- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
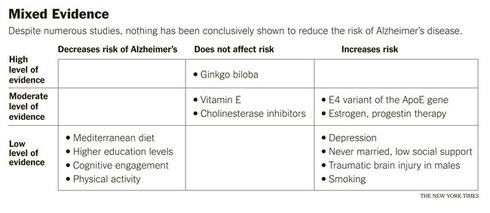
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Alzheimer's Disease
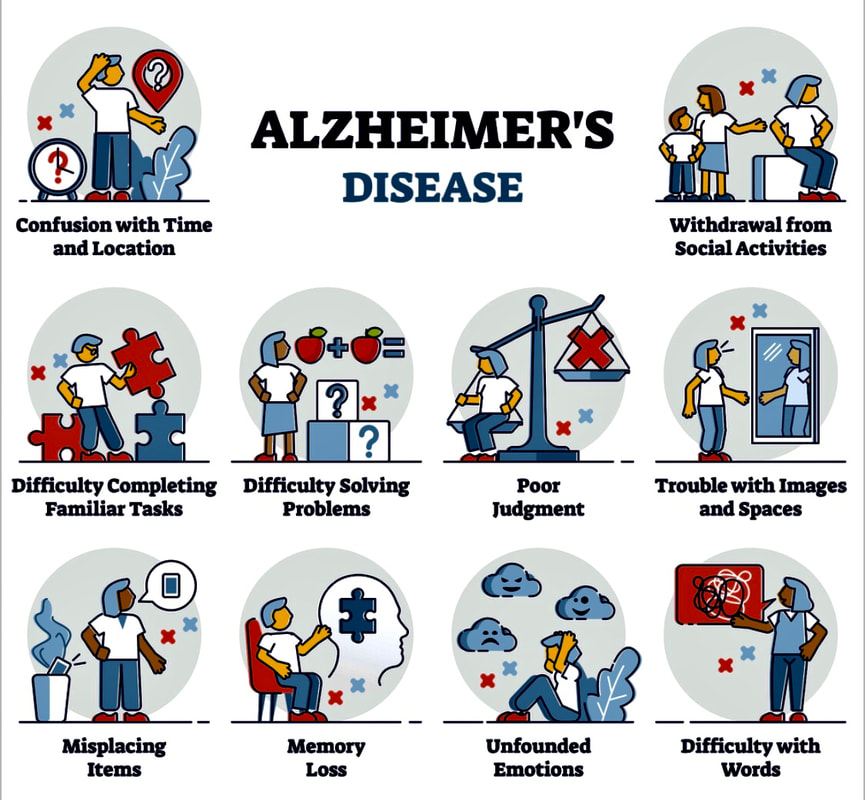
10 warning signs of Alzheimer's:
1. Memory loss. Forgetting recently learned information is one of the most common early signs of dementia. A person begins to forget more often and is unable to recall the information later.
- What's normal? Forgetting names or appointments occasionally.
2. Difficulty performing familiar tasks. People with dementia often find it hard to plan or complete everyday tasks. Individuals may lose track of the steps involved in preparing a meal, placing a telephone call or playing a game.
- What's normal? Occasionally forgetting why you came into a room or what you planned to say.
3. Problems with language. People with Alzheimer’s disease often forget simple words or substitute unusual words, making their speech or writing hard to understand. They may be unable to find the toothbrush, for example, and instead ask for "that thing for my mouth.”
- What's normal? Sometimes having trouble finding the right word.
4. Disorientation to time and place. People with Alzheimer’s disease can become lost in their own neighborhood, forget where they are and how they got there, and not know how to get back home.
- What's normal? Forgetting the day of the week or where you were going.
5. Poor or decreased judgment. Those with Alzheimer’s may dress inappropriately, wearing several layers on a warm day or little clothing in the cold. They may show poor judgment, like giving away large sums of money to telemarketers.
- What's normal? Making a questionable or debatable decision from time to time.
6. Problems with abstract thinking. Someone with Alzheimer’s disease may have unusual difficulty performing complex mental tasks, like forgetting what numbers are for and how they should be used.
- What's normal? Finding it challenging to balance a checkbook.
7. Misplacing things. A person with Alzheimer’s disease may put things in unusual places: an iron in the freezer or a wristwatch in the sugar bowl.
- What's normal? Misplacing keys or a wallet temporarily.
8. Changes in mood or behavior. Someone with Alzheimer’s disease may show rapid mood swings – from calm to tears to anger – for no apparent reason.
- What's normal? Occasionally feeling sad or moody.
9. Changes in personality. The personalities of people with dementia can change dramatically. They may become extremely confused, suspicious, fearful or dependent on a family member.
- What's normal? People’s personalities do change somewhat with age.
10. Loss of initiative. A person with Alzheimer’s disease may become very passive, sitting in front of the TV for hours, sleeping more than usual or not wanting to do usual activities.
- What's normal? Sometimes feeling weary of work or social obligations.
Is It Ordinary Memory Loss, or Alzheimer’s Disease?
By Jane E. Brody : NY Times : May 18, 2015
Soon after her 65th birthday, a close friend became increasingly worried about her memory, wondering if she could have the beginnings of dementia.
Although she seemed to have no more difficulty than the rest of us her age in remembering events, names and places, her physician suggested that, given her level of concern, she should have things checked out.
So she consulted a specialist at Mount Sinai Hospital in New York and had a full-blown neuropsychological assessment — two days of tests of her cognitive abilities. The dozen measures included I.Q. and memory scales, auditory learning and animal naming tests, an oral word association test, a connect-the-dots trail-making test, and a test of her ability to copy complex figures.
The result: reassurance and relief. Everything was in the normal range for her age, and she registered as superior on the ability to perform tasks and solve problems.
Fears about memory issues, commonplace among those of us who often misplace our cellphones and mix up the names of our children, are likely to skyrocket as baby boomers move into their 70s, 80s and beyond.
Many may be unwilling to wait to have their memories tested until symptoms develop that could herald encroaching dementia or Alzheimer’s disease, like finding one’s glasses in the refrigerator, getting lost on a familiar route or being unable to follow directions or normal conversation.
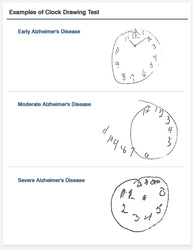
But nor do people have to endure the extensive assessment my friend had. Simple tests done in eight to 12 minutes in a doctor’s office can determine whether memory issues are normal for one’s age or are problematic and warrant a more thorough evaluation. The tests can be administered annually, if necessary, to detect worrisome changes.
However, according to researchers at the University of Michigan, more than half of older adults with signs of memory loss never see a doctor about it. Although there is still no certain way to prevent or forestall age-related cognitive disease, knowing that someone has serious memory problems can alert family members and friends to a need for changes in the person’s living arrangements that can be health- or even lifesaving.
“Early evaluation and identification of people with dementia may help them receive care earlier,” said Dr. Vikas Kotagal, the senior author of the Michigan study. “It can help families make plans for care, help with day-to-day tasks, including medication administration, and watch for future problems that can occur.”
Long the most popular screening test for memory disorders used by primary care doctors is the Mini-Mental State Exam, or MMSE, an eight-minute test in use since 1975. But neurologists say it is less discerning than the slightly longer Montreal Cognitive Assessment, or MoCA, introduced in 1996.
Both tests measure orientation to time, date and place; attention and concentration; ability to calculate; memory; language; and conceptual thinking. But while the MMSE is considered adequate for routine testing of cognitive function by the family doctor, its score can be skewed by a person’s level of education, cultural background, a learning or speech disorder, and language fluency. And according to Dr. Roy Hamilton, a neurologist at the University of Pennsylvania, this test is not sensitive enough to detect signs of mild cognitive impairment.
Furthermore, the MMSE doesn’t test for problems with executive function, defined as the ability to organize, plan and perform tasks efficiently to reach a particular goal.
“Executive function is typically the first area to suffer if you develop cognitive impairment,” Dr. Sam Gandy, the director of the Mount Sinai Center for Cognitive Health and of the N.F.L.’s neurological care program, reported last month in the School of Medicine’s newsletter, Focus on Healthy Aging. “Translated into everyday life, it’s executive function that enables us to carry out activities of daily living, such as dressing and preparing meals.”
The Montreal Cognitive Assessment, which takes 10 to 12 minutes, is more difficult and can pick up problems the MMSE might miss, Dr. Hamilton has noted. It is also more sensitive, better able to discriminate between normal cognitive function and mild impairment or dementia. Still, many memory clinics and neurologists use both tests, along with others like those taken by my friend.
The Montreal test has 11 sections and a possible total score of 30 (25 or better is considered normal). It includes an executive function test called alternating trail-making, in which lines must be drawn from numbers to letters in correct order, 1 to A, 2 to B, and so forth.
Measuring a person’s ability to follow verbal commands includes counting backward from 100 by sevens. To assess abstract thinking, the test asks a person to find common features between two words in each of three pairs. Verbal fluency, a vocabulary test, requires producing 11 or more words that start with a certain letter of the alphabet.
Copying a drawing of a cube and drawing a clock accurately assess so-called visuoconstructional skills, and memory is checked by having the person try to recall five words that were read aloud earlier in the test.
Taking such a test can be quite stressful, although allowances are made for nervousness. But practicing by taking the test in advance of an evaluation can skew the results and hurt the person taking it in the long run.
The MoCA test has proved valid for assessing people who are not demented but could be at risk for developing progressive cognitive decline.
Keep in mind, however, that neither the MMSE nor MoCA are definitive. Rather, they can indicate the need for a more extensive exam like the one my friend had.
Also, it helps to know when not to worry about memory problems. Dr. Kirk R. Daffner, the director of the Center for Brain-Mind Medicine at Brigham and Women’s Hospital in Boston, lists six “normal” memory problems that should not cause concern: a tendency to forget facts or events over time, absent-mindedness, a temporary block in retrieving a memory, recalling something accurately only in part, having a memory distorted by the power of suggestion (the recalled memory may never have happened), and having a memory influenced by bias, experiences or mood.
Questions for Your Doctor What to Ask About Alzheimer's Disease
By Irene M. Wielawski : NY Times Article : August 29, 2007
Confronting a new diagnosis can be frightening — and because research changes so often, confusing. Here are some questions you may not think to ask your doctor, along with notes on why they’re important.
How can we be sure my symptoms aren’t the result of a stroke, mental illness or another treatable condition?
What stage of Alzheimer’s disease am I in? What comes next? Clinicians classify the progressive deterioration of brain function in Alzheimer’s disease into seven stages. By the last stage, patients require round-the-clock care. In the first, second and third stages of this slow moving illness, symptoms are minimal, and many patients work and live independently.
What can I do to preserve my health and mental abilities for as long as possible? Although there are no treatments to halt or cure Alzheimer’s disease, recent studies have suggested that exercise, a healthy diet and mental stimulation may delay the onset of disabling symptoms.
What physical symptoms should I anticipate? Patients typically complain of problems with memory and organizational ability, but Alzheimer’s disease also attacks the brain’s motor centers, resulting in problems with balance, coordination, bladder and bowel control, and certain reflexes, including the ability to swallow. Patients and their caregivers should prepare for mental and physical disabilities.
Should I undergo brain neuroimaging? Imaging of the brain occasionally can help differentiate Alzheimer’s disease from other potential causes of dementia in new patients; however, imaging is rarely useful for determining the severity of the disease.
My children are worried about inheriting this illness. Would it be useful for our family to undergo genetic testing? Scientists have identified several gene mutations associated with an increased risk of developing Alzheimer’s disease, but the predictive value of each mutation is low. As a result, genetic testing is useful only for individuals who have several close relatives suffering from early-onset forms of the disease.
What drugs are currently available for Alzheimer’s disease, and how well do they work? Two types of drugs are currently prescribed for treatment of Alzheimer’s disease. Cholinesterase inhibitors, such as donepezil and galantamine, regulate acetylcholine, a neurotransmitter influential in learning and memory. The only NMDA receptor antagonist on the market, memantine, tamps down excessive brain activity. Both types have been shown to delay brain deterioration for a brief period (6 to 12 months) in about half the people treated.
My family is afraid to let me drive. Would you refer me for a driving evaluation so we can have an objective opinion of my ability? Driving is often a focal point of familial controversy. Diagnosis of Alzheimer’s disease doesn’t always require that a patient immediately stop driving. An objective medical evaluation can be helpful in clarifying the extent of a new patient’s disability.
What can I do to make things easier on my family? Because Alzheimer’s erodes cognitive ability, it’s important for patients to plan for a day when they can no longer take care of their affairs. Newly diagnosed patients should execute medical and durable powers of attorney that authorize spouses or other family members to deal with banks, insurance companies, doctors and others on their behalf.
There is no definitive test for Alzheimer’s disease, and it can be misdiagnosed in patients suffering depression, memory deficits because of normal aging, arterial blockages or even certain vitamin deficiencies. Doctors generally rule out other possibilities, then apply criteria developed by various medical organizations to arrive at the diagnosis.
Cracking the Code to the Memory Vault
By Jane E. Brody : New York Times Article : December 4, 2007
I bless the day 3M invented Post-It notes. I don’t think I could survive without them. They decorate my computer, reminding me how to do things like create a folder, undo an error or save an attachment without opening it. They adorn my refrigerator and kitchen cabinets to help me remember what to buy, what to order and when I have to be where.
Also on my refrigerator is a cartoon by Arnie Levin in The New Yorker showing two elephants. One, covered with notes, says to the other, “As I get older, I find I rely more and more on these sticky notes to remind me.”
I have notes that say, “Take Lunch,” “Take Phone,” “Turn Off Computer!” lest I forget such important tasks when I leave home.
Why do I still remember the symbols for all the elements known when I took chemistry 48 years ago, but don’t recall what I wrote about yesterday?
When I complained to my 30-something son that I cannot seem to remember anything unless I write it down and stare at it, he said reassuringly, “Mom, by now you’ve got so much crammed into your head, something is bound to fall out!”
And I know I’m not alone among the over-50 generation. A good friend, two and a half years my senior, endured a six-hour battery of neuropsychological tests because she feared encroaching Alzheimer’s disease. (She got an all clear.) We tease each other about always having to go everywhere together, because we each supply half a memory.
If my husband precedes me in death, my memory of the movies and plays I have seen will die with him. Though eight years my senior, he remembers not only what we have seen, but also where and when.
And why don’t I have a politician’s memory for names? As a reporter for The Minneapolis Tribune in 1965, I covered Hubert H. Humphrey’s first visit to his home state as vice president. Everywhere he went, he greeted people by name and asked about their relatives, also by name. And seven hours after being introduced to a half-dozen reporters, he said before departing for Washington: “Goodbye, Miss Brody. I’ll give your regards to Brooklyn next time I’m there.”
When I’m introduced to a new person, the name is gone from my memory before the handshake is over. Probably it was never there to start with, because I’ve known since childhood that I’m a visual, not an aural, learner. If a new acquaintance has no name tag, a verbally stated name goes in one ear and out the other, bypassing my brain’s memory cells.
All through school, I took voluminous notes and underlined every important sentence in my textbooks. During exams, I could visualize the answers on their respective pages. No matter how hard I tried to learn just by listening, the lesson was out of my head by the time I left the classroom.
Blocking and Blanking
Few of us escape the experience of walking from one room to another and not remembering why or what for. Chances are an extraneous thought in that brief trek blocked out its original purpose. But if you go back to the first room, you nearly always recall your mission. It’s annoying, but not really embarrassing, not like blanking on the name of someone you know well.
Like the time I tried to introduce my stepmother of 25 years to another guest at my party and could not for the life of me think of her first name. “Sandra, I’d like you to meet my motherhuh, huh, Mrs. Brody,” I finally blurted out.
In “Carved in Sand” (HarperCollins), an enlightening and rather reassuring new book on fading memory in midlife, the writer Cathryn Jakobson Ramin speaks of “‘blocking’ (or ‘blanking’) when names will not come to mind and words dart in and out of consciousness.” Ms. Ramin, like me, has often been stopped cold in the midst of writing when unable to think of what she knows is the perfect word.
Her research found that “word-retrieval failures occur not because of the loss of relevant memories, but because irrelevant ones are activated.”
Daniel L. Schacter, a psychologist and memory expert at Harvard and the author of “The Seven Sins of Memory” (Houghton Mifflin), notes that the concept of blocking exists in 51 languages and that 45 of them have a specific name for it. In English, it’s called “tip of the tongue,” lapses that become increasingly common and challenging from midlife onward.
“People can produce virtually everything they know about a person or everything they know about a word, except its label,” Dr. Schacter wrote. My friends and I often find ourselves talking about “you know who” and “thingamajigs.”
How I Cope
Mnemonics can be useful, if you can remember them and what they stand for. When my 7-year-old grandson told me to “never eat Shredded Wheat,” which he knows I like, he laughed and said it helped him remember “north, east, south and west.” To remember what I have to do or buy when I can’t write it down, I try to concoct an unforgettable mnemonic like “Babies Are Little Children” for bananas, apples, lettuce and cereal.
Whenever possible, I associate a new name with a tangible object: “Cucumber” for Kirby, the lifeguard at the Y; “ravioli” for Ralph, who sits at the desk; and “sherry” for Sherry, the locker room attendant.
For fellow Y members, after learning a name, I use it every chance I get: “Hi, Jeanette,” “So long, Sue, have a nice day,” “Cynthia, you’re early today,” and “Aviva, how’s your new job?”
And I continue to say their names aloud even after I think that they are etched in stone in my memory.
At a dinner where I’m to be seated with a table of strangers, I check the list of others at the table in advance to help me remember their names when we are introduced. And for groups that meet infrequently, I campaign for name tags. No one should have to remember the names of people she sees once or twice a year.
Though I have long worked in a state of organized chaos (I know where everything is, as long as no one moves it), I needed a better system as I advanced in years. Now, every potentially important piece of paper must go in a labeled file (even if that file has only one thing in it), and the files stored alphabetically in a labeled drawer or box, lest they never be found again.
Also, I resist all urges to reorganize my files — or my clothes, shoes, groceries or tools —because I seem to remember only the first place I put something. Move it to a new location, and it is lost until and unless I stumble upon it accidentally.
Finally, to remember when things must be done like move the car, pick up the grandchildren and turn off the oven, I invested heavily in good kitchen timers and scattered them about the house. The best I have found is made by West Bend. The model number is 40005X, and it runs for a very long time on one AAA battery.
Mental Reserves Keep Brains Agile
By Jane E. Brody : NY Times Article : December 11, 2007
My husband, at 74, is the baby of his bridge group, which includes a woman of 85 and a man of 89. This challenging game demands an excellent memory (for bids, cards played, rules and so on) and an ability to think strategically and read subtle psychological cues. Never having had a head for cards, I continue to be amazed by the mental agility of these septua- and octogenarians.
The brain, like every other part of the body, changes with age, and those changes can impede clear thinking and memory. Yet many older people seem to remain sharp as a tack well into their 80s and beyond. Although their pace may have slowed, they continue to work, travel, attend plays and concerts, play cards and board games, study foreign languages, design buildings, work with computers, write books, do puzzles, knit or perform other mentally challenging tasks that can befuddle people much younger.
But when these sharp old folks die, autopsy studies often reveal extensive brain abnormalities like those in patients with Alzheimer’s. Dr. Nikolaos Scarmeas and Yaakov Stern at Columbia University Medical Center recall that in 1988, a study of “cognitively normal elderly women” showed that they had “advanced Alzheimer’s disease pathology in their brains at death.” Later studies indicated that up to two-thirds of people with autopsy findings of Alzheimer’s disease were cognitively intact when they died.
“Something must account for the disjunction between the degree of brain damage and its outcome,” the Columbia scientists deduced. And that something, they and others suggest, is “cognitive reserve.”
Cognitive reserve, in this theory, refers to the brain’s ability to develop and maintain extra neurons and connections between them via axons and dendrites. Later in life, these connections may help compensate for the rise in dementia-related brain pathology that accompanies normal aging.
Exercise: Mental ...
As Cathryn Jakobson Ramin relates in her new book, “Carved in Sand: When Attention Fails and Memory Fades in Midlife” (HarperCollins), the brains of animals exposed to greater physical and mental stimulation appear to have a greater number of healthy nerve cells and connections between them. Scientists theorize that this excess of working neurons and interconnections compensates for damaged ones to ward off dementia.
Observing this, Dr. Stern, a neuropsychologist, and others set out to determine how people can develop cognitive reserve. They have learned thus far that there is no “quick fix” for the aging brain, and little evidence that any one supplement or program or piece of equipment can protect or enhance brain function — advertisements for products like ginkgo biloba to the contrary.
Nonetheless, well-designed studies suggest several ways to improve the brain’s viability. Though best to start early to build up cognitive reserve, there is evidence that this account can be replenished even late in life.
Cognitive reserve is greater in people who complete higher levels of education. The more intellectual challenges to the brain early in life, the more neurons and connections the brain is likely to develop and perhaps maintain into later years. Several studies of normal aging have found that higher levels of educational attainment were associated with slower cognitive and functional decline.
Dr. Scarmeas and Dr. Stern suggest that cognitive reserve probably reflects an interconnection between genetic intelligence and education, since more intelligent people are likely to complete higher levels of education.
But brain stimulation does not have to stop with the diploma. Better-educated people may go on to choose more intellectually demanding occupations and pursue brain-stimulating hobbies, resulting in a form of lifelong learning. In researching her book, Ms. Ramin said she found that novelty was crucial to providing stimulation for the aging brain.
“If you’re doing the same thing over and over again, without introducing new mental challenges, it won’t be beneficial,” she said in an interview. Thus, as with muscles, it’s “use it or lose it.” The brain requires continued stresses to maintain or enhance its strength.
So if you knit, challenge yourself with more than simply stitched scarves. Try a complicated pattern or garment. Listening to opera is lovely, but learning the libretto (available in most libraries) stimulates more neurons. In my 60s I took up knitting and crocheting and am now learning Spanish. My husband is a fanatical puzzle-doer who recently added Sudoku to the crosswords and double-crostics he carries around with him.
In 2001, Dr. Scarmeas published a long-term study of cognitively healthy elderly New Yorkers. On average, those who pursued the most leisure activities of an intellectual or social nature had a 38 percent lower risk of developing dementia. The more activities, the lower the risk.
Long-term studies in other countries, including Sweden and China, have also found that continued social interactions helped protect against dementia. The more extensive an older person’s social network, the better the brain is likely to work, the research suggests. Especially helpful are productive or mentally stimulating activities pursued with other people, like community gardening, taking classes, volunteering or participating in a play-reading group.
... and Physical
Perhaps the most direct route to a fit mind is through a fit body. As Sandra Aamodt, editor of Nature Neuroscience, and Sam Wang, a neuroscientist at Princeton University, recently stated on The New York Times’s Op-Ed page, physical exercise “improves what scientists call ‘executive function,’ the set of abilities that allows you to select behavior that’s appropriate to the situation, inhibit inappropriate behavior and focus on the job at hand in spite of distractions. Executive function includes basic functions like processing speed, response speed and working memory, the type used to remember a house number while walking from the car to a party.”
Although executive function typically declines with advancing years, “elderly people who have been athletic all their lives have much better executive function than sedentary people of the same age,” Dr. Aamodt and Dr. Wang reported.
And not just because cognitively healthy people tend to be more active. When inactive people in their 70s get more exercise, executive function improves, an analysis of 18 studies showed. Just walking fast for 30 to 60 minutes several times a week can help. And compared with those who are sedentary, people who exercise regularly in midlife are one-third as likely to develop Alzheimer’s in their 70s. Even those who start exercising in their 60s cut their risk of dementia in half.
Exercise may help by improving blood flow (and hence oxygen and nutrients) to the brain, reducing the risk of ministrokes and clogged blood vessels, and stimulating growth factors that promote the formation of new neurons and neuronal connections.
When Lapses Are Not Just Signs of Aging
By Jane E. Brody : NY Times : September 5, 2011
Who hasn’t struggled occasionally to come up with a desired word or the name of someone near and dear? I was still in my 40s when one day the first name of my stepmother of 30-odd years suddenly escaped me. I had to introduce her to a friend as “Mrs. Brody.”
But for millions of Americans with a neurological condition called mild cognitive impairment, lapses in word-finding and name recall are often common, along with other challenges like remembering appointments, difficulty paying bills or losing one’s train of thought in the middle of a conversation.
Though not as severe as full-blown Alzheimer’s disease or other forms of dementia, mild cognitive impairment is often a portent of these mind-robbing disorders. Dr. Barry Reisberg, professor of psychiatry at New York University School of Medicine, who in 1982 described the seven stages of Alzheimer’s disease, calls the milder disorder Stage 3, a condition of subtle deficits in cognitive function that nonetheless allow most people to live independently and participate in normal activities.
One of Dr. Reisberg’s patients is a typical example. In the two and a half years since her diagnosis of mild cognitive impairment at age 78, the woman learned to use the subway, piloted an airplane for the first time (with an instructor) and continued to enjoy vacations and family visits. But she also paid some of the same bills twice and spends hours shuffling papers.
Dr. Ronald C. Petersen, a neurologist at the Mayo Clinic College of Medicine in Rochester, Minn., described mild cognitive impairment as “an intermediate state of cognitive function,” somewhere between the changes seen normally as people age and the severe deficits associated with dementia.
While most people experience a gradual cognitive decline as they get older (only about one in 100 lives long without cognitive loss), others experience more extreme changes in cognitive function, the neurologist wrote in The New England Journal of Medicine in June. In population-based studies, mild cognitive impairment has been found in 10 percent to 20 percent of people older than 65, he noted.
Dr. Petersen described two “subtypes” of the condition, amnestic and nonamnestic, that have different trajectories. The more common amnestic type is associated with significant memoryproblems, and within 5 to 10 years usually — but not always — progresses to full-blown Alzheimer’s disease, he said in an interview.
“Subtle forgetfulness, such as misplacing objects and having difficulty recalling words, can plague persons as they age and probably represents normal aging,” he wrote. “The memory lossthat occurs in persons with amnestic mild cognitive impairment is more prominent. Typically, they start to forget important information that they previously would have remembered easily, such as appointments, telephone conversations or recent events that would normally interest them,” like the outcome of a ballgame would a sports fan.
The forgetfulness is often obvious to those who are affected and to people close to them, but not to casual observers.
The less common nonamnestic type, which is associated with difficulty making decisions, finding the right words, multitasking, visual-spatial tasks and navigating, can be a forerunner of other kinds of dementia, Dr. Petersen said.
In general, Dr. Reisberg said, “mild cognitive impairment lasts about seven years before it begins to interfere with the activities of daily life.”
The Correct Diagnosis
Distinguishing mild cognitive impairment from the effects of normal aging can be challenging. Typically, new patients take a short test of mental status, provide a thorough medical history and are checked for conditions that may be reversible causes of impaired cognition. Problems like depression, medication side effects, vitamin B12 deficiency or an underactive thyroid can mimic the symptoms of mild cognitive impairment.
Other tests, like an M.R.I. or CT scan of the brain, can look for evidence of a stroke, brain tumor or leaky blood vessel that may be impairing brain function.
It is natural, Dr. Petersen said, for patients and their families to want to know whether and how quickly the disorder might progress. While patients decline by about 10 percent each year, on average, certain factors are associated with more rapid progression. Among these are the presence of a gene called APOE e4, more common among patients with Alzheimer’s disease; a reduced hippocampus, a region of the brain important to memory; and a low metabolic rate in the temporal and parietal regions of the brain.
Amyloid plaques in the brain, while a hallmark of Alzheimer’s disease and a predictor of progression, have also been found at autopsy in people with perfectly normal cognitive function.
Preserving Cognitive Function
Despite a number of clinical trials that tested various medications, no drug to treat mild cognitive impairment has been approved by the Food and Drug Administration. But experts like Dr. Reisberg and Dr. Petersen suggest several approaches that may slow the decline in cognitive function.
Although studies did not show that medications like donepezil (brand name Aricept) and memantine (Namenda), both used to treat Alzheimer’s disease, do not change the ultimate course of mild cognitive impairment, Dr. Reisberg said they can be useful temporary treatments that may stabilize patients for a few years.
Although the drugs are not approved for this condition, licensed physicians can prescribe approved medications “off label.” “Clinicians have to work with what we have,” Dr. Reisberg said.
There are people who think they are having memory problems, but tests do not show anything definitive. Some may be in Stage 1 of Alzheimer’s disease, Dr. Reisberg said, and perhaps could benefit from early treatment with the drugs.
It is also important to reduce cardiovascular risk factors like smoking, elevated cholesterol and high blood pressure; keep blood sugar at normal levels; minimize stress (which in animal studies can cause the hippocampus to shrink); and avoid anticholinergic drugs that can interfere with brain chemicals important to memory. These include Demerol to treat pain, Detrol to treat a leaky bladder, tricyclic antidepressants, Valium, and over-the-counter medications with Benadryl (diphenhydramine), like Tylenol PM, Dr. Petersen said.
Some cognitive rehabilitation exercises, like computer games that enhance focus, may be helpful, Dr. Petersen said, but there have been few good studies to demonstrate a benefit. Compensatory techniques, like taking notes, creating mnemonics and making structured schedules, can be useful aids, he added.
But most promising is regular physical exercise, which in animal studies was found to reduce the accumulation of amyloid in the brain. An Australian study in patients with memory problems showed that brisk walking for 150 minutes a week improved cognitive function.
What's Good for the Heart Is Good for the Head
By Jane E. Brody : NY Times Article : March 22, 2005
For decades I've been pleading with my readers to adopt healthy habits to prevent heart disease and possibly some cancers. Now there's another organ, the brain, that these measures may protect.
Growing, scientifically sound evidence suggests that people can delay and perhaps even prevent Alzheimer's disease by taking steps like eating low-fat diets rich in antioxidants, maintaining normal weight, exercising regularly and avoiding bad habits like smoking and excessive drinking.
Several other practices - including remaining socially connected and keeping the brain stimulated by reading, doing puzzles and learning new things - also appear to protect the brain against dementia.
Achieving such protection is no minor matter. Nearly half of the people who live past 85 develop this devastating disease that ultimately divorces them from reality and those who love them. With 77 million baby boomers headed toward advanced age, much can be gained from postponing this most common form of dementia, if not preventing it entirely.
An estimated 4.5 million Americans now have Alzheimer's, and the number has doubled since 1980, as more people reach older and older ages. Alzheimer's already costs Medicare three times as much as any other disease. By 2010, Medicare costs for people with Alzheimer's are expected to rise by more than 50 percent, to $49.3 billion from $31.9 billion in 2000. Now, half of all nursing home costs are related to dementia.
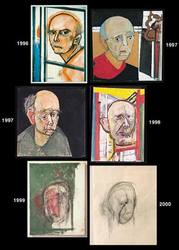
Alzheimer's is a progressive brain disorder that gradually destroys a person's memory and ability to learn, reason, make judgments, communicate and carry out normal activities of daily life.
Two changes in the brain are characteristic: abnormal microscopic structures called amyloid plaques that accumulate outside brain cells and tangles of a protein called tau that form inside brain cells. Because these changes are now seen only in autopsies, coming up with early diagnoses and tests for the disorder is a major challenge.
Early signs may include forgetting recently learned information, performing familiar tasks only with difficulty, misplacing things (putting shoes in the refrigerator, for example), fumbling for the right word for an ordinary object (like a toothbrush) and forgetting where you are or how you got there. Personalities can also change, and patients can become paranoid, suspicious, fearful or extremely confused. Some lose their judgment and suffer from mood swings or loss of initiative.
Built for Durability
The brain is a very forgiving organ. It has a very large reserve capacity and can withstand an extraordinary number of "hits" and bounce back from them. Witness how well some people recover from serious strokes and brain trauma. Likewise, autopsies often reveal considerable brain changes associated with Alzheimer's disease among subjects who showed no symptoms of dementia during their lives.
But when the brain is otherwise compromised, it may not be as able to protect itself against the encroaching damage of Alzheimer's.
So how do measures to prevent heart disease and stroke protect the brain? In an interview, Dr. Laurel Coleman, a geriatric physician in Augusta, Me., and a member of the national board of the Alzheimer's Association, explained that increasing evidence suggested an overlap between vascular disease in the brain and what happens to the brain in people who develop Alzheimer's.
The presence of vascular disease - the kind that can lead to a heart attack or stroke - seems to decrease the brain's ability to fend off the effects of Alzheimer's-related damage and increase a person's chances of showing obvious signs of dementia.
"Some people," Dr. Coleman said, "have pure Alzheimer's disease and some have pure cerebral vascular disease. But most have a mix of the two." The same risk factors that raise a person's chances of having a heart attack or stroke - high cholesterol and blood pressure, excess weight, smoking, lack of exercise - also raise the risk of developing dementia, she explained.
It's not that circulatory disease causes Alzheimer's, she emphasized. But if the brain lacks a healthy flow of blood through vessels relatively free of atherosclerotic plaques, it is less able to fight off the damage associated with dementia.
Likewise, Dr. Coleman acknowledges that genetic factors may raise a person's risk of Alzheimer's. Taking steps to reduce the risk incurred through genes, though, makes good sense. And that is achieved by controlling known risks for vascular disease.
Some large long-term observational studies, including the Nurses' Health Study and the Honolulu-Asia Aging Study, support the link between risk factors for vascular disease and Alzheimer's. For example, an increased risk of Alzheimer's or an accelerated decline in mental functioning was noted in Japanese-American men with untreated high blood pressure, in American nurses and Dutch study participants with Type 2 diabetes (a result of excess weight), in Finns with high cholesterol and high intakes of saturated fats, and in Europeans who smoked.
A study lasting for decades at the Karolinska Institute in Stockholm found a sixfold increase in the risk of Alzheimer's in people who were obese and had high blood pressure and high cholesterol.
But the most telling evidence comes from an order of nuns, nearly 700 School Sisters of Notre Dame studied over many years by Dr. David Snowdon. All the nuns in the order by and large have similar eating and exercise habits, and all agreed to allow their brains to be autopsied.
These autopsies confirmed what had been suspected from observational studies: a striking relationship between the presence in the brain of cerebral vascular disease and symptoms caused by damage related to Alzheimer's disease.
The sisters with brain abnormalities characteristic of Alzheimer's were more likely to have shown symptoms of dementia if they also had strokes or clogged brain arteries.
Recipe for Success
In addition to controlling weight and fat intake, consuming foods or supplements rich in omega-3 fatty acids, like fatty fish or supplements of DHA, appears to protect against brain deterioration. Likewise, regular exercise - like walking more than two miles a day - seems to delay the degeneration of nerve cells in the brain.
How you spend your leisure time may also make an important difference. Activities that involve mental and social stimulation, like doing crossword puzzles; playing bridge, checkers or chess; learning a language or new skill; taking up knitting or crocheting; and remaining socially involved have all been associated in various studies with preservation of normal brain function.
When these activities are combined with regular physical activity, the benefit appears to be even greater.
To spread information about such steps, the Alzheimer's Association is conducting "Maintain Your Brain" workshops across the country. Listings are at www.alz.org.
Mice and other rodents have been shown throughout their lives to be able to form new cells in the part of the brain involved in learning and memory if they live in an "enriched" environment.
Can you be any less well developed than a mouse?
Taking On Alzheimer’s
By Stephanie Saul : NY Times Article : June 10, 2007
In the book “Mrs. Frisby and the Rats of NIMH,” a group of lab rats acquire human intelligence through a genetic experiment. Every child recognizes the charming tale as pure fantasy, yet something similar is occurring at a major pharmaceuticals company, Wyeth, where rodents tested in its labs have, indeed, taken on some features of the human brain.
Unlike the fictional rats that learned to read, write and operate machinery, Wyeth’s animals are slow-witted, confused and forgetful because they suffer from the crippling dementia of Alzheimer’s disease, which they acquired from a transplanted human gene.
Something else extraordinary is going on at Wyeth. The company’s scientists not only can give rodents Alzheimer’s — they have also figured out how to take it away. Curing mice is a lot simpler than curing people, but the results are a tantalizing development that offers hope to humans suffering from the disease. The work also advances what Wyeth executives describe as their war on Alzheimer’s.
Wyeth’s team faces a formidable foe. In an industry often criticized as making pricey “me too” drugs that involve minor tweaks to competitors’ products, as well as promoting medicines of marginal value, Wyeth has decided to go full bore against Alzheimer’s, a disease that has defied effective treatment since it was first identified a century ago. The company has dedicated more than 350 scientists exclusively to Alzheimer’s research, and they are working on 23 separate projects for medicines to possibly treat the disease.
About five million people in the United States are living with Alzheimer’s, according to the Alzheimer’s Association, an advocacy group funded by individual donors as well as foundations and major corporations, including drug makers. Without a cure or new treatments, the number of those with the disease could grow to 13.2 million by 2050, the National Institute on Aging estimates.
“I think this is going to be the disease, and maybe one of the biggest health care political issues of my generation,” says Robert Essner, 59, Wyeth’s professorial chief executive. “It’s hard for anyone to envision how to provide health care in the United States if you’re going to have to deal with the burden. You just start to add up the cost, 20 years from now as my generation gets old — it’s phenomenal.”
Mr. Essner will have more than a host of grateful baby boomers awaiting him if Wyeth’s crusade is successful. The company could snare a big financial payoff from what still amounts to a risky bet, one that has already cost Wyeth about $450 million in research funds. But with a treatment that slows progress of the disease possibly selling at more than $20,000 a year, the company’s Alzheimer’s program is one reason that some analysts are voicing renewed enthusiasm about Wyeth’s stock, which had been weighed down for years by costly fen-phen diet drug litigation.
Wyeth is hardly the only company looking for Alzheimer’s treatments. Virtually every large drug maker and a number of smaller biotechnology companies are working to develop Alzheimer’s drugs, with several hundred ideas under study. Several companies are expected to announce results of clinical studies during an international Alzheimer’s meeting that is under way in Washington. “There seems to be a current of excitement,” said Peter Davies, a biochemist at the Albert Einstein College of Medicine in the Bronx, who has studied Alzheimer’s for 30 years. Dr. Davies is working with Eli Lilly and Applied NeuroSolutions on a possible course of treatment that is such a secret that he will not say anything about it. “I wouldn’t say it’s a race,” Dr. Davies said, “but this is novel and we want to get a jump on therapeutics.”
The four Alzheimer’s treatments now on the market work by regulating the action of chemical neurotransmitters in the brain. The drugs — Aricept by Eisai and Pfizer, Exelon by Novartis, Razadyne by Johnson & Johnson and Namenda by Forest Laboratories — have shown mixed results treating Alzheimer’s symptoms and do nothing to stop the disease’s progress.
Dr. Todd Golde, professor of neuroscience at the Mayo Clinic, says that the drugs are not very effective, and that consumers’ large expenditures for them — about $1.4 billion in the United States alone last year, according to data from Verispan — reflect the desperation of patients and their families to treat the disease.
“It’s scary if you look at the trials that got these drugs approved,” Dr. Golde said. “The change in mental status was so small, the average caregiver of a patient would have no way of knowing there was any difference.” While there is no evidence that any of the drugs stem the underlying disease, they were approved based on studies showing temporary improvement or stabilization in some patients with Alzheimer’s. The changes can be as minor as a better ability to dress oneself or to take out the trash.
In one study of people taking Namenda and Aricept combined for six months, 60 percent of patients either improved or did not deteriorate. “I would say that physicians do believe these drugs are of benefit to patients with Alzheimer’s,” said Stephen M. Graham, senior director of clinical development at Forest.
Spokesmen for the other companies with Alzheimer’s drugs echoed that assessment in regard to their products, pointing to clinical studies demonstrating that they help patients.
Wyeth is wagering that it can find more promising treatments for a nebulous, stealthy disease that does more than rob people of their health and well-being. It also steals some of their most precious memories.
AT first blush, Robert Essner seems an unlikely flag bearer for a corporate assault on Alzheimer’s. The son of a college professor, Mr. Essner studied humanities as an undergraduate and in graduate school, intending to teach college history. But after he graduated from the University of Chicago in 1971 with a master’s degree in history, he soon realized that jobs in his field were scarce. He says he stumbled into pharmaceuticals by answering an ad in The Wall Street Journal.
Today, he is on the leading edge of a generation that is facing a huge emotional and financial burden from a disease that leaves victims requiring full-time nursing care. He is urging a national mobilization against what he describes as a looming Alzheimer’s “epidemic.”
Mr. Essner often speaks publicly about the disease, stepping outside his role as corporate chief and into the public policy arena. Last month, he testified at a Senate hearing, recommending that the NationalInstitutes of Health double its current annual funding of $643 million for Alzheimer’s research.
Seated recently at a conference table at the company’s headquarters on pastoral property near Madison, N.J., Mr. Essner said he has taken to the podium because he thinks Alzheimer’s should garner the same attention that AIDS received during the 1980s and 1990s, when a coalition of government and industry worked feverishly to find treatments.
He says he is concerned as much about the disease’s dehumanizing effects as he is about its costs. “You see mothers who don’t recognize their daughters,” he says.
Mr. Essner also speaks from experience. While he requested that details be kept private, he confides that a relative has been caught in the disease’s maw. In fact, Mr. Essner is just one of several senior managers involved in the Alzheimer’s drug discovery program at Wyeth whose families have been affected by the disease.
Among the others is Menelas Pangalos, the company’s vice president for neuroscience research and a biochemist. He remembers visiting his grandmother in Greece while she was in the throes of the disease. While people may expect the elderly to lose their memories, Dr. Pangalos says that this is a false assumption that has gained traction only because Alzhiemer’s is so prevalent.
“The problem is that it’s so common,” he said in an interview at Wyeth’s research laboratory near Princeton, N.J., where much of its Alzheimer’s work is conducted. “You assume it’s normal and it’s natural, but it’s not.”
MR. Essner understands history well enough to recognize that big scientific breakthroughs generally accrue to those willing to take a chance. With the high failure rates in drug development, it is unlikely that any single compound now under study will make it to the market. But Mr. Essner says he believes that with so many drugs under study, at least one is likely to succeed.
Wyeth announced last month that it was moving early into advanced human trials of one experimental treatment, a biological product that many scientists view as the most promising new product under study for Alzheimer’s. Wyeth made a presentation about its Alzheimer’s work the centerpiece of the company’s annual shareholders meeting in April, as well as its annual report, which included the stories of seven Alzheimer’s sufferers.
Among those chronicled in the Wyeth accounts was Gilbert Brown, 80, a retired auto parts salesman for Sears in New Jersey. His son, Michael S. Brown, noticed changes in his father several years ago.
“We would talk on the telephone several times a week and he would sometimes say things that didn’t make sense,” said the younger Mr. Brown, who runs a state-funded program that assists low-income students at Montclair State University in Montclair, N.J. At one point, in a subtle but sure sign that something was amiss, Mr. Brown told his son in 2004 that he had lost his checkbook and insisted that he was going to Kmart for a new one.
About three years ago, his father’s gradual decline prompted the younger Mr. Brown, 59, to move him into his home in Irvington, N.J. Today, the elder Mr. Brown can no longer carry on a conversation, dress himself or shave. In fact, he cannot remember the word for shaving. Yet the elder Mr. Brown can still play church hymns on the organ, remembering old favorites like “Rock of Ages” and others that he regularly performs at a senior program. But his son struggles each morning to help his father shower and dress.
“It really hurts,” the younger Mr. Brown says. “He is a very intelligent man. He was the kind of person that his family, my mom’s family, would depend upon to do anything, conduct any business. Then to go from that to not being able to do anything.”
Mr. Brown took Aricept, one of the four Alzheimer’s drugs currently available, until his insurance company said his disease had progressed too far and he was no longer eligible.
“You don’t know what the progression of the deterioration is, so it’s hard to tell if the medicine is helping or not,” Michael Brown says.
A paucity of effective Alzheimer’s treatments reflects how difficult it remains for scientists, doctors and other medical researchers to understand and combat brain disease. Alzheimer’s research began about a century ago, when the Bavarian psychiatrist Alois Alzheimer first diagnosed a 51-year-old patient suffering from dementia, delirium and hallucinations.
The patient, whom Dr. Alzheimer called Auguste D., entered the Frankfurt asylum in 1901. The doctor’s notes on her condition reveal that she was unable to answer simple questions. “At lunch, she eats cauliflower and pork,” the notes say. “Asked what she is eating, she answers, ‘spinach.’ ” Mrs. D. complained to her doctor: “I have lost myself.”
Mrs. D. died five years later, and an autopsy revealed abnormalities in her brain, including the presence of sticky plaque and tangled fibers in nerves. The condition that Dr. Alzheimer described in Mrs. D. was later named after him. While the exact cause of the disease is still unknown, researchers believe that genetic factors play a role and that heavy plaque deposits like those Dr. Alzheimer discovered in Mrs. D.’s brain may contribute to tissue deterioration — leading to memory and recognition loss, linguistic problems and degraded motor skills. But scientists continue to debate whether plaque is a symptom or a cause of Alzheimer’s.
With more and more people living into their 80s and 90s, Alzheimer’s is more common today than it was 100 years ago. Estimates of its frequency vary, but it strikes one out of every 5 people between ages 75 and 84 and 42 percent of those over age 85, according to the Alzheimer’s Association. The organization estimates the current direct and indirect costs of the disease at nearly $150 billion a year, a figure that includes medical and nursing home costs as well as lost job productivity for family members who serve as caregivers. Two drug companies that have progressed to late-stage tests of Alzheimer’s treatments are Neurochem and Myriad Genetics. Neurochem says it may disclose results of its late-stage trial this month. Its drug, Alzhemed, aims at the plaque.
Myriad Genetics’ product, Flurizan, is similar to an anti-inflammatory drug, and it may lower the production of the protein found in plaque. Dr. Golde of the Mayo Clinic was involved in developing the compound.
The National Institutes of Health, the primary federal agency that oversees and helps fund biomedical research, is currently supporting 22 studies involving Alzheimer’s.
John Hardy, a neurogeneticist at the National Institute on Aging, a branch of the National Institutes of Health, says some of the ideas under study as Alzheimer’s treatments have little chance of success. “There’s some pretty wacky things that people try because we’re desperate,” he says.
Dr. Hardy helped to develop a leading theory, known as the “amyloid cascade,” about the biological process that results in Alzheimer’s. The hypothesis holds that Alzheimer’s brain plaque, which contains a protein called beta amyloid, causes symptoms of the disease. According to the theory, plaque develops when something goes awry in the breakdown of a substance called an amyloid precursor protein, or A.P.P.
Scientists came to believe that A.P.P. had something to do with Alzheimer’s by analyzing the genes of Alzheimer’s patients. They also discovered that people with Down syndrome — a group that commonly develops Alzheimer’s-like symptoms — are born with extra A.P.P. And mutations in A.P.P. genes are among the genetic abnormalities found in families with a hereditary form of early-onset Alzheimer’s.
A.P.P. exists in many human cells. It is normally broken down in the body without incident. But scientists believe that in Alzheimer’s patients, enzymes interfere with the breakdown, causing A.P.P. to glob together and form the sticky, toxic beta-amyloid plaque that interferes with activities in the brain.
Among the many companies going after Alzheimer’s, Wyeth is regarded as a leader. Wyeth’s biggest Alzheimer’s bet, in partnership with Elan Pharmaceuticals, involves biological products that would actually slow or reverse the progress of the disease by attacking beta-amyloid. While most researchers believe that the accumulation of beta-amyloid in the brain is the instigating factor of Alzheimer’s, that theory is not without its critics.
Dr. Davies of Einstein, who also directs an Alzheimer’s research center at North Shore-Long Island Jewish Health System, says he believes that plaque is a symptom of the disease rather than a cause. He questions whether eliminating plaque will help those with Alzheimer’s. “It’s like trying to clear up scar tissue and expecting things to get better,” he says.
He subscribes to an alternative theory that focuses on tau, a protein found in the tangled nerve fibers in the brain of Alzheimer’s patients, as the real culprit. His interests also frame a larger divide in the Alzheimer’s world. Those who embrace the beta-amyloid protein theory are nicknamed “Baptists.” Those who finger tau as the villain are called “Tauists.” The two sides recently have moved closer together, more willing to say that beta-amyloid and tau may be working together in Alzheimer’s.
If the two camps continue to merge, it may mean that in the long run Alzheimer’s patients will be treated with more than one drug, the way multipronged treatment regimens are used for cardiovascular problems.
Wyeth itself is keeping a research foot in both treatment camps, on the theory that it is better not to place all its bets on one disease pathway. It is working on compounds aiming at tau, as well as brain enzymes that have been implicated in Alzheimer’s. Its partnership with Elan began in 2000, when several key Wyeth scientists came to Mr. Essner, describing Elan’s work and asking him to sign off on a partnership.
“I asked, ‘What’s the probability of success?’ ” Mr. Essner recalls, laughing. “The first guy said 30 percent. I said: ‘Really? 30 percent, that’s very high.’ He said, ‘Well maybe 10 percent,’ then finally, ‘I have no idea.’ ”
But Mr. Essner says that it was hard to apply a financial calculus to such an undertaking. “I really came away with the impression that their passion for this was so great, that if I had said no, I would have had a mutiny,” he says.
In a development that illustrates the vicissitudes of drug development, the Wyeth-Elan partnership suffered a major setback in 2002, when the first human trial of an Alzheimer’s vaccine, called AN-1792, had to be halted. About 18 patients, or 6 percent of those enrolled, suffered inflammation in their brains. It was an apparent reaction to the vaccine, which used a strand of human protein to prompt an immune response.
Despite the severe reactions of some patients, others in the interrupted trial may have responded positively to the vaccine, according to Wyeth’s follow-up examinations. The symptoms of some patients who fared well in the trial appeared to have stabilized, a contrast to the inexorable decline usually experienced in Alzheimer’s. Autopsies of five trial participants who later died of natural causes revealed evidence of plaque-clearing in their brains.
The results supported the idea that Alzheimer’s plaque can be attacked with immunotherapy. “It looked like the vaccine was doing the same thing we’ve seen in the animals,” Dr. Pangalos says.
After the failure of AN-1792, Wyeth and Elan worked to develop a safer vaccine and also focused on another form of immunotherapy: passive immunization.
Instead of vaccinating patients with a strand of amyloid protein and letting them form their own antibodies, passive immunization injects pre-made antibodies directly into patients. In theory, the antibodies then attach themselves to harmful plaque and dissolve it. Wyeth would deliver its antibody product, bapineuzumab, to patients through infusion, in a process much like chemotherapy for cancer patients.
In a joint announcement last month, Wyeth and Elan said a late-stage trial of the drug would begin in the second half of this year. Although history shows that the odds are against the success of any individual drug, the progress is an encouraging sign for a drug that many scientists regard as the most promising treatment in development for Alzheimer’s.
“It’s going to be the first test of what we call the amyloid hypothesis of Alzheimer’s,” says David Morgan, an Alzheimer’s researcher at the University of South Florida. “Elan and Wyeth clearly are in the lead in developing immunotherapy.”
AT Wyeth’s research lab near Princeton, scientists have tested bapineuzumab and other compounds on genetically altered mice, using a special swimming pool equipped with an invisible platform.
When a mouse is placed in the pool, it instinctively begins swimming around to find a resting place. Once a normal mouse finds the platform the first time, it can find its way back on follow-up swims. But the genetically altered mice become lost.
“The Alzheimer’s mouse cannot remember the location of the platform,” says Reka Hosszu, a research scientist at Wyeth who works with the animals. She says that an Alzheimer’s mouse will paddle aimlessly in the pool.
After treatment, the Alzheimer’s mice can find the platform more easily. And their brains look better. In before-and-after images, it is clear that globs of toxic plaque have cleared. “You can get rid of pretty much all of the amyloid,” says Dr. Pangalos as he displays a three-dimensional image of a mouse brain on his computer. “And you can reverse their memory to normal, like a young mouse.”
If all goes according to Wyeth’s plan, it should work in humans, too. “We’re going after this,” Dr. Pangalos says, “and we’re not stopping until we’ve nailed it.”
Zen and the Art of Coping With Alzheimer’s
By Denise Grady : NY Times Article : August 14, 2007
During the YouTube forum with the Democratic presidential candidates in July, the first question about health care came from two middle-age brothers in Iowa, who faced the camera with their elderly mother. Not everybody with Alzheimer’s disease has two loving sons to take care of them, they said, adding that a boom in dementia is expected in the next few decades.
“What are you prepared to do to fight this disease now?” they asked.
The politicians mouthed generalities about health care, larded with poignant anecdotes. None of them answered the question about Alzheimer’s.
Science hasn’t done much better. There is no cure for Alzheimer’s and no way to prevent it. Scientists haven’t even stopped arguing about whether the gunk that builds up in the Alzheimer’s brain is a cause or an effect of the disease. Alzheimer’s is roaring down — a train wreck to come — on societies all over the world.
People in this country spend more than a $1 billion a year on prescription drugs marketed to treat it, but for most patients the pills have only marginal effects, if any, on symptoms and do nothing to stop the underlying disease process that eats away at the brain. Pressed for answers, most researchers say no breakthrough is around the corner, and it could easily be a decade or more before anything comes along that makes a real difference for patients.
Meanwhile, the numbers are staggering: 4.5 million people in the United States have Alzheimer’s, 1 in 10 over 65 and nearly half of those over 85. Taking care of them costs $100 billion a year, and the number of patients is expected to reach 11 million to 16 million by 2050. Experts say the disease will swamp the health system.
It’s already swamping millions of families, who suffer the anguish of seeing a loved one’s mind and personality disintegrate, and who struggle with caregiving and try to postpone the wrenching decision about whether they can keep the patient at home as helplessness increases, incontinence sets in and things are only going to get worse.
Drug companies are placing big bets on Alzheimer’s. Wyeth, for instance, has 23 separate projects aimed at developing new treatments. Hundreds of theories are under study at other companies large and small. Why not? People with Alzheimer’s and their families are so desperate that they will buy any drug that offers even a shred of hope, and many will keep using the drug even if the symptoms don’t get better, because they can easily be convinced that the patient would be even worse off without it.
It is telling, maybe a tacit admission of defeat, that a caregiving industry has sprung up around Alzheimer’s. Books, conferences and Web sites abound — how to deal with the anger, the wandering, the sleeping all day and staying up all night, the person who asks the same question 15 times in 15 minutes, wants to wear the same blouse every day and no longer recognizes her own children or knows what a toilet is for.
The advice is painfully and ironically reminiscent of the 1960s and ’70s, the literal and figurative high point for many of the people who are now coping with demented parents. The theme is, essentially, go with the flow. People with Alzheimer’s aren’t being stubborn or nasty on purpose; they can’t help it. Arguing and correcting will not only not help, but they will ratchet up the hostility level and make things worse. The person with dementia has been transported into a strange, confusing new world and the best other people can do is to try to imagine the view from there and get with the program.
If a patient asks for her mother, for instance, instead of pointing out that her mother has been dead for 40 years, it is better to say something like, “I wish your mother were here, too,” and then maybe redirect the conversation to something else, like what’s for lunch.
If Dad wants to polish off the duck sauce in a Chinese restaurant like it’s a bowl of soup, why not? If Grandma wants to help out by washing the dishes but makes a mess of it, leave her to it and just rewash them later when she’s not looking. Pull out old family pictures to give the patient something to talk about. Learn the art of fragmented, irrational conversation and follow the patient’s lead instead of trying to control the dialogue.
Basically, just tango on. And hope somebody will do the same for you when your time comes. Unless the big breakthrough happens first.
Alzheimer's Disease Overview
Alzheimer's disease (AD), one form of dementia, is a progressive, degenerative brain disease. It affects memory, thinking, and behavior.
Memory impairment is a necessary feature for the diagnosis of this or any type of dementia. Change in one of the following areas must also be present: language, decision-making ability, judgment, attention, and other areas of mental function and personality.
The rate of progression is different for each person. If AD develops rapidly, it is likely to continue to progress rapidly. If it has been slow to progress, it will likely continue on a slow course.
Alternative Names Senile dementia/Alzheimer's type (SDAT)
Causes » More than 4 million Americans currently have AD. The older you get, the greater your risk of developing AD, although it is not a part of normal aging. Family history is another common risk factor.
In addition to age and family history, risk factors for AD may include:
- Longstanding high blood pressure
- History of head trauma
- High levels of homocysteine (a body chemical that contributes to chronic illnesses such as heart disease, depression, and possibly AD)
- Female gender -- because women usually live longer than men, they are more likely to develop AD
The cause of AD is not entirely known but is thought to include both genetic and environmental factors. A diagnosis of AD is made based on characteristic symptoms and by excluding other causes of dementia.
Prior theories regarding the accumulation of aluminum, lead, mercury, and other substances in the brain leading to AD have been disproved. The only way to know for certain that someone had AD is by microscopic examination of a sample of brain tissue after death.
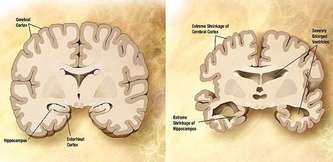
The brain tissue shows "neurofibrillary tangles" (twisted fragments of protein within nerve cells that clog up the cell), "neuritic plaques" (abnormal clusters of dead and dying nerve cells, other brain cells, and protein), and "senile plaques" (areas where products of dying nerve cells have accumulated around protein). Although these changes occur to some extent in all brains with age, there are many more of them in the brains of people with AD.
The destruction of nerve cells (neurons) leads to a decrease in neurotransmitters (substances secreted by a neuron to send a message to another neuron). The correct balance of neurotransmitters is critical to the brain.
By causing both structural and chemical problems in the brain, AD appears to disconnect areas of the brain that normally work together.
About 10 percent of all people over 70 have significant memory problems and about half of those are due to AD. The number of people with AD doubles each decade past age 70. Having a close blood relative who developed AD increases your risk.
Early onset disease can run in families and involves autosomal dominant, inherited mutations that may be the cause of the disease. So far, three early onset genes have been identified.
Late onset AD, the most common form of the disease, develops in people 60 and older and is thought to be less likely to occur in families. Late onset AD may run in some families, but the role of genes is less direct and definitive. These genes may not cause the problem itself, but simply increase the likelihood of formation of plaques and tangles or other AD-related pathologies in the brain.
In-Depth Causes »
In the early stages, the symptoms of AD may be subtle and resemble signs that people mistakenly attribute to "natural aging." Symptoms often include:
- Repeating statements
- Misplacing items
- Having trouble finding names for familiar objects
- Getting lost on familiar routes
- Personality changes
- Losing interest in things previously enjoyed
- Difficulty performing tasks that take some thought, but used to come easily, like balancing a checkbook, playing complex games (such as bridge), and learning new information or routines
- Forgetting details about current events
- Forgetting events in your own life history, losing awareness of who you are
- Problems choosing proper clothing
- Hallucinations, arguments, striking out, and violent behavior
- Delusions, depression, agitation
- Difficulty performing basic tasks like preparing meals and driving
- Understand language
- Recognize family members
- Perform basic activities of daily living such as eating, dressing, and bathing
The first step in diagnosing Alzheimer's disease is to establish that dementia is present. Then, the type of dementia should be clarified. A health care provider will take a history, do a physical exam (including a neurological exam), and perform a mental status examination.
Tests may be ordered to help determine if there is a treatable condition that could be causing dementia or contributing to the confusion of AD. These conditions include thyroid disease, vitamin deficiency, brain tumor, drug and medication intoxication, chronic infection, anemia, and severe depression.
AD usually has a characteristic pattern of symptoms and can be diagnosed by history and physical exam by an experienced clinician. Tests that are often done to evaluate or exclude other causes of dementia include computed tomography (CT), magnetic resonance imaging (MRI), and blood tests.
In the early stages of dementia, brain image scans may be normal. In later stages, an MRI may show a decrease in the size of the cortex of the brain or of the area of the brain responsible for memory (the hippocampus). While the scans do not confirm the diagnosis of AD, they do exclude other causes of dementia (such as stroke and tumor).
In-Depth Diagnosis »
Treatment
Unfortunately, there is no cure for AD. The goals in treating AD are to:
- Slow the progression of the disease.
- Manage behavior problems, confusion, and agitation.
- Modify the home environment.
- Support family members and other caregivers.
LIFESTYLE CHANGES
The following steps can help people with AD:
- Walk regularly with a caregiver or other reliable companion. This can improve communication skills and prevent wandering.
- Use bright light therapy to reduce insomnia and wandering.
- Listen to calming music. This may reduce wandering and restlessness, boost brain chemicals, ease anxiety, enhance sleep, and improve behavior.
- Get a pet dog.
- Practice relaxation techniques.
- Receive regular massages. This is relaxing and provides social interactions.
Several drugs are available to try to slow the progression of AD and possibly improve the person's mental capabilities. Memantine (Namenda) is currently the only drug approved for the treatment of moderate-to-severe Alzheimer’s disease.
Other medicines include donepezil (Aricept), rivastigmine (Exelon), galantamine (Razadyne, formerly called Reminyl), and tacrine (Cognex). These drugs affect the level of a neurotransmitter in the brain called acetylcholine. They may cause nausea and vomiting. Tacrine also causes an elevation in liver enzymes and must be taken four times a day. It is now rarely used.
Aricept is taken once a day and may stabilize or even improve the person's mental capabilities. It is generally well tolerated. Exelon seems to work in a similar way. It is taken twice a day.
Other medicines may be needed to control aggressive, agitated, or dangerous behaviors. These are usually given in very low doses.
It may be necessary to stop any medications that make confusion worse. Such medicines may include pain killers, cimetidine, central nervous system depressants, antihistamines, sleeping pills, and others. Never change or stop taking any medicines without first talking to your doctor.
SUPPLEMENTS
Folate (vitamin B9) is critical to the health of the nervous system. Together with some other B vitamins, folate is also responsible for clearing homocysteine (a body chemical that contributes to chronic illnesses) from the blood. High levels of homocysteine and low levels of both folate and vitamin B12 have been found in people with AD. Although the benefits of taking these B vitamins for AD is not entirely clear, it may be worth considering them, particularly if your homocysteine levels are high.
Antioxidant supplements, like ginkgo biloba and vitamin E, scavenge free radicals. These products of metabolism are highly reactive and can damage cells throughout the body.
Vitamin E dissolves in fat, readily enters the brain, and may slow down cell damage. In at least one well-designed study of people with AD who were followed for 2 years, those who took vitamin E supplements had improved symptoms compared to those who took a placebo pill. Patients who take blood-thinning medications like warfarin (Coumadin) may should talk to their doctor before taking vitamin E.
Ginkgo biloba is an herb widely used in Europe for treating dementia. It improves blood flow in the brain and contains flavonoids (plant substances) that act as antioxidants. Although many of the studies to date have been somewhat flawed, the idea that ginkgo may improve thinking, learning, and memory in those with AD has been promising. DO NOT use ginkgo if you take blood-thinning medications like warfarin (Coumadin) or a class of antidepressants called monoamine oxidase inhibitors (MAOIs).
If you are considering any drugs or supplements, you MUST talk to your doctor first. Remember that herbs and supplements available over the counter are NOT regulated by the FDA.
SUPPORT AT HOME
Someone with AD will need support in the home as the disease worsens. Family members or other caregivers can help by trying to understand how the person with AD perceives his or her world. Simplify the patient's surroundings. Give frequent reminders, notes, lists of routine tasks, or directions for daily activities. Give the person with AD a chance to talk about their challenges and participate in their own care.
OTHER PRACTICAL STEPS
The person with AD should have their eyes and ears checked. If problems are found, hearing aids, glasses, or cataract surgery may be needed.
Those with AD may have particular dietary requirements such as:
- Extra calories due to increased physical activity from restlessness and wandering.
- Supervised meals and help with feeding. People with AD often forget to eat and drink, and can become dehydrated as a result.
Eventually, 24-hour monitoring and assistance may be necessary to provide a safe environment, control aggressive or agitated behavior, and meet physiologic needs. This may include in-home care, nursing homes, or adult day care.
Support Groups For additional information and resources for people with Alzheimer's disease and their caregivers, see Alzheimer's disease support groups.
Expectations (prognosis) The probable outcome is poor. The disorder is usually progresses steadily. Total disability is common. Death normally occurs within 15 years, usually from an infection or a failure of other body systems.
Complications
- Loss of ability to function or care for self
- Bedsores, muscle contractures (loss of ability to move joints because of loss of muscle function), infection (particularly urinary tract infections and pneumonia), and other complications related to immobility during end-stages of AD
- Falls and broken bones
- Loss of ability to interact
- Malnutrition and dehydration
- Failure of body systems
- Reduced life span
- Harmful or violent behavior toward self or others
- Abuse by an over-stressed caregiver
- Side effects of medications
Call your health care provider if a person with this disorder experiences a sudden change in mental status. (A rapid change may indicate other illness.)
Discuss the situation with your health care provider if you are caring for a person with this disorder and the condition deteriorates to the point where you can no longer care for the person in your home.
Prevention » Although there is no proven way to prevent AD, there are some practices that may be worth incorporating into your daily routine, particularly if you have a family history of dementia. Talk to your doctor about any of these approaches, especially those that involve taking a medication or supplement.
- Consume a low-fat diet.
- Eat cold-water fish (like tuna, salmon, and mackerel) rich in omega-3 fatty acids, at least 2 to 3 times per week.
- Reduce your intake of linoleic acid found in margarine, butter, and dairy products.
- Increase antioxidants like carotenoids, vitamin E, and vitamin C by eating plenty of darkly colored fruits and vegetables.
- Maintain a normal blood pressure.
- Stay mentally and socially active throughout your life.
- Consider taking non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin), sulindac (Clinoril), or indomethacin (Indocin). Statin drugs, a class of medications normally used for high cholesterol, may help lower your risk of AD. Talk to your doctor about the pros and cons of using these medications for prevention.
In-Depth Prevention »
References » Rakel P. Conn’s Current Therapy 2005. 57th ed. Philadelphia, Pa: Saunders; 2005.
Moore DP, Jefferson JW. Handbook of Medical Psychiatry. 2nd ed. St. Louis, Mo: Mosby; 2004.
Goetz CG, Pappert EJ. Textbook of Clinical Neurology. 2nd ed. Philadelphia, Pa: Saunders; 2003.
See All References »
Review Date: 5/16/2006
Reviewed By: Daniel Kantor, M.D., Director of the Comprehensive MS Center, Neuroscience Institute, University of Florida Health Science Center, Jacksonville, FL. Review provided by VeriMed Healthcare Network.
Doctors Say Medication Is Overused in Dementia
By Laurie Tarkan : NY Times Article : June 24, 2008
Ramona Lamascola thought she was losing her 88-year-old mother to dementia. Instead, she was losing her to overmedication.
Last fall her mother, Theresa Lamascola, of the Bronx, suffering from anxiety and confusion, was put on the antipsychotic drug Risperdal. When she had trouble walking, her daughter took her to another doctor — the younger Ms. Lamascola’s own physician — who found that she had unrecognized hypothyroidism, a disorder that can contribute to dementia.
Theresa Lamascola was moved to a nursing home to get these problems under control. But things only got worse. “My mother was screaming and out of it, drooling on herself and twitching,” said Ms. Lamascola, a pediatric nurse. The psychiatrist in the nursing home stopped the Risperdal, which can cause twitching and vocal tics, and prescribed a sedative and two other antipsychotics.
“I knew the drugs were doing this to her,” her daughter said. “I told him to stop the medications and stay away from Mom.”Not until yet another doctor took Mrs. Lamascola off the drugs did she begin to improve.
The use of antipsychotic drugs to tamp down the agitation, combative behavior and outbursts of dementia patients has soared, especially in the elderly. Sales of newer antipsychotics like Risperdal, Seroquel and Zyprexa totaled $13.1 billion in 2007, up from $4 billion in 2000, according to IMS Health, a health care information company.
Part of this increase can be traced to prescriptions in nursing homes. Researchers estimate that about a third of all nursing home patients have been given antipsychotic drugs.
The increases continue despite a drumbeat of bad publicity. A 2006 study of Alzheimer’s patients found that for most patients, antipsychotics provided no significant improvement over placebos in treating aggression and delusions.
In 2005, the Food and Drug Administration ordered that the newer drugs carry a “black box” label warning of an increased risk of death. Last week, the F.D.A. required a similar warning on the labels of older antipsychotics.
The agency has not approved marketing of these drugs for older people with dementia, but they are commonly prescribed to these patients “off label.” Several states are suing the top sellers of antipsychotics on charges of false and misleading marketing.
Ambre Morley, a spokeswoman for Janssen, the division of Johnson & Johnson that manufactures Risperdal, would not comment on the suits, but said: “As with any medication, the prescribing of a medication is up to a physician. We only promote our products for F.D.A.-approved indications.”
Nevertheless, many doctors say misuse of the drugs is widespread. “These antipsychotics can be overused and abused,” said Dr. Johnny Matson, a professor of psychology at Louisiana State University. “And there’s a lot of abuse going on in a lot of these places.”
Dr. William D. Smucker, a member of the American Medical Directors Association, a group of health professionals who work in nursing homes, agreed. Though the group encourages doctors to conduct a thorough assessment and prescribe antipsychotics only as a last resort, he said, “Many physicians are absent without leave in the nursing home and don’t take an active role in the assessment of the patient.”
Some nursing homes are trying a different approach, so-called environmental intervention. The strategies include reducing boredom, providing intellectual and physical stimulation, exercise, calming music, bringing in pets for therapy and improving how the staff approaches and talks to dementia patients.
At the Margaret Teitz Nursing and Rehabilitation Center in Queens, social workers do life reviews of patients to understand their interests, lifestyle and former occupations.
“I had a patient who used to be in fashion,” said Nancy Goldwasser, the director of social services. “So we got her fabric samples. And she’d sit and look through the books, touch the fabric, and it would calm her.”
But such approaches are time consuming, they do not help all patients, they can be prohibitively expensive and they will be more difficult to provide as Alzheimer’s continues to increase.
“Our health care system isn’t set up to address the mental, emotional and behavioral problems of the elderly,” said Dr. Gary S. Moak, president of the American Association for Geriatric Psychiatry.
Nursing homes are short staffed, and insurers do not generally pay for the attentive medical care and hands-on psychosocial therapy that advocates recommend. It is much easier to use sedatives and antipsychotics, despite their side effects.
The first generation of antipsychotics, like Haldol, carry a significant risk of repetitive movement disorders and sedation. Second-generation antipsychotics, also called atypicals, are more commonly prescribed because the risk of movement disorders is lower. But they, too, can cause sedation, and they contribute to weight gain and diabetes.
Used correctly, the drugs do have a role in treating some seriously demented patients, who may be incapacitated by paranoia or are self-destructive or violent. Taking the edge off the behavior can keep them safe and living at home, rather than in a nursing home.
If patients are prescribed an antipsychotic, it should be a very low dose for the shortest period necessary, said Dr. Dillip V. Jeste, a professor of psychiatry and neuroscience at the University of California, San Diego.
It may take a few weeks or months to control behavior. In many cases, the patient can then be weaned off of the drugs or kept at a very low dose.
Some experts say another group of medications — antidementia drugs like Aricept, Exelon and Namenda — are underused. Research shows that 10 to 20 percent of Alzheimer’s patients had noticeable positive responses to the drugs, and 40 percent more showed some cognitive improvement, even if it was not noticeable to an observer.
“Sometimes, it’s enough to take the edge off the behavioral problems, so the family and patient can live with it and you don’t expose people to much risk,” said Dr. Gary J. Kennedy, director of geriatric psychiatry at the Montefiore Medical Center in the Bronx.
Other experts cite a lack of research backing these drugs for behavioral problems.
If patients begin showing behavioral symptoms of dementia, doctors said, they should have complete medical and psychiatric workups first, especially if symptoms develop suddenly.
“Just because someone is 95 does not mean one should not do a workup, especially if she’s been healthy,” Dr. Kennedy said.
Common causes of the symptoms include ministrokes, reparable brain hemorrhage from a mild bump on the head, hypothyroidism, dehydration, malnourishment, depression and sleep disorders.
Some doctors point out that simply paying attention to a nursing home patient can ease dementia symptoms. They note that in randomized trials of antipsychotic drugs for dementia, 30 to 60 percent of patients in the placebo groups improved.
“That’s mind boggling,” Dr. Jeste said. “These severely demented patients are not responding to the power of suggestion. They’re responding to the attention they get when they participate in a clinical trial.
“They receive both T.L.C. and good general medical and humane care, which they did not receive until now. That’s a sad commentary on the way we treat dementia patients.”
To family members looking at a nursing home for an aging parent, experts recommend seeking out homes with low staff turnover, a high ratio of staff members to patients, and programs with psychosocial components.
The Medicare Web site has basic information on individual homes at www.medicare.gov/NHcompare. The National Citizens’ Coalition for Nursing Home Reform, at www.nccnhr.org, offers a consumer guide to choosing a nursing home.
If medications are necessary, a family member should communicate with the prescribing doctor, learn the goal of each medication and be involved in making the decision.
Dr. Moak, of the psychiatry association, emphasized seeking out the doctor. Family members, he said, “often speak through the nursing staff, and that’s a huge mistake.”
Family members who are not convinced that a relative is receiving the best care should get a second opinion, as Ramona Lamascola did.
The physician she consulted, Dr. Kennedy of Montefiore, stopped her mother’s antipsychotics and sedatives and prescribed Aricept.
“It’s not clear whether it was getting her hypothyroid and other medical issues finally under control or getting rid of the offending medications,” he said. “But she had a miraculous turnaround.”
Theresa Lamascola still has dementia, but she went from confinement in a wheelchair — unable to sit still and screaming out in fear — to being able to walk with help, sit peacefully, have some memory and ability to communicate, understand subtleties of conversations and even make jokes.
Or, as her daughter put it, “I got my mother back.”
For a Sharp Brain, Stimulation
By Roni Caryn Rabin : NY Times Article : May 13, 2008
Americans may worry about heart disease, stroke and diabetes, but they downright dread Alzheimer’s disease, a recent survey found.
For good reason. One in eight adults over 65 is affected by the disease. Those who are spared know they may end up with the burden of caring for a parent or a spouse who is affected. Even though the number of older adults with dementias is rising rapidly, only a few drugs that have been approved to treat symptoms are on the market, and they slow down the disease but do not cure it.
Researchers, however, are more optimistic than ever about the potential of the aging brain, because recent evidence has challenged long-held beliefs by demonstrating that the brain can grow new nerve cells.
“For a long time, we held the assumption that we’re born with all the nerve cells we’re ever going to have, and that the brain is not capable of generating new ones — that once these cells die we’re unable to replace them,” said Molly V. Wagster, chief of the Neuropsychology of Aging branch of the National Institute on Aging. “Those assumptions have been challenged and put by the wayside.”
The birth of new nerve cells, she said, “has been shown to occur in the adult — not only in adult rats and monkeys, but also in older adult humans.” Most of the areas that show neurogenesis and that have been investigated so far are important for learning and memory, particularly the hippocampus, she added.
So how does one stimulate neurogenesis?
Scientists do not have all the answers, but studies of older people who have maintained their mental acuity provide some clues. They tend to be socially connected, with strong ties to relatives, friends and community. They are often both physically healthy and physically active. And they tend to be engaged in stimulating or intellectually challenging activities.
The big question is whether they remain mentally alert because they engage in these activities, or whether they are able to engage in these activities because they are cognitively intact.
“We don’t know whether this is an example of reverse causation or not — it’s probably a two-way street,” said Bruce S. McEwen, who heads the neuroendocrinology lab at Rockefeller University in New York.
But some interventional studies that have introduced older adults to exercise regimens have reported remarkable results. Researchers at the University of Illinois at Urbana-Champaign recruited a group of sedentary adults between the ages of 60 and 75, assigning half of them to an aerobic exercise program that met three times a week to walk, while a control group did anaerobic stretching and toning.
The scientists measured the group’s cognitive function before and after the six-month program and found improvements among those who had done the walking.
“Six months of exercise will buy you a 15 to 20 percent improvement in memory, decision-making ability and attention,” said Arthur F. Kramer, a professor of psychology at the University of Illinois. “It will also buy you increases in the volume of various brain regions in the prefrontal and temporal cortex, and more efficient neuronetworks that support the kind of cognition we examined.”
Other studies have found improvements in cognitive function after a combined regimen of physical exercise and cognitive training.
But skeptics say there is no guarantee that intellectual stimulation will prevent Alzheimer’s disease or other forms of dementia. “Maybe it does, but I don’t think we have a shred of evidence,” said Dr. Robert N. Butler, a psychiatrist and gerontologist who is president of the International Longevity Center-USA. “What it does is maintain good health,” he said, adding, “I don’t think we can go much further than that.”
But there is consensus among scientists on a few recommendations for action that, most agree, cannot hurt.
Regular physical activity may improve brain function, both by increasing blood flow to the brain and stimulating the production of hormones and nerve growth factors involved in neurogenesis. Animal studies have found that physically active animals have better memories and more cells in their hippocampus. Exercise also plays a role in countering diseases like Type 2 diabetes, which increases the risk of dementia. Cholesterol and hypertension, which affect vascular health, also need to be kept in check.
Seeking out stimulation through interesting work, volunteer opportunities or continuing education is beneficial. Travel, read, take up a new language or learn to play a musical instrument. Staying socially connected is also associated with brain health, as is managing stress effectively. Chronic stress can lead to the rewiring of areas of the brain that are involved in emotion, memory and decision-making, Dr. McEwen said, “and the brain becomes more biased toward more anxiety, more depression, less flexibility in terms of decision-making and becomes less able to store information.”
Most scientists recommend eating a Mediterranean-style diet, including fish and nuts containing omega-3 fatty acids, antioxidant-rich fruits and vegetables, olive oil and possibly some red wine. (Blueberries are also recommended.) Some also suggest avoiding playing games like football, because of the risk of head injuries, staying away from pesticides and insecticides that contain neurotoxins and not drinking excessively.
“Another thing that’s important as people get older is to maintain flexible attitudes and be willing to try new things,” said K. Warner Schaie, who in 1956 started the Seattle Longitudinal Study, which follows the psychological development of participants through adulthood. “You have to expect things will shift over time and won’t be the same as when you were young. Those who manage to roll with the punches, and enjoy change rather than fighting it, tend to do well.”
An active social life appears to delay memory loss as we age, a new study shows.
The finding, which appears in the July issue of The American Journal of Public Health, suggests that strong social ties, through friends, family and community groups, can preserve our brain health as we age and that social isolation may be an important risk factor for cognitive decline in the elderly.
Researchers at the Harvard School of Public Health used data gathered from 1998 to 2004 from the Health and Retirement Study, a large, nationally representative population of American adults ages 50 and older. Participants took memory tests at two-year intervals during the study period. Testers read a list of 10 common nouns to survey respondents, who were then asked to recall as many words as possible immediately and again after a five-minute delay. The researchers also measured social integration based on marital status, volunteer activities, and contact with parents, children and neighbors.
The results showed that individuals who in their 50s and 60s engaged in a lot of social activity also had the slowest rate of memory decline. In fact, compared to those who were the least socially active, study subjects who had the highest social integration scores had less than half the rate of memory loss. The researchers controlled for variables like age, gender, race and health status. Those who had the fewest years of formal education appeared to have the most to gain from an active social life as they aged. The study showed that the protective effect of social integration was greatest among individuals with fewer than 12 years of education.
“The working hypothesis is that social engagement is what makes you mentally engaged,'’ said Lisa F. Berkman, the study’s senior author and director of the Harvard Center for Population and Development Studies. “You can’t sit and withdraw if you’re constantly talking and working on things and figuring out problems in your daily life. It’s not just completing a crossword puzzle, it’s living your life.'’
The data are particularly important for those caring for aging family members. Simply visiting and giving support to an older family member does not make them socially engaged. “A lot of people when they think about the elderly focus on social support — things like what can I do for an older mother,'’ Dr. Berkman said. “But having someone to count on is not what we’re measuring. It’s not about support, it’s about being completely engaged and participating in our society.'’
What was notable about the study is that participants didn’t have to be married or surrounded by extensive family to receive the protective effect of social engagement. “There are lots of relationships that are substitutable,'’ Dr. Berkman said. “You don’t have to have friends if you have family. If you don’t have family but you have friends, that’s good. If you volunteer in civic organizations, that can substitute. People don’t have to have all of these things. They just have to have some breadth and diversity in the kinds of networks and ties they have in a community.'’
How Soon Is Too Soon to Screen
People for Alzheimer's Disease?
By Shirley Wang : WSJ Article : November 18, 2007
Early detection of Alzheimer's disease can be crucial, giving patients a chance to plan for the future and take medication to keep symptoms from worsening, at least for a while. Many geriatric experts advocate routine screening of older people for the disease, to give patients their best shot at treatment.
But a number of patient advocates and physicians say the push for widespread screening is premature. There are no data showing that screening people who have no memory complaints actually leads to better outcomes. And there are potential negative consequences, these critics say, including false positives that needlessly put patients at risk for depression or anxiety.
"The worry," says Bill Thies, vice president of medical and scientific relations at the Alzheimer's Association, is that patients may react to positive results in "inappropriate" ways. "Will they become fully depressed?" he says. "If that's the case, then you're going to obscure any public-health benefit."
Screening proponents say the Alzheimer's tests are quick, easy to use and can identify most people with memory problems who warrant further evaluation. Screening can involve just a few tests, such as word recall. And it could be part of a routine physical for patients over 65 years old, according to a proposal from the Alzheimer's Disease Screening Discussion Group -- a group of academic health centers, drug companies and patient-advocacy groups that met at a drug-industry-sponsored meeting last month.
One organization, the Alzheimer's Foundation of America, has held a national memory-screening day each of the past five years. "What we're trying to do now is make memory screening a part of the actual physical process," says Eric Hall, chief executive of the foundation. "What would be so terribly wrong with doctors capturing a baseline memory score for future reference?"
Many researchers, as well as the Alzheimer's Association, a nonprofit focused on disease research and patient care, believe that in patients who aren't exhibiting noticeable memory problems, the benefits of screening aren't clear. Some patients worry that if they screen positive, they might lose their driver's license or job, or have trouble getting life insurance, even if their symptoms don't yet affect their daily functioning.
Some doctors also note that it doesn't help to diagnose people who don't yet have noticeable memory problems because existing medications appear to help only patients who are already suffering clear symptoms.
The lack of systematic follow-up for screening adds to the worry for some doctors and researchers. A recent study in the Journal of General Internal Medicine found that of 524 adults screened in a doctor's office, only one in five who screened positive was referred to a specialist or received a diagnosis or a prescription for medication.
Study author Soo Borson, professor and dementia specialist at the University of Washington, says researchers didn't determine why there was so little follow-up, but lack of time may be one issue.
What doctors and geriatric researchers generally agree on is that testing is helpful in diagnosing patients who are already showing signs of memory problems.
Kathy Frank of Beech Grove, Ind., had concerns about her 66-year-old husband, Charles, for nearly two years. She remembers a time when he forgot his Social Security number and other instances when he couldn't recall certain words. When she suggested he get tested, he jokingly replied, "I think you should get tested."
After becoming disoriented at work several months ago, however, Mr. Frank was concerned enough that he went to the doctor, who found he had had a stroke. The doctor recommended further evaluation, in part because Mr. Frank had a family history of Alzheimer's. He went through a battery of neuropsychological tests that lasted several hours and evaluated many aspects of his cognitive functioning. So far, tests indicate Mr. Frank doesn't have Alzheimer's, but his memory will be re-evaluated next year.
Money Woes Can Be Early Clue to Alzheimer’s
By Gina Kolata : NT Times : October 30, 2010
Renee Packel used to have a typical suburban life. Her husband, Arthur, was a lawyer and also sold insurance. They lived in a town house just outside Philadelphia, and Mrs. Packel took care of their home and family.
One day, it all came crashing down. The homeowners’ association called asking for their fees. To Mrs. Packel’s surprise, her husband had simply stopped paying them. Then she learned he had stopped writing checks to his creditors, too.
It turned out that Mr. Packel was developing “It just disappeared,” she said.
What happened to the Packels is all too common, Alzheimer’s experts say. New research shows that one of the first signs of impending dementia is an inability to understand money and credit, contracts and agreements.
It is not just families who are affected — financial advisers and lawyers say they are finding themselves in a bind when their clients’ minds seem to be slipping.
The Financial Industry Regulatory Authority, the largest nongovernmental regulator for securities firms doing business in the United States, recently met with individual financial services companies and the Alzheimer’s Association to formulate guidelines on how to deal with clients who have trouble remembering and reasoning, a problem that is not new but is increasing as the population ages.
The issue is far from simple. Dr. Jason Karlawish, an associate professor of medicine and medical ethics at the University of Pennsylvania, says it is generally agreed that decisions by a competent adult should be respected.
But, he said, “What do we mean when we say someone has enough decision-making capacity to be ‘competent’? The law, psychology and finance are all waking up to issue of decision-making capacity.”
The issue promises to become even more complicated as researchers and doctors diagnose Alzheimer’s earlier and earlier. If new brain scans and other methods show signs that a person is developing dementia, does that mean the patient should be watched, or that there should be limits on his or her abilities to make financial or legal decisions?
Financial firms are in “a dicey situation” if they have to decide whether a client can make major decisions about finances or future plans, said John M. Gannon, senior vice president for investor education with the financial regulatory agency. “Even doctors can have trouble figuring that out,” he said.
And yet, according to research by Daniel C. Marson, a neuropsychologist at the University of Alabama, Birmingham, confusion over money and finances is perhaps the most important and most predictable early functional change as people descend into dementia.
For lawyers, the main question is at what point a client lacks the capacity to execute a will or other document, and who decides when that point has been reached. And if a lawyer lets a client go ahead, will the document be challenged?
Lawyers have guidelines, published in 2005, that include warning signs of diminished capacity, like memory loss and problems communicating and doing calculations. The guidelines instruct lawyers to look at the legal requirements for capacity in specific situations, like making a gift. But many questions remain, said Charles P. Sabatino, who leads the American Bar Association’s Commission on Law and Aging.
“Courts are always struggling to come up with principles and definitions of capacity,” Mr. Sabatino said. Definitions of capacity vary among the states.
All too often, though, no one protects people who are losing their capacity to execute documents and their judgment about finances. Their stories of decisions gone awry tend to end badly.
Mrs. Packel had to close her husband’s business and sell their house to pay lawyers and creditors. Now they live in a one-bedroom apartment in Philadelphia. Mrs. Packel, who is 75, supports herself and her husband by working as a receptionist. He goes to adult day care.
“It’s such a complete turnaround,” Mrs. Packel said. “Arthur was a very, very bright man.”
Spotting the Problem
Last year, Fidelity Investments surveyed 350 investment advisers. The advisers were asked if they suspected that any of their clients had Alzheimer’s or were developing it, and what they did about it. The advisers also were asked if they had mentioned the problem to their clients.
Most — 84 percent — said they thought they had had clients with Alzheimer’s or symptoms indicating that they were developing it. And 96 percent said they did not feel prepared to deal with those clients. Half said they were not comfortable even raising the subject of dementia. They worried that they might be wrong about a client’s mental capacity, and even if they were right, they did not know what they were supposed to do about it or where to refer the client for assessment and help.
The survey was an impetus for this year’s meeting involving investment advisers, the Alzheimer’s Association and the financial regulatory agency, said David Canter, an executive vice president at Fidelity.
‘Protect Your Client’
Lawyers see another side of the dementia problem. They too can end up in situations with no clear resolutions.
Robert Grant, a lawyer in Palo Alto, Calif., explained what happens in California.
“Your first duty is to your client,” Mr. Grant said. “You have a duty to protect your client. Often there will be discussions with the family about whether your client is capable of handling things. But you are prohibited from disclosing information about your client without the client’s permission.”
And clients — suspicious, forgetful, disturbed by or denying their impending dementia — may not want their lawyer to discuss their behavior with their families.
“In one sense it is straightforward,” Mr. Grant said. “You have a bunch of rules out there.”
For example, a lawyer has to make an independent determination that the client is competent. If the lawyer determines the client is incompetent but the client insists on executing a document, the rules say the lawyer should withdraw representation. However, Mr. Grant said, “one can question whether withdrawal from representation of an incompetent client is actually in the client’s best interest.”
Bruce Wampler of Glenwood Springs, Colo., said the law was of limited help in dealing with his father, who lived alone in Casper, Wyo., and, in his dementia, had forbidden his son to visit him.
Concerned about his father’s capacity to make decisions, Mr. Wampler went to court and won guardianship, angering his father so much that he refused to speak to Mr. Wampler for nearly a year.
Meanwhile, a neighbor who believed that the elderly Mr. Wampler was being ignored by his family found a lawyer who arranged to have the guardianship rescinded. The neighbor also encouraged the father to change his will, leaving much of his money to organizations he had never supported, his son said. At the same time, the elder Mr. Wampler was sending substantial amounts to lottery schemes.
The bar association’s handbook for lawyers, written with the American Psychological Association, tries to provide some guidance. But the handbook acknowledges that it may not be easy to determine a client’s capacity to sign a will, execute a contract or transfer property.
“The law wants a yes-or-no answer,” Mr. Sabatino said.
But medical evaluations come in shades of gray, discussing strengths and weakness in reasoning and mental abilities. The assessments place patients on a continuum. “They don’t like to give a yes-or-no answer,” Mr. Sabatino said.
And persuading clients to have medical evaluations can be difficult, as the law association’s handbook acknowledges.
“A referral to a clinician requires client consent, and can be quite traumatic for the client, as well as unsettling for the lawyer-client relationship,” the handbook states, adding, “Also, it is expensive.”
Losing Everything
Dr. Max Gomez had problems with both finances and legal documents. And by the time his son found out, Dr. Gomez had lost everything.
Dr. Gomez, an obstetrician-gynecologist, lived alone in Miami and worked at a nearby general medical clinic where he was the director. His son, who is also named Max, is the medical correspondent for CBS News and lives in New York.
Dr. Gomez was no longer seeing patients, his son said. The clinic, he explained, “was basically a place that gave him somewhere to go and something to do.” It operated under Dr. Gomez’s license.
It turned out that Dr. Gomez actually was the medical director for as many as five or six clinics, his son said, adding, “Whether he realized that and signed on or whether someone put papers in front of him and said, ‘Here, sign this and you’ll be medical director’ is not really clear.”
At least one of the clinics also appropriated Dr. Gomez’s identification number for Medicare and Medicaid, using it to fraudulently bill for several million dollars worth of goods and services, as Dr. Gomez’s son learned from the Federal Bureau of Investigation.
Then Dr. Gomez’s son got a call from his father’s condominium association. His fees were not being paid. The clinic was supposed to have been paying but had stopped.
The clinic had closed, but Dr. Gomez did not realize that. When he drove there and the doors were locked he would think it was a weekend and drive home, his son said.
The clinic had also stopped paying Dr. Gomez’s mortgage. Dr. Gomez thought the clinic was buying the apartment and allowing him to live there. Instead, it turned out that Dr. Gomez was the owner. His son later learned that, at closing, the clinic also took out a second mortgage on the apartment in Dr. Gomez’s name. He was responsible for both mortgages. The bank foreclosed.
As Dr. Gomez’s son tried untangling the mess, he discovered his father’s bank account had been plundered by a woman who talked him out of his savings. There was check after check written to the woman, signed by Dr. Gomez but made out in someone else’s handwriting.
Only his Social Security payments were left. They were being deposited in a bank account that Dr. Gomez had forgotten about. The complications mushroomed. Dr. Gomez’s son received a letter from a bank saying his father owed about $50,000. It turned out that Dr. Gomez was listed as an officer of the clinic and a personal guarantor on a loan. “I talked to attorneys, and they said, ‘That’s crazy, no one signs to be a personal guarantor on a commercial loan,’ ” his son said.
Dr. Gomez’s creditors could not collect, though. His assets were gone.
He now lives in an assisted-living facility in New York and seems content, his son said. He seems to have forgotten most of his experiences in Miami.
But every now and then, Dr. Gomez will be troubled.
“He will see me filling out papers for Medicaid,” his son says. “He says, ‘Medicaid? But I have money.’ ”
“He’s a proud man,” Dr. Gomez’s son said. “He is used to giving orders rather than taking them.
“It’s a sad story. But I’m afraid it’s not an uncommon one.”
Finding Alzheimer’s Before a Mind Fails
By Denise Grady : NY Times Article : December 26, 2007
For a perfectly healthy woman, Dianne Kerley has had quite a few medical tests in recent years: M.R.I. and PET scans of her brain, two spinal taps and hours of memory and thinking tests.
Ms. Kerley, 52, has spent much of her life in the shadow of an illness that gradually destroys memory, personality and the ability to think, speak and live independently. Her mother, grandmother and a maternal great-aunt all developed Alzheimer’s disease. Her mother, 78, is in a nursing home in the advanced stages of dementia, helpless and barely responsive.
“She’s in her own private purgatory,” Ms. Kerley said.
Ms. Kerley is part of an ambitious new scientific effort to find ways to detect Alzheimer’s disease at the earliest possible moment. Although the disease may seem like a calamity that strikes suddenly in old age, scientists now think it begins long before the mind fails.
“Alzheimer’s disease may be a chronic condition in which changes begin in midlife or even earlier,” said Dr. John C. Morris, director of the Alzheimer’s Disease Research Center at Washington University in St. Louis, where Ms. Kerley volunteers for studies.
But currently, the diagnosis is not made until symptoms develop, and by then it may already be too late to rescue the brain. Drugs now in use temporarily ease symptoms for some, but cannot halt the underlying disease.
Many scientists believe the best hope of progress, maybe the only hope, lies in detecting the disease early and devising treatments to stop it before brain damage becomes extensive. Better still, they would like to intervene even sooner, by identifying risk factors and treating people preventively — the same strategy that has markedly lowered death rates from heart disease, stroke and some cancers.
So far, Alzheimer’s has been unyielding. But research now under way may start answering major questions about when the disease begins and how best to fight it.
A radioactive dye called PIB (for Pittsburgh Compound B) has made it possible to use PET scans to find deposits of amyloid, an Alzheimer’s-related protein, in the brains of live human beings. It may lead to earlier diagnosis, help doctors distinguish Alzheimer’s from other forms of dementia and let them monitor the effects of treatment.
Studies with the dye have already found significant deposits in 20 percent to 25 percent of seemingly normal people over 65, suggesting that they may be on the way to Alzheimer’s, though only time will tell.
“PIB is about the future of where Alzheimer’s disease needs to be,” said Dr. William E. Klunk, a co-discoverer of the dye at the Alzheimer’s research center at the University of Pittsburgh. “PIB is being used today to help determine whether drugs that are meant to prevent or remove amyloid from the brain are working, so we can find drugs that prevent the underlying pathology of the disease.”
Though PIB is experimental now, studies began in November that are intended to lead to government approval for wider use.
Currently, for the most common form of Alzheimer’s disease, which occurs after age 65, there is no proven means of early detection, no definitive genetic test. But PIB tests might be ready before new treatments emerge, making it possible to predict who will develop Alzheimer’s — without being able to help.
Researchers are also using M.R.I. scans to look for early brain changes, and testing blood and spinal fluid for amyloid and other “biomarkers” to see if they can be used to predict Alzheimer’s or find it early.
Studies of families in which multiple members have dementia are helping to sort out the genetic underpinnings of the disease.
Finally, experiments are under way to find out whether drugs and vaccines can remove amyloid from the brain or prevent its buildup, and whether doing so would help patients. The new drugs, unlike the ones now available, have the potential to stop or slow the progress of the disease. At the very least, the drug studies will be the first real test of the leading theory of Alzheimer’s, which blames amyloid for setting off a chain of events that ultimately ruin the brain.
Some scientists doubt the amyloid theory, but even a staunch skeptic said the studies were important.
Among the skeptics is Dr. Peter Davies, a professor at Albert Einstein Medical College, who said: “You’ve got to try. Somebody’s going to get this right.”
But if the amyloid hypothesis does not hold up, much of Alzheimer’s research could wind up back at Square 1.
Answers are urgently needed. Alzheimer’s was first recognized 100 years ago, and in all that time science has been completely unable to change the course of the disease. Desperate families spend more than $1 billion a year on drugs approved for Alzheimer’s that generally have only small effects, if any, on symptoms. Patients’ agitation and hallucinations often drive relatives and nursing homes to resort to additional, powerful drugs approved for other diseases like schizophrenia, drugs that can deepen the oblivion and cause severe side effects like diabetes, stroke and movement disorders.
Alzheimer’s is the most common cause of dementia (artery disease, Parkinson’s and other brain disorders can also lead to dementia). Five million people in the United States have Alzheimer’s, most of them over 65. It is the nation’s sixth leading cause of death by disease, killing nearly 66,000 people a year and probably contributing to many more deaths. By 2050, according to the Alzheimer’s Association, 11 million to 16 million Americans will have the disease. “Sixteen million is a future we can’t countenance,” said William H. Thies, the association’s vice president for medical and scientific relations. “It will bankrupt our health care system.”
The costs are already enormous, $148 billion a year — more than three times the cost of chronic lung disease, even though Alzheimer’s kills only half as many people. To a great extent, increases in dementia are the price of progress: more and more people are living long enough to get Alzheimer’s, some because they survived heart disease, strokes or cancer. It is a cruel trade-off. The disease is by no means inevitable, but among people 85 and older, about 40 percent develop Alzheimer’s and spend their so-called golden years in a thicket of confusion, ultimately becoming incontinent, mute, bedridden or forced to use a wheelchair and completely dependent on others.
“It makes people wonder whether they really want to live that long,” Dr. Klunk said.
The potential market for prevention and treatment is enormous, and drug companies are eager to exploit it. If a drug could prevent Alzheimer’s or just reduce the risk, as statins like Lipitor do for heart disease, half the population over 55 would probably need to take it, Dr. Thies said.
If new drugs do emerge, they will come from studies in patients who already have symptoms, Dr. Thies said. But he said the emphasis would quickly shift to treating people at risk, before symptoms set in. Many researchers doubt that even the best preventive drugs will be able to heal the brains of people who are already demented.
Treating preventively, Dr. Thies said, “will be more satisfying to patients and physicians, and there will be an economic incentive because you’ll wind up treating more people.”
The only thing that could slow the drive for early treatment, he said, would be serious side effects — and Dr. Morris, at Washington University, said drugs powerful enough to treat Alzheimer’s would probably have strong side effects.
Researchers are especially eager to study people like Ms. Kerley, because the children of Alzheimer’s patients have a higher-than-average risk of dementia themselves, and tracking their brains and minds may open a window onto the earliest stages of the disease.
“I want to do anything I can possibly do to help find a cure or find a way to identify it earlier,” Ms. Kerley said. “We need to stop this. I don’t know if it will help my generation, but it will help my son’s.”
She figures that being a research subject may have advantages, too.
“We’re the first ones in line,” she said. “If I am genetically predisposed, and they have a preventive medication, they’ll tell me right away.”
Alzheimer’s Beginnings
Some forgetfulness is normal. Distraction, stress, fatigue and medications can contribute. A joking rule of thumb about Alzheimer’s is actually close to the truth: it’s O.K. to forget where you put your car keys, as long as you remember what a key is for. But worsening forgetfulness is a cause for concern.
Doctors use standard memory and reasoning tests to diagnose dementia, along with symptoms reported by the patient and family members. The term “mild cognitive impairment” is sometimes applied to small but measurable memory problems. But its meaning is unclear: some studies find that the impairment can resolve itself, while others suggest that it always progresses to dementia.
Even if older patients think more slowly or take longer to remember, as long as they can still function independently, they are not demented, Dr. Morris said.
In her heart, Ms. Kerley suspects that her mother’s Alzheimer’s disease began long before the official diagnosis in 2001 or even the tentative one in 1995 — years before, maybe decades. She wonders if the disease might explain, at least in part, her mother’s difficult personality and lack of interest in reading or education.
When does Alzheimer’s begin? The question haunts families and captivates scientists.
Dr. Morris said, “We think that by the time an individual begins to experience memory loss, there is already substantial brain damage in areas critical to memory and learning.”
No one knows whether the disease affects thinking, mood or personality before memory fails. Researchers think that the brain, like other vital organs, has a huge reserve capacity that can, at least for a time, hide the fact that a disease is steadily destroying it.
“I’m speculating that it does affect you throughout life,” said Dr. Richard Mayeux, a professor of neurology, psychiatry and epidemiology at Columbia University, and co-director of its Taub Institute for Research on Alzheimer’s Disease and the Aging Brain. “I think there’s a very long phase where people aren’t themselves.”
If Dr. Mayeux asks family members when a patient’s memory problem began, they almost always say it started a year and a half before. If he then asks when was the last time they thought the patient’s memory was perfectly normal, many reply that the patient never really had a great memory.
Several studies in which people had intelligence tests early in life and were then evaluated decades later have found that compared with the healthy people, those with Alzheimer’s had lower scores on the early tests.
“It raises the possibility for me that this is a genetic disorder that starts early in life,” Dr. Mayeux said.
He said those findings also made him wonder about the widely dispensed advice to read, take courses, solve puzzles and stay mentally active to ward off Alzheimer’s. The advice is based on studies showing that highly educated people have a lower risk of Alzheimer’s than do less-accomplished ones. But does that mean that mental activity prevents Alzheimer’s — or vice versa?
‘I Have Lost Myself’
The disease is named for Alois Alzheimer, a German doctor who first described it in Auguste D., a 51-year-old patient he saw in 1901. Her memory, speech and comprehension were failing, and she suffered from hallucinations and paranoid delusions that her husband was unfaithful. Unable to finish writing her own name, she told Alzheimer, “I have lost myself.”
She died in 1906, “completely apathetic,” curled up in a fetal position and “in spite of all the care and attention,” suffering from bedsores, Alzheimer wrote.
A century later, patients still die in much the same way. Although Alzheimer’s itself can kill by shutting down vital brain functions, infections usually end things first — pneumonia, bladder infections, sepsis from bedsores.
When Alzheimer dissected Auguste’s brain, he found it markedly shrunken, a wasteland of dead and dying nerve cells littered with strange deposits.
There were two types of deposits, plaques and tangles. Plaques occur between nerve cells, and are now known to consist of clumps of beta amyloid, an abnormal protein. Tangles form inside nerve cells, and are made of a protein called tau that is normally part of a system of tubules that carry nutrients to feed the cell. Once tau is damaged, the nerve cells essentially starve to death.
Until the 1970s Alzheimer’s disease was considered a rare brain disorder that mysteriously struck younger people like Auguste D.
It was thought to be different from “senility,” which was assumed to be a consequence of aging. But then researchers compared the brains of younger people who had died of Alzheimer’s with those of elderly people who had been senile, and discovered the same pathology — plaques and tangles. Senility, they decided, was not a natural part of aging; it was a disease.
The Amyloid Hypothesis
The leading theory of Alzheimer’s says that beta amyloid, or A-beta, is the main culprit, building gradually in the brain over decades and short-circuiting synapses, the junctions where nerve cells transmit signals to one other. Gradually, the theory goes, the cells quit working and die.
Everybody produces A-beta, but its purpose is not known. People who develop Alzheimer’s either make too much or cannot get rid of it. Although scientists once blamed plaques for all the trouble, more recent research suggests that the real toxins are smaller bundles of A-beta molecules that form long before plaques do.
Dr. Dennis J. Selkoe, a professor of neurologic diseases at Harvard, said that just as lowering cholesterol
Several drugs and vaccines are now being tested that either block the production of A-beta or help the body get rid of it.
Researchers are also testing anti-amyloid antibodies, which are proteins made by the immune system, as well as blood serum that contains the antibodies.
Eventually, Dr. Selkoe said, screening tests for Alzheimer’s “will be like getting an EKG in the doctor’s office at 45 or 50, and you’ll start treating right away to prevent Alzheimer’s rather than treat it.”
Other researchers are less enthusiastic, noting that there have been numerous failures and disappointments along the way. A vaccine study had to be halted in 2002 because 18 of 300 patients developed encephalitis, and 2 died. Some scientists worry that anti-amyloid vaccines in general could be dangerous, in part because the role of amyloid is not well understood and the brain may actually need it.
No Choice but to Cope
Even if current research yields new drugs, there is not likely to be a miracle pill that will bring people back from deep dementia. For now, there is no choice but to cope with the disease. Seventy percent of Alzheimer’s patients are cared for at home, and millions of families are struggling to look after them, piecing together a patchwork of relatives, friends, paid health aides and adult day-care programs.
Barbara Latshaw, 79, lives with her husband, David, and her sister in Crafton, Pa., near Pittsburgh. Ms. Latshaw, whose dementia was diagnosed in 1991, has not spoken in four years, and she can no longer smile. But she locks eyes with visitors and will not let go.
“There is still something alive in there,” said her sister, Fritzie Hess, 69. “I’m convinced of it.”
The family believes that, at least some of the time, she still understands them. They speak to her as if she does. She is with them, and yet gone, and they miss her terribly.
“We hope to keep her here at home until she passes on,” Ms. Hess said. “She’s a joy to us.”
Many families hope to keep Alzheimer’s patients at home, but not all can manage it, especially if family members have to go work or patients become combative, incontinent, immobile or unable to sleep at night.
“There are three of us taking care of my sister, and it works out beautifully,” Ms. Hess said. “We spell each other. I don’t know how these spouses manage, when it’s one on one.”
Ms. Hess and her brother-in-law are retired, and Ms. Latshaw’s daughter, Becky Bannon, 53, is free to visit many mornings to help them get her mother out of bed, massage and exercise her arms and legs, change her diaper and dress and feed her.
Ms. Latshaw used to be full of life. She loved to cook, played tennis and bridge, raised two children and took charge of redecorating the grand old family home. Then her memory began to slip: guests would arrive for dinner, and she would have no memory of inviting them. She forgot to look before pulling into traffic, and nearly caused an accident. She would wander out of the house, and local store clerks would take her home. She never turned hostile or angry, as many demented patients do, but she had vivid hallucinations of strings being caught in her teeth, and little men getting into her bed and jabbing her with broom straws. On especially bad nights, her husband would get up with her at 2 or 3 a.m. and make the two of them hot chocolate.
Aricept, an Alzheimer’s drug, made the hallucinations worse, while another drug, an antipsychotic used for schizophrenia, seemed to quell them. But the second drug had side effects: after taking it for several years, Ms. Latshaw began to grind her teeth, and could not stop moving her arms and legs.
Their father also suffered from dementia, Ms. Hess said, admitting that she wonders about herself.
“Naturally I’m a little bit concerned, but I think worry is such a waste of time, so I don’t dwell on it; I just don’t,” she said. “My friends always said, ‘You always had a bad memory.’ I see Barbara and David’s children having that same kind of memory.”
Ms. Hess has volunteered for studies at the University of Pittsburgh Medical Center, where she became the first person in the United States to have a PIB study of her brain.
“I’m very anxious to get to the bottom of this whole Alzheimer’s thing,” she said.
Nothing Left to Give
In an interview in the summer of 2006, Ms. Kerley described her mother this way: “She’s completely withdrawn in herself. She hasn’t recognized us for a few years. Basically she hums one line of one song over and over again. She seems to be stuck somewhere in her life between age 4 and 5.”
Ms. Kerley said she and her son Michael, then 21, visited every week or two.
“She loves getting her back rubbed, being smiled at, being hugged,” Ms. Kerley said. “She doesn’t know who we are. We’re going for us, not for her, because she doesn’t remember us the minute we walk out the door.”
She had signed her mother up for hospice care at the nursing home, meaning that she would receive medical care to keep her comfortable but no extraordinary measures like resuscitation if she began to fail. She said her mother would not want to be kept alive in her present condition.
“She has nothing left to give the world, and the world has nothing left to give to her,” Ms. Kerley said.
Nearly a year and a half later, her mother is still alive, even though Ms. Kerley has declined liquid nutritional supplements, antibiotics and flu and pneumonia shots.
Her mother does not even hum anymore, and spends much of her time in a fetal position, except when she is at the dinner table. She can still walk, if led.
“If my mother had her own choice, she would have offed herself a long time ago,” Ms. Kerley said. “There is no quality to her life.
“When she does go, it will be a blessing.”
Ms. Kerley has already arranged to donate her mother’s brain and her own to Washington University. She seriously doubts that she will develop Alzheimer’s. She is more like her father than her mother, she said, and she is the most educated person in her family, reads constantly and stays in shape by swing dancing two to five nights a week. And her students keep her sharp.
“If you want to keep up with me until you retire, that’s fine,” she said. “I’m betting I’m not going to have that problem.” can prevent heart disease, lowering A-beta may prevent Alzheimer’s or slow it, particularly in the early stages — provided that drugs can be created to do the job.
Older folks should beware of the potential side effects of drugs with anti-cholinergic properties.
These are commonly prescribed, but can in some patients have untoward mental status changes. Agents with anticholinergic properties are as follows:
· Anticholinergics ·
- Atropine, scopolamine
- Glycopyrrolate
- Benztropine, trihexyphenidyl
- Chlorpheniramine
- Cyproheptadine
- Doxylamine
- Hydroxyzine
- Dimenhydrinate
- Diphenhydramine
- Meclizine
- Promethazine
- Chlorpromazine
- Clozapine
- Mesoridazine
- Olanzapine
- Quetiapine
- Thioridazine
- Clidinium
- Dicyclomine
- Hyoscyamine
- Oxybutynin
- Propantheline
- Amitriptyline
- Amoxapine
- Clomipramine
- Desipramine
- Doxepin
- Imipramine
- Nortriptyline
- Protriptyline
- Cyclopentolate
- Homatropine
- Tropicamide
- Amanita muscaria (fly agaric)
- Amanita pantherina (panther mushroom)
- Arctium lappa (burdock root)
- Atropa belladonna (deadly nightshade)
- Cestrum nocturnum (night blooming jessamine)
- Datura suaveolens (angel's trumpet)
- Datura stramonium (jimson weed)
- Hyoscyamus niger (black henbane)
- Lantana camara (red sage)
- Solanum carolinensis (wild tomato)
- Solanum dulcamara (bittersweet)
- Solanum pseudocapsicum (Jerusalem cherry)
- Solanum tuberosum (potato)
- carbamazepine,
- cyclobenzaprine
- orphenadrine
DEMENTIA SCREENING QUESTIONNAIRE
If you are worried that you or a relative is developing Alzheimer's, answer the following questions. Answer "yes" if the behavior indicates a change in the last several years.
1. Problems with judgment (such as trouble making decisions, bad financial moves)
2. Less interest in hobbies or activities
3. Repeating the same things over and over (questions, stories or statements)
4. Trouble learning how to use a tool, appliance or gadget
5. Forgets correct month or year
6. Trouble handling complicated financial affairs (such as income taxes, balancing checkbook)
7. Trouble remembering appointments
8. Daily problems with thinking and/or memory
Scoring: A "yes" to none or just one question probably does not indicate any kind of dementia, although the questionnaire can't rule out very early cases. So don't hesitate to get help if you continue to be concerned. If you answer yes to two or more questions, you should seek an assessment by a specialist.
Source: Adapted from J.E. Galvin et. al., "The AD8, a Brief Informant Interview to Detect Dementia," Neurology 65 (2005): 559-64.
The Science Behind 'Senior Moments'
By Melinda Beck : WSJ Article : May 28, 2008
Of all the telltale signs of aging, the scariest are those that affect the mind. I sometimes think of one word and type another, an unsettling trait for a journalist. It's usually a word that's close to the one I want, like "of" instead of "for," or "there" instead of "their."
Turns out there's a name for this -- a literal paraphasia -- and it's just one kind of "senior moment," an unscientific term for a variety of mental glitches. Most common is the temporary inability to recall a name or a number or what you were about to do.
"We think the vast majority of these are probably benign, but many cases of Alzheimer's do start out as 'senior moments,'" says P. Murali Doraiswamy, chief of Biological Psychiatry at Duke University Medical School and co-author of "The Alzheimer's Action Plan," a new book for people who are worried.
Even in normal aging, there's a general slowing of cognitive function, starting in the 50s and 60s. Neurotransmitters, the chemicals that allow nerve cells to communicate, diminish. The brain itself shrinks. White matter -- the fiber tracks connecting the front of the brain to storage areas -- changes so that information takes longer to process. It's like a computer that freezes temporarily as it tries to call up a file.
Names and dates that take time to retrieve "generally aren't well-archived," says Dr. Doraiswamy. You may not have paid much attention to them in the first place -- especially if you were multitasking. "Your brain has an inexhaustible amount of storage, but you can't have too many programs running at the same time, or it's hard to attend to them," says Gayatri Devi, a psychiatrist and neurologist who runs the New York Memory Center. That may explain the in-one-ear-and-out-the-other phenomenon that plagues some people.
Paying attention is critical to laying down memories, which scientists now think are distributed all around the brain. What a rose looks like, smells like, the pain of the thorn and emotions attached to it are all in different parts. When you think of a rose, "it's like your frontal cortex does a Google search through every part of your brain for an association with 'rose' that's been stored," says Dr. Doraiswamy.
"The richer you can make the experience, the more memorable it is," says Dr. Devi. "If you have a fantastic evening with the best bottle of wine in a lovely setting, you'll remember that event because the trace that's created is very wide." And every time you play it back in your mind, you are physically reinforcing it.
Repetition also helps reinforce abstract things like names or numbers, as does a mnemonic association, like noting that Jane is far from plain. Such tricks are often automatic for people who pride themselves on remembering names. But it's harder if you are sleep-deprived, anxious or under stress -- like, say, a new CEO who starts to thank the chairman from the podium and suddenly blanks on his name.
It's just as important to forget extraneous things and minimize mental clutter, says Dr. Devi. You can't dump those 1960s TV jingles from long-term memory, but you can free up your short-term memory by using calendars, lists and personal-digital assistants. "Put the burden on gadgets," says Dr. Doraiswamy.
When should you be concerned about memory lapses?
In Alzheimer's, people often retain obscure old memories, but have trouble recalling recent events and conversations. Or they may forget the names of simple things. "If a person can't find their car in a six-floor garage at JFK because they forgot to look at the number, that's probably just a senior moment," says Dr. Doraiswamy. "But if they can't remember the color or make of the car they've been driving for years," that could be more serious.
Changes in behavior or mood or memory can also signal early Alzheimer's. "If you've always been a ditz, it's not so unusual if you can't remember well," says Dr. Devi. "But if you had a remarkable memory and now you can't remember things, that's more cause for concern."
Some of these distinctions are subtle -- and there's a vast middle ground of "mild cognitive impairment" in between normal aging and Alzheimer's. If you're concerned, get evaluated by a family doctor or a memory specialist, and the sooner, the better. A host of other conditions can cause memory problems -- including depression, alcohol abuse, thyroid problems, vitamin deficiencies and hormone fluctuations -- and many are treatable. If it is Alzheimer's, getting help early may be able to reduce symptoms and slow the progress of the disease.
Years Later, No Magic Bullet Against Alzheimer’s Disease
By Gina Kolata: NY Times : August 28, 2010
The scene was a kind of science court. On trial was the question “Can anything — running on a treadmill, eating more spinach, learning Arabic — prevent National Institutes of Health sponsored the court, appointing a jury of 15 medical scientists with no vested interests in Alzheimer’s research. They would hear the evidence and reach a judgment on what the data showed.
For a day and a half last spring, researchers presented their cases, describing studies and explaining what they had hoped to show. The jury also heard from scientists from Duke University who had been commissioned to look at the body of evidence — hundreds of research papers — and weigh it. And the jury members had read the papers themselves, preparing for this day.
The studies included research on nearly everything proposed to prevent the disease: exercise, mental stimulation, healthy diet, social engagement, nutritional supplements, anti-inflammatory drugs or those that lower cholesterol or blood pressure, even the idea that people who marry or stay trim might be saved from dementia. And they included research on traits that might hasten Alzheimer’s onset, like not having much of an education or being a loner.
It is an issue that has taken on intense importance because scientists recently reported compelling evidence that two types of tests, PET scans of Alzheimer’s plaque in the brain and tests of spinal fluid, can find signs of the disease years before people have symptoms. That gives rise to the question: What, if anything, can people do to prevent it?
But the jury’s verdict was depressing and distressing. So far, nothing has been found to prevent or delay this devastating disease, which ceaselessly kills brain cells, eventually leaving people mute, incontinent, unable to feed themselves, unaware of who they are or who their family and friends are.
“Currently,” the panel wrote, “no evidence of even moderate scientific quality exists to support the association of any modifiable factor (such as nutritional supplements, herbal preparations, dietary factors, prescription or nonprescription drugs, social or economic factors, medical conditions, toxins or environmental exposures) with reduced risk of Alzheimer’s disease.”
“I was surprised and, at the same time, very sad” about the lack of evidence, said Dr. Martha L. Daviglus, the panel chairwoman and a professor of preventive medicine and medicine at the Feinberg School of Medicine at Northwestern University. “This is something that could happen to any of us, and yet we are at such a primitive state of research.”
She said, “In the end, we concluded that the evidence is the evidence and we have to say what it is.”
The state of the evidence reflects in part the long time it took before researchers even realized that Alzheimer’s was a disease, said Dr. Richard J. Hodes, director of the National Institute on Aging. Until the mid-1980s, many thought dementia was a normal part of aging, and so serious studies of its causes and prevention did not really begin until then. Scientists have spent the years since searching for factors that might affect risk, checking data from other studies to see if, for example, diet or blood pressure or years of education might be associated with the disease.
In the meantime, doctors are in a bind. Should they tell people to do things like walk briskly or eat vegetables — activities that might someday be shown to protect against Alzheimer’s and that certainly cannot hurt? Or should they wait for absolute proof, confirmation that a diet or a drug or an exercise regimen prevents Alzheimer’s?
The Alzheimer’s Association tells people to exercise, challenge themselves mentally, remain socially engaged and keep their hearts healthy. Such measures can only help, says Dr. Maria C. Carrillo, a senior director of the organization.
But, she said, “The Alzheimer’s Association certainly agrees that there is not enough evidence to say anything definitive about the prevention of Alzheimer’s disease and any kind of intervention.”
Of course, Dr. Hodes said, there are many reasons to follow practices to improve general health. But, he said, researchers have to be careful about implying that any measures will protect against this degenerative brain disease.
“We don’t know that yet,” Dr. Hodes said.
Rating the Quality
Dr. John W. Williams Jr., head of the Duke group that evaluated the studies, thought the task would not be too arduous. He expected relatively few studies and clear results.
To its great surprise, the Duke group discovered a vast amount of literature on Alzheimer’s prevention. Instead of coming up empty on many topics, Dr. Williams said, “We came up empty on very few.”
The problem, the group wrote, was that “the quality of the evidence was typically low.”
Most studies observed people who happened to use or not use a possible preventive measure and then determined whether they got Alzheimer’s or not.
Such studies, known as observational ones, are not the gold standard, like those in which people are randomly assigned to take a pill or do something like exercise, or not. Observational studies are useful in generating hypotheses but are not proof. Still, if several well-done studies of this type come to the same conclusion, they can be valuable evidence.
In the case of Alzheimer’s prevention, though, the studies tended to have problems, Dr. Williams said.
Often it was not clear precisely what subjects were doing. They might have been using a drug or a supplement at the start of the study but the dose was not specified, nor was it clear whether subjects were taking the same doses, or for how long.
Some studies of drugs to lower blood pressure used self-reports as opposed to, for example, pharmacy data. A 12-year study asked participants about their use of cholesterol-lowering statins at the start of the study but never did again. A nine-year statin study used pharmacy records but included as users those who took the drugs at any time during the study period.
Definitions of conditions, like high blood pressure, tended to vary from study to study.
Descriptions of factors like “strong social support” were vague or idiosyncratic. For example, some studies classified married people as having strong social support for that reason alone, with no evaluation of whether the marriage was good or bad.
Often, there were vague assessments of Alzheimer’s disease. And often studies did not take into account other differences among subjects, like age or family history of Alzheimer’s, that might have independently led some to get the disease and others not.
Looking over the piles of studies, the group rated evidence as high, moderate or low, depending on how confident they were in the findings.
Low confidence did not necessarily mean the measures did not work — it meant the evidence was so faulty that there was no way of deciding.
In the end, it said it was highly confident in the findings for just one thing, the herb ginkgo biloba. But in that case the evidence pointed in only one direction: it did not prevent Alzheimer’s.
Moderate evidence, not totally convincing but not worthless, applied to only four factors studied.
Two were factors that increased risk. They were a particular gene, ApoE4, which, moderate evidence showed, increased risk about threefold, and menopause therapy with a combination of estrogens and progestins, which doubled risk.
The other moderate evidence indicated that certain things that had been hoped to be protective were not. For instance, there was moderate evidence that vitamin E, found in nuts, vegetable oils, green leafy vegetables and fortified cereals, had no effect on risk. There was also moderate evidence that cholinesterase inhibitors, drugs often used to treat Alzheimer’s symptoms, had no effect.
Other than that, evidence was poor.
There is only poor evidence, for example, that keeping your brain active, having a high level of education or exercising has a protective effect. There is also only poor evidence that eating a Mediterranean diet — high in fruits and vegetables, fish and olive oil — will help stave off Alzheimer’s.
There is only poor evidence that having poor social support or smoking increases risk.
In a way, it is not surprising that many thought the evidence was stronger than it was, says Dr. James R. Burke, a member of the Duke group and director of the Memory Disorders Clinic at Duke.
“You remember the positive studies,” Dr. Burke said. “The ones that are more marginal, you tend to put them out of your mind.”
And many things thought to protect against Alzheimer’s — a healthy diet, vigorous exercise and an active brain — just seem to be common sense. The science jury said it was still possible that those measures might be found to help and urged that better quality studies be done.
But that may not be so easy if studies have to follow people until they get the disease. Alzheimer’s seems to progress silently in the brain for a decade before the earliest symptoms of memory problems surface. It can take another decade until the distinctive signs of Alzheimer’s appear: profound memory loss and an inability to handle the normal activities of daily life like bathing and dressing.
“Once there is even minimal cognitive impairment, the brain is damaged, inflamed, burning like a bonfire,” said Dr. Caleb Finch, director of the Gerontology Research Institute at the University of Southern California.
As a result, high-quality studies of possible factors like diet and exercise or mental stimulation before the disease’s onset might have to last for decades.
In the meantime, patients, like those at Dr. Burke’s Memory Disorders Clinic, and their frightened family members want advice about things they can do now.
He tells them to do all they can to stay healthy: keep their heart disease risk factors under control, eat a good diet, exercise. He tells them that even if good health cannot prevent Alzheimer’s, it might delay its onset.
“We don’t have compelling evidence or proof that this will prevent Alzheimer’s disease,” he says. But those measures, he adds, “would improve quality of life.”
But Dr. Williams, head of the Duke group, said it was also important to keep an open mind; the measures may or may not affect a person’s chances of getting Alzheimer’s.
“Unfortunately, in medicine,” he said, “things that are logical and make good sense don’t necessarily work out.”
The Problem, Personified
Elise Schoux of Washington is facing the prevention problem. She is 53, an age when prevention might make sense — when Alzheimer’s strikes, people usually are in their 70s and 80s — and she is watching her 70-year-old husband’s slow decline into the dread disease.
Bill Schoux’s memory had been deteriorating for years, but in July 2009, when he got the diagnosis, Mrs. Schoux was devastated.
“For two weeks, we were at a loss, we would burst into tears,” she said. “How could this be?”
Mr. Schoux had been an athlete all his life, he ate a healthy diet, he was friendly and outgoing. He had been an expert on foreign aid, traveling around the world, and had certainly had a mentally stimulating career. Mrs. Schoux is not sure how much more her husband could have done to ward off Alzheimer’s. But she wants to do everything she can to protect herself from getting it and to slow the disease in him.
So Mrs. Schoux now unfailingly goes to the gym with her husband several days a week, lifting weights and spending 30 minutes on a treadmill or an elliptical cross trainer.
Her husband always worked crossword puzzles. Now she does them, too. She and her husband have a subscription to a local theater. And they read the newspaper every day.
“It can’t hurt to keep the brain cells moving,” Mrs. Schoux said.
Mrs. Schoux also tries to eat blueberries, salmon, intensely colored fruits and dark leafy vegetables, in case that helps.
She knows that much of what she is trying is unproved but feels that it can, at worst, be harmless.
“I don’t know what the answers are,” Mrs. Schoux said. “I hope they find something. It is a seriously debilitating disease.”
By Gina Kolata: NY Times : August 28, 2010
The scene was a kind of science court. On trial was the question “Can anything — running on a treadmill, eating more spinach, learning Arabic — prevent National Institutes of Health sponsored the court, appointing a jury of 15 medical scientists with no vested interests in Alzheimer’s research. They would hear the evidence and reach a judgment on what the data showed.
For a day and a half last spring, researchers presented their cases, describing studies and explaining what they had hoped to show. The jury also heard from scientists from Duke University who had been commissioned to look at the body of evidence — hundreds of research papers — and weigh it. And the jury members had read the papers themselves, preparing for this day.
The studies included research on nearly everything proposed to prevent the disease: exercise, mental stimulation, healthy diet, social engagement, nutritional supplements, anti-inflammatory drugs or those that lower cholesterol or blood pressure, even the idea that people who marry or stay trim might be saved from dementia. And they included research on traits that might hasten Alzheimer’s onset, like not having much of an education or being a loner.
It is an issue that has taken on intense importance because scientists recently reported compelling evidence that two types of tests, PET scans of Alzheimer’s plaque in the brain and tests of spinal fluid, can find signs of the disease years before people have symptoms. That gives rise to the question: What, if anything, can people do to prevent it?
But the jury’s verdict was depressing and distressing. So far, nothing has been found to prevent or delay this devastating disease, which ceaselessly kills brain cells, eventually leaving people mute, incontinent, unable to feed themselves, unaware of who they are or who their family and friends are.
“Currently,” the panel wrote, “no evidence of even moderate scientific quality exists to support the association of any modifiable factor (such as nutritional supplements, herbal preparations, dietary factors, prescription or nonprescription drugs, social or economic factors, medical conditions, toxins or environmental exposures) with reduced risk of Alzheimer’s disease.”
“I was surprised and, at the same time, very sad” about the lack of evidence, said Dr. Martha L. Daviglus, the panel chairwoman and a professor of preventive medicine and medicine at the Feinberg School of Medicine at Northwestern University. “This is something that could happen to any of us, and yet we are at such a primitive state of research.”
She said, “In the end, we concluded that the evidence is the evidence and we have to say what it is.”
The state of the evidence reflects in part the long time it took before researchers even realized that Alzheimer’s was a disease, said Dr. Richard J. Hodes, director of the National Institute on Aging. Until the mid-1980s, many thought dementia was a normal part of aging, and so serious studies of its causes and prevention did not really begin until then. Scientists have spent the years since searching for factors that might affect risk, checking data from other studies to see if, for example, diet or blood pressure or years of education might be associated with the disease.
In the meantime, doctors are in a bind. Should they tell people to do things like walk briskly or eat vegetables — activities that might someday be shown to protect against Alzheimer’s and that certainly cannot hurt? Or should they wait for absolute proof, confirmation that a diet or a drug or an exercise regimen prevents Alzheimer’s?
The Alzheimer’s Association tells people to exercise, challenge themselves mentally, remain socially engaged and keep their hearts healthy. Such measures can only help, says Dr. Maria C. Carrillo, a senior director of the organization.
But, she said, “The Alzheimer’s Association certainly agrees that there is not enough evidence to say anything definitive about the prevention of Alzheimer’s disease and any kind of intervention.”
Of course, Dr. Hodes said, there are many reasons to follow practices to improve general health. But, he said, researchers have to be careful about implying that any measures will protect against this degenerative brain disease.
“We don’t know that yet,” Dr. Hodes said.
Rating the Quality
Dr. John W. Williams Jr., head of the Duke group that evaluated the studies, thought the task would not be too arduous. He expected relatively few studies and clear results.
To its great surprise, the Duke group discovered a vast amount of literature on Alzheimer’s prevention. Instead of coming up empty on many topics, Dr. Williams said, “We came up empty on very few.”
The problem, the group wrote, was that “the quality of the evidence was typically low.”
Most studies observed people who happened to use or not use a possible preventive measure and then determined whether they got Alzheimer’s or not.
Such studies, known as observational ones, are not the gold standard, like those in which people are randomly assigned to take a pill or do something like exercise, or not. Observational studies are useful in generating hypotheses but are not proof. Still, if several well-done studies of this type come to the same conclusion, they can be valuable evidence.
In the case of Alzheimer’s prevention, though, the studies tended to have problems, Dr. Williams said.
Often it was not clear precisely what subjects were doing. They might have been using a drug or a supplement at the start of the study but the dose was not specified, nor was it clear whether subjects were taking the same doses, or for how long.
Some studies of drugs to lower blood pressure used self-reports as opposed to, for example, pharmacy data. A 12-year study asked participants about their use of cholesterol-lowering statins at the start of the study but never did again. A nine-year statin study used pharmacy records but included as users those who took the drugs at any time during the study period.
Definitions of conditions, like high blood pressure, tended to vary from study to study.
Descriptions of factors like “strong social support” were vague or idiosyncratic. For example, some studies classified married people as having strong social support for that reason alone, with no evaluation of whether the marriage was good or bad.
Often, there were vague assessments of Alzheimer’s disease. And often studies did not take into account other differences among subjects, like age or family history of Alzheimer’s, that might have independently led some to get the disease and others not.
Looking over the piles of studies, the group rated evidence as high, moderate or low, depending on how confident they were in the findings.
Low confidence did not necessarily mean the measures did not work — it meant the evidence was so faulty that there was no way of deciding.
In the end, it said it was highly confident in the findings for just one thing, the herb ginkgo biloba. But in that case the evidence pointed in only one direction: it did not prevent Alzheimer’s.
Moderate evidence, not totally convincing but not worthless, applied to only four factors studied.
Two were factors that increased risk. They were a particular gene, ApoE4, which, moderate evidence showed, increased risk about threefold, and menopause therapy with a combination of estrogens and progestins, which doubled risk.
The other moderate evidence indicated that certain things that had been hoped to be protective were not. For instance, there was moderate evidence that vitamin E, found in nuts, vegetable oils, green leafy vegetables and fortified cereals, had no effect on risk. There was also moderate evidence that cholinesterase inhibitors, drugs often used to treat Alzheimer’s symptoms, had no effect.
Other than that, evidence was poor.
There is only poor evidence, for example, that keeping your brain active, having a high level of education or exercising has a protective effect. There is also only poor evidence that eating a Mediterranean diet — high in fruits and vegetables, fish and olive oil — will help stave off Alzheimer’s.
There is only poor evidence that having poor social support or smoking increases risk.
In a way, it is not surprising that many thought the evidence was stronger than it was, says Dr. James R. Burke, a member of the Duke group and director of the Memory Disorders Clinic at Duke.
“You remember the positive studies,” Dr. Burke said. “The ones that are more marginal, you tend to put them out of your mind.”
And many things thought to protect against Alzheimer’s — a healthy diet, vigorous exercise and an active brain — just seem to be common sense. The science jury said it was still possible that those measures might be found to help and urged that better quality studies be done.
But that may not be so easy if studies have to follow people until they get the disease. Alzheimer’s seems to progress silently in the brain for a decade before the earliest symptoms of memory problems surface. It can take another decade until the distinctive signs of Alzheimer’s appear: profound memory loss and an inability to handle the normal activities of daily life like bathing and dressing.
“Once there is even minimal cognitive impairment, the brain is damaged, inflamed, burning like a bonfire,” said Dr. Caleb Finch, director of the Gerontology Research Institute at the University of Southern California.
As a result, high-quality studies of possible factors like diet and exercise or mental stimulation before the disease’s onset might have to last for decades.
In the meantime, patients, like those at Dr. Burke’s Memory Disorders Clinic, and their frightened family members want advice about things they can do now.
He tells them to do all they can to stay healthy: keep their heart disease risk factors under control, eat a good diet, exercise. He tells them that even if good health cannot prevent Alzheimer’s, it might delay its onset.
“We don’t have compelling evidence or proof that this will prevent Alzheimer’s disease,” he says. But those measures, he adds, “would improve quality of life.”
But Dr. Williams, head of the Duke group, said it was also important to keep an open mind; the measures may or may not affect a person’s chances of getting Alzheimer’s.
“Unfortunately, in medicine,” he said, “things that are logical and make good sense don’t necessarily work out.”
The Problem, Personified
Elise Schoux of Washington is facing the prevention problem. She is 53, an age when prevention might make sense — when Alzheimer’s strikes, people usually are in their 70s and 80s — and she is watching her 70-year-old husband’s slow decline into the dread disease.
Bill Schoux’s memory had been deteriorating for years, but in July 2009, when he got the diagnosis, Mrs. Schoux was devastated.
“For two weeks, we were at a loss, we would burst into tears,” she said. “How could this be?”
Mr. Schoux had been an athlete all his life, he ate a healthy diet, he was friendly and outgoing. He had been an expert on foreign aid, traveling around the world, and had certainly had a mentally stimulating career. Mrs. Schoux is not sure how much more her husband could have done to ward off Alzheimer’s. But she wants to do everything she can to protect herself from getting it and to slow the disease in him.
So Mrs. Schoux now unfailingly goes to the gym with her husband several days a week, lifting weights and spending 30 minutes on a treadmill or an elliptical cross trainer.
Her husband always worked crossword puzzles. Now she does them, too. She and her husband have a subscription to a local theater. And they read the newspaper every day.
“It can’t hurt to keep the brain cells moving,” Mrs. Schoux said.
Mrs. Schoux also tries to eat blueberries, salmon, intensely colored fruits and dark leafy vegetables, in case that helps.
She knows that much of what she is trying is unproved but feels that it can, at worst, be harmless.
“I don’t know what the answers are,” Mrs. Schoux said. “I hope they find something. It is a seriously debilitating disease.”
Making Homes Safer for Dementia Patients
By Dale Russakoff : NY Times Article : July 19, 2010
Just about everyone with an older parent living alone worries about falls, and there is no shortage of suggestions for how to elder-proof a home in order to minimize trips and slips. But experts say it is also important to minimize household dangers for people with dementia and Alzheimer’s disease.
The Visiting Nurse Service of New York, which sends caregivers to 38,000 mostly elderly patients a day, has come up with a list of tips for adapting homes for dementia patients. It was complied by Cathy Castronova, a registered nurse and case manager with the service’s affiliate, Partners in Care, who assesses the homes of older people for safety and has taught numerous classes on helping seniors remain safe at home.
“There are a lot of safety issues for people who are not oriented,” said Ms. Castronova. “A lot of times they’ll come to your attention when they’re going home from a hospital stay, and you’ll assess the home and say to yourself, ‘She’s been living alone like this all this time? With a gas stove? What if she caught the knob on her pocket and turned it on by accident?’”
(Her tip for gas stoves, which did not make the top 15, is to disable the gas and switch to a microwave or toaster oven.)
Here are her suggestions:
1. Create a “wander loop” in your home, a safe pathway that allows the patient to safely roam.
2. Use reflector tape to create a path to the bathroom.
3. Cover radiators and electrical outlets with guards.
4. Lock doors that lead to places like basements and garages.
5. Lock cabinets that contain liquor, medications, household chemicals and any other toxic substances that could be swallowed.
6. Get rid of firearms, or store them in a locked cabinet with bullets in a separate locked cabinet.
7. Install safety locks and alarms on exit doors and gates.
8. Cover smooth or shiny surfaces to reduce confusing glare.
9. Eliminate shadows with a lamp that reflects off the ceiling.
10. Cover or remove mirrors if they are upsetting to a person with hallucinations.
11. Store car keys in a locked container; disable the car.
12. Do not allow unattended smoking.
13. Make sure an I.D. bracelet is being worn at all times.
14. When selecting home care, make sure to hire an aide who has been trained to deal with dementia and Alzheimer’s patients, and is under the supervision of a skilled home care nurse.
15. And, most importantly, constantly re-assess your parent’s abilities with the help of a nurse or physician.
By Dale Russakoff : NY Times Article : July 19, 2010
Just about everyone with an older parent living alone worries about falls, and there is no shortage of suggestions for how to elder-proof a home in order to minimize trips and slips. But experts say it is also important to minimize household dangers for people with dementia and Alzheimer’s disease.
The Visiting Nurse Service of New York, which sends caregivers to 38,000 mostly elderly patients a day, has come up with a list of tips for adapting homes for dementia patients. It was complied by Cathy Castronova, a registered nurse and case manager with the service’s affiliate, Partners in Care, who assesses the homes of older people for safety and has taught numerous classes on helping seniors remain safe at home.
“There are a lot of safety issues for people who are not oriented,” said Ms. Castronova. “A lot of times they’ll come to your attention when they’re going home from a hospital stay, and you’ll assess the home and say to yourself, ‘She’s been living alone like this all this time? With a gas stove? What if she caught the knob on her pocket and turned it on by accident?’”
(Her tip for gas stoves, which did not make the top 15, is to disable the gas and switch to a microwave or toaster oven.)
Here are her suggestions:
1. Create a “wander loop” in your home, a safe pathway that allows the patient to safely roam.
2. Use reflector tape to create a path to the bathroom.
3. Cover radiators and electrical outlets with guards.
4. Lock doors that lead to places like basements and garages.
5. Lock cabinets that contain liquor, medications, household chemicals and any other toxic substances that could be swallowed.
6. Get rid of firearms, or store them in a locked cabinet with bullets in a separate locked cabinet.
7. Install safety locks and alarms on exit doors and gates.
8. Cover smooth or shiny surfaces to reduce confusing glare.
9. Eliminate shadows with a lamp that reflects off the ceiling.
10. Cover or remove mirrors if they are upsetting to a person with hallucinations.
11. Store car keys in a locked container; disable the car.
12. Do not allow unattended smoking.
13. Make sure an I.D. bracelet is being worn at all times.
14. When selecting home care, make sure to hire an aide who has been trained to deal with dementia and Alzheimer’s patients, and is under the supervision of a skilled home care nurse.
15. And, most importantly, constantly re-assess your parent’s abilities with the help of a nurse or physician.
The faces of Alzheimer's Disease
New guidelines call for diagnosing early Alzheimer’s Disease
By Rob Stein : Washington Post : April 19, 2011
U.S. health authorities recommended Tuesday that doctors diagnose the risk of developing Alzheimer’s disease before people develop full-blown dementia.
The National Institutes of Health and the Alzheimer’s Association made the recommendation, which could at least double the number of Americans receiving a diagnosis of Alzheimer’s and its early phases. It is the first revision of the guidelines for diagnosing the brain disease in 27 years.
In addition to updating the criteria for diagnosing full Alzheimer’s, the health authorities created two new categories of the illness: a “preclinical” phase that occurs before patients show any memory loss or other thinking problems, and “mild cognitive impairment,” in which symptoms are subtle.
The recommendations are based on the growing realization that Alzheimer’s is the result of a gradual destruction of brain cells that control memory and other cognitive abilities, a process that begins years before clear-cut dementia becomes apparent.
“The new guidelines reflect today’s understanding of how key changes in the brain lead to Alzheimer’s disease,” Creighton Phelps of the NIH’s National Institute on Aging told reporters during a briefing held Monday before the guidelines were released.
The recommendations are aimed at helping patients and their families prepare financially, logistically and emotionally for the disease, which can require years of intensive, expensive care.
“For many people, it is important to them to know to make plans to be able to discuss with their family at a point when they are still able to make decisions for themselves,” said Reisa A. Sperling of Harvard’s medical school, who helped develop the guidelines. “And for many people, it will put their mind at ease, even if it is the case that we will say one day that yes, this looks like Alzheimer’s may be beginning in your brain.”
Officials also hope the guidelines will identify more patients in the early stages of the disease who could volunteer for studies testing experimental drugs that could delay the disease, in addition to blood tests, brain scans and spinal taps that could use “biological markers” to provide more definitive diagnoses.
“Ultimately, it may be that we will try these drugs in people before they have symptoms but have evidence of Alzheimer’s in their brain, just as right now we try to lower cholesterol or treat diabetes before there are symptoms,” Sperling said.
About 5.4 million Americans have Alzheimer’s, which robs people of their memory and other thinking abilities. It often dramatically changes personalities and eventually renders those with the disease confused and unable to care for themselves or to recognize their loved ones.
As the population ages, Alzheimer’s is becoming more common, raising fears about getting the disease and increasing frustration about the dearth of ways to diagnose and treat it. That has intensified the urgency of developing better ways to identify it, distinguish it from other forms of dementia and find ways to treat it, or at least delay symptoms.
Although several drugs have been approved to treat the symptoms of the disease, none are very effective. Experimental medications are being developed to alleviate symptoms and delay the progression, which many experts think is the most promising way to fight the disease.
Alzheimer’s is diagnosed through interviewing patients and family members. Doctors also conduct tests to exclude other causes, such as brain tumors, strokes and side effects of medications. A conclusive diagnosis comes from an examination of brain tissue after death.
Several experimental tests have shown promise for providing a more definitive diagnosis. They include scans that look for telltale buildups of plaque in the brain that damage cells, and spinal cord fluid and blood tests that can identify substances that play a role in creating those plaques.
Experts stressed that more research is needed to validate those tests before they are used outside carefully designed studies, which can only occur if more people receive diagnoses in the early stages so they can volunteer.
Some experts said they fear the recommendations might be misinterpreted by some patients, family members and doctors to mean that the experimental biomarker tests are ready for widespread use.
“At this point, we don’t know enough to be able to advise patients properly about what their risk for later dementia might be,” said John C. Morris of the Washington University School of Medicine in St. Louis. “Even if we do determine what that risk might be, we don’t have treatment to reduce that risk. It will raise a lot of concern.”
The recommendations are based on two years of study by four groups of experts organized by the NIH and the Alzheimer’s Association, which described their conclusions and recommendations in four papers being published in the journal Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
The hope is that Alzheimer’s will become more like heart disease, in which patients at increased risk can be identified early, just as patients at risk of heart attacks and strokes can be identified through cholesterol and blood pressure tests.
“The new criteria are really extending the range of our ability to investigate this disease and eventually find the treatments that will be so necessary to avoid the epidemic of Alzheimer’s disease that we see facing us,” said William Thies of the Alzheimer’s Association.
By Rob Stein : Washington Post : April 19, 2011
U.S. health authorities recommended Tuesday that doctors diagnose the risk of developing Alzheimer’s disease before people develop full-blown dementia.
The National Institutes of Health and the Alzheimer’s Association made the recommendation, which could at least double the number of Americans receiving a diagnosis of Alzheimer’s and its early phases. It is the first revision of the guidelines for diagnosing the brain disease in 27 years.
In addition to updating the criteria for diagnosing full Alzheimer’s, the health authorities created two new categories of the illness: a “preclinical” phase that occurs before patients show any memory loss or other thinking problems, and “mild cognitive impairment,” in which symptoms are subtle.
The recommendations are based on the growing realization that Alzheimer’s is the result of a gradual destruction of brain cells that control memory and other cognitive abilities, a process that begins years before clear-cut dementia becomes apparent.
“The new guidelines reflect today’s understanding of how key changes in the brain lead to Alzheimer’s disease,” Creighton Phelps of the NIH’s National Institute on Aging told reporters during a briefing held Monday before the guidelines were released.
The recommendations are aimed at helping patients and their families prepare financially, logistically and emotionally for the disease, which can require years of intensive, expensive care.
“For many people, it is important to them to know to make plans to be able to discuss with their family at a point when they are still able to make decisions for themselves,” said Reisa A. Sperling of Harvard’s medical school, who helped develop the guidelines. “And for many people, it will put their mind at ease, even if it is the case that we will say one day that yes, this looks like Alzheimer’s may be beginning in your brain.”
Officials also hope the guidelines will identify more patients in the early stages of the disease who could volunteer for studies testing experimental drugs that could delay the disease, in addition to blood tests, brain scans and spinal taps that could use “biological markers” to provide more definitive diagnoses.
“Ultimately, it may be that we will try these drugs in people before they have symptoms but have evidence of Alzheimer’s in their brain, just as right now we try to lower cholesterol or treat diabetes before there are symptoms,” Sperling said.
About 5.4 million Americans have Alzheimer’s, which robs people of their memory and other thinking abilities. It often dramatically changes personalities and eventually renders those with the disease confused and unable to care for themselves or to recognize their loved ones.
As the population ages, Alzheimer’s is becoming more common, raising fears about getting the disease and increasing frustration about the dearth of ways to diagnose and treat it. That has intensified the urgency of developing better ways to identify it, distinguish it from other forms of dementia and find ways to treat it, or at least delay symptoms.
Although several drugs have been approved to treat the symptoms of the disease, none are very effective. Experimental medications are being developed to alleviate symptoms and delay the progression, which many experts think is the most promising way to fight the disease.
Alzheimer’s is diagnosed through interviewing patients and family members. Doctors also conduct tests to exclude other causes, such as brain tumors, strokes and side effects of medications. A conclusive diagnosis comes from an examination of brain tissue after death.
Several experimental tests have shown promise for providing a more definitive diagnosis. They include scans that look for telltale buildups of plaque in the brain that damage cells, and spinal cord fluid and blood tests that can identify substances that play a role in creating those plaques.
Experts stressed that more research is needed to validate those tests before they are used outside carefully designed studies, which can only occur if more people receive diagnoses in the early stages so they can volunteer.
Some experts said they fear the recommendations might be misinterpreted by some patients, family members and doctors to mean that the experimental biomarker tests are ready for widespread use.
“At this point, we don’t know enough to be able to advise patients properly about what their risk for later dementia might be,” said John C. Morris of the Washington University School of Medicine in St. Louis. “Even if we do determine what that risk might be, we don’t have treatment to reduce that risk. It will raise a lot of concern.”
The recommendations are based on two years of study by four groups of experts organized by the NIH and the Alzheimer’s Association, which described their conclusions and recommendations in four papers being published in the journal Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association.
The hope is that Alzheimer’s will become more like heart disease, in which patients at increased risk can be identified early, just as patients at risk of heart attacks and strokes can be identified through cholesterol and blood pressure tests.
“The new criteria are really extending the range of our ability to investigate this disease and eventually find the treatments that will be so necessary to avoid the epidemic of Alzheimer’s disease that we see facing us,” said William Thies of the Alzheimer’s Association.
Detective Work:
The False Alzheimer's Diagnosis
Melinda Beck : WSJ : August 27, 2012
Family members of J.D. "Jasper" Cain suspected he had Alzheimer's disease as they watched the once fun-loving father and husband struggle with memory and movement. Three doctors thought he had Parkinson's disease and kept raising his medication dose when he didn't improve.
At his daughter's suggestion, Mr. Cain, of Bedford, Ind., saw a neurologist last year who did an MRI, then a spinal tap. He found that Mr. Cain had a buildup of fluid in the brain called normal pressure hydrocephalus. The fluid was drained with a surgically implanted shunt. Now, 13 years after his symptoms began Mr. Cain, 70, is walking, joking and matching wits with TV's "Jeopardy" again. "It was just like getting my life back," he says.
Alzheimer's symptoms such as confusion, memory loss and personality changes also can be side effects from medication—even commonly used drugs. For example, the entire class of anticholinergic drugs, which includes many antihistamines, antianxiety drugs, muscle relaxants and sleeping pills, block the brain chemical acetylcholine, which sends signals in the nervous system. It is the same chemical that many Alzheimer's medications boost. Cholesterol-reducing statins have also been linked to brain fog in some people.
In many cases, the cognitive symptoms vanish when medication is stopped. "I have had people referred to me with a clear history of dementia and when I started to peel back the medications, they were much better," says Gary Kennedy, chief of geriatric psychiatry at Montefiore Medical Center in the Bronx, N.Y.
It isn't just primary-care physicians who may miss underlying conditions. "Every Alzheimer's expert living today has been fooled," says P. Murali Doraiswamy, chief of biological psychiatry at Duke University Medical Center in Durham, N.C.
Autopsy studies of nearly 1,000 dementia patients at 30 top centers supported by the National Institute on Aging from 2005 to 2010 found that between 17% and 30% of those diagnosed with Alzheimer's disease had been misdiagnosed and had other conditions. The study, published in the Journal of Neuropathology and Experimental Neurology in April, also found nearly 40% of patients not diagnosed with Alzheimer's during their lifetimes had evidence of Alzheimer's when autopsied.
Traditionally, Alzheimer's disease, whose main symptoms include memory loss, confusion and changes in personality or mood, could only be definitively diagnosed when an autopsy revealed the telltale amyloid plaques and tangles in the brain. But a new form of PET scan can spot such amyloid buildup in the living.
A positive test can't confirm Alzheimer's, because some people have amyloid plaques and never develop Alzheimer's. But a negative PET scan can rule out Alzheimer's and spur physicians to search for other explanations. An amyloid PET scan costs about $4,000; Medicare and private insurers have not decided whether to cover it.
Exposure to high levels of iron, lead and copper can also cause Alzheimer's-like symptoms. Heavy alcohol consumption for long periods can deplete levels of thiamine, impairing brain function, a condition called Wernicke-Korsakoff syndrome.
Urinary tract infections can cause delirium that is often confused with dementia; symptoms usually resolve after a course of antibiotics. The herpes simplex virus type 1 can home in on the brain and damage the hippocampus, causing acute memory loss, even long after the acute phases of the infection have passed. Why it occurs in some people with herpes but not others remains a mystery.
Meds that Mimic Alzheimer's
Over 100 different drugs have side effects that can mimic Alzheimer's in some people. Among the most common:
Depression is also sometimes confused with Alzheimer's. One way to distinguish between them is by patients' responses to cognition tests, Dr. Kennedy says. "If a person with Alzheimer's disease doesn't know an answer, they'll fabricate one—they still try to please you. A person who is depressed is more likely to say, 'I can't do that,' " he says. Frequently, patients have both Alzheimer's and depression. Studies by the National Institute on Aging have found people who develop depression late in life are at high risk for developing Alzheimer's for reasons not well understood.
There is mounting evidence that some cognitive problems may be due to blockages in tiny blood vessels in the brain known as "silent emboli." A study in the American Journal of Psychiatry in March found 43% of Alzheimer's patients had these emboli—and their cognitive function deteriorated twice as fast as those that didn't have them. High blood pressure, high cholesterol and diabetes all raise the risk for such silent emboli, as do many common surgical procedures. The damage they cause can't be reversed but experts say reducing risk factors may prevent further harm.
The buildup of fluid in the brain that Mr. Cain suffered may be more common than previously suspected. A 2007 study of 147 nursing-home residents estimated that 9% to 14% met the criteria for normal pressure hydrocephalus.
Typically, the cerebrospinal fluid that bathes and protects the brain is absorbed and replenished constantly. In NPH, it accumulates, putting pressure on the brain and causing memory loss, difficulty walking and often incontinence. The enlarged ventricles can be seen on an MRI, but to confirm the diagnosis, doctors withdraw fluid with a spinal tap to see if the patient's symptoms improve. If they do, a surgically implanted shunt that drains excess fluid from the brain into the abdomen can bring a significant improvement.
"I've seen patients go from about to enter a nursing home to playing golf again and traveling," says Joseph Zabramski, a neurosurgeon at the Barrow Neurological Institute in Phoenix.
Like Mr. Cain, Alicia Harper, 78, of Longwood, Fla., suffered from the severe confusion, forgetfulness and difficulty walking characteristic of NPH. After a shunt was surgically implanted three years ago, "We go to church. She can play the piano, it's amazing," says her husband, Nildo Harper. "I don't remember much of this—and I'm thankful I don't remember," Mrs. Harper adds.
NPH experts stress it is important to confirm the diagnosis with a spinal tap before surgery. "We don't want to raise false hopes—it's not a large percentage of Alzheimer's patients who have NPH," says Mark Luciano, a neurosurgeon at Cleveland Clinic. "But the idea that there may be even a small percentage of patients who have the potential to be dramatically improved with a shunt is amazing—if we can find them."
The False Alzheimer's Diagnosis
Melinda Beck : WSJ : August 27, 2012
Family members of J.D. "Jasper" Cain suspected he had Alzheimer's disease as they watched the once fun-loving father and husband struggle with memory and movement. Three doctors thought he had Parkinson's disease and kept raising his medication dose when he didn't improve.
At his daughter's suggestion, Mr. Cain, of Bedford, Ind., saw a neurologist last year who did an MRI, then a spinal tap. He found that Mr. Cain had a buildup of fluid in the brain called normal pressure hydrocephalus. The fluid was drained with a surgically implanted shunt. Now, 13 years after his symptoms began Mr. Cain, 70, is walking, joking and matching wits with TV's "Jeopardy" again. "It was just like getting my life back," he says.
Alzheimer's symptoms such as confusion, memory loss and personality changes also can be side effects from medication—even commonly used drugs. For example, the entire class of anticholinergic drugs, which includes many antihistamines, antianxiety drugs, muscle relaxants and sleeping pills, block the brain chemical acetylcholine, which sends signals in the nervous system. It is the same chemical that many Alzheimer's medications boost. Cholesterol-reducing statins have also been linked to brain fog in some people.
In many cases, the cognitive symptoms vanish when medication is stopped. "I have had people referred to me with a clear history of dementia and when I started to peel back the medications, they were much better," says Gary Kennedy, chief of geriatric psychiatry at Montefiore Medical Center in the Bronx, N.Y.
It isn't just primary-care physicians who may miss underlying conditions. "Every Alzheimer's expert living today has been fooled," says P. Murali Doraiswamy, chief of biological psychiatry at Duke University Medical Center in Durham, N.C.
Autopsy studies of nearly 1,000 dementia patients at 30 top centers supported by the National Institute on Aging from 2005 to 2010 found that between 17% and 30% of those diagnosed with Alzheimer's disease had been misdiagnosed and had other conditions. The study, published in the Journal of Neuropathology and Experimental Neurology in April, also found nearly 40% of patients not diagnosed with Alzheimer's during their lifetimes had evidence of Alzheimer's when autopsied.
Traditionally, Alzheimer's disease, whose main symptoms include memory loss, confusion and changes in personality or mood, could only be definitively diagnosed when an autopsy revealed the telltale amyloid plaques and tangles in the brain. But a new form of PET scan can spot such amyloid buildup in the living.
A positive test can't confirm Alzheimer's, because some people have amyloid plaques and never develop Alzheimer's. But a negative PET scan can rule out Alzheimer's and spur physicians to search for other explanations. An amyloid PET scan costs about $4,000; Medicare and private insurers have not decided whether to cover it.
Exposure to high levels of iron, lead and copper can also cause Alzheimer's-like symptoms. Heavy alcohol consumption for long periods can deplete levels of thiamine, impairing brain function, a condition called Wernicke-Korsakoff syndrome.
Urinary tract infections can cause delirium that is often confused with dementia; symptoms usually resolve after a course of antibiotics. The herpes simplex virus type 1 can home in on the brain and damage the hippocampus, causing acute memory loss, even long after the acute phases of the infection have passed. Why it occurs in some people with herpes but not others remains a mystery.
Meds that Mimic Alzheimer's
Over 100 different drugs have side effects that can mimic Alzheimer's in some people. Among the most common:
- Antihistimatines (Benadryl, diphenhydramine)
- Sleeping pills (Ambien, Sonata)
- Painkillers (Darvon, Toradol, Demerol, Naproxen, Aleve)
- Anti-anxiety drugs (Valium, Librium, Halcion, Xanax)
- Anti-psychotic drugs (Risperdal, Seroquel, Zyprexa)
- Cholesterol drugs (Lipitor and other statins)
- Older antidepressants (Elavil, Miltown, Tofranil)
- Incontinence drugs (Detrol, Ditropan, Toviaz)
- Acid-reflux drugs (Zantac)
- Blood pressure drugs (Procardia, Adalat)
- Tranquilizers (Serentil, Thorazine, Mellaril)
- Heart drugs (Norpace, Lanoxin, Aldoril, Vasodilan, Cardura, Aldomet)
- Stomach drugs (Bentyl, Levsin, Donnatal, Librax)
- Parkinson's drugs (benztropine, trihexyphenidyl)
Depression is also sometimes confused with Alzheimer's. One way to distinguish between them is by patients' responses to cognition tests, Dr. Kennedy says. "If a person with Alzheimer's disease doesn't know an answer, they'll fabricate one—they still try to please you. A person who is depressed is more likely to say, 'I can't do that,' " he says. Frequently, patients have both Alzheimer's and depression. Studies by the National Institute on Aging have found people who develop depression late in life are at high risk for developing Alzheimer's for reasons not well understood.
There is mounting evidence that some cognitive problems may be due to blockages in tiny blood vessels in the brain known as "silent emboli." A study in the American Journal of Psychiatry in March found 43% of Alzheimer's patients had these emboli—and their cognitive function deteriorated twice as fast as those that didn't have them. High blood pressure, high cholesterol and diabetes all raise the risk for such silent emboli, as do many common surgical procedures. The damage they cause can't be reversed but experts say reducing risk factors may prevent further harm.
The buildup of fluid in the brain that Mr. Cain suffered may be more common than previously suspected. A 2007 study of 147 nursing-home residents estimated that 9% to 14% met the criteria for normal pressure hydrocephalus.
Typically, the cerebrospinal fluid that bathes and protects the brain is absorbed and replenished constantly. In NPH, it accumulates, putting pressure on the brain and causing memory loss, difficulty walking and often incontinence. The enlarged ventricles can be seen on an MRI, but to confirm the diagnosis, doctors withdraw fluid with a spinal tap to see if the patient's symptoms improve. If they do, a surgically implanted shunt that drains excess fluid from the brain into the abdomen can bring a significant improvement.
"I've seen patients go from about to enter a nursing home to playing golf again and traveling," says Joseph Zabramski, a neurosurgeon at the Barrow Neurological Institute in Phoenix.
Like Mr. Cain, Alicia Harper, 78, of Longwood, Fla., suffered from the severe confusion, forgetfulness and difficulty walking characteristic of NPH. After a shunt was surgically implanted three years ago, "We go to church. She can play the piano, it's amazing," says her husband, Nildo Harper. "I don't remember much of this—and I'm thankful I don't remember," Mrs. Harper adds.
NPH experts stress it is important to confirm the diagnosis with a spinal tap before surgery. "We don't want to raise false hopes—it's not a large percentage of Alzheimer's patients who have NPH," says Mark Luciano, a neurosurgeon at Cleveland Clinic. "But the idea that there may be even a small percentage of patients who have the potential to be dramatically improved with a shunt is amazing—if we can find them."
Coping With Mild Cognitive Impairment
By Judith Graham : NY Times September 10, 2012
About 10 to 15 percent of adults age 65 and older are believed to have mild cognitive impairment -- a condition commonly characterized by memory problems, well beyond those associated with normal aging.
Alarmingly, mild cognitive impairment, or M.C.I., can signal serious problems ahead: About half of people with this condition go on to a diagnosis of Alzheimer's disease or another dementia within five years.
Yet when researchers from the University of Toronto searched worldwide for programs that educate people about M.C.I. and how to adapt to it, they found only five -- three in Canada, one in Germany and one in Rochester, Minn., home to the Mayo Clinic, which first defined M.C.I. in 1999. Similarly, a North American search for support groups for people with M.C.I. turned up just a handful.
The University of Toronto researchers set out to rectify this lack of attention by writing "Living With Mild Cognitive Impairment," published recently by Oxford University Press. One of its authors, Nicole Anderson, an associate professor of psychiatry at the University of Toronto, spoke with me at length, and our conversation has been edited for clarity and length.
Q.
There's some confusion about mild cognitive impairment. Is it the earliest stage of dementia or something else?
A.
Most often, it is the earliest, preclinical stage of dementia. That means symptoms are not severe enough to meet the criteria for dementia. But pathology is developing in the brain that will likely lead to dementia.
Sometimes, however, people have other health problems that lead to an M.C.I. diagnosis, and once these are treated their cognition improves.
Q.
What cognitive functions are affected by M.C.I.?
A.
The most typical one is memory. Also common are subtle language difficulties and executive functioning deficits. This refers to an ability to multitask, switch back and forth between two tasks, or inhibit irrelevant information and stay focused on what's important.
Q.
What isn't affected?
A.
People's general knowledge. Their vocabulary. Their intellectual ability. And by definition, people with M.C.I. do not have deficits in their ability to engage in activities of daily living, such as bathing, eating or cooking.
Q.
What about work?
A.
People will still be able to work. But they might find they need to put some more supports in place. They may become more reliant on Day-Timers or need more reminders from a secretary keeping track of their schedule. And they might find it takes them longer to do complicated activities.
Q.
What changes in the brain are observed with M.C.I.?
A.
A vast majority of research has been done on people with "amnestic" M.C.I. - the kind involving memory loss. There we see shrinkage of key brain areas important for memory: the hippocampus and other areas around it in the medial temporal lobes. We can now also scan for amyloid protein in the brain, and often we will see elevated levels.
Q.
Yet high concentrations of amyloid don't always signify dementia.
A.
That brings up the whole notion of cognitive reserve. This refers to the idea that people can engage in certain activities in their lives -- getting higher levels of education, exercise, eating a healthy diet, being bilingual -- that help protect them against the clinical impact of various brain diseases, especially dementia.
Q.
How does that work?
A.
We don't know for sure, but people with larger reserves often have greater connectivity between different brain regions and use different areas of the brain to do different tasks.
Q.
Why is this important?
A.
We don't have any medications at this point to prevent or treat M.C.I. or dementia. Yet we can engage in activities that will help reduce the impact of the disease and maintain our level of functioning.
Q.
What contributes to cognitive reserve?
A.
The most studied and validated factors are education, exercise and Mediterranean-style diets. There is also some evidence that the more complex your occupation is, the less likely you are to develop dementia. And people who have larger social networks are less likely to develop dementia, especially if the social connections they have are meaningful or rewarding.
Q.
What diminishes reserve?
A.
Having a prior head injury. Having high blood pressure, diabetes, high cholesterol.
Q.
What are M.C.I. symptoms to watch out for?
A.
A. Repeatedly asking questions or making the same comments. Getting lost in a place that you're familiar with. Forgetting an important event -- say, a big meeting coming up -- when that's not something you would have done before.
Q.
Do people who come in for testing often have negative results?
A.
That is common. We see a lot of the worried well. Usually, what we detect with them is normal aging.
Q.
What is normal, when it comes to the aging brain?
A.
As we get older, our memory starts to decline, starting in our 20s. Primarily affected is the ability to get new information stored in long-term memory. How fast we think and do simple mental activities slows down. And word problems become more prevalent as we become older.
Q.
Are there other reasons older adults might have cognitive problems?
A.
Absolutely. Thyroid problems, a vitamin B12 deficiency and depression can all be involved, and it's important that all these be ruled out.
It's notable that research also shows about 25 percent of people initially diagnosed with M.C.I. turn out to be normal. That tells us we don't have a perfectly accurate way of testing for this yet.
Q.
You've said there are no medical treatments for M.C.I.
A.
True, but there are ways of elevating the levels at which a person functions so that the impact of M.C.I. will be smaller. I've mentioned several already. I'd add to those developing a good set of memory strategy habits.
Q.
Can you give some examples?
A.
There are a number of them. One, for remembering things in the future, involves regularly using a Day-Timer or a personal digital assistant. A lot of older adults just have the fridge calendar at home. It's a problem because it's at home -- it's not with them when their friend says, "Let's have lunch next week," or the doctor says, "Let's schedule a new appointment."
We really encourage people to carry a memory book with them at all times, including a section for making notes and lists, a calendar, a phone book, a to-do list and essentials like a record of their medications. It absolutely helps. There's research going on here that when you train people with profound amnesia to use devices like an iPhone they can live independently.
Another memory strategy is spaced retrieval. That involves repeating a word or phrase, then waiting a few seconds, then waiting a few more, and then waiting a few more before each repetition.
That way, you're putting what you want to remember into long-term memory and pulling it out again.
A big problem with memory is that we don't pay attention. So, what most of these strategies are doing is forcing us to pay attention. Another way to do that is to say out loud, "I'm going to go into the other room and get my book," when that's what you plan to do. Then, imagine yourself walking into the room and picking up the book. That forces you to pay attention to your intention and solidifies it in memory.
Q.
You and your co-authors are involved in a program for people with M.C.I. and their families in Toronto. What have you learned?
A.
It's hugely beneficial for people. We have eight sessions, each two hours long. In the first hour, everyone is all together and there's an educational session. The second hour, the family members go to another room where they meet with health care professionals who talk to them about diet or community resources or estate planning.
Meanwhile, the people with M.C.I. stay in the room and learn practical memory strategies. They practice them over and over again. Then they get homework during the week to implement those strategies. What we hear from people is that this helps them regain their confidence because now they're armed with ways of combating the effects of cognitive symptoms.