- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
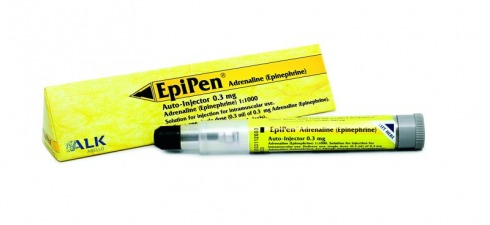
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
ALLERGIES
The Season's Public Enemies
With Trees Shedding Pollen Early, Allergy Sufferers Are in for Unusually Severe Symptoms
Laura Landro : WSJ : March 13, 2012
Jeffrey Bryant is used to the discomforts of hay fever in spring, when trees normally bloom in his hometown of Louisville, Ky. This year was different: Mr. Bryant felt his symptoms come on with a vengeance when it was still January.
"It's never been as bad as this and never started as early," Mr. Bryant says. The 48-year-old computer programmer usually relies on medications to ease his coughing, sneezing and other symptoms. Now, he is working with his doctor to get started on a series of shots that he hopes will control his allergies within a few weeks.
Mild winter temperatures in many parts of the country—the fourth warmest winter since record-keeping began—have triggered an unusually early release of pollen from trees. That bodes badly for the millions of people who suffer from allergic rhinitis—commonly known as hay fever.
Allergists are predicting a longer, and more intense, allergy season than normal. Once people have been exposed to the early pollen, essentially priming the immune system to react to the allergens, there is little chance of relief even if temperatures cool down again. This priming effect can bring on even more severe symptoms for allergy patients, especially those with asthma, says Neil Kao, an allergist in Greenville, N.C.
Medications, including eye drops, antihistamines and nasal sprays, can relieve hay-fever symptoms for many people. For greatest effect, these products usually need to be used just before any exposure to pollen, says Stanley Fineman, an allergy specialist in Marietta, Ga. But this year "we didn't catch it in time because we didn't know the pollen was going to start so early," says Dr. Fineman, who also is president of the American College of Allergy, Asthma & Immunology, which represents allergists. Weather websites often signal when local pollen counts start to rise.
More aggressive treatments, including immune-boosting allergy shots, are also available, and specialists expect more patients may pursue these remedies this year if their symptoms are worse than normal.
Different pollens serve as triggers to different people. Allergy shots, which administer escalating doses of the offending allergens, work like a vaccine to create resistance in the patient. But these can take several months to become effective. Doctors increasingly are recommending faster treatment protocols that deliver the shots over a shorter period and can bring relief within a few weeks.
Allergists also may offer the same type of immunotherapy in the form of drops under the tongue, which patients can use at home after an initial visit. Pharmaceutical firms are developing immunotherapy tablets, to be taken orally, including one from Merck & Co . that has been shown in trials to reduce symptoms of ragweed allergy.
Other researchers are investigating new methods to give patients faster and more effective allergy relief, such as delivering the allergens through the skin or by way of the lymph nodes.
As many as 30% of children and up to 40% of adults suffer from seasonal allergies that cause reactions such as sneezing, itching, stuffy nose, and watery eyes. Trees are one of the earliest plants to release pollen, followed later by pollen from grass and flowering plants. For example, high concentrations of tree pollen in Kansas City, Mo., Tuesday came mainly from juniper, elm and maple trees, according to data compiled by the National Allergy Bureau, part of research group American Academy of Allergy, Asthma & Immunology. Ditto for Atlanta, where the top offenders were pine, oak and birch.
Some studies suggest climate change, by promoting longer blooming seasons, may increase the prevalence of certain allergens and the time during which people are exposed to them. Warmer temperatures also can boost concentrations of mold, another allergen that is usually killed by colder weather, says James Sublett, the Louisville allergy specialist treating Mr. Bryant.
Improved medications have been introduced to treat allergy symptoms in recent years, including antihistamines, nasal steroid sprays and drugs that block inflammatory chemicals produced by the body. The products are generally safe and effective. But in a large survey of adults presented at an annual allergy conference in 2006, about a third of respondents said they switched medication either because of a lack of effectiveness or side effects.
Unlike medication, allergy shots can potentially lead to lasting remission of symptoms after three to five years.
The treatment, which is formally known as subcutaneous immunotherapy and is generally covered by health insurance plans, may also help prevent development of asthma and new allergies. The shots are typically given once or twice a week for about five months, after which their frequency is reduced.
Growing in popularity is a faster treatment, known as "cluster" therapy, that involves two to four injections one day a week for three weeks. Patients' own immune systems are mobilized and able to counteract naturally occurring allergens often within a few weeks, says Richard Weber, an allergy specialist at National Jewish Health in Denver. Risks include an increased chance of irritation at the injection site and a possibly serious reaction to the allergen.
Rachel Lowe, a 40-year-old plastic-surgery nurse in Marietta, Ga., recently started cluster shots recommended by Dr. Fineman after her allergies kicked in in early February. "I always dread when everything is in bloom because my allergies are so bad that I need to lock myself indoors sometimes and can't enjoy the spring," she says.
Some physicians are administering drops under the tongue, known as sublingual immunotherapy, that contain the same substances used in shots. The technique has been used since the 1980s in Europe, where it has been shown to produce lasting remissions in long-term use. It doesn't have U.S. regulatory approval, but some doctors give it to patients anyway as an "off-label" use of the substance.
Other doctors steer clear of the technique because insurers typically don't cover it and there are no standards in the U.S. for dosage and duration of treatment, says Linda Cox, an allergist in Fort Lauderdale, Fla. Another concern, she says: potential liability if something goes wrong.
Steven Prager, an allergist in California, says he began offering sublingual immunotherapy two years ago because many patients don't like shots or find multiple office visits inconvenient. He says he develops a formula for the drops for each patient based on the severity of their allergies. The treatments cost about $75 a month.
A Child’s Allergies Are Serious but
Can Be Treated Effectively
By Walecia Konrad : NT Times Article : March 5, 2010
It starts with a telltale sniffle, itchy eyes and an occasional cough. You think your little one is getting a cold, but the cold never comes while the runny nose seems never to leave.
“That could be a sign of allergies,” says Dr. Kevin Weiss, an expert on allergies and president of the American Board of Medical Specialties. Not a surprising diagnosis when you consider that more than 40 percent of children (and 20 to 30 percent of adults) suffer from allergic rhinitis, often simply called allergies. With spring pollen season just around the corner, parents are bound to hear more of those telltale sniffles.
Allergies are no trivial matter. Each year, allergic rhinitis accounts for two million missed school days and $2.3 million in health care costs for children younger than 12. It’s not unusual for allergy sufferers to spend thousands of dollars each year on doctor visits, medications and other products, says Dr. Linda Cox, an allergist practicing in Ft. Lauderdale, Fla., and a former committee chairwoman for the American College of Allergy, Asthma and Immunology
What’s more, Dr. Cox said, allergies left untreated in children can often lead to asthma, a chronic and debilitating pulmonary disease.
For the purposes of this article I’ll focus on allergic rhinitis, particularly among children. (The subject of food allergies may warrant a separate, future column.) The condition can be set off by outside elements like pollen from ragweed, grasses and trees and indoor allergens like dust mites and pet dander.
Combating allergies often requires a multipronged and sometimes costly approach. Here’s what you can do to make sure your child gets the best results.
THE RIGHT DOCTOR
Most allergies can be identified and treated by a pediatrician or family doctor. The doctor will use blood tests and your child’s symptoms to come up with an educated guess on what is causing the problem.
“Mild allergies can be treated without a lot of testing,” Dr. Weiss said. New nondrowsy prescription and over-the-counter medications make it easier to treat symptoms, he added. Your child’s doctor should know which drugs are appropriate for children.
That’s good news, because allergists aren’t always part of an insurer’s network or covered under high-deductible plans.
Nevertheless, an allergist can best treat your child if symptoms become moderate to severe. If your child is extremely uncomfortable, losing sleep or missing a lot of school, and the current medications he or she is using aren’t working, you may need to take the next step. An allergist will most likely do a skin test to pinpoint exactly what your child is allergic to. This is often more precise than the blood tests and is usually covered by insurance.
ELIMINATE THE SOURCE
After you and your child’s doctor have narrowed down the possible culprits, it’s time to reduce or remove the troublemakers. Many of the most effective ways to do this are labor-intensive but low in cost, said Dr. James Sublett, an allergist in Louisville, Ky., and professor of pediatric allergy and immunology at the University of Louisville School of Medicine.
Keep your pet away from carpeted rooms, sleeping areas, upholstered furniture and other places where it becomes difficult or impossible to remove dander. Cats are the animals that cause the most allergy problems, and cat allergen can remain in a house for an average of 20 weeks after an animal is removed.
If you and your doctor suspect dust mites are a problem, remove drapes, stuffed animals, pet bedding, upholstered furniture and even carpeting from the bedroom. Wash linens frequently. Dust with a moist cloth or an electrostatic fabric duster. Both do a better job of actually collecting dust rather than just stirring it around. Remember: dust takes a couple of hours to settle after cleaning and vacuuming.
Tumble-drying stuffed animals on high heat for 20 minutes will also kill dust mites.
Get rid of any pest problems, like roaches or mice. Both can be huge allergy triggers. In addition, keep windows closed during peak allergy season.
CONSIDER IMMUNOTHERAPY
Even after you’ve identified and tried to eliminate the source of your child’s allergies, he or she may still be suffering. If that happens, you may have to go for the shots.
Allergy shots have come in for criticism over the years because, well, they are shots and require repeat visits to the doctor’s office — two things children really don’t like.
And many parents may wonder — in some cases, rightfully, alas — whether the allergy doctor is overdiagnosing allergies and overtreating their children. Dr. Cox argues that allergists get to the root of the cause instead of just treating symptoms. General practitioners can prescribe medicines to treat symptoms without easing the condition, she says. In any case, it is important to get a referral from a pediatrician or family doctor whom you trust to do what’s right for your child.
A new study published last month in the peer-reviewed Annals of Allergy, Asthma and Immunology found that allergy shots, also known as immunotherapy, could actually help eliminate allergy symptoms after only 18 months. What’s more, shots may help save you money in the long run. Among the children with allergic rhinitis studied, shots helped to reduce total health care costs by a third, and prescription drug costs by 16 percent, said Dr. Cox, who was a co-author of the study.
In immunotherapy, an allergist injects a small amount of the allergen into a patient. This prompts the body to make natural antibodies, which naturally increase one’s immunity to the culprit. “It is the only therapy that doesn’t just treat allergy symptoms but tries to get at the cause,” Dr. Cox said.
But because the allergist personally mixes the allergens according to a patient’s needs, the shots are not considered pharmaceuticals and are sometimes not covered by insurance.
The first year of allergy shots, which includes a three-month build-up period during which a child receives injections as often as twice a week until the proper dosage is found, would cost a bit less than $1,000 for the year, according to Dr. Cox. The next year, with twice-a-month injections, would total an estimated $350.
For parents who are uninsured and cannot afford shots for their children, Dr. Cox suggests contacting the state allergy society for a list of allergists and clinics that may offer low or no-cost treatments. (Because there is no clearinghouse for such information, you’ll probably have to do your own Web sleuthing.)
AVOID THE UNNECESSARY
There’s no end to the number of products marketed to allergy sufferers, including air filters, humidifiers, dehumidifiers, ozone machines, mattress and pillow encasements, special breathing masks and more. Many of these products are expensive and some are ineffective. Ozone, for instance, can be a pollutant and actually worsen allergies, Dr. Sublett said.
Several studies show that there are no significant improvements from using mattress and pillow encasements and other allergy-fighting products. The best thing to do is to take the necessary steps to remove allergens like the ones discsponsored by the American College of Allergy, Asthma and Immunology. If you’re covered by an H.M.O. or other health network, you’ll need to ask your primary physician for a referral.
With Trees Shedding Pollen Early, Allergy Sufferers Are in for Unusually Severe Symptoms
Laura Landro : WSJ : March 13, 2012
Jeffrey Bryant is used to the discomforts of hay fever in spring, when trees normally bloom in his hometown of Louisville, Ky. This year was different: Mr. Bryant felt his symptoms come on with a vengeance when it was still January.
"It's never been as bad as this and never started as early," Mr. Bryant says. The 48-year-old computer programmer usually relies on medications to ease his coughing, sneezing and other symptoms. Now, he is working with his doctor to get started on a series of shots that he hopes will control his allergies within a few weeks.
Mild winter temperatures in many parts of the country—the fourth warmest winter since record-keeping began—have triggered an unusually early release of pollen from trees. That bodes badly for the millions of people who suffer from allergic rhinitis—commonly known as hay fever.
Allergists are predicting a longer, and more intense, allergy season than normal. Once people have been exposed to the early pollen, essentially priming the immune system to react to the allergens, there is little chance of relief even if temperatures cool down again. This priming effect can bring on even more severe symptoms for allergy patients, especially those with asthma, says Neil Kao, an allergist in Greenville, N.C.
Medications, including eye drops, antihistamines and nasal sprays, can relieve hay-fever symptoms for many people. For greatest effect, these products usually need to be used just before any exposure to pollen, says Stanley Fineman, an allergy specialist in Marietta, Ga. But this year "we didn't catch it in time because we didn't know the pollen was going to start so early," says Dr. Fineman, who also is president of the American College of Allergy, Asthma & Immunology, which represents allergists. Weather websites often signal when local pollen counts start to rise.
More aggressive treatments, including immune-boosting allergy shots, are also available, and specialists expect more patients may pursue these remedies this year if their symptoms are worse than normal.
Different pollens serve as triggers to different people. Allergy shots, which administer escalating doses of the offending allergens, work like a vaccine to create resistance in the patient. But these can take several months to become effective. Doctors increasingly are recommending faster treatment protocols that deliver the shots over a shorter period and can bring relief within a few weeks.
Allergists also may offer the same type of immunotherapy in the form of drops under the tongue, which patients can use at home after an initial visit. Pharmaceutical firms are developing immunotherapy tablets, to be taken orally, including one from Merck & Co . that has been shown in trials to reduce symptoms of ragweed allergy.
Other researchers are investigating new methods to give patients faster and more effective allergy relief, such as delivering the allergens through the skin or by way of the lymph nodes.
As many as 30% of children and up to 40% of adults suffer from seasonal allergies that cause reactions such as sneezing, itching, stuffy nose, and watery eyes. Trees are one of the earliest plants to release pollen, followed later by pollen from grass and flowering plants. For example, high concentrations of tree pollen in Kansas City, Mo., Tuesday came mainly from juniper, elm and maple trees, according to data compiled by the National Allergy Bureau, part of research group American Academy of Allergy, Asthma & Immunology. Ditto for Atlanta, where the top offenders were pine, oak and birch.
Some studies suggest climate change, by promoting longer blooming seasons, may increase the prevalence of certain allergens and the time during which people are exposed to them. Warmer temperatures also can boost concentrations of mold, another allergen that is usually killed by colder weather, says James Sublett, the Louisville allergy specialist treating Mr. Bryant.
Improved medications have been introduced to treat allergy symptoms in recent years, including antihistamines, nasal steroid sprays and drugs that block inflammatory chemicals produced by the body. The products are generally safe and effective. But in a large survey of adults presented at an annual allergy conference in 2006, about a third of respondents said they switched medication either because of a lack of effectiveness or side effects.
Unlike medication, allergy shots can potentially lead to lasting remission of symptoms after three to five years.
The treatment, which is formally known as subcutaneous immunotherapy and is generally covered by health insurance plans, may also help prevent development of asthma and new allergies. The shots are typically given once or twice a week for about five months, after which their frequency is reduced.
Growing in popularity is a faster treatment, known as "cluster" therapy, that involves two to four injections one day a week for three weeks. Patients' own immune systems are mobilized and able to counteract naturally occurring allergens often within a few weeks, says Richard Weber, an allergy specialist at National Jewish Health in Denver. Risks include an increased chance of irritation at the injection site and a possibly serious reaction to the allergen.
Rachel Lowe, a 40-year-old plastic-surgery nurse in Marietta, Ga., recently started cluster shots recommended by Dr. Fineman after her allergies kicked in in early February. "I always dread when everything is in bloom because my allergies are so bad that I need to lock myself indoors sometimes and can't enjoy the spring," she says.
Some physicians are administering drops under the tongue, known as sublingual immunotherapy, that contain the same substances used in shots. The technique has been used since the 1980s in Europe, where it has been shown to produce lasting remissions in long-term use. It doesn't have U.S. regulatory approval, but some doctors give it to patients anyway as an "off-label" use of the substance.
Other doctors steer clear of the technique because insurers typically don't cover it and there are no standards in the U.S. for dosage and duration of treatment, says Linda Cox, an allergist in Fort Lauderdale, Fla. Another concern, she says: potential liability if something goes wrong.
Steven Prager, an allergist in California, says he began offering sublingual immunotherapy two years ago because many patients don't like shots or find multiple office visits inconvenient. He says he develops a formula for the drops for each patient based on the severity of their allergies. The treatments cost about $75 a month.
A Child’s Allergies Are Serious but
Can Be Treated Effectively
By Walecia Konrad : NT Times Article : March 5, 2010
It starts with a telltale sniffle, itchy eyes and an occasional cough. You think your little one is getting a cold, but the cold never comes while the runny nose seems never to leave.
“That could be a sign of allergies,” says Dr. Kevin Weiss, an expert on allergies and president of the American Board of Medical Specialties. Not a surprising diagnosis when you consider that more than 40 percent of children (and 20 to 30 percent of adults) suffer from allergic rhinitis, often simply called allergies. With spring pollen season just around the corner, parents are bound to hear more of those telltale sniffles.
Allergies are no trivial matter. Each year, allergic rhinitis accounts for two million missed school days and $2.3 million in health care costs for children younger than 12. It’s not unusual for allergy sufferers to spend thousands of dollars each year on doctor visits, medications and other products, says Dr. Linda Cox, an allergist practicing in Ft. Lauderdale, Fla., and a former committee chairwoman for the American College of Allergy, Asthma and Immunology
What’s more, Dr. Cox said, allergies left untreated in children can often lead to asthma, a chronic and debilitating pulmonary disease.
For the purposes of this article I’ll focus on allergic rhinitis, particularly among children. (The subject of food allergies may warrant a separate, future column.) The condition can be set off by outside elements like pollen from ragweed, grasses and trees and indoor allergens like dust mites and pet dander.
Combating allergies often requires a multipronged and sometimes costly approach. Here’s what you can do to make sure your child gets the best results.
THE RIGHT DOCTOR
Most allergies can be identified and treated by a pediatrician or family doctor. The doctor will use blood tests and your child’s symptoms to come up with an educated guess on what is causing the problem.
“Mild allergies can be treated without a lot of testing,” Dr. Weiss said. New nondrowsy prescription and over-the-counter medications make it easier to treat symptoms, he added. Your child’s doctor should know which drugs are appropriate for children.
That’s good news, because allergists aren’t always part of an insurer’s network or covered under high-deductible plans.
Nevertheless, an allergist can best treat your child if symptoms become moderate to severe. If your child is extremely uncomfortable, losing sleep or missing a lot of school, and the current medications he or she is using aren’t working, you may need to take the next step. An allergist will most likely do a skin test to pinpoint exactly what your child is allergic to. This is often more precise than the blood tests and is usually covered by insurance.
ELIMINATE THE SOURCE
After you and your child’s doctor have narrowed down the possible culprits, it’s time to reduce or remove the troublemakers. Many of the most effective ways to do this are labor-intensive but low in cost, said Dr. James Sublett, an allergist in Louisville, Ky., and professor of pediatric allergy and immunology at the University of Louisville School of Medicine.
Keep your pet away from carpeted rooms, sleeping areas, upholstered furniture and other places where it becomes difficult or impossible to remove dander. Cats are the animals that cause the most allergy problems, and cat allergen can remain in a house for an average of 20 weeks after an animal is removed.
If you and your doctor suspect dust mites are a problem, remove drapes, stuffed animals, pet bedding, upholstered furniture and even carpeting from the bedroom. Wash linens frequently. Dust with a moist cloth or an electrostatic fabric duster. Both do a better job of actually collecting dust rather than just stirring it around. Remember: dust takes a couple of hours to settle after cleaning and vacuuming.
Tumble-drying stuffed animals on high heat for 20 minutes will also kill dust mites.
Get rid of any pest problems, like roaches or mice. Both can be huge allergy triggers. In addition, keep windows closed during peak allergy season.
CONSIDER IMMUNOTHERAPY
Even after you’ve identified and tried to eliminate the source of your child’s allergies, he or she may still be suffering. If that happens, you may have to go for the shots.
Allergy shots have come in for criticism over the years because, well, they are shots and require repeat visits to the doctor’s office — two things children really don’t like.
And many parents may wonder — in some cases, rightfully, alas — whether the allergy doctor is overdiagnosing allergies and overtreating their children. Dr. Cox argues that allergists get to the root of the cause instead of just treating symptoms. General practitioners can prescribe medicines to treat symptoms without easing the condition, she says. In any case, it is important to get a referral from a pediatrician or family doctor whom you trust to do what’s right for your child.
A new study published last month in the peer-reviewed Annals of Allergy, Asthma and Immunology found that allergy shots, also known as immunotherapy, could actually help eliminate allergy symptoms after only 18 months. What’s more, shots may help save you money in the long run. Among the children with allergic rhinitis studied, shots helped to reduce total health care costs by a third, and prescription drug costs by 16 percent, said Dr. Cox, who was a co-author of the study.
In immunotherapy, an allergist injects a small amount of the allergen into a patient. This prompts the body to make natural antibodies, which naturally increase one’s immunity to the culprit. “It is the only therapy that doesn’t just treat allergy symptoms but tries to get at the cause,” Dr. Cox said.
But because the allergist personally mixes the allergens according to a patient’s needs, the shots are not considered pharmaceuticals and are sometimes not covered by insurance.
The first year of allergy shots, which includes a three-month build-up period during which a child receives injections as often as twice a week until the proper dosage is found, would cost a bit less than $1,000 for the year, according to Dr. Cox. The next year, with twice-a-month injections, would total an estimated $350.
For parents who are uninsured and cannot afford shots for their children, Dr. Cox suggests contacting the state allergy society for a list of allergists and clinics that may offer low or no-cost treatments. (Because there is no clearinghouse for such information, you’ll probably have to do your own Web sleuthing.)
AVOID THE UNNECESSARY
There’s no end to the number of products marketed to allergy sufferers, including air filters, humidifiers, dehumidifiers, ozone machines, mattress and pillow encasements, special breathing masks and more. Many of these products are expensive and some are ineffective. Ozone, for instance, can be a pollutant and actually worsen allergies, Dr. Sublett said.
Several studies show that there are no significant improvements from using mattress and pillow encasements and other allergy-fighting products. The best thing to do is to take the necessary steps to remove allergens like the ones discsponsored by the American College of Allergy, Asthma and Immunology. If you’re covered by an H.M.O. or other health network, you’ll need to ask your primary physician for a referral.
An Abundance of Remedies but
Little Relief
Peter Jaret : NY Times Article : October 25, 2007
In Brief:
Despite dozens of over-the-counter and prescription remedies, millions of allergy sufferers seek better relief.
Allergies are often overlooked by doctors and patients but can lead to serious health problems, including asthma in children.
Rush immunotherapy regimens offer a fast response -- and hold out hope for long-term relief -- but require close monitoring.
Under-the-tongue remedies offer an alternative for the needle shy but aren’t yet F.D.A.-approved.
With more than 35 over-the-counter remedies and 28 prescription medications crowding the market, you’d think it would be easy for hay fever sufferers to find relief.
Think again.
Most of the estimated 50 million Americans who suffer the runny noses, raw and itchy eyes, clogged sinuses and hammering headaches of allergic rhinitis, as hay fever is medically known, aren’t getting the relief they seek. According to a 2005 survey conducted by the Asthma and Allergy Foundation of America, more than half say they’re “very interested” in finding a new medication. One in four reports “constantly trying different medications to find one that works for me.”
Why is it so hard to find an effective treatment?
One problem, experts say, is that allergic rhinitis isn’t taken seriously enough, by doctors or allergy sufferers. “Allergic rhinitis is typically a doorknob complaint,” said Dr. Bradley Marple, professor of otolaryngology at the University of Texas Southwestern Medical School in Dallas. “Patients wait until they’re almost out the door before they say, ’Oh, and by the way, my allergies have been acting up.’” Too many doctors quickly write a prescription or recommend an over-the-counter antihistamine but fail to follow up to see if it worked.
Four out of five allergy sufferers never even make it to the doctor’s office, relying instead on over-the-counter remedies, according to the A.A.F.A. survey. “Unfortunately, that usually means there’s no treatment plan in place,” said Dr. Marple. “A patient may try one antihistamine and if it doesn’t work try another, when what they really need is a decongestant, or a drug that targets another part of the allergic reaction, or a corticosteroid nasal spray.”
That’s too bad, and not only because it means needless suffering. Allergies can lead to sleep problems and set sufferers up for more serious respiratory problems. Children with allergic rhinitis are three times more likely than their non-sniffling counterparts to develop asthma. Kids and adults alike are more likely to develop sinus and ear infections, especially if their allergies go untreated.
The strongest argument for taking allergies seriously comes from results of an ongoing experiment called the Preventive Allergy Treatment Study in Denmark. Seven years after completing a course of allergy shots aimed at quieting an overcharged immune response to harmless substances such as pollen, children in the study were more than four times less likely to develop asthma.
“Those results are really remarkable,” said Dr. Harold Nelson, an allergist at the National Jewish Medical and Research Center in Denver. Along with other evidence, he explained, they show that immunotherapy doesn’t just alleviate symptoms but actually changes the immune system of people with allergies, restoring it to normal.
Unfortunately, few studies have been done to compare one course of allergy treatment with another. Instead, physicians must rely not on evidence-based research but what’s referred to as “expert opinion.” And as Dr. Marple said, “experts can disagree.”
Still, a consensus on the basic plan of attack is emerging.
For mild to moderate allergic rhinitis, over-the-counter remedies are a reasonable first step. Decongestants work by constricting tiny blood vessels and shrinking swollen and inflamed tissue in the lining of the sinuses. Antihistamines block one of the biochemical steps of the allergic process.
If over-the-counter medicines don’t work, it’s time to talk to a doctor or allergist. Many prescribe corticosteroid nasal sprays, which suppress the allergic process at the heart of the problem.
Typically, immunotherapy is the last resort. The treatment involves identifying the specific culprit that’s causing the problem through a series of skin tests or, in some cases, a blood test. Tiny doses of allergen are then injected under the skin in a weekly series of allergy shots to desensitize the immune system.
Some doctors now offer an accelerated protocol called rush or cluster immunotherapy, in which patients receive several shots a day, spaced half an hour apart. “Instead of the six to eight months it usually takes with standard immunotherapy, we can get to maintenance levels in four weeks,” said Dr. Nelson. Because this rush procedure can lead to serious immune reactions, including shock, it must be closely monitored. A ragweed vaccine given over six weeks is also currently in testing.
For the needle-shy, another advance is making immunotherapy more attractive: the use of allergens that dissolve under the tongue. Although widely used in Europe, sublingual allergens haven’t yet won F.D.A. approval in the United States. Allergists are free to prescribe them, but insurance companies won’t cover the cost. Another drawback is that sublingual allergens are only about half as effective as injections in desensitizing the immune system. But patients can take them at home, rather than having to make an office visit for each treatment - an important advantage.
For his part, Dr. Nelson thinks more patients should consider immunotherapy, especially those with severe and persistent allergic rhinitis. “Medications work only as long as you keep taking them,” he said. “Immunotherapy is the only treatment we have that alters the immune system, restoring the same response to allergens like ragweed that we see in normal nonallergic people.”
Unlike pills and nasal sprays, in other words, immunotherapy holds out the possibility of something far better: a cure.
Expert Q + A
On the Trail of Allergy Relief
Peter Jaret : NY Times Article : October 25, 2007
Dr. Bradley Marple is a professor of otolaryngology at the University of Texas Southwestern Medical School and a member of the American Academy of Otolaryngic Allergy Working Group on Allergic Rhinitis.
Q: What causes allergic rhinitis?
A: The immediate trigger can be ragweed pollen, pets, dust mites and a range of other allergens, or substances that stimulate the immune system. For most people these are innocuous substances. People who develop allergic rhinitis have an excess of a certain class of antibodies, called IgE, which makes them unusually sensitive to these otherwise harmless substances. All the symptoms of allergic rhinitis are really part of the immune response.
Q: Does the condition run in families?
A: To a certain extent, yes. If both parents have allergies, a child stands a 75 percent chance of developing them. If neither parent is allergic, the risk drops to 25 percent. The genetic aspects are numerous and overlapping, which means we’re not going to find a single gene that accounts for allergies. And as the percentages suggest, environmental factors also play a role.
Q: How does environment influence the risk of developing allergic rhinitis?
A: To answer that, let me recount a fascinating story. When the Berlin Wall fell in the late 1980s, East Germans on one side of the wall turned out to have a much lower incidence of allergic rhinitis and asthma
One possible answer is what’s called the hygiene hypothesis. The immune system was designed to be exposed in early life to a variety of viruses, bacteria and fungi. Those exposures allow it to develop normally. In a society with very high standards of hygiene, such as West Germany and the United States, the immune system isn’t challenged in the same way. Instead of developing to target real threats, such as bacteria, the immune system may dysfunction and begin to trigger allergies.
Q: Should we be sending children to spend time on farms?
A: That’s one idea. Another more reasonable lesson to learn is that we should be more judicious in our use of antibiotics. A lot of kids develop runny noses, and we shouldn’t be so quick to rush to treat them. Having pets might help. Studies show that young children who grow up with a cat in the house are less likely to develop allergies or asthma. Since I’m allergic to cats, though, I offer that advice reluctantly.
Q: Are there other ways to prevent allergic rhinitis?
A: The key to prevention is avoidance, which is easier said than done. You can eradicate the disease if you can get rid of the allergen that’s causing problems. In the case of dust mites, which tend to live in the bedroom, you can wash sheets regularly and keep humidity down to below 50 percent, which drives down dust mite populations. You can remove carpeting and any stuffed animals from the bedroom, which are also home to dust mites. Of course if you’re allergic to cats or dogs, it’s a good idea not to let them share the bedroom. Since we spend one-third of our lives sleeping, you can reduce your exposure somewhat by targeting the bedroom. Avoiding outdoor allergens, such as ragweed pollen, is much more difficult, unless you hermetically seal yourself up in a container. In that case, the best approach is treatment.
Q: Do over-the-counter medicines work?
A: Yes. Many are good at relieving symptoms such as congestion or itchy eyes or runny nose. But they often have side effects, and it’s important not to overuse them, so I recommend reading the label and following instructions. If you have a cough along with congestion and itchy eyes, it’s wise to see a doctor. A cough can be a sign of asthma. If you try over-the-counter drugs and they aren’t helping, see your doctor. That’s especially important for children with symptoms of allergic rhinitis, since we know that treating the condition can greatly lessen the risk of going on to develop asthma.
Q: What about prescription drug options?
A: There are several classes of prescription medications, with more and more emerging out of new research. Antihistamines block the histamine receptor on mast cells, which are the main culprits in allergic reactions. They are very effective at treating the symptoms.
Another newer class of drugs, called anti-leukotrienes, targets another substance involved in allergic responses. Mast cell stabilizers have also been developed that help keep these cells from breaking down and releasing allergic mediators. Probably the most effective medication is topical steroid nasal spray, such as Flonase, Nasonax and Rhinocort. These contain steroids that remain on the surface of cells, decreasing a huge number of inflammatory responses associated with allergic rhinitis. Because corticosteroid nasal sprays take a while to take effect, we usually recommend starting them before allergy season begins.
Immunotherapy offers another alternative, especially when medication doesn’t provide complete relief. The treatment involves identifying the specific allergen and desensitizing the immune system by injecting small amounts of it under the skin over time.
Q: You’ve mentioned allergic rhinitis and asthma. What’s the connection?
A: Both are mediated by an excess of IgE, a class of antibodies. Twenty years ago we thought asthma was caused by bronchial constriction. Now we know the main cause is allergic inflammation. Inflammation needs to be controlled in order to prevent more serious problems from asthma. Allergists now use the term “unified airway” to describe a new understanding that the nose, sinuses and lungs aren’t separate systems but part of the same system. What goes on in the upper respiratory tract can exacerbate problems in the lower respiratory tract. And it’s now clear that treating inflammation in the upper respiratory tract can help prevent development of asthma.
Q: Are you excited about the prospect for new treatments under development?
A: Absolutely. There are many promising avenues of research. Purified antigens are being tested that can lead to a more rapid desensitization in immunotherapy. There’s interest in putting specific antigens onto viral vectors that will carry them directly to mast cells. Ultimately that could mean that one injection would render people nonallergic, instead of the years of immunotherapy now often required. Before long, I hope, sublingual immunotherapy, which uses antigens that dissolve under the tongue instead of injections, may be approved in the United States. It offers two important advantages. It’s very, very safe. And you don’t have to come into a doctor’s office. You can do immunotherapy yourself at home.
Questions for Your Doctor
What to Ask About Allergic Rhinitis
By Peter Jaret : NY Times Article : October 25, 2007
Confronting a new diagnosis can be frightening -- and because research changes so often, confusing. Here are some questions you may not think to ask your doctor, along with notes on why they’re important.
What’s the likely cause of my allergies?
Allergies that occur year-round are likely to be caused by something in the house or immediate environment, such as dust mites or pet dander. Seasonal allergies are more likely to be caused by pollen from ragweed, grasses or trees. Identifying your particular culprit -- or at least making an informed guess about its source -- is useful in trying to prevent allergy attacks. If you decide to have allergy shots, also called immunotherapy, your doctor will determine exactly what the allergen is by doing skin tests or a blood test.
Is there anything I can do to prevent allergies?
The best form of prevention is avoiding allergy-inducing substances. That’s easier said than done. Washing your bed sheets and vacuuming around the house regularly can lower your exposure to dust mites or animal dander. Staying inside as much as possible during allergy season can help prevent pollen-induced allergic rhinitis. Some people have gone so far as moving to another part of the country. Unfortunately, pulling up stakes usually offers only temporary respite. If you’re prone to allergic rhinitis, you’re likely to become sensitive to something in the new environment.
Should I try an over-the-counter allergy medicine?
Most allergy sufferers start by trying over-the-counter remedies. If you have a mild to moderate case of seasonal allergies, antihistamines available on drugstore shelves can help reduce inflammation. Many cause drowsiness, so use them with care. Allergy eye drops can ease the itchy watery eyes.
How long can I go on using an over-the-counter allergy medicine?
Overuse of some over-the-counter medicines can cause inflammation, triggering the same symptoms you’re hoping to treat, a condition known as rhinitis medicamentosa. With decongestants, for example, studies show the problem begins to arise after about 10 days of use.
What about prescription allergy medications?
More than three dozen prescription remedies are available. Among the most effective are corticosteroid nasal sprays, which suppress the immune reaction that causes runny noses, congestion and itchy eyes. A recent study that compared four different prescription nasal sprays found that all were equally effective, so it’s worth checking the cost. It’s important to follow the package instructions exactly, since overuse can cause inflammation.
Should I consider getting allergy shots?
Although over-the-counter and prescription medicines ease symptoms, they don’t cure allergic rhinitis. The only way to treat the underlying condition is immunotherapy, which involves exposure to controlled doses of the allergen. A 2007 review of 51 studies that included 2,971 participants found that immunotherapy is both effective -- measured by reduction in symptoms and need for allergy medicines -- and safe.
Should I consider an accelerated course of immunotherapy?
Although effective, standard immunotherapy requires multiple visits to the doctor, often over the course of several years. Some allergy clinics around the country offer a speeded up protocol called rush immunotherapy. A study involving 893 patients at the Allergy and Asthma Center in Fort Wayne, Indiana, found that rush immunotherapy offers significantly faster relief than conventional protocols of allergy shots. But because the accelerated protocol also raises the risk of a serious immune reaction, it’s essential that rush immunotherapy be done by qualified allergists.
What’s the safest and most effective treatment for children with allergic rhinitis?
Some medicines are safe; others shouldn’t be used by children. Be sure to read package inserts and always ask your doctor if you aren’t sure. Immunotherapy is considered safe for children over 2 years of age, although getting kids to submit to a treatment that involves needles may not be easy. Still, it’s important to take allergic rhinitis in children seriously, since it can lead to the development of asthma.
House Dust Tips:
If you have dust mite allergy, pay careful attention to dust-proofing your bedroom. The worst things to have in the bedroom are:
Carpets trap dust and make dust control impossible.
Reducing the amount of dust mites in your home may mean new cleaning techniques as well as some changes in furnishings to eliminate dust collectors. Water is often the secret to effective dust removal.
If you use sprays:
Controlling Cat & Dog Allergies Tips:
Actually, these are tips for controlling allergies to all the furry creatures you can’t help but cuddle.
If you or your child is allergic to furry pets, especially cats, the best way to avoid allergic reactions is to find them another home. If you are like most people who are attached to their pets, that is usually not a desirable option. There are ways, however, to help lower the levels of animal allergens in the air, which may reduce allergic reactions.
Other tips for controlling allergies:
If you have dust mite allergy, pay careful attention to dust-proofing your bedroom. The worst things to have in the bedroom are:
- Wall-to-wall carpet
- Blinds
- Down-filled blankets
- Feather pillows
- Stuffed animals
- Heating vents with forced hot air
- Dogs and cats
- Closets full of clothing
Carpets trap dust and make dust control impossible.
- Shag carpets are the worst type of carpet for people who are sensitive to dust mites.
- Vacuuming doesn’t get rid of dust mite proteins in furniture and carpeting, but redistributes them back into the room, unless the vacuum has a special HEPA (high-efficiency particulate air) filter.
- Rugs on concrete floors encourage dust mite growth.
Reducing the amount of dust mites in your home may mean new cleaning techniques as well as some changes in furnishings to eliminate dust collectors. Water is often the secret to effective dust removal.
- Clean washable items, including throw rugs, often, using water hotter than 130 degrees Fahrenheit. Lower temperatures will not kill dust mites.
- Clean washable items at a commercial establishment that uses high water temperature, if you cannot or do not want to set water temperature in your home at 130 degrees. (There is a danger of getting scalded if the water is more than 120 degrees.)
- Dust frequently with a damp cloth or oiled mop.
- Do not leave food or garbage out.
- Store food in airtight containers.
- Clean all food crumbs or spilled liquids right away.
If you use sprays:
- Do not spray in food preparation or storage areas.
- Do not spray in areas where children play or sleep.
- Limit the spray to the infested area.
- Follow instructions on the label carefully.
- Make sure there is plenty of fresh air when you spray.
- Keep the person with allergies or asthma out of the room while spraying.
Controlling Cat & Dog Allergies Tips:
Actually, these are tips for controlling allergies to all the furry creatures you can’t help but cuddle.
If you or your child is allergic to furry pets, especially cats, the best way to avoid allergic reactions is to find them another home. If you are like most people who are attached to their pets, that is usually not a desirable option. There are ways, however, to help lower the levels of animal allergens in the air, which may reduce allergic reactions.
- Bathe your cat weekly and brush it more frequently (ideally, a non-allergic person should do this).
- Keep cats out of your bedroom.
- Remove carpets and soft furnishings, which collect animal allergens.
- Use a vacuum cleaner and room air cleaners with HEPA filters.
- Wear a face mask while house and cat cleaning
Other tips for controlling allergies:
- Take a quick shower at night to clean off any pollen from your hair
- Wash and change your pillow case frequently
- Wear sunglasses when you are outdoors especially if it is windy
- Avoid touching your face and rubbing your eyes
- Use your home and car air conditioner. Remember to change the filter.
- Keep bedroom windows closed especially if near trees
- Avoid parking your car under a tree
- Medication: Claritin or Zyrtec are both available over the counter without a prescription. Take either of these once during the day and you can add either chlotrimeton 4mg or Benadryl 25mg at bedtime.
- Women should be aware that wine and certain foods can exacerbate and worsen allergies (see article below)
The CLAIM: Alcohol Worsens Allergies
By Anahad O'Connor : NY Times Article : April 19, 2010
THE FACTS:
Sniffling, sneezing and struggling through allergy season this year?
You may want to lay off alcohol for a while. Studies have found that alcohol can cause or worsen the common symptoms of asthma and hay fever, like sneezing, itching, headaches and coughing.
But the problem is not always the alcohol itself. Beer, wine and liquor contain histamine, produced by yeast and bacteria during the fermentation process. Histamine, of course, is the chemical that sets off allergy symptoms. Wine and beer also contain sulfites, another group of compounds known to provoke asthma and other allergy-like symptoms.
In one study in Sweden in 2005 , scientists looked at thousands of people and found that compared with the general population, those with diagnoses of asthma, bronchitis and hay fever were far more likely to experience sneezing, a runny nose and “lower-airway symptoms” after having a drink. Red wine and white wine were the most frequent triggers, and women, for unknown reasons, were about twice as likely to be affected as men.
Another study of thousands of women published in the journal Clinical and Experimental Allergy in 2008 found that having more than two glasses of wine a day almost doubles the risk of allergy symptoms, even among women who were free of seasonal and perennial allergies at the start of the study.
It helps to be on the lookout for other foods that either contain or release histamine, like aged cheeses, pickled or fermented products and yeast-containing foods, like bread, cider and grapes.
THE BOTTOM LINE :
Drinking alcohol can cause or worsen allergies, particularly in women.
Food Allergies Less Common Than Believed
By Gina Kolata : NY Times Article : May 11, 2010
Many who think they have food allergies actually do not.
A new report, commissioned by the federal government, finds the field is rife with poorly done studies, misdiagnoses and tests that can give misleading results.
While there is no doubt that people can be allergic to certain foods, with reproducible responses ranging from a rash to a severe life-threatening reaction, the true incidence of food allergies is only about 8 percent for children and less than 5 percent for adults, said Dr. Marc Riedl, an author of the new paper and an allergist and immunologist at the University of California, Los Angeles.
Yet about 30 percent of the population believe they have food allergies. And, Dr. Riedl said, about half the patients coming to his clinic because they had been told they had a food allergy did not really have one.
Dr. Riedl does not dismiss the seriousness of some people’s responses to foods. But, he says, “That accounts for a small percentage of what people term ‘food allergies.’ ”
Even people who had food allergies as children may not have them as adults. People often shed allergies, though no one knows why. And sometimes people develop food allergies as adults, again for unknown reasons.
For their report, Dr. Riedl and his colleagues reviewed all the papers they could find on food allergies published between January 1988 and September 2009 — more than 12,000 articles. In the end, only 72 met their criteria, which included having sufficient data for analysis and using more rigorous tests for allergic responses.
“Everyone has a different definition” of a food allergy, said Dr. Jennifer J. Schneider Chafen of the Department of Veterans Affairs’ Palo Alto Health Care System in California and Stanford’s Center for Center for Primary Care and Outcomes Research, who was the lead author of the new report. People who receive a diagnosis after one of the two tests most often used — pricking the skin and injecting a tiny amount of the suspect food and looking in blood for IgE antibodies, the type associated with allergies — have less than a 50 percent chance of actually having a food allergy, the investigators found.
One way to see such a reaction is with what is called a food challenge, giving people a suspect food disguised so they do not know if they are eating it or a placebo food. If the disguised food causes a reaction, the person has an allergy.
But in practice, most doctors are reluctant to use food challenges, Dr. Riedl said. They believe the test to be time consuming, and worry about asking people to consume a food, like peanuts, that can elicit a frightening response.
The paper, to be published Wednesday in The Journal of the American Medical Association, is part of a large project organized by the National Institute of Allergy and Infectious Diseases to try to impose order on the chaos of food allergy testing. An expert panel will provide guidelines defining food allergies and giving criteria to diagnose and manage patients. They hope to have a final draft by the end of June.
“We were approached as in a sense the honest broker who could get parties together to look at this question,” said Dr. Matthew J. Fenton, who oversees the guidelines project for the allergy institute.
Authors of the new report — and experts on the guidelines panel — say even accepted dogma, like the idea that breast-fed babies have fewer allergies or that babies should not eat certain foods like eggs for the first year of life, have little evidence behind them.
Part of the confusion is over what is a food allergy and what is a food intolerance, Dr. Fenton said. Allergies involve the immune system, while intolerances generally do not. For example, a headache from sulfites in wine is not a food allergy. It is an intolerance. The same is true for lactose intolerance, caused by the lack of an enzyme needed to digest sugar in milk.
And other medical conditions can make people think they have food allergies, Dr. Fenton said. For example, people sometimes interpret acid reflux symptoms after eating a particular food as an allergy.
The chairman of the guidelines project, Dr. Joshua Boyce, an associate professor of medicine at Harvard and an allergist and pediatric pulmonologist, said one of the biggest misconceptions some doctors and patients have is that a positive test for IgE antibodies to a food means a person is allergic to that food. It is not necessarily so, he said.
During development, he said, the immune system tends to react to certain food proteins, producing IgE antibodies. But, Dr. Boyce said, “these antibodies can be transient and even inconsequential.”
“There are plenty of individuals with IgE antibodies to various foods who don’t react to those foods at all,” Dr. Boyce said.
The higher the levels of IgE antibodies to a particular food, the greater the likelihood the person will react in an allergic way. But even then, the antibodies do not necessarily portend a severe reaction, Dr. Boyce said. Antibodies to some foods, like peanuts, are much more likely to produce a reaction than ones to other foods, like wheat or corn or rice. No one understands why.
The guidelines panel hopes its report will lead to new research as well as clarify the definition and testing for food allergies.
But for now, Dr. Fenton said, doctors should not use either the skin-prick test or the antibody test as the sole reason for thinking their patients have a food allergy.
“By themselves they are not sufficient,” Dr. Fenton said.
By Gina Kolata : NY Times Article : May 11, 2010
Many who think they have food allergies actually do not.
A new report, commissioned by the federal government, finds the field is rife with poorly done studies, misdiagnoses and tests that can give misleading results.
While there is no doubt that people can be allergic to certain foods, with reproducible responses ranging from a rash to a severe life-threatening reaction, the true incidence of food allergies is only about 8 percent for children and less than 5 percent for adults, said Dr. Marc Riedl, an author of the new paper and an allergist and immunologist at the University of California, Los Angeles.
Yet about 30 percent of the population believe they have food allergies. And, Dr. Riedl said, about half the patients coming to his clinic because they had been told they had a food allergy did not really have one.
Dr. Riedl does not dismiss the seriousness of some people’s responses to foods. But, he says, “That accounts for a small percentage of what people term ‘food allergies.’ ”
Even people who had food allergies as children may not have them as adults. People often shed allergies, though no one knows why. And sometimes people develop food allergies as adults, again for unknown reasons.
For their report, Dr. Riedl and his colleagues reviewed all the papers they could find on food allergies published between January 1988 and September 2009 — more than 12,000 articles. In the end, only 72 met their criteria, which included having sufficient data for analysis and using more rigorous tests for allergic responses.
“Everyone has a different definition” of a food allergy, said Dr. Jennifer J. Schneider Chafen of the Department of Veterans Affairs’ Palo Alto Health Care System in California and Stanford’s Center for Center for Primary Care and Outcomes Research, who was the lead author of the new report. People who receive a diagnosis after one of the two tests most often used — pricking the skin and injecting a tiny amount of the suspect food and looking in blood for IgE antibodies, the type associated with allergies — have less than a 50 percent chance of actually having a food allergy, the investigators found.
One way to see such a reaction is with what is called a food challenge, giving people a suspect food disguised so they do not know if they are eating it or a placebo food. If the disguised food causes a reaction, the person has an allergy.
But in practice, most doctors are reluctant to use food challenges, Dr. Riedl said. They believe the test to be time consuming, and worry about asking people to consume a food, like peanuts, that can elicit a frightening response.
The paper, to be published Wednesday in The Journal of the American Medical Association, is part of a large project organized by the National Institute of Allergy and Infectious Diseases to try to impose order on the chaos of food allergy testing. An expert panel will provide guidelines defining food allergies and giving criteria to diagnose and manage patients. They hope to have a final draft by the end of June.
“We were approached as in a sense the honest broker who could get parties together to look at this question,” said Dr. Matthew J. Fenton, who oversees the guidelines project for the allergy institute.
Authors of the new report — and experts on the guidelines panel — say even accepted dogma, like the idea that breast-fed babies have fewer allergies or that babies should not eat certain foods like eggs for the first year of life, have little evidence behind them.
Part of the confusion is over what is a food allergy and what is a food intolerance, Dr. Fenton said. Allergies involve the immune system, while intolerances generally do not. For example, a headache from sulfites in wine is not a food allergy. It is an intolerance. The same is true for lactose intolerance, caused by the lack of an enzyme needed to digest sugar in milk.
And other medical conditions can make people think they have food allergies, Dr. Fenton said. For example, people sometimes interpret acid reflux symptoms after eating a particular food as an allergy.
The chairman of the guidelines project, Dr. Joshua Boyce, an associate professor of medicine at Harvard and an allergist and pediatric pulmonologist, said one of the biggest misconceptions some doctors and patients have is that a positive test for IgE antibodies to a food means a person is allergic to that food. It is not necessarily so, he said.
During development, he said, the immune system tends to react to certain food proteins, producing IgE antibodies. But, Dr. Boyce said, “these antibodies can be transient and even inconsequential.”
“There are plenty of individuals with IgE antibodies to various foods who don’t react to those foods at all,” Dr. Boyce said.
The higher the levels of IgE antibodies to a particular food, the greater the likelihood the person will react in an allergic way. But even then, the antibodies do not necessarily portend a severe reaction, Dr. Boyce said. Antibodies to some foods, like peanuts, are much more likely to produce a reaction than ones to other foods, like wheat or corn or rice. No one understands why.
The guidelines panel hopes its report will lead to new research as well as clarify the definition and testing for food allergies.
But for now, Dr. Fenton said, doctors should not use either the skin-prick test or the antibody test as the sole reason for thinking their patients have a food allergy.
“By themselves they are not sufficient,” Dr. Fenton said.
Food Allergy Advice for Kids: Don't Delay Peanuts, Eggs
Sumathi Reddy : WSJ : March 4, 2013
Parents trying to navigate the confusing world of children's food allergies now have more specific advice to consider. Highly allergenic foods such as peanut butter, fish and eggs can be introduced to babies between 4 and 6 months and may even play a role in preventing food allergies from developing.
These recommendations regarding children and food allergies—a rising phenomenon that researchers don't fully understand—come from the American Academy of Allergy, Asthma & Immunology in a January article in the Journal of Allergy & Clinical Immunology: In Practice. The AAAAI's Adverse Reactions to Foods Committee outlined how and when to introduce highly allergenic foods, which include wheat, soy, milk, tree nuts, and shellfish.
The recommendations are a U-turn from 2000, when the American Academy of Pediatrics issued guidelines that children should put off having milk until age 1, eggs until 2 and peanuts, shellfish, tree nuts and fish until 3. In 2008, the AAP revised its guidelines, citing little evidence that such delays prevent the development of food allergies, but it didn't say when and how to introduce such foods.
Food allergies affect an estimated 5% of children under the age of 5 in the U.S., according to the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. The prevalence of a food allergy for children under 18 increased by 18% from 1997 to 2007.
"There's been more studies that find that if you introduce them early it may actually prevent food allergy," said David Fleischer, co-author of the article and a pediatric allergist at National Jewish Health in Denver. "We need to get the message out now to pediatricians, primary-care physicians and specialists that these allergenic foods can be introduced early."
Dr. Fleischer said more study results are needed to conclusively determine whether early introduction will in fact lead to lower food-allergy rates and whether they should be recommended as a practice.
The first trials to split children into groups, with some eating highly allergenic foods early on and others delaying, are continuing in the United Kingdom and Australia with some preliminary results expected to be out next year. This type of trial with children is rare and the results are highly anticipated.
One theory to explain why early introduction is important holds that if babies aren't exposed early enough to certain foods, their immune systems will treat them as foreign substances and attack them, resulting in an allergy.
"The body has to be trained in the first year of life," says Katie Allen, a professor and allergist at the Murdoch Childrens Research Institute at Royal Children's Hospital in Australia. (The institute was founded in part by the late Dame Elisabeth Murdoch, mother of Rupert Murdoch, who is chairman of News Corp., which owns The Wall Street Journal.) "We think there's a critical window, probably around 4 to 6 months, when the child first starts to eat solids," she says.
Another possible explanation from some experts for the increase in allergies: As westernized countries have become more hygienic, children don't have the same exposure to germs, which affects the development of the immune system.
Dr. Allen believes there may be a link between food allergies and vitamin D. In a study out this week in the Journal of Allergy and Clinical Immunology, researchers took blood samples from more than 5,000 babies and found that those with low vitamin D levels were three times more likely to have a food allergy.
Food-allergy reactions range from hives and eczema to asthma, vomiting and anaphylaxis, a life-threatening reaction in which the body's major systems quickly shut down. A 2011 prevalence study in the journal Pediatrics found that 39% of children with food allergies have a history of severe reactions.
The new recommendations include introducing highly allergenic foods after typical first foods have been eaten and tolerated, such as rice cereal, fruits and vegetables. They suggest children be fed the foods at home and in gradually increasing amounts. The AAAAI recommendations cited about half-a-dozen studies in making its new guidelines.
One observational study compared Jewish children in the United Kingdom with those in Israel, where the peanut-allergy rate is low. The 2008 study of more than 5,000 children in each country in the Journal of Allergy Clinical Immunology found the rate of peanut allergies among the U.K. children was 10 times that of those in Israel. Gideon Lack, a professor of paediatric allergy at King's College London, said the researchers followed up with surveys given to the parents of about 100 infants hundred in each country. They found that popular snacks with peanuts were given to Israeli babies often before they were 6 months of age, whereas the majority of babies in the United Kingdom didn't taste peanut products until after the age of 1.
Dr. Lack is in the midst of the much-anticipated, randomized controlled trial in the U.K., which is following 640 children with a high risk of allergy—determined by eczema—from infancy to the age of 5. Half of the children are consuming at least 24 grams of peanuts three times a week, while the others have none. About two-thirds of the children are now 5 and receiving peanut-allergy testing. Preliminary results are expected next year.
Some experts are critical of the observational studies cited in the recommendations. "The evidence that has come up is of great interest but it's all either anecdotal or epidemiological and not the intervention studies that are going on right now that will lead to answers in the next three years," said Robert Wood, director of Pediatric Allergy and Immunology at Johns Hopkins University School of Medicine.
Dr. Wood said he tells parent they don't need to feel pressured to do an early introduction. "You can do whatever you want because we're not sure what makes a difference," he said.
When food allergies first started becoming more common in the 1990s, the prevailing thought among experts was that delaying introduction of such foods would reduce the prevalence of food allergies.
"As these guidelines were implemented we've seen a paradoxical increase in foods allergies in young children, especially with peanut allergies," said Anna Nowak-Wegrzyn, associate professor of pediatrics at the Icahn School of Medicine at Mount Sinai Hospital.
The new recommendations from the AAAAI committee say an allergist should be consulted in cases when an infant has eczema that is difficult to control, or an existing food allergy. For children who have a sibling with a peanut allergy—and have a 7% greater risk of a peanut allergy—parents may request an evaluation but the risks of introducing peanut at home in infancy are low, the recommendations noted.
Debby Beerman, a Chicago-area mom, has two boys, ages 4 and 3, with a number of allergies.
"It scares me to think that you would give the food to a child at such a young age when they can't really express that they're not feeling well or they're in distress or something's not right," said Ms. Beerman, a member of the Food Allergy Research & Education, an advocacy group. "But if the data was there to support it, I think we would all do anything we could to try and avoid this.
Sumathi Reddy : WSJ : March 4, 2013
Parents trying to navigate the confusing world of children's food allergies now have more specific advice to consider. Highly allergenic foods such as peanut butter, fish and eggs can be introduced to babies between 4 and 6 months and may even play a role in preventing food allergies from developing.
These recommendations regarding children and food allergies—a rising phenomenon that researchers don't fully understand—come from the American Academy of Allergy, Asthma & Immunology in a January article in the Journal of Allergy & Clinical Immunology: In Practice. The AAAAI's Adverse Reactions to Foods Committee outlined how and when to introduce highly allergenic foods, which include wheat, soy, milk, tree nuts, and shellfish.
The recommendations are a U-turn from 2000, when the American Academy of Pediatrics issued guidelines that children should put off having milk until age 1, eggs until 2 and peanuts, shellfish, tree nuts and fish until 3. In 2008, the AAP revised its guidelines, citing little evidence that such delays prevent the development of food allergies, but it didn't say when and how to introduce such foods.
Food allergies affect an estimated 5% of children under the age of 5 in the U.S., according to the National Institute of Allergy and Infectious Diseases, part of the National Institutes of Health. The prevalence of a food allergy for children under 18 increased by 18% from 1997 to 2007.
"There's been more studies that find that if you introduce them early it may actually prevent food allergy," said David Fleischer, co-author of the article and a pediatric allergist at National Jewish Health in Denver. "We need to get the message out now to pediatricians, primary-care physicians and specialists that these allergenic foods can be introduced early."
Dr. Fleischer said more study results are needed to conclusively determine whether early introduction will in fact lead to lower food-allergy rates and whether they should be recommended as a practice.
The first trials to split children into groups, with some eating highly allergenic foods early on and others delaying, are continuing in the United Kingdom and Australia with some preliminary results expected to be out next year. This type of trial with children is rare and the results are highly anticipated.
One theory to explain why early introduction is important holds that if babies aren't exposed early enough to certain foods, their immune systems will treat them as foreign substances and attack them, resulting in an allergy.
"The body has to be trained in the first year of life," says Katie Allen, a professor and allergist at the Murdoch Childrens Research Institute at Royal Children's Hospital in Australia. (The institute was founded in part by the late Dame Elisabeth Murdoch, mother of Rupert Murdoch, who is chairman of News Corp., which owns The Wall Street Journal.) "We think there's a critical window, probably around 4 to 6 months, when the child first starts to eat solids," she says.
Another possible explanation from some experts for the increase in allergies: As westernized countries have become more hygienic, children don't have the same exposure to germs, which affects the development of the immune system.
Dr. Allen believes there may be a link between food allergies and vitamin D. In a study out this week in the Journal of Allergy and Clinical Immunology, researchers took blood samples from more than 5,000 babies and found that those with low vitamin D levels were three times more likely to have a food allergy.
Food-allergy reactions range from hives and eczema to asthma, vomiting and anaphylaxis, a life-threatening reaction in which the body's major systems quickly shut down. A 2011 prevalence study in the journal Pediatrics found that 39% of children with food allergies have a history of severe reactions.
The new recommendations include introducing highly allergenic foods after typical first foods have been eaten and tolerated, such as rice cereal, fruits and vegetables. They suggest children be fed the foods at home and in gradually increasing amounts. The AAAAI recommendations cited about half-a-dozen studies in making its new guidelines.
One observational study compared Jewish children in the United Kingdom with those in Israel, where the peanut-allergy rate is low. The 2008 study of more than 5,000 children in each country in the Journal of Allergy Clinical Immunology found the rate of peanut allergies among the U.K. children was 10 times that of those in Israel. Gideon Lack, a professor of paediatric allergy at King's College London, said the researchers followed up with surveys given to the parents of about 100 infants hundred in each country. They found that popular snacks with peanuts were given to Israeli babies often before they were 6 months of age, whereas the majority of babies in the United Kingdom didn't taste peanut products until after the age of 1.
Dr. Lack is in the midst of the much-anticipated, randomized controlled trial in the U.K., which is following 640 children with a high risk of allergy—determined by eczema—from infancy to the age of 5. Half of the children are consuming at least 24 grams of peanuts three times a week, while the others have none. About two-thirds of the children are now 5 and receiving peanut-allergy testing. Preliminary results are expected next year.
Some experts are critical of the observational studies cited in the recommendations. "The evidence that has come up is of great interest but it's all either anecdotal or epidemiological and not the intervention studies that are going on right now that will lead to answers in the next three years," said Robert Wood, director of Pediatric Allergy and Immunology at Johns Hopkins University School of Medicine.
Dr. Wood said he tells parent they don't need to feel pressured to do an early introduction. "You can do whatever you want because we're not sure what makes a difference," he said.
When food allergies first started becoming more common in the 1990s, the prevailing thought among experts was that delaying introduction of such foods would reduce the prevalence of food allergies.
"As these guidelines were implemented we've seen a paradoxical increase in foods allergies in young children, especially with peanut allergies," said Anna Nowak-Wegrzyn, associate professor of pediatrics at the Icahn School of Medicine at Mount Sinai Hospital.
The new recommendations from the AAAAI committee say an allergist should be consulted in cases when an infant has eczema that is difficult to control, or an existing food allergy. For children who have a sibling with a peanut allergy—and have a 7% greater risk of a peanut allergy—parents may request an evaluation but the risks of introducing peanut at home in infancy are low, the recommendations noted.
Debby Beerman, a Chicago-area mom, has two boys, ages 4 and 3, with a number of allergies.
"It scares me to think that you would give the food to a child at such a young age when they can't really express that they're not feeling well or they're in distress or something's not right," said Ms. Beerman, a member of the Food Allergy Research & Education, an advocacy group. "But if the data was there to support it, I think we would all do anything we could to try and avoid this.
New Rules for Food Allergies
Fewer Children May Be Diagnosed as Doctors Told Not to Rely Solely on Standard Skin and Blood Tests
Melinda Beck : WSJ Article : December 7, 2010
Parents who have eliminated foods from their children's diets based on allergy tests alone may find that some are safe to eat after all.
The National Institute for Allergy and Infectious Diseases issued the first clinical guidelines for diagnosing and treating food allergies Monday, saying that blood or skin tests aren't sufficient when making a diagnosis.
An allergy should be suspected if someone has a reaction within minutes or hours of eating a food, according to the guidelines. Physicians should then take a detailed medical history, conduct a physical exam and confirm the allergy with a skin-prick test, in which tiny drops of the suspected allergen are pricked into the skin, usually in the forearm, to see if red wheals form. None of those steps is definitive by itself, the recommendations say, which will likely to lead to fewer diagnoses.
For a correct diagnosis, "it takes a combination, and in some cases an oral food challenge," in which patients are exposed to tiny amounts of the suspect food under close medical supervision, says Hugh A. Sampson, director of the Jaffe Food Allergy Institute at Mount Sinai Medical Center in New York and one of the authors.
The guidelines, published this week in the Journal of Allergy and Clinical Immunology, are aimed at resolving wide discrepancies in diagnosing and treating food allergies among allergists, dermatologists, gastroenterologists, pulmonologists and emergency physicians, as well as pediatricians and internists. More than 30 professional organizations, federal agencies and patient groups were involved in the report, which was in the works for two years. The research company Rand Corp. contributed a review of scientific studies.
Roughly 4% of children under age 18—about three million—reported having food allergies in 2007, an 18% increase from 1997, according to the Centers for Disease Control and Prevention. Milk, eggs, peanuts, wheat, soy, fish and shellfish are the most common culprits, although more than 170 other foods have been reported to cause allergic reactions. Symptoms can range from eczema and hives to asthma, inflammation of the esophagus, diarrhea, vomiting and life-threatening anaphylaxis, in which major body systems quickly shut down.
The prevalence of food allergies has been difficult to gauge because of different standards in diagnosing and a proliferation of tests being marketed to doctors. Some tests have not been scientifically validated, experts say, and some doctors lack the expertise to interpret those that have been. The report did not state that kids were being misdiagnosed, but it did note that erroneous diagnoses could affect their nutritional well-being and quality of life.
Blood tests that measure immunoglobulin E (IgE) antibodies are very often misinterpreted, experts say. Having IgE antibodies to specific foods doesn't necessarily mean a person will have an allergic reaction when eating the foods. Skin-prick tests are more predictive, but they, too, measure IgE "sensitization," which may not result in an actual reaction. The report estimates that 50% to 90% of presumed allergies are not, in fact, allergies.
In the Report
Other guidelines from the National Institute for Allergy and Infectious Diseases:
"We get patients referred to us all the time who have been placed on very restrictive diets. They may be off 10 or 20 foods," says Dr. Sampson. "We go through a full evaluation, and it turns out they are allergic to only one or two."
It's especially hard to pinpoint a true food allergy in young children with eczema, since they make IgE antibodies to many foods. "If you did 100 food tests, all 100 would be positive. That's what we see from patients coming in from around the country," says David Fleischer, an assistant professor of pediatrics at National Jewish Health in Denver, which specializes in allergy and respiratory diseases.
In a study published online in the Journal of Pediatrics this fall, a review of 125 children evaluated for food allergies and eczema at National Jewish in 2007 and 2008 found that over 90% of the foods they were avoiding were returned to their diets after food challenges.
The guidelines also recommend against using intradermal tests, in which a potential allergen is introduced deep under the skin, and skin-patch tests, a larger version of skin pricks, to diagnose food allergies. And they note that there is little scientific data to support a long list of other tests for allergy assessments, including hair analysis, facial thermography, which detects heat patterns and histamines in the skin, and immunoglobulin G tests, which purport to measure hypersensitivity to 100 or more foods at a time.
Medical history is the most important key to a diagnosis, experts say. "The major piece of the puzzle is what happened? What did they eat and when? How long was it between eating and having symptoms? What else was going on?" says A. Wesley Burks, chief of pediatric allergy and immunology at Duke University Medical Center and another author of the guidelines. In the real world, it's often far from clear which of dozens of different foods a child eats during the day, or what unknown ingredient in a restaurant meal, may have set off a reaction. That's why the guidelines also call for using a skin-prick test to verify that the patient does have an immune reaction to a suspected food.
In more than 50% of cases, the report notes, the presumed food allergy isn't a real allergy. A different food could be responsible, or there could be some other cause entirely, particularly with gastrointestinal symptoms.
If the diagnosis still isn't clear, the most definitive test is an oral food challenge. The gold standard is a double-blind placebo-controlled challenge, in which neither the tester nor the patient knows which sample is a potentially allergenic food and which is harmless but looks and tastes similar.
But food challenges are time consuming, labor-intensive and nerve-wracking. They're too risky—and not widely reimbursed by insurers—to be done in private physicians' offices. Most are done at academic research centers, which sometimes have long waiting lists for appointments.
Food challenges can bring some relief, however. A study of 167 Australian children with egg allergies published in the journal Pediatric Allergy and Immunology last year found that the families of those whose allergies had not been confirmed with a food challenge were more stressed out than those who had, even the child had a bad reaction.
"Doing a food-challenge test helps manage their anxiety," says Julie Bradsher, chief executive of the Food Allergy and Anaphylaxis Network, a patient-advocacy group, one of many organizations that helped review the guidelines. With the new guidelines, parents "can say, 'I want to make sure that my child is being diagnosed using these guidelines, as opposed to just one or two steps.' "
Fewer Children May Be Diagnosed as Doctors Told Not to Rely Solely on Standard Skin and Blood Tests
Melinda Beck : WSJ Article : December 7, 2010
Parents who have eliminated foods from their children's diets based on allergy tests alone may find that some are safe to eat after all.
The National Institute for Allergy and Infectious Diseases issued the first clinical guidelines for diagnosing and treating food allergies Monday, saying that blood or skin tests aren't sufficient when making a diagnosis.
An allergy should be suspected if someone has a reaction within minutes or hours of eating a food, according to the guidelines. Physicians should then take a detailed medical history, conduct a physical exam and confirm the allergy with a skin-prick test, in which tiny drops of the suspected allergen are pricked into the skin, usually in the forearm, to see if red wheals form. None of those steps is definitive by itself, the recommendations say, which will likely to lead to fewer diagnoses.
For a correct diagnosis, "it takes a combination, and in some cases an oral food challenge," in which patients are exposed to tiny amounts of the suspect food under close medical supervision, says Hugh A. Sampson, director of the Jaffe Food Allergy Institute at Mount Sinai Medical Center in New York and one of the authors.
The guidelines, published this week in the Journal of Allergy and Clinical Immunology, are aimed at resolving wide discrepancies in diagnosing and treating food allergies among allergists, dermatologists, gastroenterologists, pulmonologists and emergency physicians, as well as pediatricians and internists. More than 30 professional organizations, federal agencies and patient groups were involved in the report, which was in the works for two years. The research company Rand Corp. contributed a review of scientific studies.
Roughly 4% of children under age 18—about three million—reported having food allergies in 2007, an 18% increase from 1997, according to the Centers for Disease Control and Prevention. Milk, eggs, peanuts, wheat, soy, fish and shellfish are the most common culprits, although more than 170 other foods have been reported to cause allergic reactions. Symptoms can range from eczema and hives to asthma, inflammation of the esophagus, diarrhea, vomiting and life-threatening anaphylaxis, in which major body systems quickly shut down.
The prevalence of food allergies has been difficult to gauge because of different standards in diagnosing and a proliferation of tests being marketed to doctors. Some tests have not been scientifically validated, experts say, and some doctors lack the expertise to interpret those that have been. The report did not state that kids were being misdiagnosed, but it did note that erroneous diagnoses could affect their nutritional well-being and quality of life.
Blood tests that measure immunoglobulin E (IgE) antibodies are very often misinterpreted, experts say. Having IgE antibodies to specific foods doesn't necessarily mean a person will have an allergic reaction when eating the foods. Skin-prick tests are more predictive, but they, too, measure IgE "sensitization," which may not result in an actual reaction. The report estimates that 50% to 90% of presumed allergies are not, in fact, allergies.
In the Report
Other guidelines from the National Institute for Allergy and Infectious Diseases:
- Introducing solid foods to infants should not be delayed beyond 4 to 6 months old.
- People with an egg allergy need not avoid the measles, mumps, rubella (MMR) vaccine. But they should avoid vaccines for influenza, yellow fever or rabies.
- Even those at high risk for food allergies, such as family members of those with allergies, may not need routine testing. One exception: siblings of children with severe peanut allergies.
"We get patients referred to us all the time who have been placed on very restrictive diets. They may be off 10 or 20 foods," says Dr. Sampson. "We go through a full evaluation, and it turns out they are allergic to only one or two."
It's especially hard to pinpoint a true food allergy in young children with eczema, since they make IgE antibodies to many foods. "If you did 100 food tests, all 100 would be positive. That's what we see from patients coming in from around the country," says David Fleischer, an assistant professor of pediatrics at National Jewish Health in Denver, which specializes in allergy and respiratory diseases.
In a study published online in the Journal of Pediatrics this fall, a review of 125 children evaluated for food allergies and eczema at National Jewish in 2007 and 2008 found that over 90% of the foods they were avoiding were returned to their diets after food challenges.
The guidelines also recommend against using intradermal tests, in which a potential allergen is introduced deep under the skin, and skin-patch tests, a larger version of skin pricks, to diagnose food allergies. And they note that there is little scientific data to support a long list of other tests for allergy assessments, including hair analysis, facial thermography, which detects heat patterns and histamines in the skin, and immunoglobulin G tests, which purport to measure hypersensitivity to 100 or more foods at a time.
Medical history is the most important key to a diagnosis, experts say. "The major piece of the puzzle is what happened? What did they eat and when? How long was it between eating and having symptoms? What else was going on?" says A. Wesley Burks, chief of pediatric allergy and immunology at Duke University Medical Center and another author of the guidelines. In the real world, it's often far from clear which of dozens of different foods a child eats during the day, or what unknown ingredient in a restaurant meal, may have set off a reaction. That's why the guidelines also call for using a skin-prick test to verify that the patient does have an immune reaction to a suspected food.
In more than 50% of cases, the report notes, the presumed food allergy isn't a real allergy. A different food could be responsible, or there could be some other cause entirely, particularly with gastrointestinal symptoms.
If the diagnosis still isn't clear, the most definitive test is an oral food challenge. The gold standard is a double-blind placebo-controlled challenge, in which neither the tester nor the patient knows which sample is a potentially allergenic food and which is harmless but looks and tastes similar.
But food challenges are time consuming, labor-intensive and nerve-wracking. They're too risky—and not widely reimbursed by insurers—to be done in private physicians' offices. Most are done at academic research centers, which sometimes have long waiting lists for appointments.
Food challenges can bring some relief, however. A study of 167 Australian children with egg allergies published in the journal Pediatric Allergy and Immunology last year found that the families of those whose allergies had not been confirmed with a food challenge were more stressed out than those who had, even the child had a bad reaction.
"Doing a food-challenge test helps manage their anxiety," says Julie Bradsher, chief executive of the Food Allergy and Anaphylaxis Network, a patient-advocacy group, one of many organizations that helped review the guidelines. With the new guidelines, parents "can say, 'I want to make sure that my child is being diagnosed using these guidelines, as opposed to just one or two steps.' "
Have a Food Allergy?
It’s Time to Recheck
By Jane E. Brody : NY Times : January 10, 2011
Food allergies have generated a great deal of anxiety in recent years, with some schools going so far as to ban popular staples — especially peanut butter — after appeals from worried parents.
Some airlines have quit serving peanut snacks, and more and more restaurants are offering dishes for diners concerned about gluten or dairy allergies.
There is no question that some foods, especially peanuts and shellfish, can provoke severe reactions in a small fraction of the population. But a new analysis of the best available evidence finds that many children and adults who think they have food allergies are mistaken.
According to a definitive report compiled for the National Institute of Allergy and Infectious Diseases by a 25-member panel of experts, a big part of the problem is misdiagnosis, from overreliance on two tests — a skin-prick test and a blood test for antibodies — that can produce misleading results.
The mere presence of antibodies to a particular substance in food does not mean that someone would have an allergic reaction after eating that food. in And a skin-prick test can remain positive long after an allergy is gone.
Sometimes a diagnosis is based on no test at all, solely on a patient’s or parent’s report of a bad reaction after a particular food was eaten. People often mistake food intolerance, like difficulty digesting the lactose in milk, for an allergy. (Allergies involve the immune system; lactose intolerance results from deficiency of an enzyme.)
Facts and Fallacies
The only test that can definitively establish a food allergy is a so-called oral challenge, in which the patient ingests the suspect food and waits for a reaction. This can be safely done only by an experienced health professional with emergency treatment at hand in case of a severe reaction.
Understandably, doctors are often reluctant to try an oral challenge. But in challenges where a suspect food is compared with a placebo and neither doctor nor patient knows which food is which, only about a third of the foods have been found to cause allergies, the panel reported.
Nonetheless, genuine food allergies seem to have risen during the last decade or two, for reasons no one knows, said Dr. Anthony S. Fauci, director of the allergy institute. The institute, a division of the National Institutes of Health, sponsored the panel’s two-year effort to establish national guidelines for the definition, diagnosis and treatment of food allergies.
According to the panel’s detailed and well-documented report, about one child in 20 and one adult in 25 have a food allergy, nowhere near popular estimates that up to 30 percent of Americans are afflicted.
The panel also reported that most children outgrow allergies to milk, egg, soy and wheat, but until they are properly tested they may not know it is now safe to eat the food — or, perhaps more important, to receive a vaccine prepared in eggs.
Allergies to peanuts and tree nuts are relatively rare (about half of 1 percent of the population in each case, according to the panel). But they tend to be lifelong and life-threatening, and can require extreme vigilance.
Some food allergies start in adulthood, and tend to last indefinitely as well. In particular, shellfish allergies, which can be life-threatening, occur in only 0.5 percent of children but 2.5 percent of adults.
It is not possible to predict the severity of a food allergy reaction based on past reactions. In the case of nut allergy, for example, subsequent exposures can be much worse than what a child first experienced.
There are no treatments for food allergy except to avoid the culprit food, which may require careful reading of labels and potentially embarrassing inquiries when eating away from home. Although immunotherapy has been proposed as a means of curbing an established food allergy, the panel did not recommend this outside of “highly controlled clinical settings.”
Many packaged food labels now warn not only that a particular allergen is present, but also that the product was prepared where allergens like nuts, wheat or soy are present. But Mount Sinai Medical Center in Manhattan did a study of parents’ label reading and found that they were surprisingly poor at identifying foods to which their children were allergic.
Symptoms of food allergies are often confusing and can be mistaken for other problems. They can affect the skin (for example, as eczema or hives), eyes, upper or lower respiratory tract, any part of the digestive tract, and the cardiovascular system. But unless a food allergy is proved, the panel does not recommend avoiding foods to control allergic dermatitis, asthma or inflammation of the esophagus.
As for vaccines, the panel said that even children with an egg allergy could safely be immunized for measles, mumps, rubella and varicella (chickenpox), but the flu vaccine should not be given.
When and When Not to Worry
The experts found little evidence that restricting a woman’s diet during pregnancy and lactation was effective in preventing food allergies in her offspring. Nor did they find strong evidence that exclusive breast-feeding for four to six months can prevent allergic disease. The panel said substituting soy for cow’s milk infant formula did not prevent food allergies in infants thought to be at risk because of a family history of allergy.
Moreover, there is danger in restricting children’s diets for fear of allergies, even real ones: They can develop nutrient deficiencies that result in retarded growth and development. Thus, the panel recommended “nutritional counseling and regular growth monitoring for all children with food allergies.”
The panel devoted the last section of its lengthy report to food-induced anaphylaxis, a potentially fatal disorder that is often recognized too late for adequate treatment. The most common food causes of anaphylaxis, the panel said, are peanuts, tree nuts, milk, eggs, fish and crustacean shellfish, and a life-threatening reaction can occur even the first time a person is exposed.
Symptoms that occur within minutes to several hours after exposure may involve lesions of the skin and mouth; difficulty breathing; a precipitous drop in blood pressure, dizziness or rapid heart rate; abdominal pain, vomiting or diarrhea; and anxiety, mental confusion, lethargy or seizures.
Anyone with a life-threatening food allergy must always have readily available two doses of self-injectable epinephrine (commonly known by the brand EpiPen), to be injected into the thigh muscle. Treatment with an antihistamine is not an effective substitute, the panel warned.
Fatalities result when the use of epinephrine is delayed or the dose given is inadequate. When in doubt, treat, the panel said; then call 911. The EpiPen is a stopgap measure to buy time until life-saving care can be administered.
Parents, baby sitters, school nurses and camp counselors must have two epinephrine pens handy and know how to use them for each child at risk of anaphylaxis. The pens must be stored at 59 to 89 degrees Fahrenheit, and must be replaced annually.
ANAPHYLAXIS
Anaphylaxis is a very serious allergic reaction to a food, medication, material (such as latex) or insect sting. It could be life-threatening, and requires immediate medical attention.
The common warning signs of anaphylaxis include:
The common warning signs of anaphylaxis include:
Who Should Worry About House Dust Mites
(and Who Shouldn’t)
By Lesley Alderman : NY Times : March 4, 2011
The other night my husband and I were having serious pillow talk. But not the kind you might think. Ours went something like this:
Husband: Don’t we need new pillows? We’ve been sleeping on ours for, like, seven years.
Me: They seem fine to me.
Husband: But they are probably full of dust mites and other gross stuff.
Me: Ugh. O.K.
A cool $400 later, I had bought eight new down pillows — two for each member of our family. I was about to investigate dust mite protection covers (an additional $100) when I stopped myself.
Really, should I care this much about dust mites? I have mild allergies and so does my husband, but I’ve never felt that my pillow was making me sick. And these fluffy new pillows and covers were expensive.
Dust mites are microscopic creatures, about 0.4 millimeters in length, that feast on flakes of human skin. Their feces contains a substance called DerP1, a very potent allergen. People who are allergic to dust mites may have asthmalike symptoms, eczema or chronic sinus problems.
Many of us believe that bed linens, pillows and mattresses must be replaced regularly to prevent them from becoming home to vast colonies of these nasty creatures, lest their feces spread and cause allergic reactions in family members.
According to most experts, the truth is a bit more prosaic. People who have allergies to dust mites should indeed take measures to protect themselves. But everyone else can skip the expensive trips to Linens “R” Us.
The trouble is, it’s not always clear whether you have a mite allergy. And even when you know you are allergic, there’s a lot of confusion about which strategies really work.
Here’s how to decide if you should be worrying about your bedding and the dust mites that take up residence in them — along with expert advice on the most effective home interventions.
AN ALLERGY TEST
Mites proliferate in warm, humid climates. They are almost nonexistent in places like New Mexico but thrive in tropical areas like Florida. Here’s a mite test: “If your home is full of static electricity, you likely do not have mites at the moment,” said Dr. Thomas Platts-Mills, director of the Asthma and Allergic Disease Center at the University of Virginia.
But if the temperature and humidity rise, watch out. About one in four Americans has some type of allergy, and within that group about two-thirds are allergic to dust mites, said Dr. James Sublett, an allergist in Louisville, Ky., who is chairman of the Indoor Allergen Committee of the American College of Allergy, Asthma and Immunology.
“Very few people are allergic to just one thing,” he said.
If you’re not sure whether you have a sensitivity to dust mites, ask yourself these questions: Do I have persistent sniffles and sinus headaches? Do I often wake up with scratchy eyes? Do I sneeze repeatedly first thing in the morning?
“Sometimes symptoms are obvious, but sometimes they are subtle,” said Dr. Diego Saporta, an otolaryngologist in Elizabeth, N.J., who specializes in allergy management. “Your only symptom might be chronic nasal congestion.”
If you do have bothersome symptoms, consider seeing an allergist for testing. And don’t forget the children: Dust mite allergy is common among children and a risk factor for developing asthma, said Dr. Platts-Mills. The sooner you intervene, the less likely your child’s symptoms will escalate into something more severe.
Allergy tests take about an hour and most insurers cover the expense, which can range from $500 to $1,000, depending on where you live. At the end of your visit, you will know what you are allergic to and to what degree.
THE SCIENTIFIC CONTROVERSY
If you are allergic to dust mites, you will need to reduce your exposure to them. But first, you should know about a scientific dispute over bedding.
Most researchers endorse protective bedding as a way to reduce exposure to dust mites. But a meta-analysis of 54 studies on interventions to control dust mites, published in 2008 by the nonprofit Cochrane Collaboration, concluded, “Chemical and physical methods aimed at reducing exposure to house dust mite allergens cannot be recommended.”
Dr. Peter Gotzsche, lead author of the study and director of the Nordic Cochrane Center in Copenhagen, said in an e-mail, “The reduction in exposure to mites and mite allergens that can be obtained by encasings, chemicals, vacuum cleaning, etc., is far too small to have any effect.”
Most allergists and environmental health experts disagree. The American Academy of Allergy, Asthma and Immunology and the National Heart, Lung and Blood Institute, for example, tell allergic consumers to encase mattresses, box springs and pillows in special allergen-proof fabric covers.
Though the research has been mixed, a study published in the New England Journal of Medicine in 2004 found that covering children’s mattresses and pillows with special mite-proof casings helped reduce asthma complications. A similar study, published by Dutch researchers in Clinical and Experimental Allergy in 2002, found that mattress encasings helped to reduce symptoms in asthmatic patients and concluded that “their use should be recommended.”
APPROPRIATE STEPS
Dr. Gotzsche’s views notwithstanding, most experts recommend a variety of interventions for those allergic to dust mites.
Mites multiply quickly in high humidity and can take up residence in sheets and blankets in a matter of days. Wash your bedding (including comforters and duvet covers) weekly in hot water and use a hot dryer. It is not necessary to replace them with new linens. But if you’d rather start fresh, spring for new pillows.
It doesn’t matter what kind you buy; it matters more that you protect both your pillows and your mattress with special mite-proof covers, experts say.
The new covers are made of old-fashioned typewriter ribbon material, which has a tight weave that does not allow mites to penetrate but is soft to the touch. Be sure you get covers from a reputable company, like Mission Allergy or National Allergy Supply. Covers cost $15 to $40 for pillows and $100 or more for mattresses.
If your allergies are severe, your doctor may also suggest that you remove carpets from your home, or at least from your bedroom, and use Venetian blinds rather than fabric drapes. Dust mites take refuge in carpets but can’t live on hard surfaces like wood floors or plastic.
If you aren’t allergic to dust mites, forget the urban horror stories about tumbleweeds of mite feces blowing through your home. Simply replace your pillows when you notice they are not supporting your neck and head as well as they used to.
An exception to the rule: If you spill liquid on pillows or comforters, consider discarding them, to avoid hatching a mold colony where you sleep.
My husband and I didn’t need new pillows, it turns out, and if we were allergic to dust mites, we should have gotten protective covers, too. Still, our new pillows are a joy to sleep on, much more luxurious and supportive than the old ones. Maybe it wasn’t so much to pay for a chance to rest easy.
(and Who Shouldn’t)
By Lesley Alderman : NY Times : March 4, 2011
The other night my husband and I were having serious pillow talk. But not the kind you might think. Ours went something like this:
Husband: Don’t we need new pillows? We’ve been sleeping on ours for, like, seven years.
Me: They seem fine to me.
Husband: But they are probably full of dust mites and other gross stuff.
Me: Ugh. O.K.
A cool $400 later, I had bought eight new down pillows — two for each member of our family. I was about to investigate dust mite protection covers (an additional $100) when I stopped myself.
Really, should I care this much about dust mites? I have mild allergies and so does my husband, but I’ve never felt that my pillow was making me sick. And these fluffy new pillows and covers were expensive.
Dust mites are microscopic creatures, about 0.4 millimeters in length, that feast on flakes of human skin. Their feces contains a substance called DerP1, a very potent allergen. People who are allergic to dust mites may have asthmalike symptoms, eczema or chronic sinus problems.
Many of us believe that bed linens, pillows and mattresses must be replaced regularly to prevent them from becoming home to vast colonies of these nasty creatures, lest their feces spread and cause allergic reactions in family members.
According to most experts, the truth is a bit more prosaic. People who have allergies to dust mites should indeed take measures to protect themselves. But everyone else can skip the expensive trips to Linens “R” Us.
The trouble is, it’s not always clear whether you have a mite allergy. And even when you know you are allergic, there’s a lot of confusion about which strategies really work.
Here’s how to decide if you should be worrying about your bedding and the dust mites that take up residence in them — along with expert advice on the most effective home interventions.
AN ALLERGY TEST
Mites proliferate in warm, humid climates. They are almost nonexistent in places like New Mexico but thrive in tropical areas like Florida. Here’s a mite test: “If your home is full of static electricity, you likely do not have mites at the moment,” said Dr. Thomas Platts-Mills, director of the Asthma and Allergic Disease Center at the University of Virginia.
But if the temperature and humidity rise, watch out. About one in four Americans has some type of allergy, and within that group about two-thirds are allergic to dust mites, said Dr. James Sublett, an allergist in Louisville, Ky., who is chairman of the Indoor Allergen Committee of the American College of Allergy, Asthma and Immunology.
“Very few people are allergic to just one thing,” he said.
If you’re not sure whether you have a sensitivity to dust mites, ask yourself these questions: Do I have persistent sniffles and sinus headaches? Do I often wake up with scratchy eyes? Do I sneeze repeatedly first thing in the morning?
“Sometimes symptoms are obvious, but sometimes they are subtle,” said Dr. Diego Saporta, an otolaryngologist in Elizabeth, N.J., who specializes in allergy management. “Your only symptom might be chronic nasal congestion.”
If you do have bothersome symptoms, consider seeing an allergist for testing. And don’t forget the children: Dust mite allergy is common among children and a risk factor for developing asthma, said Dr. Platts-Mills. The sooner you intervene, the less likely your child’s symptoms will escalate into something more severe.
Allergy tests take about an hour and most insurers cover the expense, which can range from $500 to $1,000, depending on where you live. At the end of your visit, you will know what you are allergic to and to what degree.
THE SCIENTIFIC CONTROVERSY
If you are allergic to dust mites, you will need to reduce your exposure to them. But first, you should know about a scientific dispute over bedding.
Most researchers endorse protective bedding as a way to reduce exposure to dust mites. But a meta-analysis of 54 studies on interventions to control dust mites, published in 2008 by the nonprofit Cochrane Collaboration, concluded, “Chemical and physical methods aimed at reducing exposure to house dust mite allergens cannot be recommended.”
Dr. Peter Gotzsche, lead author of the study and director of the Nordic Cochrane Center in Copenhagen, said in an e-mail, “The reduction in exposure to mites and mite allergens that can be obtained by encasings, chemicals, vacuum cleaning, etc., is far too small to have any effect.”
Most allergists and environmental health experts disagree. The American Academy of Allergy, Asthma and Immunology and the National Heart, Lung and Blood Institute, for example, tell allergic consumers to encase mattresses, box springs and pillows in special allergen-proof fabric covers.
Though the research has been mixed, a study published in the New England Journal of Medicine in 2004 found that covering children’s mattresses and pillows with special mite-proof casings helped reduce asthma complications. A similar study, published by Dutch researchers in Clinical and Experimental Allergy in 2002, found that mattress encasings helped to reduce symptoms in asthmatic patients and concluded that “their use should be recommended.”
APPROPRIATE STEPS
Dr. Gotzsche’s views notwithstanding, most experts recommend a variety of interventions for those allergic to dust mites.
Mites multiply quickly in high humidity and can take up residence in sheets and blankets in a matter of days. Wash your bedding (including comforters and duvet covers) weekly in hot water and use a hot dryer. It is not necessary to replace them with new linens. But if you’d rather start fresh, spring for new pillows.
It doesn’t matter what kind you buy; it matters more that you protect both your pillows and your mattress with special mite-proof covers, experts say.
The new covers are made of old-fashioned typewriter ribbon material, which has a tight weave that does not allow mites to penetrate but is soft to the touch. Be sure you get covers from a reputable company, like Mission Allergy or National Allergy Supply. Covers cost $15 to $40 for pillows and $100 or more for mattresses.
If your allergies are severe, your doctor may also suggest that you remove carpets from your home, or at least from your bedroom, and use Venetian blinds rather than fabric drapes. Dust mites take refuge in carpets but can’t live on hard surfaces like wood floors or plastic.
If you aren’t allergic to dust mites, forget the urban horror stories about tumbleweeds of mite feces blowing through your home. Simply replace your pillows when you notice they are not supporting your neck and head as well as they used to.
An exception to the rule: If you spill liquid on pillows or comforters, consider discarding them, to avoid hatching a mold colony where you sleep.
My husband and I didn’t need new pillows, it turns out, and if we were allergic to dust mites, we should have gotten protective covers, too. Still, our new pillows are a joy to sleep on, much more luxurious and supportive than the old ones. Maybe it wasn’t so much to pay for a chance to rest easy.
Adult Mystery: Sudden 'Allergy
By Melinda Beck : WSJ : August 16, 2011
Teri Augustyn developed a runny nose and itchy eyes when she went near grasses, trees and even the dog she'd had for years after she moved from Michigan to Washington when she was 38.
Pollen may irritate respiratory passages more as people age.
At age 25, Kiley Gwynn started having headaches and stomachaches and one day her regular soy chai latte gave her a 20-minute coughing fit. Her allergist traced the reaction to soy, which she'd eaten all of her life without problems.
Lauri Granoff was 53 when she opened a package of wet wipes and suddenly couldn't breathe. The fragrance set off an asthma-like reaction that made her throat close up and her chest tighten. Now, coming close to perfume, hairspray, hand lotion or other chemical fragrance will leave her gasping for breath. She enclosed an insert in her son's wedding invitations begging guests not to wear scented products of any kind.
Severe reactions like these to foods, drugs, pollen and other substances can develop, seemingly out of the blue, at any age.
The symptoms mimic allergy attacks, and the misery they cause can be just as severe.
But many times, they aren't true allergies, experts say. The reactions involve different biochemical pathways than those in allergies, and they often respond to different treatments.
A true allergic reaction occurs when a person's immune system misidentifies a harmless substance as an invader and develops IgE antibodies against it. The antibodies attach themselves to mast cells in the bloodstream, which release histamines and other inflammatory chemicals whenever that substance is near. The resulting inflammation may cause a runny nose, itchy eyes, swelling, hives or skin rashes.
But when seasonal allergy symptoms crop up for the first time in adulthood, they are more likely due to an irritation of the nasal membranes known as vasomotor or nonallergic rhinitis than to an IgE response, experts say.
As people age, their immune systems weaken and their mucous membranes lose elasticity, making them more sensitive to irritants. "Even cold air becomes more problematic as we get older," says Rohit Katial, director of adult allergy and immunology services at National Jewish Health, a Denver hospital. "Suddenly your nose starts running all the time."
Because the IgE reaction isn't involved in vasomotor rhinitis, antihistamines and other over-the-counter allergy medications aren't very effective, nor are allergy shots. But nasal steroid sprays such as Flonase and Nasonex can reduce the inflammation and make nasal passages less sensitive. "Half the people who come to me who think they have allergies don't, and they're frustrated because their over-the-counter allergy medications don't work," says Michael Blaiss, an allergist at the University of Tennessee in Memphis and past president of the American College of Allergy, Asthma and Immunology.
Reactions to perfume and other scents also are more likely to be irritations than allergies and can range from headaches to life-threatening asthma-like attacks. Cigarette smoke, soot and other airborne particles also can be irritating to people who are sensitive, and there, too, antihistamines generally aren't effective.
Many sufferers, though, find relief using inhalers with fast-acting anticholinergic agents, which block the nerve impulses that play a role in the reactions. Ms. Granoff also uses a carbon-filter mask to screen out scents and particulates and carries a portable nebulizer and an epinephrine pen for emergencies. Many patients at National Jewish Health learn breathing exercises to help keep their airways open during an attack.
About 1% of people—and 10% of those with asthma—develop a sudden sensitivity to aspirin, ibuprofen and other nonsteroidal anti-inflammatory drugs (NSAIDs). Experts say these reactions—which may include swelling of the lips, tongue, hands and feet, as well as hives and other rashes—may happen because the NSAID doesn't fully block the body's inflammation-causing chemicals, and some overproduce instead. Researchers aren't sure why this suddenly occurs in people who have taken NSAIDs without problems for years, although stress and genetics may play roles.
Some food allergies actually do develop mainly in adults. A prime example is shellfish. But in many other cases, reactions that are widely assumed to be food allergies prove negative in medically supervised food challenges.
Often, it is simply mistaken identity. "Somebody might develop hives one afternoon, and it's natural to think, 'It must have been the eggs I had at lunch'," says Dr. Katial. "A lot of times we don't know what the cause is, but we know it's not the food allergy."
Skin-prick and blood tests can help confirm or rule out allergies by revealing the presence of IgE antibodies to specific substances. But a positive skin test alone doesn't necessarily mean a person will have a bad reaction from eating the food. That's why experts say children and adults shouldn't eliminate foods from their diets based on suspicion or a positive skin test alone.
The incidence of actual allergies is rising in adults and children around the world, for reasons that aren't totally understood. A popular theory is that modern hygiene has reduced the number of germs children are exposed to, so that their immune systems don't develop fully and attack harmless substances. Allergies may develop late in life, or seem to do so, in adults who had mild seasonal allergies that went unnoticed when they were children; the allergies may have become more severe as pollen counts have worsened.
Some environmental triggers are getting worse. In northern U. S. and Canada, pollen season in 2009 lasted 27 days longer than in 1995, a recent study found. Ragweed season in the New York-New Jersey area started last week, 10 days earlier than usual, says Leonard Bielory, an allergy specialist at Rutgers University and co-author of the study in the Proceedings of the National Academy of Science. "My prediction is that next week, it will just explode."
A new environmental irritant, a previously mild allergy and the aging process can add up to new misery. Pregnancy, hormonal changes and many illnesses can alter a person's immune system. "As we get older, things change," Dr. Bielory says.
Does it matter which mechanism creates a bad reaction? Not to suffering patients—although some worry that an "irritation" isn't taken as seriously as an "allergy." But a true diagnosis is critical to getting the right treatment. "I tell primary-care doctors that if you think the patient has allergies and they get better on over-the-counter antihistamines, I don't need to see them," says Dr. Blaiss. "But if they are still having problems or getting worse, we should investigate further."
Allergies and Beyond
Are a runny nose, itchy eyes, swelling or hives signs of an adult-onset allergy—or something else?
Vasomotor rhinitis
Pollen, dander, smoke, perfume—even cold air—can irritate respiratory passages; aging makes people more susceptible
Treatment: Allergy shots and antihistamines don't help, but nasal steroid sprays, anticholinergic inhalers, masks and breathing exercises may provide relief.
Severity: Mild sniffles to life-threatening airway blockage
Prevalence: 20% of U.S. adults report seasonal symptoms, 4% fragrance sensitivity
Aspirin sensitivity
Nonsteroidal anti-inflammatory drugs like aspirin and ibuprofen can trigger swelling, hives and breathing problems
Treatment: IV antihistamines; epinephrine; avoidance; desensitization
Severity: Mild swelling to life-threatening anaphylaxis
Prevalence: 1% of population; 10% of asthmatics
Seasonal allergies
Rising pollen counts, ozone and other pollutants are making some mild allergies far more severe
Treatment: Antihistamines; nasal sprays, steroids, allergy shots
Severity: Mild sneezing to congestion that interferes with work, sleep, daily life
Prevalence: 20% to 40% of U.S. adults report some form
of allergy
By Melinda Beck : WSJ : August 16, 2011
Teri Augustyn developed a runny nose and itchy eyes when she went near grasses, trees and even the dog she'd had for years after she moved from Michigan to Washington when she was 38.
Pollen may irritate respiratory passages more as people age.
At age 25, Kiley Gwynn started having headaches and stomachaches and one day her regular soy chai latte gave her a 20-minute coughing fit. Her allergist traced the reaction to soy, which she'd eaten all of her life without problems.
Lauri Granoff was 53 when she opened a package of wet wipes and suddenly couldn't breathe. The fragrance set off an asthma-like reaction that made her throat close up and her chest tighten. Now, coming close to perfume, hairspray, hand lotion or other chemical fragrance will leave her gasping for breath. She enclosed an insert in her son's wedding invitations begging guests not to wear scented products of any kind.
Severe reactions like these to foods, drugs, pollen and other substances can develop, seemingly out of the blue, at any age.
The symptoms mimic allergy attacks, and the misery they cause can be just as severe.
But many times, they aren't true allergies, experts say. The reactions involve different biochemical pathways than those in allergies, and they often respond to different treatments.
A true allergic reaction occurs when a person's immune system misidentifies a harmless substance as an invader and develops IgE antibodies against it. The antibodies attach themselves to mast cells in the bloodstream, which release histamines and other inflammatory chemicals whenever that substance is near. The resulting inflammation may cause a runny nose, itchy eyes, swelling, hives or skin rashes.
But when seasonal allergy symptoms crop up for the first time in adulthood, they are more likely due to an irritation of the nasal membranes known as vasomotor or nonallergic rhinitis than to an IgE response, experts say.
As people age, their immune systems weaken and their mucous membranes lose elasticity, making them more sensitive to irritants. "Even cold air becomes more problematic as we get older," says Rohit Katial, director of adult allergy and immunology services at National Jewish Health, a Denver hospital. "Suddenly your nose starts running all the time."
Because the IgE reaction isn't involved in vasomotor rhinitis, antihistamines and other over-the-counter allergy medications aren't very effective, nor are allergy shots. But nasal steroid sprays such as Flonase and Nasonex can reduce the inflammation and make nasal passages less sensitive. "Half the people who come to me who think they have allergies don't, and they're frustrated because their over-the-counter allergy medications don't work," says Michael Blaiss, an allergist at the University of Tennessee in Memphis and past president of the American College of Allergy, Asthma and Immunology.
Reactions to perfume and other scents also are more likely to be irritations than allergies and can range from headaches to life-threatening asthma-like attacks. Cigarette smoke, soot and other airborne particles also can be irritating to people who are sensitive, and there, too, antihistamines generally aren't effective.
Many sufferers, though, find relief using inhalers with fast-acting anticholinergic agents, which block the nerve impulses that play a role in the reactions. Ms. Granoff also uses a carbon-filter mask to screen out scents and particulates and carries a portable nebulizer and an epinephrine pen for emergencies. Many patients at National Jewish Health learn breathing exercises to help keep their airways open during an attack.
About 1% of people—and 10% of those with asthma—develop a sudden sensitivity to aspirin, ibuprofen and other nonsteroidal anti-inflammatory drugs (NSAIDs). Experts say these reactions—which may include swelling of the lips, tongue, hands and feet, as well as hives and other rashes—may happen because the NSAID doesn't fully block the body's inflammation-causing chemicals, and some overproduce instead. Researchers aren't sure why this suddenly occurs in people who have taken NSAIDs without problems for years, although stress and genetics may play roles.
Some food allergies actually do develop mainly in adults. A prime example is shellfish. But in many other cases, reactions that are widely assumed to be food allergies prove negative in medically supervised food challenges.
Often, it is simply mistaken identity. "Somebody might develop hives one afternoon, and it's natural to think, 'It must have been the eggs I had at lunch'," says Dr. Katial. "A lot of times we don't know what the cause is, but we know it's not the food allergy."
Skin-prick and blood tests can help confirm or rule out allergies by revealing the presence of IgE antibodies to specific substances. But a positive skin test alone doesn't necessarily mean a person will have a bad reaction from eating the food. That's why experts say children and adults shouldn't eliminate foods from their diets based on suspicion or a positive skin test alone.
The incidence of actual allergies is rising in adults and children around the world, for reasons that aren't totally understood. A popular theory is that modern hygiene has reduced the number of germs children are exposed to, so that their immune systems don't develop fully and attack harmless substances. Allergies may develop late in life, or seem to do so, in adults who had mild seasonal allergies that went unnoticed when they were children; the allergies may have become more severe as pollen counts have worsened.
Some environmental triggers are getting worse. In northern U. S. and Canada, pollen season in 2009 lasted 27 days longer than in 1995, a recent study found. Ragweed season in the New York-New Jersey area started last week, 10 days earlier than usual, says Leonard Bielory, an allergy specialist at Rutgers University and co-author of the study in the Proceedings of the National Academy of Science. "My prediction is that next week, it will just explode."
A new environmental irritant, a previously mild allergy and the aging process can add up to new misery. Pregnancy, hormonal changes and many illnesses can alter a person's immune system. "As we get older, things change," Dr. Bielory says.
Does it matter which mechanism creates a bad reaction? Not to suffering patients—although some worry that an "irritation" isn't taken as seriously as an "allergy." But a true diagnosis is critical to getting the right treatment. "I tell primary-care doctors that if you think the patient has allergies and they get better on over-the-counter antihistamines, I don't need to see them," says Dr. Blaiss. "But if they are still having problems or getting worse, we should investigate further."
Allergies and Beyond
Are a runny nose, itchy eyes, swelling or hives signs of an adult-onset allergy—or something else?
Vasomotor rhinitis
Pollen, dander, smoke, perfume—even cold air—can irritate respiratory passages; aging makes people more susceptible
Treatment: Allergy shots and antihistamines don't help, but nasal steroid sprays, anticholinergic inhalers, masks and breathing exercises may provide relief.
Severity: Mild sniffles to life-threatening airway blockage
Prevalence: 20% of U.S. adults report seasonal symptoms, 4% fragrance sensitivity
Aspirin sensitivity
Nonsteroidal anti-inflammatory drugs like aspirin and ibuprofen can trigger swelling, hives and breathing problems
Treatment: IV antihistamines; epinephrine; avoidance; desensitization
Severity: Mild swelling to life-threatening anaphylaxis
Prevalence: 1% of population; 10% of asthmatics
Seasonal allergies
Rising pollen counts, ozone and other pollutants are making some mild allergies far more severe
Treatment: Antihistamines; nasal sprays, steroids, allergy shots
Severity: Mild sneezing to congestion that interferes with work, sleep, daily life
Prevalence: 20% to 40% of U.S. adults report some form
of allergy
Infinite Itch: Learning to Live With
Hives
Jane E. Brody : NY Times : May 7, 2012
Bill Brancaccio inherited a sharp mind and a brawny physique from his Long Island family, and something more: a susceptibility to hives, itchy, red welts that can last for minutes or for days, sometimes recurring for weeks, months or even years.
Mr. Brancaccio’s first attack occurred in his midteens. “I became allergic to cold water,” he said. “I went swimming and developed hives all over my body. They went away in an hour or two, but recurred every time I swam.”
When he was stung by a bee a year or so later, hives popped out over half his body and lasted about a day. Then, as a 21-year-old college senior taking several honors classes, he said, “All of a sudden, out of the blue, I had hives over my entire body. Only my face was spared.”
Despite a series of treatments that did little more than add 40 pounds to his athletic frame, the attack lasted from March through August. He said his intensely itchy body “looked as if it had been burned.”
To hide his terrible-looking skin and ease the itchiness somewhat, he wore long sleeves and long pants. But the itching kept him awake night after night. After not sleeping for two or three days, he said, he “would crash and sleep 12 hours straight.”
He had to drop some classes but managed to graduate and get a job in finance in New York City. But doxepin, the drug that finally suppressed the hives, made him so sleepy that he repeatedly dozed off on a desk during six weeks of job training.
Mr. Brancaccio has a condition called chronic idiopathic urticaria, which dermatologists believe is an autoimmune disorder and which affects one in a thousand people in this country. It often runs in families.
Mr. Brancaccio’s mother, Lydia Brancaccio, of Water Mill, N.Y., experienced her first episode of hives only recently. But, she said, “My mother, sister and daughter have them, and they can last for weeks.”
Her sister “reacts to sun and can’t go anywhere on vacation where there’s sun,” Ms. Brancaccio added. “Even sun-blocking clothing doesn’t help. She just gets covered with hives.”
The disorder, Mr. Brancaccio said, “exposes you to the limits of modern medicine.” The term “idiopathic” indicates that the cause is not known.
The name “makes it seem like the problem is solved,” he said. “But you’ve still got hives.”
Cause Unknown
Hives of one sort or another afflicts about one person in five at some time during their lives. For most, the problem is short-lived or “acute,” lasting less than six weeks. A specific cause, or trigger, can usually be identified.
Common triggers of acute urticaria include medications like antibiotics, aspirin and other Nsaids (nonsteroidal anti-inflammatory drugs), and opiates; foods like nuts, peanuts, fish and shellfish, wheat, eggs, milk and soybeans; infections of all kinds, including upper respiratory infections; insect stings, especially by bees and wasps; allergens like latex or pollen; and physical stimuli like cold, heat, exercise or sweat.
As I recall, a high school friend who was sensitive to cold air used to develop hives on her face going to and from school in winter. Dr. Vincent S. Beltrani, a dermatologist in Poughkeepsie, N.Y., noted that in patients whose symptoms have an identifiable cause, “the episode usually resolves spontaneously within hours after the trigger is removed.”
But the likelihood of finding a cause for chronic urticaria “is quite small,” Dr. Supriya Varadarajulu, allergist at the Park Nicollet Clinic in Minneapolis, said in an interview. In a few cases, a cause can be identified by taking a careful history, “but usually the condition remains idiopathic.”
Studies have indicated that up to 40 percent of patients with chronic urticaria, especially those more severely affected, have antibodies targeting the body’s own tissues circulating in their blood. These patients or their blood relatives may have other autoimmune disorders, like thyroid disease, diabetes or lupus.
About a quarter of patients with chronic urticaria have thyroid autoantibodies, and many of them are found to have thyroid dysfunction. Unfortunately, treating their thyroid condition does not eliminate the hives, Dr. Varadarajulu said.
Some people who get hives also have a related condition called angioedema, a swelling of tissues deep in the skin (hives develop at the skin’s surface). Although angioedema usually doesn’t cause itchiness, it can cause pain or a burning sensation.
It most often involves the lips, eyelids, face, arms and legs and genitalia. Dr. Varadarajulu said the swelling can show up suddenly and last for hours or days. A friend of mine who had angioedema of the face occasionally needed emergency treatment when the swelling of her tongue threatened to cut off her airway.
Treating Outbreaks
The duration of chronic hives varies widely. According to Dr. Beltrani, it disappears in 3 to 12 months in up to half of patients, but persists for up to five years in 20 percent of patients and for 20 or more years in 1.5 percent. Half of patients will have recurrences from time to time.
He and Dr. Varadarajulu emphasized that there was no magic bullet, or even a standard treatment, for chronic idiopathic urticaria. Rather, a series of antihistamines are commonly tried, both singly and in combination.
Dr. Varadarajulu said one of the newer nonsedating oral antihistamines is the treatment of first choice, though patients often need twice the standard dose, taking the drug every 12 hours rather than once a day.
Sometimes Zantac or Tagamet is added; though normally prescribed for heartburn, these drugs have antihistamine properties.
Another option, doxepin, the drug that finally helped Mr. Brancaccio, is an antidepressant with both antihistamine properties and potent anti-itch action. It causes severe sedation and dry mouth, however, and is used only if less debilitating therapies fail to bring relief.
Still, chronic urticaria remains a challenge because “the extreme itchiness can drive people crazy,” Dr. Varadarajulu said, and no cause can be found in most cases.
Nonetheless, she said, “excellent disease control can be achieved with appropriate use of antihistamines until the disease spontaneously resolves over time.”
Mr. Brancaccio had to take doxepin for many weeks after his hives abated to keep them from recurring. Now 30, living and working in Manhattan, he has been in remission for years.
“I don’t know why, but I no longer react to cold water or bee stings,” he said.
MOLD :
Don’t Catch What Ails Your House
By Jane E. Brody : NY Times : Sept 1, 2014
You don’t need a flood to develop a mold problem. It can happen anywhere moisture is present — a hidden leak, for example, or condensation around windows or pipes. You may not even be aware of the problem, only the distress it causes.
Typical symptoms resemble those of an allergy like hay fever: a runny nose, sneezing, red or itchy eyes, throat irritation and coughing. Some people develop a skin rash; those with asthma may have an attack. According to research by the Mayo Clinic, an immunological response to mold may cause most cases of chronic sinusitis.
Mold can even infect the central nervous system, often fatally, as occurred in a 2012 outbreak of meningitis from epidural injections contaminated by Exserohilum rostratum. Of the 751 people infected across the country, 64 died.
The types of mold usually found in homes do not produce dangerous toxins. But they can bring misery and are best controlled by preventing their growth.
Molds are a type of fungus, and they grow by releasing spores into the air. The spores are not visible to the naked eye, but when they land on a moist surface (or when the surface they are on becomes moist), they begin to grow. Outdoors, molds play an important role in the decomposition of organic matter, like leaves and fallen trees.
Even the driest buildings contain mold spores, and those with indoor moisture may have thousands in every cubic foot of air. The spores are ubiquitous and can survive extreme dryness and cold, remaining dormant until moisture and oxygen provide a chance to grow.
These measures can reduce the buildup of indoor mold:
■ Fix leaks immediately, and thoroughly dry the affected area.
■ Regularly clear debris from roof gutters.
■ Keep air conditioner and refrigerator drip pans clean.
■ Insulate cold-water pipes.
■ Use an air conditioner or a dehumidifier, or both, and change the filters regularly to maintain a relative humidity below 60 percent. (The lower, the better.)
■ Vent appliances like clothes dryers that generate moisture to the outside.
■ Use an exhaust fan or open a window when washing dishes, cooking or showering.
■ Keep crawl space vents clear.
Do not use carpets in potentially moist areas like a laundry room, bathroom and basement. Replace sponges and dishcloths often, or wash and dry them with the regular laundry.
Roof leaks can be especially challenging, leaving wet insulation and moisture behind walls. Roofing is best restored or replaced on a schedule before a leak occurs.
Keeping a house warm suppresses mold growth. Alas, my house still gets musty in winter; to save oil and money, I set the thermostat at 55 degrees when I’m not there.
Some people, especially those with severe allergies, chronic lung disease or suppressed immunity, are affected by outdoor mold in compost piles, cut grass and wooded areas. When cleaning the yard and raking or sweeping dead leaves, they should consider wearing a face mask or an N-95 respirator (a fancy dust mask that costs $12 to $25).
Cleaning up mold requires care. Limit your exposure by wearing goggles, a face mask and long rubber, neoprene or PVC gloves. You need not use chlorine bleach; soap and water, or a nontoxic commercial cleaner and a scrubbing sponge or brush, will work well on hard surfaces. Dry the area thoroughly after cleaning.
If you do use a bleach solution (no stronger than one cup of bleach to one gallon of water), never mix it with ammonia or a product that contains ammonia.
Do not paint over or caulk moldy surfaces. Clean away the mold first, and then use paint with a mold inhibitor.
Porous materials like ceiling tiles and carpets that have become moldy can be difficult to clean adequately and usually must be replaced.
You may need a professional contractor skilled in mold cleanup if the affected area is larger than 10 square feet. The Environmental Protection Agency recommends checking references and making sure the contractor consults its guide, Mold Remediation in Schools and Commercial Buildings, available at www.epa.gov/mold. The agency also provides a guide to cleaning contaminated heating and air conditioning systems.
WE REFER OUR PATIENTS TO THE FOLLOWING ALLERGISTS
- Gary P. Gurka, MD Phone: (781)648-2540 in Arlington
- Hana M. Laznickova, MD Phone: (781)861-2049 in Lexington
- Vandana Krishna, MD Phone: (781)729-2293 in Winchester
- Curtis T. Moody, MD Phone: (617)735-8750 in Brookline
- Frank J. Twarog, MD Phone: (617)735-8750 in Brookline