tests are often covered by insurance if your doctor suspects sleep apnea. They can cost from $1,500 to $3,000, depending on where you live and how extensive your study is.
If you do not have insurance coverage or you cannot afford the co-pay, ask your doctor about performing some of the tests at home with special equipment. If you must go to a sleep lab without coverage, ask for a price similar to what an insurer would pay, not what you would be billed as a private patient.
THE MASK
One of the most effective treatments for sleep apnea, continuous positive airway pressure, or CPAP, pronounced SEE-pap, also eliminates garden-variety snoring. But since it is a pressurized mask that forces cold air to the lungs, many patients find it uncomfortable or annoying and end up abandoning the treatment. With a price tag ranging from $1,500 to $2,500 for a CPAP machine, that can be an expensive experiment, especially for uninsured patients.
If you use a CPAP machine, do not give it up without talking to your doctor. He or she may be able to make the device more comfortable by adding a heated humidifier. There are also some newer, more advanced versions that apply less pressure and may be more comfortable.
ORAL APPLIANCES
These are form-fitting mouthguards that usually move your lower jaw forward to increase space around your airways. One of these devices finally worked for Dr. Walton.
A dentist who specializes in sleep medicine fits an appliance to your mouth, usually for $1,500 to $3,000. That price should include all follow-up visits and any adjustments that need to be made, said Dr. Sheri Katz, president of the American Academy of Dental Sleep Medicine.
Studies show that custom-fit appliances ease mild to moderate sleep apnea in about 75 percent of patients and snoring in 80 to 90 percent of patients who use them regularly, said Dr. Katz. Dental insurance rarely covers the devices, but medical insurance often will if they are used to treat sleep apnea.
THE LAST RESORT
Removal of excess tissue in the throat and nose, whether it is through traditional surgery or newer methods, is a fairly drastic and expensive step. Some procedures can be painful and cause serious side effects.
In a procedure called uvulopalatopharyngoplasty, a surgeon trims and tightens excess tissue in the airway while you are under general anesthetic.
In an outpatient procedure called laser-assisted uvulopalatoplasty, a laser is used to remove your uvula and shorten your soft palate. This procedure has not been proven to improve sleep apnea, but it is used to get snoring under control.
Two newer procedures are available. Somnoplasty relies on radio frequency to remove some of the soft palate. This is also done on an outpatient basis and is generally considered less painful than other snoring surgery. The Pillar procedure involves implanting polyester fibers in the soft palate to stiffen the tissue and decrease vibrations. This is usually done in a doctor’s office under local anesthesia and is less invasive than other surgical treatments.
More data is needed on the long-term effectiveness of the two newer procedures. And like the other treatments discussed, only those surgeries prescribed to help you with a diagnosed case of obstructive sleep apnea will be covered by insurance.
Simple Rules for Better Sleep
By Paula Span : NY Times : January 23, 2011
This sounds way too good to be true: a quick, effective solution to the insomnia that plagues an estimated 15 to 30 percent of older adults — without drugs, without even needing to consult a physician.
A University of Pittsburgh team, testing its method on 79 seniors with chronic insomnia (average age: 72), has reported very encouraging results. The treatment required just two explanatory sessions (the first lasts 45 to 60 minutes, the second about half an hour) with a nurse-practitioner, plus two brief follow-up phone calls, over the course of a month.
Afterward, the researchers recently reported in The Archives of Internal Medicine, two-thirds of those treated reported a clearly measurable improvement in sleep, compared with 25 percent of those in a control group.
“Their total sleep time improved,” the lead author, Dr. Daniel Buysse, a psychiatry professor and sleep specialist, told me in an interview. Indeed, 55 percent of those treated no longer had insomnia at all. And six months later, three-quarters of those tested had maintained or improved their better sleep patterns.
So what was this potential wonder nondrug? That’s the interesting part. The treatment was a “brief behavioral treatment intervention” known to be an effective antidote to insomnia, as documented by extensive research for over 30 years. It’s a change in what you do, not in what you ingest. Emphasis on brief.
“If behavioral treatments are ever to become widespread, they have to be simple and quick and produce noticeable results,” Dr. Buysse explained. “If you don’t see substantial improvement in a month or so, patients’ motivation to persevere will diminish” — which often happens with behavioral treatments offered by clinical psychologists, which generally involve six to eight sessions.
So the researchers distilled those principles into four simple rules, came up with a workbook and sleep diaries to help patients follow them, and trained a nurse-practitioner to explain the regimen and the physiology behind it.
Insomnia, like other sleep disorders, can take a serious toll on seniors’ health. It’s associated with depression, with falls and fractures, with higher mortality — and its prevalence increases with age. So doctors take insomnia seriously and prescribe medications to help patients sleep.
But sedatives can create problems of their own. In older patients, sleep drugs can cause daytime drowsiness and impair memory, and they’re also associated with falls. A review of 24 studies of these “sedative hypnotics” in older people with insomnia, published in the British Medical Journal in 2005, concluded that while the drugs improved sleep, their effects were small and the hazards significant. “In people over 60, the benefits of these drugs may not justify the increased risk,” the researchers wrote.
An intervention not involving drugs would therefore be a great boon to seniors and their caregivers. “In an ideal health care system, one would expect behavioral treatment for insomnia to be widely disseminated because of the data showing efficacy,” not to mention the cost savings from reduced drug use and fewer side effects and injuries, Thomas C. Neylan, a psychiatrist at the University of California, San Francisco, wrote in a commentary accompanying the study.
So why isn’t this method commonly prescribed? Dr. Buysse’s hypothesis: “I believe the biggest barriers are that people think the interventions are complicated and costly. So we really tried to distill the proven techniques into the simplest possible form.” The method will need testing on a larger scale, and nurses or other professionals will need training before they can help patients use it — but not a lot of training. Dr. Buysse estimates that groups of instructors can be prepared with an eight-hour course.
The idea is to stick to a schedule that maximizes your “sleep efficiency” — the amount of time in bed you spend sleeping, instead of tossing and hoping that sleep will descend.
That involves four rules:
The nurse instructing patients in the technique uses diagrams and examples, describes the physiology involved, cautions that people may feel tired and sleep-deprived for the first few weeks but usually go on to deeper, more restful sleep that comes more quickly. Still, that’s about all that needs to be said — not much. In the study, three brochures given to the control group contained a lot of the same information, but just reading about better sleep habits didn’t do the trick.
However obvious the strategy may sound, “the reality is, people gravitate toward the exact opposite behavior,” Dr. Buysse said. “It’s common to see older adults spend 10 or 12 hours in bed in order to get five hours of sleep. It’s very frustrating.”
But it’s also frustrating to think that a potentially safe and effective answer to a widespread problem might once more fail to make its way out of an academic journal and into physicians’ offices and people’s bedrooms. Maybe it needs a jazzier name than “brief behavioral treatment intervention” — something incorporating “Medicare” and “cost-cutting.”
By Paula Span : NY Times : January 23, 2011
This sounds way too good to be true: a quick, effective solution to the insomnia that plagues an estimated 15 to 30 percent of older adults — without drugs, without even needing to consult a physician.
A University of Pittsburgh team, testing its method on 79 seniors with chronic insomnia (average age: 72), has reported very encouraging results. The treatment required just two explanatory sessions (the first lasts 45 to 60 minutes, the second about half an hour) with a nurse-practitioner, plus two brief follow-up phone calls, over the course of a month.
Afterward, the researchers recently reported in The Archives of Internal Medicine, two-thirds of those treated reported a clearly measurable improvement in sleep, compared with 25 percent of those in a control group.
“Their total sleep time improved,” the lead author, Dr. Daniel Buysse, a psychiatry professor and sleep specialist, told me in an interview. Indeed, 55 percent of those treated no longer had insomnia at all. And six months later, three-quarters of those tested had maintained or improved their better sleep patterns.
So what was this potential wonder nondrug? That’s the interesting part. The treatment was a “brief behavioral treatment intervention” known to be an effective antidote to insomnia, as documented by extensive research for over 30 years. It’s a change in what you do, not in what you ingest. Emphasis on brief.
“If behavioral treatments are ever to become widespread, they have to be simple and quick and produce noticeable results,” Dr. Buysse explained. “If you don’t see substantial improvement in a month or so, patients’ motivation to persevere will diminish” — which often happens with behavioral treatments offered by clinical psychologists, which generally involve six to eight sessions.
So the researchers distilled those principles into four simple rules, came up with a workbook and sleep diaries to help patients follow them, and trained a nurse-practitioner to explain the regimen and the physiology behind it.
Insomnia, like other sleep disorders, can take a serious toll on seniors’ health. It’s associated with depression, with falls and fractures, with higher mortality — and its prevalence increases with age. So doctors take insomnia seriously and prescribe medications to help patients sleep.
But sedatives can create problems of their own. In older patients, sleep drugs can cause daytime drowsiness and impair memory, and they’re also associated with falls. A review of 24 studies of these “sedative hypnotics” in older people with insomnia, published in the British Medical Journal in 2005, concluded that while the drugs improved sleep, their effects were small and the hazards significant. “In people over 60, the benefits of these drugs may not justify the increased risk,” the researchers wrote.
An intervention not involving drugs would therefore be a great boon to seniors and their caregivers. “In an ideal health care system, one would expect behavioral treatment for insomnia to be widely disseminated because of the data showing efficacy,” not to mention the cost savings from reduced drug use and fewer side effects and injuries, Thomas C. Neylan, a psychiatrist at the University of California, San Francisco, wrote in a commentary accompanying the study.
So why isn’t this method commonly prescribed? Dr. Buysse’s hypothesis: “I believe the biggest barriers are that people think the interventions are complicated and costly. So we really tried to distill the proven techniques into the simplest possible form.” The method will need testing on a larger scale, and nurses or other professionals will need training before they can help patients use it — but not a lot of training. Dr. Buysse estimates that groups of instructors can be prepared with an eight-hour course.
The idea is to stick to a schedule that maximizes your “sleep efficiency” — the amount of time in bed you spend sleeping, instead of tossing and hoping that sleep will descend.
That involves four rules:
- Reduce the time spent in bed.
- Get up at the same time every day.
- Don’t go to bed until you feel sleepy.
- Don’t stay in bed if you’re not sleeping.
The nurse instructing patients in the technique uses diagrams and examples, describes the physiology involved, cautions that people may feel tired and sleep-deprived for the first few weeks but usually go on to deeper, more restful sleep that comes more quickly. Still, that’s about all that needs to be said — not much. In the study, three brochures given to the control group contained a lot of the same information, but just reading about better sleep habits didn’t do the trick.
However obvious the strategy may sound, “the reality is, people gravitate toward the exact opposite behavior,” Dr. Buysse said. “It’s common to see older adults spend 10 or 12 hours in bed in order to get five hours of sleep. It’s very frustrating.”
But it’s also frustrating to think that a potentially safe and effective answer to a widespread problem might once more fail to make its way out of an academic journal and into physicians’ offices and people’s bedrooms. Maybe it needs a jazzier name than “brief behavioral treatment intervention” — something incorporating “Medicare” and “cost-cutting.”
Medications that can interfere with sleep:
Some medications that have been reported to cause abnormal dreams and other sleep disturbances.
Five foods that can help you sleep:
1. Cherries. Fresh and dried cherries are one of the only natural food sources of melatonin, the chemical that controls the body's internal clock to regulate sleep. Researchers who tested tart cherries and found high levels of melatonin recommend eating them an hour before bedtime or before a trip when you want to sleep on the plane.
2. Bananas. Potassium and magnesium are natural muscle relaxants, and bananas are a good source of both. They also contain the amino acid L-tryptophan, which gets converted to 5-HTP in the brain. The 5-HTP in turn is converted to serotonin (a relaxing neurotransmitter) and melatonin.
3. Toast. Carbohydrate-rich foods trigger insulin production, which induces sleep by speeding up the release of tryptophan and serotonin, two brain chemicals that relax you and send you to sleep.
4. Oatmeal. Like toast, a bowl of oatmeal triggers a rise in blood sugar, which in turn triggers insulin production and the release of sleep-inducing brain chemicals. Oats are also rich in melatonin, which many people take as a sleep aid.
5. Warm milk. Like bananas, milk contains the amino acid L-tryptophan, which turns to 5-HTP and releases relaxing serotonin. It's also high in calcium, which promotes sleep.
Some medications that have been reported to cause abnormal dreams and other sleep disturbances.
- ADHD drugs: Ritalin, Vyvanse, Adderall
- AIDS drugs: Sustiva
- Antianxiety drugs: Cymbalta, Effexor
- Antibiotics: Cipro
- Antidepressants: Tricyclics (Elavil, Tofranil, Remeron); SSRIs (Prozac, Paxil, Lexapro, Celexa);
- Non-tricyclics (Wellbutrin); MAOI inhibitors (Nardil)
- Antihistamines
- Antiseizure drugs: Phenobarbital, Klonopin, Valpax
- Dementia drugs: Aricept, Risperdal, Exelon
- Heart medications: Beta blockers (Tenormin, Nadolol); also Digoxin, Coumadin
- High blood pressure drugs: ACE-inhibitors (Vasotec); calciumchannel blockers (Plendil, Sular, Covera); also: Kapvay, Nexiclon, Cozaar
- Pain relievers: Naproxen, Ketamine, morphine
- Parkinson's disease drugs: Symadine, Symmetrel, Requip
- Schizophrenia drugs: Clozapine, Risperdal, Zyprexa
- Sleep Aids: Restoril, Halcion, Ambien, Lunesta
- Smoking-cessation drugs: Chantix, nicotine patches, Zyban
- Statins: Lipitor, Zocor, Crestor
Five foods that can help you sleep:
1. Cherries. Fresh and dried cherries are one of the only natural food sources of melatonin, the chemical that controls the body's internal clock to regulate sleep. Researchers who tested tart cherries and found high levels of melatonin recommend eating them an hour before bedtime or before a trip when you want to sleep on the plane.
2. Bananas. Potassium and magnesium are natural muscle relaxants, and bananas are a good source of both. They also contain the amino acid L-tryptophan, which gets converted to 5-HTP in the brain. The 5-HTP in turn is converted to serotonin (a relaxing neurotransmitter) and melatonin.
3. Toast. Carbohydrate-rich foods trigger insulin production, which induces sleep by speeding up the release of tryptophan and serotonin, two brain chemicals that relax you and send you to sleep.
4. Oatmeal. Like toast, a bowl of oatmeal triggers a rise in blood sugar, which in turn triggers insulin production and the release of sleep-inducing brain chemicals. Oats are also rich in melatonin, which many people take as a sleep aid.
5. Warm milk. Like bananas, milk contains the amino acid L-tryptophan, which turns to 5-HTP and releases relaxing serotonin. It's also high in calcium, which promotes sleep.
Five foods that can "prevent" you from getting a good night's rest:
1. Preserved and smoked meats. Slap your hand away when it reaches to make a ham sandwich as an evening snack. Ham, bacon, sausages, and smoked meats contain high levels of the amino acid tyramine, which triggers the brain to release norepinephrine, a brain stimulant that makes us feel alert and wired.
2. Chocolate. Love an evening cup of cocoa? That sundae in front of the TV? Be careful of chocolate in all its disguises. Many people are increasingly sensitive to caffeine as they get older, and even the little chocolate chunks in chocolate chip ice cream could zap you just enough to prevent ZZZZs. Chocolate also contains tyrosine, a stimulating amino acid.
3. Energy drinks. Red Bull and other energy drinks are high in caffeine as well as the amino acid taurine, which boosts alertness and adrenaline. Recent studies have shown that even if you drink energy drinks early in the day, the combined high dosage of taurine and caffeine can make it hard to sleep, or to sleep well, later on.
4. Tomato sauce, chili, pizza, and spicy foods. Digestive disturbances are a common source of sleep problems, but many people fail to make the connection. Acidic and spicy foods can cause reflux, heartburn, and other symptoms that interrupt sleep.
5. The nightcap. A drink or two may make you feel more relaxed after dinner, but it comes back to haunt you -- literally -- a few hours later, by preventing you from achieving deep sleep. And because alcohol both dehydrates you and makes you have to pee, it wakes you up, too. Wine is high in the stimulant tyrosine as well.
Getting back to sleep if you awaken during the night
First off, it's important to understand that as we get older, our bodies' ability to hold fluids for long periods decreases, thanks to a decline in antidiuretic hormones. So even though we're drinking the same amount, we have to go the bathroom more often. This is why middle-of-the-night bathroom runs become so common as we age. (According to the National Sleep Foundation, 65 percent of older adults have sleep deprivation resulting from waking up frequently to use the bathroom.)
Since our bodies are losing the ability to hold fluids -- and since aging also makes it more difficult to fall back asleep after we wake up -- the best solution to this problem is to try not to wake up in the first place.
Here are strategies that can help relieve pressure on the bladder and prevent other digestive symptoms:
*Don't drink liquids for three hours before bedtime.
*Cut down consumption of coffee and tea, which irritate the bladder.
*Don't eat foods with high liquid content, such as soup or fruit, for dinner or after dinner.
*Don't eat for the three hours before going to sleep if you're prone to heartburn or gastric reflux.
A prescription antidiuretic can cut down on nighttime urination if this is the only problem.
However, it's also possible that a separate health condition is leading to the nocturnal bathroom problem. In men, frequent urination at night is often a sign of prostate trouble. Inflammation of the prostate, benign prostatic hyperplasia (BPN), and prostate tumors can all cause this symptom, so call your doctor for a prostate exam and PSA test if nighttime waking to urinate suggests a possible prostate condition.
In women, frequent urination can go hand in hand with urinary issues such as incontinence, overactive bladder, urinary tract infections, or cystitis. So, women, you'll also need to see your doctor for a checkup if you suspect any of these problems.
Urinary tract problems such as overactive bladder can be helped with Kegel exercises -- both men and women can learn these exercises to strengthen the muscles at the neck of the bladder.
Once you're awake, a separate set of issues ensues. You may have developed some habits that work against your return to slumber. Here are some suggestions for getting back to sleep quickly:
*Keep the room dark. If you typically have to get up at least once during the night, keep a small book light or mini flashlight next to your bed and use it to navigate your way to the bathroom. Or put a dim night-light in the bathroom and leave the door cracked, so you can use the sliver of light to find your way there. Whatever you do, don't turn on the overhead light in the bathroom once you're there.
*Don't give in to the temptation to turn on the TV or computer. The idea that watching TV can soothe you back to sleep is a misconception; TV and computers function as stimulants. The light from the screen "resets" your internal clock and makes it harder for you to fall back asleep.
*Don't eat unless you're truly hungry. If you're sure a growling stomach is going to keep you awake, have a small snack. Otherwise, getting your digestive system revved up can keep you awake.
*Keep a pen and paper next to your bed. If you're often kept awake by your mind racing or by the common tendency to worry and make to-do lists in your head, keep a pen or pencil and a small pad of paper by your bed and write down your list. As you put each item down on paper, imagine yourself setting aside that concern. (Again, use a book light; don't turn on the overhead or a bright bedside light to write.)
*Do a simple isolation and relaxation exercise. If your body feels tense once you lie down again, try to relax methodically. Starting with your feet, tense the muscles as hard as you can, then relax completely. Do the same with your calves, thighs, buttocks, hands, arms, and on up. By the time you get to your neck and head, you should have banished much of the tension.
*Use an eye mask and ear plugs if noise and shadows are keeping you awake. Some people find that when they wake in the middle of the night, they're much more sensitive to light and sound than they are in the evening, so they need to take steps to block out as many stimuli as possible.
Waking up to urinate more than once a night can also be one of the indicators for sleep apnea. If the problem persists, ask your doctor to evaluate you for sleep apnea or Upper Airway Resistance Syndrome, a milder breathing issue associated with sleep disorder. It's possible that what's happening is that a breathing problem is waking you up or causing you to sleep lightly, which in turn makes you aware of the need to go to the bathroom. While you feel as if you have a full bladder, you would have been able to sleep through the night if you hadn't awakened in the first place.
First off, it's important to understand that as we get older, our bodies' ability to hold fluids for long periods decreases, thanks to a decline in antidiuretic hormones. So even though we're drinking the same amount, we have to go the bathroom more often. This is why middle-of-the-night bathroom runs become so common as we age. (According to the National Sleep Foundation, 65 percent of older adults have sleep deprivation resulting from waking up frequently to use the bathroom.)
Since our bodies are losing the ability to hold fluids -- and since aging also makes it more difficult to fall back asleep after we wake up -- the best solution to this problem is to try not to wake up in the first place.
Here are strategies that can help relieve pressure on the bladder and prevent other digestive symptoms:
*Don't drink liquids for three hours before bedtime.
*Cut down consumption of coffee and tea, which irritate the bladder.
*Don't eat foods with high liquid content, such as soup or fruit, for dinner or after dinner.
*Don't eat for the three hours before going to sleep if you're prone to heartburn or gastric reflux.
A prescription antidiuretic can cut down on nighttime urination if this is the only problem.
However, it's also possible that a separate health condition is leading to the nocturnal bathroom problem. In men, frequent urination at night is often a sign of prostate trouble. Inflammation of the prostate, benign prostatic hyperplasia (BPN), and prostate tumors can all cause this symptom, so call your doctor for a prostate exam and PSA test if nighttime waking to urinate suggests a possible prostate condition.
In women, frequent urination can go hand in hand with urinary issues such as incontinence, overactive bladder, urinary tract infections, or cystitis. So, women, you'll also need to see your doctor for a checkup if you suspect any of these problems.
Urinary tract problems such as overactive bladder can be helped with Kegel exercises -- both men and women can learn these exercises to strengthen the muscles at the neck of the bladder.
Once you're awake, a separate set of issues ensues. You may have developed some habits that work against your return to slumber. Here are some suggestions for getting back to sleep quickly:
*Keep the room dark. If you typically have to get up at least once during the night, keep a small book light or mini flashlight next to your bed and use it to navigate your way to the bathroom. Or put a dim night-light in the bathroom and leave the door cracked, so you can use the sliver of light to find your way there. Whatever you do, don't turn on the overhead light in the bathroom once you're there.
*Don't give in to the temptation to turn on the TV or computer. The idea that watching TV can soothe you back to sleep is a misconception; TV and computers function as stimulants. The light from the screen "resets" your internal clock and makes it harder for you to fall back asleep.
*Don't eat unless you're truly hungry. If you're sure a growling stomach is going to keep you awake, have a small snack. Otherwise, getting your digestive system revved up can keep you awake.
*Keep a pen and paper next to your bed. If you're often kept awake by your mind racing or by the common tendency to worry and make to-do lists in your head, keep a pen or pencil and a small pad of paper by your bed and write down your list. As you put each item down on paper, imagine yourself setting aside that concern. (Again, use a book light; don't turn on the overhead or a bright bedside light to write.)
*Do a simple isolation and relaxation exercise. If your body feels tense once you lie down again, try to relax methodically. Starting with your feet, tense the muscles as hard as you can, then relax completely. Do the same with your calves, thighs, buttocks, hands, arms, and on up. By the time you get to your neck and head, you should have banished much of the tension.
*Use an eye mask and ear plugs if noise and shadows are keeping you awake. Some people find that when they wake in the middle of the night, they're much more sensitive to light and sound than they are in the evening, so they need to take steps to block out as many stimuli as possible.
Waking up to urinate more than once a night can also be one of the indicators for sleep apnea. If the problem persists, ask your doctor to evaluate you for sleep apnea or Upper Airway Resistance Syndrome, a milder breathing issue associated with sleep disorder. It's possible that what's happening is that a breathing problem is waking you up or causing you to sleep lightly, which in turn makes you aware of the need to go to the bathroom. While you feel as if you have a full bladder, you would have been able to sleep through the night if you hadn't awakened in the first place.
Treating Sleep Apnea Without the Mask
By Ahanad O'Connor : NY Times : April 9, 2012
Joseph A. Golish, M.D.A new C.P.A.P. device has two small plugs that create just enough air pressure to keep the airways open at night.About 28 million Americans have sleep apnea, which causes repeated awakenings and pauses in breathing during the night, sometimes resulting in loud snoring and gasps for air. For decades, the standard treatment has been “continuous positive airway pressure.” A mask worn at night pushes air into the nasal passages, enabling easier breathing. C.P.A.P. reduces and in some cases completely prevents episodes of apnea. But the mask is like something from a bad science fiction movie: big, bulky and obtrusive. Many patients simply refuse to wear it or rip it off while asleep. Studies show that about half of all people prescribed C.P.A.P. machines stop using them in one to three weeks.
“For a lot of people out there, the C.P.A.P. machine turns into a doorstop,” said Dr. Joseph Golish, the former chief of sleep medicine at the Cleveland Clinic. “C.P.A.P. is very effective in the sleep lab. But when people go home, there’s a good chance they won’t use it, and the success rate of an unused C.P.A.P. machine is absolutely zero.”
Now an alternative form of C.P.A.P. is gaining popularity: a patch that fits over the nostrils. Called Provent, the patch holds two small plugs, one for each nostril, that create just enough air pressure to keep the airways open at night. It is far less intrusive than the traditional C.P.A.P. machine. It is also more expensive, and it doesn’t work for every patient.
Approved by the Food and Drug Administration in 2008, Provent has spread mostly by word of mouth. But it has caught on fast. Its manufacturer, Ventus Medical, says it has shipped one million of the devices in the past 12 months, up from a half million total in the two years prior. Doctors say it has given them a new weapon in the battle against sleep apnea, and many patients who struggled with C.P.A.P. call it a godsend.
Bob Bleck, who owns a computer networking firm in Ohio, struggled with poor sleep and chronic fatigue for decades. But it was only a year and a half ago that he finally went to a sleep clinic, prodded by his wife, who worried about his heavy snoring.
The diagnosis was severe sleep apnea. Tests showed that in a typical night, Mr. Bleck, 47, awoke or stopped breathing 42 times an hour.
His doctor prescribed a C.P.A.P. machine, and Mr. Bleck hated it.
“I had this constricted feeling,” he said. “It would be incorporated into these dreams where I was tied up, like in the movie ‘Alien.’ It was more difficult to sleep with that thing on then to just get through the night with the apnea.”
Mr. Bleck got rid of the machine after he discovered Provent. “After I started using it, I noticed a difference right away,” he said. “My symptoms subsided dramatically.”
Provent works like a traditional C.P.A.P. machine but is only a fraction of the size. When people with apnea fall asleep, their throat muscles collapse, constricting the airway and causing the body to fight for air. C.P.A.P. machines use mild air pressure to keep the airway from constricting.
Provent does too, but in a different way. The device contains two pinhole-size valves, one over each nostril. The valves let air in easily — most people breathe through their nostrils while asleep — but there is resistance as the user exhales. That resistance creates a backpressure in the airways, dilating the muscles that would otherwise collapse in the middle of the night. In the morning, the patch is removed; a new one is used every night.
Last year, in a large study of 250 apnea sufferers published in the medical journal Sleep and subsidized by Ventus, researchers found that those who used Provent devices over a three-month period saw their apnea episodes fall sharply, compared with people who were given a sham, or placebo, device. A follow-up study tracked people over the course of a year and had similar results.
But not everyone finds that Provent alleviates their apnea. In interviews, sleep specialists said that a third or more of patients do not end up using it.
“It works like a champ in some people and doesn’t work on other people,” said Dr. Nancy Appelblatt, an ear, nose and throat surgeon in Sacramento who has prescribed it to about 100 patients. “All sleep apnea is not created equal.”
Some people, for example, breathe through the mouth at night, not the nostrils. In those people, Provent typically doesn’t work. Nor will it work very well in someone who has severe nasal allergies and has a blocked nose at night, said one of the leaders of the Provent studies, Dr. Meir H. Kryger, a professor at Yale Medical School and founder of the National Sleep Foundation.
Unlike C.P.A.P., Provent is not covered by Medicare and most major insurers, though some doctors say they expect that will change in the near future. In the meantime, a 30-day supply of the patches costs $65 to $80.
Dr. Lee A. Surkin, a cardiologist and sleep medicine specialist in Greenville, N.C., said patients typically start with a 10-day trial pack that costs $10. He has prescribed Provent to about 300 of his patients.
“The No. 1 reason people don’t continue it is the out-of-pocket expense,” he said.
For now, Dr. Kryger and others say that C.P.A.P. will continue to be the gold standard, and certainly the first option for patients with severe apnea. But for the roughly 50 percent of patients in whom C.P.A.P. fails, Provent may be a reliable alternative.
Dr. Surkin said some patients use C.P.A.P. at home, but take their pocket-size Provent patches with them when they travel to avoid the hassle of lugging a machine through airports.
“To me, it’s a miracle,” said Joyce Nemoga, 64. Ms. Nemoga, who lives in Baldwin Harbor, N.Y., has moderate apnea that caused her to snore and gasp in her sleep. She tried C.P.A.P. but could not sleep comfortably with the device.
“Every time you turn over, you have to take the hose with you,” she said. “I tried it for six months, and I don’t think I had one full night of sleep the whole time.”
A doctor suggested Provent, and Ms. Nemoga saw quick results.
“I’m just so happy that I found it,” she said.
For sleep studies I recommend either of the following:
Boston SleepCare Center
85 1st Avenue
Waltham, MA 02451-1105
(781) 895-7960
NeuroCare Center for Sleep
70 Wells Avenue
Newton, MA 02459-3233
(800) 432-8808
The A-to-Z Cure
By Roz Chast : NY Times Article : March 8, 2010
One thing I do when I can’t sleep is play alphabet games. I try to list various things from A to Z: countries, rock groups, prescription drugs, movies, books, celebrities whose first and last names begin with the same letter… you get the idea. I don’t mind repeating categories from one night to another. Diseases might seem to be an unlikely insomnia game category, but for some reason, it’s one of my favorites. I like to combine ailments that terrified me in childhood (lockjaw) with ones that I didn’t know about until I was an adult (Ebola). And there are certain ailments that are never, ever on the list. Ever.
Roz Chast began contributing to The New Yorker in 1978 and became a staff cartoonist in 1979. Since then, she has contributed over 1,000 drawings and several covers to the magazine.
By Roz Chast : NY Times Article : March 8, 2010
One thing I do when I can’t sleep is play alphabet games. I try to list various things from A to Z: countries, rock groups, prescription drugs, movies, books, celebrities whose first and last names begin with the same letter… you get the idea. I don’t mind repeating categories from one night to another. Diseases might seem to be an unlikely insomnia game category, but for some reason, it’s one of my favorites. I like to combine ailments that terrified me in childhood (lockjaw) with ones that I didn’t know about until I was an adult (Ebola). And there are certain ailments that are never, ever on the list. Ever.
Roz Chast began contributing to The New Yorker in 1978 and became a staff cartoonist in 1979. Since then, she has contributed over 1,000 drawings and several covers to the magazine.