- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
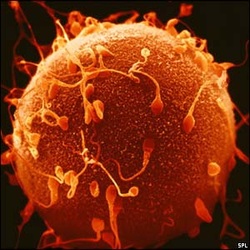
PREGNANT
or
thinking about getting pregnant?
Oversold prenatal tests
By Beth Daley : NE Center for Investigative Reporting : December 14, 2014
Stacie Chapman’s heart skipped when she answered the phone at home and her doctor — rather than a nurse — was on the line. More worrisome was the doctor’s gentle tone as she asked, “Where are you?”
On that spring day in 2013, Dr. Jayme Sloan had bad news for Chapman, who was nearly three months pregnant. Her unborn child had tested positive for Edwards syndrome, a genetic condition associated with severe birth defects. If her baby — a boy, the screening test had shown — was born alive, he probably would not live long.
Sloan explained that the test — MaterniT21 PLUS — has a 99 percent detection rate. Though Sloan offered additional testing to confirm the result, a distraught Chapman said she wanted to terminate the pregnancy immediately.
What she — and the doctor — did not understand, Chapman’s medical records indicate, was that there was a good chance her screening result was wrong. There is, it turns out, a huge and crucial difference between a test that can detect a potential problem and one reliable enough to diagnose a life-threatening condition for certain. The screening test only does the first.
Sparked by the sequencing of the human genome a decade ago, a new generation of prenatal screening tests, including MaterniT21, has exploded onto the market in the past three years. The unregulated screens claim to detect with near-perfect accuracy the risk that a fetus may have Down or Edwards syndromes, and a growing list of other chromosomal abnormalities.
Hundreds of thousands of women in early pregnancy have taken these tests — through a simple blood draw in the doctor’s office — and studies show them to perform far better than traditional blood tests and ultrasound screening.
But a three-month examination by the New England Center for Investigative Reporting has found that companies are overselling the accuracy of their tests and doing little to educate expecting parents or their doctors about the significant risks of false alarms.
Two recent industry-funded studies show that test results indicating a fetus is at high risk for a chromosomal condition can be a false alarm half of the time. And the rate of false alarms goes up the more rare the condition, such as Trisomy 13, which almost always causes death.
Companies selling the most popular of these screens do not make it clear enough to patients and doctors that the results of their tests are not reliable enough to make a diagnosis.
California-based Sequenom Inc., for instance, promises on its web page that its MaterniT21 blood test provides “simple, clear results.” Only far down below does Sequenom disclose that “no test is perfect” and that theirs can produce erroneous results “in rare cases.”
Now, evidence is building that some women are terminating pregnancies based on the screening tests alone. A recent study by another California-based testing company, Natera Inc., which offers a screen called Panorama, found that 6.2 percent of women who received test results showing their fetus at high risk for a chromosomal condition terminated pregnancies without getting a diagnostic test such as an amniocentesis.
And at Stanford University, there have been at least three cases of women aborting healthy fetuses that had received a high-risk screen result.
“The worry is women are terminating without really knowing if [the initial test result] is true or not,” said Athena Cherry, professor of pathology at the Stanford University School of Medicine, whose lab examined the cells of the healthy aborted fetuses.
In one of the three Stanford cases, the woman actually obtained a confirmatory test and was told the fetus was fine, but aborted anyway because of her faith in the screening company’s accuracy claims. “She felt it couldn’t be wrong,” Cherry said.
Companies that sell the screens stand behind their tests, saying they provide much more reliable assurance for expecting mothers than earlier screens. Some say their research focused first on how to accurately identify fetuses with potential genetic defects and only recently have they been able to get enough data to understand how often positive tests are wrong.
“The clinical performance of [noninvasive prenatal tests] has been extremely robust,” Dr. Vance Vanier, vice president of marketing for reproductive and genetic health for San Diego-based Illumina Inc., which offers the Verifi prenatal screen, wrote in an e-mail statement.
The screens are not subject to approval by the Food and Drug Administration. Because of a regulatory loophole, the companies operate free of agency oversight and the kind of independent analysis that would validate their accuracy claims. Doctors often get that information from salespeople, according to doctors themselves.
And there are other emerging concerns about the new generation of prenatal tests. Two Boston-area obstetricians, with funding from a testing company, recently sent samples from two nonpregnant women to five testing companies for analysis. Three companies returned samples indicating they came from a woman who was carrying a healthy female fetus.
Meanwhile, there are a growing number of cases emerging of women told their screen shows virtually no chance of a fetus having a problem but who then deliver a child with a genetic condition.
“My son lived for four days,’’ said Belinda Boydston, a web/graphic designer in Chandler, Ariz., whose son was born with Edwards syndrome despite a screening test showing that he was extremely unlikely to carry the condition.
But Stacie Chapman knew nothing about these uncertainties when Dr. Sloan told her that her unborn son had screened positive for a genetic condition that was largely incompatible with life.
Hysterical with grief when she hung up, Chapman phoned her husband at a Las Vegas airport on his way home from a business trip. Together, sobbing, they concluded that their son would only suffer if he survived birth. So, that afternoon, Sloan put her in touch with a nurse who found a doctor who could do the termination the next morning.
Chapman spent the afternoon Googling the horrors of Edwards syndrome, with its heart defects, development delays, and extraordinarily high mortality. She was steeling herself for the termination when Sloan called back,urging her to wait, according to Chapman’s medical record.
Chapman had a diagnostic test and learned her son did not have Edwards syndrome. A healthy Lincoln Samuel just turned 1 and has a wide smile that reminds Chapman of her recently deceased father.
However briefly considered, their decision to abort — informed by the MaterniT21’s advertised 99 percent detection statistic — haunts them to this day.
“He is so perfect,’’ Chapman, 43, said, choking up as she watched her son play with a toy lamb. “I almost terminated him.”
Overselling a screen
Advertisements for these new prenatal screens are filled with bright skies, serene, full-bellied women, and, most of all, assurances that the tests can be trusted.
“Never maybe,” promises MaterniT21 in pamphlets. Panorama states its test is “99% Accurate, Simple & Trusted” on a web page.
The screens, conducted as early as nine weeks into a pregnancy, detect placental DNA in a mother’s blood and test it for chromosomal abnormalities as well as gender.
Originally designed for older women and others at higher risk for having a problematic fetus, some of the screens are now marketed to all pregnant women. Company and analyst data indicate there have probably been between 450,000 to 800,000 tests performed in the United States since 2011 and several companies are racing to corner what one market research firm predicts will be a $3.6 billion global industry by 2019.
Independent medical experts say the new screens are far better able to rule out the possibility of certain fetal conditions, especially Down syndrome, than traditional ultrasounds and blood screenings.
That dramatically cuts down on the number of women who are incorrectly told their fetus may have a problem and helps them avoid a more invasive follow-up test, such as amniocentesis, which carries a small risk of miscarriage.
But the new screens are not perfect and can indicate fetuses may have serious genetic abnormalities when they do not, the industry’s own research shows.
For example, among older pregnant women such as Chapman, for whom chromosomal abnormalities are more common, a positive test result for Edwards syndrome is accurate around 64 percent of the time, according to a recent study by Quest Diagnostics, a large provider of medical tests and other services. That means Baby Lincoln had about a 36 percent chance of not having the condition.
Among younger women who are at lower risk for fetal abnormalities, the error rate is even higher. Only about 40 percent of the positive tests showing high risk for Edwards syndrome turned out to be accurate, according to a recent well-regarded Illumina study of its Verifi screen.
The testing companies do recommend that women who get a positive screen result should seek additional tests to confirm it — much the way a woman whose mammogram showed potential breast cancer would undergo a biopsy to determine whether the dark spots actually are cancerous.
But some companies blur the distinction between the results of their screening tests and a true diagnosis, potentially confusing patients and doctors about the trustworthiness and meaning of their test results. Illumina, for example, claims its Verifi screen has “near-diagnostic accuracy,” a term medical experts say has no meaning.
“The companies have done a very poor job of education [and] advertising this new technology, failing to make clear that it is screening testing with very good but inevitably not perfect test performance . . . and that doctors are recommending, offering, ordering a test they do not fully understand,’’ said Dr. Michael Greene, director of obstetrics at Massachusetts General Hospital and a professor at Harvard Medical School.
Company officials say they are now focusing on the accuracy of all test results, including false positives, carrying out research on their frequency, and looking for ways to reduce the stress of these events.
Getting patients to understand limits on the accuracy of positive test results can be “extremely challenging,” said Juan-Sebastian Saldivar, vice president of clinical services and medical affairs at Sequenom, which offers the screen that Chapman used. He said the company works with doctors on how to best explain it to patients.
Officials at Natera, which offers the Panorama test, insist their screens are highly accurate and produce relatively few false alarms. A company-funded study found that positive test results are correct 83 percent of the time, which is more accurate than studies of other tests have shown.
Melissa Stosic, Natera’s director of medical education and clinical affairs, stresses that the company doesn’t oversell the test, working to educate doctors “to be very clear it’s a screening and not diagnostic.”
However, the same Natera study found that some women are ignoring that advice and having abortions without getting a confirmatory diagnostic test. In its study, 22 women out of 356 who were told their fetuses were at high risk for some abnormality terminated the pregnancy without getting an invasive test to confirm the results.
“It’s troubling,’’ said Katie Stoll, a genetic counselor in Washington state who has written extensively on the marketing of noninvasive prenatal screens. “Women are getting the wrong message.”
A short life
The field of this prenatal testing is so new, and the research so dominated by the companies selling the tests, that basic questions about their reliability and testing methods remain unresolved.
For instance, screening companies say they have had exceedingly few cases of women whose screen shows little problem, but then deliver a baby with a genetic condition. Yet such cases are popping up across the country.
It is not clear how large a problem it is, but critics say the troubling anecdotes are another example of quality control concerns that are not being independently vetted.
Belinda Boydston, 43, of Arizona, was stunned to give birth to a baby with Edwards syndrome after a Harmony screen result in October 2013 showed her fetus had only a 0.01 percent chance of having Edwards syndrome, also known as Trisomy 18.
“I delivered prematurely, and they knew right away he had Trisomy 18,” Boydston said, recounting the scene in the delivery room. “I could hear them talking, ‘Didn’t she have that test?’ ”
This year alone, at the Emory Healthcare Department of Human Genetics in Georgia, officials have seen five newborns with Down syndrome whose prenatal noninvasive screens indicated that there was little risk of the condition.
And a couple in Belmont, Calif., sued Ariosa Diagnostics Inc. last year, alleging its Harmony screen falsely indicated their child would not have Down syndrome and that the company’s marketing material misled patients about the screen’s accuracy. The lawsuit is still pending. Ariosa declined to comment, as did Roche, which is acquiring it.
“There needs to be more transparency and accuracy from the companies about what their results mean,’’ said Mary Norton, vice chair of genetics in the department of obstetrics, gynecology, and reproductive sciences at the University of California San Francisco. Norton, who has received funding from Ariosa and Natera, said research in the field is almost all being funded by industry. “There isn’t a lot of independent research going on.”
FDA regulatory loophole
The loophole that allows unregulated tests in the marketplace dates back to the mid-1970s, when the FDA began overseeing diagnostic tests. The FDA exempted what was then a small group of relatively simple tests developed, manufactured, and performed all in a single lab — for example, in a hospital.
In the past decade, for-profit companies have used that regulatory running room to develop complex tests to diagnose or screen for conditions ranging from cancer to Lyme disease and now, fetal chromosomal conditions. Not all tests undergo robust independent review and it is challenging for the public to distinguish good and bad tests, medical experts say.
In late September, the FDA stepped in, publishing draft regulations for the industry expected to take nine years to be fully phased in. Officials there said that the new prenatal tests would probably be among the first few groups to be regulated. Already, the industry is expected to challenge the legality of those rules and a trade group, the American Clinical Laboratory Association, has retained Harvard Law professor Laurence Tribe to help represent them.
However, the FDA has made it clear that the companies don’t have to wait for regulations to act.
We “have told the [prenatal] companies . . . they really should bring their test into the agency,’’ said Alberto Gutierrez, director of the FDA’s office of in vitro diagnostics in the Center for Devices and Radiological Health. He indicated they could voluntarily submit to regulation, as other types of diagnostic testing companies have done.
While the regulatory fight goes on, doctors say one immediate way to limit potential misuse of possibly inaccurate prenatal screening results is for women to receive genetic counseling before they get the screens — and after. Several women, including Chapman, told the New England Center they were offered the prenatal screens without any clear understanding of what their fetus would be tested for other than Down syndrome and to learn the sex of the baby.
Lincoln Chapman, Stacie’s husband, said he will be forever grateful to Dr. Sloan, of Harvard Vanguard Medical Associates in Boston, for calling Stacie Chapman back to more strongly recommend further tests.
But Stacie Chapman remains conflicted about the doctor’s first call that set in motion the near termination of her pregnancy. Sloan did not stress that the test was just a screen that could be wrong, she recalled.
“I didn’t seek this test out — this test was offered to me by the doctor’s office. They should know how it performs,’’ Chapman said, adding that she would never have considered a pregnancy termination if she had better understood the odds that her result could be wrong.
A health professional involved in Chapman’s case who was not authorized by her employer to comment said Sloan initially was unaware that the screen could be wrong a significant amount of the time.
Sloan did not return calls to discuss her understanding of the statistics, but a Harvard Vanguard statement noted its policy recommends genetic counseling and confirmatory testing for women whose fetuses test positive for a genetic abnormality.
Chapman said enormous heartache could have been avoided in her family if companies advertised more scrupulously, or if her doctor had understood the limitations of the screen.
As millions of women in the United States and elsewhere expect babies this year, some inevitably will be in the same situation as Chapman.
“You know, when I found out [the baby] was fine, my midwife said, ‘You are one in a million, you are so lucky,’ ” Chapman recalls. “But you know? I really wasn’t.”
By Beth Daley : NE Center for Investigative Reporting : December 14, 2014
Stacie Chapman’s heart skipped when she answered the phone at home and her doctor — rather than a nurse — was on the line. More worrisome was the doctor’s gentle tone as she asked, “Where are you?”
On that spring day in 2013, Dr. Jayme Sloan had bad news for Chapman, who was nearly three months pregnant. Her unborn child had tested positive for Edwards syndrome, a genetic condition associated with severe birth defects. If her baby — a boy, the screening test had shown — was born alive, he probably would not live long.
Sloan explained that the test — MaterniT21 PLUS — has a 99 percent detection rate. Though Sloan offered additional testing to confirm the result, a distraught Chapman said she wanted to terminate the pregnancy immediately.
What she — and the doctor — did not understand, Chapman’s medical records indicate, was that there was a good chance her screening result was wrong. There is, it turns out, a huge and crucial difference between a test that can detect a potential problem and one reliable enough to diagnose a life-threatening condition for certain. The screening test only does the first.
Sparked by the sequencing of the human genome a decade ago, a new generation of prenatal screening tests, including MaterniT21, has exploded onto the market in the past three years. The unregulated screens claim to detect with near-perfect accuracy the risk that a fetus may have Down or Edwards syndromes, and a growing list of other chromosomal abnormalities.
Hundreds of thousands of women in early pregnancy have taken these tests — through a simple blood draw in the doctor’s office — and studies show them to perform far better than traditional blood tests and ultrasound screening.
But a three-month examination by the New England Center for Investigative Reporting has found that companies are overselling the accuracy of their tests and doing little to educate expecting parents or their doctors about the significant risks of false alarms.
Two recent industry-funded studies show that test results indicating a fetus is at high risk for a chromosomal condition can be a false alarm half of the time. And the rate of false alarms goes up the more rare the condition, such as Trisomy 13, which almost always causes death.
Companies selling the most popular of these screens do not make it clear enough to patients and doctors that the results of their tests are not reliable enough to make a diagnosis.
California-based Sequenom Inc., for instance, promises on its web page that its MaterniT21 blood test provides “simple, clear results.” Only far down below does Sequenom disclose that “no test is perfect” and that theirs can produce erroneous results “in rare cases.”
Now, evidence is building that some women are terminating pregnancies based on the screening tests alone. A recent study by another California-based testing company, Natera Inc., which offers a screen called Panorama, found that 6.2 percent of women who received test results showing their fetus at high risk for a chromosomal condition terminated pregnancies without getting a diagnostic test such as an amniocentesis.
And at Stanford University, there have been at least three cases of women aborting healthy fetuses that had received a high-risk screen result.
“The worry is women are terminating without really knowing if [the initial test result] is true or not,” said Athena Cherry, professor of pathology at the Stanford University School of Medicine, whose lab examined the cells of the healthy aborted fetuses.
In one of the three Stanford cases, the woman actually obtained a confirmatory test and was told the fetus was fine, but aborted anyway because of her faith in the screening company’s accuracy claims. “She felt it couldn’t be wrong,” Cherry said.
Companies that sell the screens stand behind their tests, saying they provide much more reliable assurance for expecting mothers than earlier screens. Some say their research focused first on how to accurately identify fetuses with potential genetic defects and only recently have they been able to get enough data to understand how often positive tests are wrong.
“The clinical performance of [noninvasive prenatal tests] has been extremely robust,” Dr. Vance Vanier, vice president of marketing for reproductive and genetic health for San Diego-based Illumina Inc., which offers the Verifi prenatal screen, wrote in an e-mail statement.
The screens are not subject to approval by the Food and Drug Administration. Because of a regulatory loophole, the companies operate free of agency oversight and the kind of independent analysis that would validate their accuracy claims. Doctors often get that information from salespeople, according to doctors themselves.
And there are other emerging concerns about the new generation of prenatal tests. Two Boston-area obstetricians, with funding from a testing company, recently sent samples from two nonpregnant women to five testing companies for analysis. Three companies returned samples indicating they came from a woman who was carrying a healthy female fetus.
Meanwhile, there are a growing number of cases emerging of women told their screen shows virtually no chance of a fetus having a problem but who then deliver a child with a genetic condition.
“My son lived for four days,’’ said Belinda Boydston, a web/graphic designer in Chandler, Ariz., whose son was born with Edwards syndrome despite a screening test showing that he was extremely unlikely to carry the condition.
But Stacie Chapman knew nothing about these uncertainties when Dr. Sloan told her that her unborn son had screened positive for a genetic condition that was largely incompatible with life.
Hysterical with grief when she hung up, Chapman phoned her husband at a Las Vegas airport on his way home from a business trip. Together, sobbing, they concluded that their son would only suffer if he survived birth. So, that afternoon, Sloan put her in touch with a nurse who found a doctor who could do the termination the next morning.
Chapman spent the afternoon Googling the horrors of Edwards syndrome, with its heart defects, development delays, and extraordinarily high mortality. She was steeling herself for the termination when Sloan called back,urging her to wait, according to Chapman’s medical record.
Chapman had a diagnostic test and learned her son did not have Edwards syndrome. A healthy Lincoln Samuel just turned 1 and has a wide smile that reminds Chapman of her recently deceased father.
However briefly considered, their decision to abort — informed by the MaterniT21’s advertised 99 percent detection statistic — haunts them to this day.
“He is so perfect,’’ Chapman, 43, said, choking up as she watched her son play with a toy lamb. “I almost terminated him.”
Overselling a screen
Advertisements for these new prenatal screens are filled with bright skies, serene, full-bellied women, and, most of all, assurances that the tests can be trusted.
“Never maybe,” promises MaterniT21 in pamphlets. Panorama states its test is “99% Accurate, Simple & Trusted” on a web page.
The screens, conducted as early as nine weeks into a pregnancy, detect placental DNA in a mother’s blood and test it for chromosomal abnormalities as well as gender.
Originally designed for older women and others at higher risk for having a problematic fetus, some of the screens are now marketed to all pregnant women. Company and analyst data indicate there have probably been between 450,000 to 800,000 tests performed in the United States since 2011 and several companies are racing to corner what one market research firm predicts will be a $3.6 billion global industry by 2019.
Independent medical experts say the new screens are far better able to rule out the possibility of certain fetal conditions, especially Down syndrome, than traditional ultrasounds and blood screenings.
That dramatically cuts down on the number of women who are incorrectly told their fetus may have a problem and helps them avoid a more invasive follow-up test, such as amniocentesis, which carries a small risk of miscarriage.
But the new screens are not perfect and can indicate fetuses may have serious genetic abnormalities when they do not, the industry’s own research shows.
For example, among older pregnant women such as Chapman, for whom chromosomal abnormalities are more common, a positive test result for Edwards syndrome is accurate around 64 percent of the time, according to a recent study by Quest Diagnostics, a large provider of medical tests and other services. That means Baby Lincoln had about a 36 percent chance of not having the condition.
Among younger women who are at lower risk for fetal abnormalities, the error rate is even higher. Only about 40 percent of the positive tests showing high risk for Edwards syndrome turned out to be accurate, according to a recent well-regarded Illumina study of its Verifi screen.
The testing companies do recommend that women who get a positive screen result should seek additional tests to confirm it — much the way a woman whose mammogram showed potential breast cancer would undergo a biopsy to determine whether the dark spots actually are cancerous.
But some companies blur the distinction between the results of their screening tests and a true diagnosis, potentially confusing patients and doctors about the trustworthiness and meaning of their test results. Illumina, for example, claims its Verifi screen has “near-diagnostic accuracy,” a term medical experts say has no meaning.
“The companies have done a very poor job of education [and] advertising this new technology, failing to make clear that it is screening testing with very good but inevitably not perfect test performance . . . and that doctors are recommending, offering, ordering a test they do not fully understand,’’ said Dr. Michael Greene, director of obstetrics at Massachusetts General Hospital and a professor at Harvard Medical School.
Company officials say they are now focusing on the accuracy of all test results, including false positives, carrying out research on their frequency, and looking for ways to reduce the stress of these events.
Getting patients to understand limits on the accuracy of positive test results can be “extremely challenging,” said Juan-Sebastian Saldivar, vice president of clinical services and medical affairs at Sequenom, which offers the screen that Chapman used. He said the company works with doctors on how to best explain it to patients.
Officials at Natera, which offers the Panorama test, insist their screens are highly accurate and produce relatively few false alarms. A company-funded study found that positive test results are correct 83 percent of the time, which is more accurate than studies of other tests have shown.
Melissa Stosic, Natera’s director of medical education and clinical affairs, stresses that the company doesn’t oversell the test, working to educate doctors “to be very clear it’s a screening and not diagnostic.”
However, the same Natera study found that some women are ignoring that advice and having abortions without getting a confirmatory diagnostic test. In its study, 22 women out of 356 who were told their fetuses were at high risk for some abnormality terminated the pregnancy without getting an invasive test to confirm the results.
“It’s troubling,’’ said Katie Stoll, a genetic counselor in Washington state who has written extensively on the marketing of noninvasive prenatal screens. “Women are getting the wrong message.”
A short life
The field of this prenatal testing is so new, and the research so dominated by the companies selling the tests, that basic questions about their reliability and testing methods remain unresolved.
For instance, screening companies say they have had exceedingly few cases of women whose screen shows little problem, but then deliver a baby with a genetic condition. Yet such cases are popping up across the country.
It is not clear how large a problem it is, but critics say the troubling anecdotes are another example of quality control concerns that are not being independently vetted.
Belinda Boydston, 43, of Arizona, was stunned to give birth to a baby with Edwards syndrome after a Harmony screen result in October 2013 showed her fetus had only a 0.01 percent chance of having Edwards syndrome, also known as Trisomy 18.
“I delivered prematurely, and they knew right away he had Trisomy 18,” Boydston said, recounting the scene in the delivery room. “I could hear them talking, ‘Didn’t she have that test?’ ”
This year alone, at the Emory Healthcare Department of Human Genetics in Georgia, officials have seen five newborns with Down syndrome whose prenatal noninvasive screens indicated that there was little risk of the condition.
And a couple in Belmont, Calif., sued Ariosa Diagnostics Inc. last year, alleging its Harmony screen falsely indicated their child would not have Down syndrome and that the company’s marketing material misled patients about the screen’s accuracy. The lawsuit is still pending. Ariosa declined to comment, as did Roche, which is acquiring it.
“There needs to be more transparency and accuracy from the companies about what their results mean,’’ said Mary Norton, vice chair of genetics in the department of obstetrics, gynecology, and reproductive sciences at the University of California San Francisco. Norton, who has received funding from Ariosa and Natera, said research in the field is almost all being funded by industry. “There isn’t a lot of independent research going on.”
FDA regulatory loophole
The loophole that allows unregulated tests in the marketplace dates back to the mid-1970s, when the FDA began overseeing diagnostic tests. The FDA exempted what was then a small group of relatively simple tests developed, manufactured, and performed all in a single lab — for example, in a hospital.
In the past decade, for-profit companies have used that regulatory running room to develop complex tests to diagnose or screen for conditions ranging from cancer to Lyme disease and now, fetal chromosomal conditions. Not all tests undergo robust independent review and it is challenging for the public to distinguish good and bad tests, medical experts say.
In late September, the FDA stepped in, publishing draft regulations for the industry expected to take nine years to be fully phased in. Officials there said that the new prenatal tests would probably be among the first few groups to be regulated. Already, the industry is expected to challenge the legality of those rules and a trade group, the American Clinical Laboratory Association, has retained Harvard Law professor Laurence Tribe to help represent them.
However, the FDA has made it clear that the companies don’t have to wait for regulations to act.
We “have told the [prenatal] companies . . . they really should bring their test into the agency,’’ said Alberto Gutierrez, director of the FDA’s office of in vitro diagnostics in the Center for Devices and Radiological Health. He indicated they could voluntarily submit to regulation, as other types of diagnostic testing companies have done.
While the regulatory fight goes on, doctors say one immediate way to limit potential misuse of possibly inaccurate prenatal screening results is for women to receive genetic counseling before they get the screens — and after. Several women, including Chapman, told the New England Center they were offered the prenatal screens without any clear understanding of what their fetus would be tested for other than Down syndrome and to learn the sex of the baby.
Lincoln Chapman, Stacie’s husband, said he will be forever grateful to Dr. Sloan, of Harvard Vanguard Medical Associates in Boston, for calling Stacie Chapman back to more strongly recommend further tests.
But Stacie Chapman remains conflicted about the doctor’s first call that set in motion the near termination of her pregnancy. Sloan did not stress that the test was just a screen that could be wrong, she recalled.
“I didn’t seek this test out — this test was offered to me by the doctor’s office. They should know how it performs,’’ Chapman said, adding that she would never have considered a pregnancy termination if she had better understood the odds that her result could be wrong.
A health professional involved in Chapman’s case who was not authorized by her employer to comment said Sloan initially was unaware that the screen could be wrong a significant amount of the time.
Sloan did not return calls to discuss her understanding of the statistics, but a Harvard Vanguard statement noted its policy recommends genetic counseling and confirmatory testing for women whose fetuses test positive for a genetic abnormality.
Chapman said enormous heartache could have been avoided in her family if companies advertised more scrupulously, or if her doctor had understood the limitations of the screen.
As millions of women in the United States and elsewhere expect babies this year, some inevitably will be in the same situation as Chapman.
“You know, when I found out [the baby] was fine, my midwife said, ‘You are one in a million, you are so lucky,’ ” Chapman recalls. “But you know? I really wasn’t.”
Breakthroughs in Prenatal Screening
By Jane E. Brody : NY Times : October 7, 2013
More than 30 years ago, a 37-year-old friend of mine with an unplanned fourth pregnancy was told by her obstetrician that an amniocentesis was “too dangerous” and could cause a miscarriage. She ultimately bore a child severely affected by Down syndrome, which could have been detected with the test.
Today, my friend’s story would have a different trajectory. She would have a series of screening tests, and if the results suggested a high risk of Down syndrome, then an amniocentesis or chorionic villus sampling (C.V.S.) to make the diagnosis. She’d be given the option to abort the pregnancy.
In the future, a woman who decides to continue a Down syndrome pregnancy may also be offered prenatal treatment to temper the developmental harm to the fetus.
Prenatal diagnosis, today a routine part of obstetric care, has made great strides since the mid-1970s and is now on the cusp of further revolutionary developments.
In the nearly four decades since amniocentesis became widely accepted, new techniques have gradually improved the safety and accuracy of prenatal diagnosis. Prenatal tests for more than 800 genetic disorders have been developed. And the number of women who must undergo amniocentesis or C.V.S. has been greatly reduced.
The newest screening test, highly accurate and noninvasive, relies on fetal genetic fragments found in the mother’s blood. Available commercially from four companies, this test is so accurate in detecting Down syndrome that few, if any, affected fetuses are missed, and far fewer women need an invasive procedure to confirm or refute the presence of Down, according to studies in several countries.
The new test, done late in the first trimester of pregnancy, can also detect other genetic diseases, like extra copies of chromosomes 13 and 18, and a missing sex chromosome. It is not yet approved by the Food and Drug Administration, however, and the American College of Obstetrics and Gynecology currently recommends it only for women at high risk for having a baby with a chromosomal abnormality.
But any woman can get the new screening test if her doctor orders it and she is willing to pay for it herself, according to Dr. Diana W. Bianchi, a neonatologist and geneticist at Tufts University School of Medicine. Dr. Bianchi said she expects it will soon become routine for all pregnant women because, in addition to its “extraordinary accuracy” in detecting a Down syndrome pregnancy, it can be done earlier than other tests, and reduces costs and the risk of complications.
Down syndrome, which occurs in about one in every 700 births in the United States, is by far the most common chromosomal abnormality. It causes physical and intellectual disabilities that range from mild to severe.
In the past, the decision to undergo an amniocentesis or C.V.S. was based on a woman’s age or genetic history. The older the woman, the greater her risk of bearing a child with genetic defects due to an abnormal number of chromosomes.
It is now standard practice to offer all pregnant women a series of noninvasive screening tests in the first and second trimesters of pregnancy to assess the chances that a fetus has the extra copy of chromosome 21, which causes Down syndrome. It is then up to the woman to decide whether to undergo C.V.S. or an amniocentesis.
Taken together, these older screening tests pick up about 92 percent of cases of Down syndrome but miss 8 percent. And they yield false-positive results incorrectly indicating the presence of Down in about 5 percent of fetuses.
“This means a lot of women are needlessly worried and a lot have amnios that are not medically necessary,” Dr. Bianchi explained at a meeting last December of the March of Dimes.
Amniocentesis is performed between 15 and 20 weeks of gestation and involves inserting a long needle into a woman’s uterus to extract some of the fluid and cells surrounding the fetus. In C.V.S., usually done at 11 weeks gestation, the fetal cell sample is taken from the placenta. The cells are then analyzed for possible genetic defects. There is a small risk of miscarriage associated with both procedures.
But the new tests of fetal DNA from the mother’s blood detect all or nearly all cases of Down syndrome, and they return false-positive results in fewer than 1 percent of cases. Only those with a positive result need a C.V.S. or amniocentesis to confirm a Down syndrome pregnancy, and only about one woman in 1,000 who are tested requires such an invasive procedure to learn that her fetus does not have Down syndrome.
In a recent article in The New England Journal of Medicine, however, Stephanie Morain, a doctoral candidate at Harvard who studies medical ethics, and her co-authors said the fetal DNA tests have some disadvantages. They miss some chromosomal abnormalities detected by standard screening techniques, and they are “not widely covered by insurance.” Prices for the tests range from about $800 to more than $2,000, although some companies offer “introductory pricing” specials at about $200.
The new tests are also not required to meet the strict standards of safety and effectiveness established by the F.D.A., and they are valid only in singleton pregnancies. Nonetheless, tens of thousands of the fetal DNA tests have been performed to date.
The new test requires just a few teaspoons of a pregnant woman’s blood. During pregnancy, a woman’s blood contains cell-free DNA from herself and her unborn baby. On average, Dr. Bianchi said in an interview, at around 10 weeks of gestation, about 10 to 12 percent of the DNA in a woman’s blood will be fetal DNA from the placenta.
Using modern genetic sequencing techniques, the fetal DNA can be rapidly analyzed at a relatively low cost, in part because multiple samples from different women can be examined simultaneously.
As with other screening tests, the new DNA tests are “not diagnostic,” Dr. Lee P. Shulman, a geneticist at Northwestern University Feinberg School of Medicine, emphasized. A positive result on the test must always be confirmed by a C.V.S. or amniocentesis. Dr. Bianchi is now most excited by the prospect of treating a Down syndrome fetus before birth to minimize the disorder’s neurological effects. Studies have shown that giving pregnant mice medication that counters fetal oxidative stress results in more normal brain development of pups with Down syndrome.
When prenatal testing reveals that a fetus has a chromosomal defect or some other serious birth defect, the March of Dimes recommends that parents:
* Consult a specialist in maternal-fetal medicine who is specially trained to treat high-risk pregnancies.
* Arrange to give birth in a hospital with a Level III newborn intensive care unit (NICU) staffed and equipped to provide the expert care needed by infants with special needs.
* Discuss the best way to deliver the baby with the doctor; a cesarean section is safer than a vaginal birth for babies with certain birth defects.
* Consult a pediatrician who specializes in the kind of care (for example, cardiac or neurological) that the baby will need after birth.
* Join an organization or volunteer group that can provide support and education about how best to care for the baby’s specific needs.
By Jane E. Brody : NY Times : October 7, 2013
More than 30 years ago, a 37-year-old friend of mine with an unplanned fourth pregnancy was told by her obstetrician that an amniocentesis was “too dangerous” and could cause a miscarriage. She ultimately bore a child severely affected by Down syndrome, which could have been detected with the test.
Today, my friend’s story would have a different trajectory. She would have a series of screening tests, and if the results suggested a high risk of Down syndrome, then an amniocentesis or chorionic villus sampling (C.V.S.) to make the diagnosis. She’d be given the option to abort the pregnancy.
In the future, a woman who decides to continue a Down syndrome pregnancy may also be offered prenatal treatment to temper the developmental harm to the fetus.
Prenatal diagnosis, today a routine part of obstetric care, has made great strides since the mid-1970s and is now on the cusp of further revolutionary developments.
In the nearly four decades since amniocentesis became widely accepted, new techniques have gradually improved the safety and accuracy of prenatal diagnosis. Prenatal tests for more than 800 genetic disorders have been developed. And the number of women who must undergo amniocentesis or C.V.S. has been greatly reduced.
The newest screening test, highly accurate and noninvasive, relies on fetal genetic fragments found in the mother’s blood. Available commercially from four companies, this test is so accurate in detecting Down syndrome that few, if any, affected fetuses are missed, and far fewer women need an invasive procedure to confirm or refute the presence of Down, according to studies in several countries.
The new test, done late in the first trimester of pregnancy, can also detect other genetic diseases, like extra copies of chromosomes 13 and 18, and a missing sex chromosome. It is not yet approved by the Food and Drug Administration, however, and the American College of Obstetrics and Gynecology currently recommends it only for women at high risk for having a baby with a chromosomal abnormality.
But any woman can get the new screening test if her doctor orders it and she is willing to pay for it herself, according to Dr. Diana W. Bianchi, a neonatologist and geneticist at Tufts University School of Medicine. Dr. Bianchi said she expects it will soon become routine for all pregnant women because, in addition to its “extraordinary accuracy” in detecting a Down syndrome pregnancy, it can be done earlier than other tests, and reduces costs and the risk of complications.
Down syndrome, which occurs in about one in every 700 births in the United States, is by far the most common chromosomal abnormality. It causes physical and intellectual disabilities that range from mild to severe.
In the past, the decision to undergo an amniocentesis or C.V.S. was based on a woman’s age or genetic history. The older the woman, the greater her risk of bearing a child with genetic defects due to an abnormal number of chromosomes.
It is now standard practice to offer all pregnant women a series of noninvasive screening tests in the first and second trimesters of pregnancy to assess the chances that a fetus has the extra copy of chromosome 21, which causes Down syndrome. It is then up to the woman to decide whether to undergo C.V.S. or an amniocentesis.
Taken together, these older screening tests pick up about 92 percent of cases of Down syndrome but miss 8 percent. And they yield false-positive results incorrectly indicating the presence of Down in about 5 percent of fetuses.
“This means a lot of women are needlessly worried and a lot have amnios that are not medically necessary,” Dr. Bianchi explained at a meeting last December of the March of Dimes.
Amniocentesis is performed between 15 and 20 weeks of gestation and involves inserting a long needle into a woman’s uterus to extract some of the fluid and cells surrounding the fetus. In C.V.S., usually done at 11 weeks gestation, the fetal cell sample is taken from the placenta. The cells are then analyzed for possible genetic defects. There is a small risk of miscarriage associated with both procedures.
But the new tests of fetal DNA from the mother’s blood detect all or nearly all cases of Down syndrome, and they return false-positive results in fewer than 1 percent of cases. Only those with a positive result need a C.V.S. or amniocentesis to confirm a Down syndrome pregnancy, and only about one woman in 1,000 who are tested requires such an invasive procedure to learn that her fetus does not have Down syndrome.
In a recent article in The New England Journal of Medicine, however, Stephanie Morain, a doctoral candidate at Harvard who studies medical ethics, and her co-authors said the fetal DNA tests have some disadvantages. They miss some chromosomal abnormalities detected by standard screening techniques, and they are “not widely covered by insurance.” Prices for the tests range from about $800 to more than $2,000, although some companies offer “introductory pricing” specials at about $200.
The new tests are also not required to meet the strict standards of safety and effectiveness established by the F.D.A., and they are valid only in singleton pregnancies. Nonetheless, tens of thousands of the fetal DNA tests have been performed to date.
The new test requires just a few teaspoons of a pregnant woman’s blood. During pregnancy, a woman’s blood contains cell-free DNA from herself and her unborn baby. On average, Dr. Bianchi said in an interview, at around 10 weeks of gestation, about 10 to 12 percent of the DNA in a woman’s blood will be fetal DNA from the placenta.
Using modern genetic sequencing techniques, the fetal DNA can be rapidly analyzed at a relatively low cost, in part because multiple samples from different women can be examined simultaneously.
As with other screening tests, the new DNA tests are “not diagnostic,” Dr. Lee P. Shulman, a geneticist at Northwestern University Feinberg School of Medicine, emphasized. A positive result on the test must always be confirmed by a C.V.S. or amniocentesis. Dr. Bianchi is now most excited by the prospect of treating a Down syndrome fetus before birth to minimize the disorder’s neurological effects. Studies have shown that giving pregnant mice medication that counters fetal oxidative stress results in more normal brain development of pups with Down syndrome.
When prenatal testing reveals that a fetus has a chromosomal defect or some other serious birth defect, the March of Dimes recommends that parents:
* Consult a specialist in maternal-fetal medicine who is specially trained to treat high-risk pregnancies.
* Arrange to give birth in a hospital with a Level III newborn intensive care unit (NICU) staffed and equipped to provide the expert care needed by infants with special needs.
* Discuss the best way to deliver the baby with the doctor; a cesarean section is safer than a vaginal birth for babies with certain birth defects.
* Consult a pediatrician who specializes in the kind of care (for example, cardiac or neurological) that the baby will need after birth.
* Join an organization or volunteer group that can provide support and education about how best to care for the baby’s specific needs.
That Prenatal Visit May Be Months Too Late
By Roni Rabin : NY Times : November 28, 2006
For years, women have had it drummed into them that prenatal care is the key to having a healthy baby, and that they should see a doctor as soon as they know they are pregnant.
But by then, it may already be too late. Public health officials are now encouraging women to make sure they are in optimal health well in advance of a pregnancy to reduce the risk of preventable birth defects and complications. They have recast the message to emphasize not only prenatal care, as they did in the past, but also what they are calling “preconception care.”
The problem, doctors say, is that by the first prenatal visit, a woman is usually 10 to 12 weeks pregnant. “If a birth defect is going to happen, it’s already happened,” said Dr. Peter S. Bernstein, a maternal fetal medicine specialist at Montefiore Medical Center in New York who helped write new government guidelines on preconception care.
For many women, Dr. Bernstein said, “The most important doctor’s visit may be the one that takes place before a pregnancy is conceived.”
The new guidelines, issued by the Centers for Disease Control and Prevention last spring, include 10 specific health care recommendations and advise prepregnancy checkups that include screening for diabetes, H.I.V. and obesity; managing chronic medical conditions; reviewing medications that may harm a fetus; and making sure vaccinations are up to date.
Much of the advice directed to women is fairly standard: they should abstain from smoking, alcohol and drugs, and should take prenatal vitamins, including folic acid.
For Diane Jackey, a mother of five from Hempstead, N.Y., maintaining preconception health meant continuing prenatal vitamins between pregnancies, snatching exercise whenever she could and maintaining a balanced diet. “I don’t smoke, and I don’t drink at all,” Ms. Jackey said.
What is new and somewhat controversial about the guidelines is the suggestion that they should apply to women throughout their reproductive years, even when they are not planning pregnancies. (Men should be wary of exposures to toxins that cause birth defects and should avoid sexually transmitted diseases, experts say.)
But while the report was criticized in some quarters for treating all women as though they were eternally “prepregnant,” it also discusses the importance of family planning and child spacing and encourages young people to develop a “reproductive life plan.” Half of all pregnancies in the United States are unplanned, experts say, and preparing for a healthy pregnancy can require behavioral changes that may take months. Even daily supplements of folic acid should ideally be taken for three months before conception.
“It’s not like we have an injection we can give someone” to prepare her for pregnancy, said Dr. Hani Atrash, associate director for program development at the National Center on Birth Defects and Developmental Disabilities at the disease centers. “Some of the interventions, like weight management, need time to happen. You cannot quit smoking in one day.”
The issue of preconception health has taken on added urgency in recent years because while infant mortality rates were on the decline from 1980 to 2000, the proportion of small and preterm babies increased significantly. And low birth weight, which has been linked to maternal smoking and multiple births, is a leading cause of death and disability for infants.
In 2002, the infant mortality rate in the United States increased for the first time in more than 40 years, to 7.0 deaths per 1,000 live births in 2002 from 6.8 deaths per 1,000 live births in 2001. The rate dropped back to 6.8 per 1,000 in 2003. Blacks are at the highest risk for preterm birth and low birth weights, and their infant mortality rates are more than double that of whites.
Meanwhile, rising obesity rates and the tendency to postpone motherhood mean far more women are overweight when they become pregnant and thus are more likely to have high blood pressure, diabetes or prediabetes, which complicate pregnancy.
“There is no question the No. 1 issue for women in America is their weight,” said Dr. Gary Hankins, who leads the committee on obstetrics practice of the American College of Obstetricians and Gynecologists.
Pre-existing diabetes significantly increases the risk of birth defects, but the risk is virtually eliminated if the disease is controlled before conception, Dr. Hankins said. Obese women who become pregnant face a higher risk of developing gestational diabetes and of having a large baby and a difficult delivery.
While doctors have been recommending preconception care for many years, it has never really caught on. Only one in six health care providers said they had provided preconception care to patients, one study found, and most health plans do not cover it. Medicaid, the government health plan for the poor, often only covers women after they are pregnant.
Rochelle Carr, 31, a Bronx mother, sought preconception counseling because she worried that her asthma medications might harm a developing fetus. Ms. Carr was also concerned because she had suffered a life-threatening pulmonary embolism, or blood clot to the lung, when she was 29.
Ms. Carr’s doctor referred her to a maternal fetal medicine specialist at Montefiore Medical Center. Dr. Ashlesha Dayal reviewed Ms. Carr’s medications and advised her to stop taking an asthma drug linked to birth defects and to start taking folic acid daily.
Once Ms. Carr became pregnant, Dr. Dayal prescribed an anticoagulant because Ms. Carr was at high risk for developing another blood clot. The doctor also explained the risks of taking the anticoagulant. “She really put my mind at ease,” said Ms. Carr, who delivered a healthy baby, Joshua, on Nov. 29, 2005.
Doctors say that planning pregnancies and using reliable contraception are part and parcel of preconception care, and they are encouraging all health providers — not just obstetricians but emergency room doctors, primary care physicians, cardiologists and endocrinologists — to counsel women of childbearing age about the possibility of pregnancy. “What we’re actually talking about,” Dr. Atrash said, “is women’s health.”
By Roni Rabin : NY Times : November 28, 2006
For years, women have had it drummed into them that prenatal care is the key to having a healthy baby, and that they should see a doctor as soon as they know they are pregnant.
But by then, it may already be too late. Public health officials are now encouraging women to make sure they are in optimal health well in advance of a pregnancy to reduce the risk of preventable birth defects and complications. They have recast the message to emphasize not only prenatal care, as they did in the past, but also what they are calling “preconception care.”
The problem, doctors say, is that by the first prenatal visit, a woman is usually 10 to 12 weeks pregnant. “If a birth defect is going to happen, it’s already happened,” said Dr. Peter S. Bernstein, a maternal fetal medicine specialist at Montefiore Medical Center in New York who helped write new government guidelines on preconception care.
For many women, Dr. Bernstein said, “The most important doctor’s visit may be the one that takes place before a pregnancy is conceived.”
The new guidelines, issued by the Centers for Disease Control and Prevention last spring, include 10 specific health care recommendations and advise prepregnancy checkups that include screening for diabetes, H.I.V. and obesity; managing chronic medical conditions; reviewing medications that may harm a fetus; and making sure vaccinations are up to date.
Much of the advice directed to women is fairly standard: they should abstain from smoking, alcohol and drugs, and should take prenatal vitamins, including folic acid.
For Diane Jackey, a mother of five from Hempstead, N.Y., maintaining preconception health meant continuing prenatal vitamins between pregnancies, snatching exercise whenever she could and maintaining a balanced diet. “I don’t smoke, and I don’t drink at all,” Ms. Jackey said.
What is new and somewhat controversial about the guidelines is the suggestion that they should apply to women throughout their reproductive years, even when they are not planning pregnancies. (Men should be wary of exposures to toxins that cause birth defects and should avoid sexually transmitted diseases, experts say.)
But while the report was criticized in some quarters for treating all women as though they were eternally “prepregnant,” it also discusses the importance of family planning and child spacing and encourages young people to develop a “reproductive life plan.” Half of all pregnancies in the United States are unplanned, experts say, and preparing for a healthy pregnancy can require behavioral changes that may take months. Even daily supplements of folic acid should ideally be taken for three months before conception.
“It’s not like we have an injection we can give someone” to prepare her for pregnancy, said Dr. Hani Atrash, associate director for program development at the National Center on Birth Defects and Developmental Disabilities at the disease centers. “Some of the interventions, like weight management, need time to happen. You cannot quit smoking in one day.”
The issue of preconception health has taken on added urgency in recent years because while infant mortality rates were on the decline from 1980 to 2000, the proportion of small and preterm babies increased significantly. And low birth weight, which has been linked to maternal smoking and multiple births, is a leading cause of death and disability for infants.
In 2002, the infant mortality rate in the United States increased for the first time in more than 40 years, to 7.0 deaths per 1,000 live births in 2002 from 6.8 deaths per 1,000 live births in 2001. The rate dropped back to 6.8 per 1,000 in 2003. Blacks are at the highest risk for preterm birth and low birth weights, and their infant mortality rates are more than double that of whites.
Meanwhile, rising obesity rates and the tendency to postpone motherhood mean far more women are overweight when they become pregnant and thus are more likely to have high blood pressure, diabetes or prediabetes, which complicate pregnancy.
“There is no question the No. 1 issue for women in America is their weight,” said Dr. Gary Hankins, who leads the committee on obstetrics practice of the American College of Obstetricians and Gynecologists.
Pre-existing diabetes significantly increases the risk of birth defects, but the risk is virtually eliminated if the disease is controlled before conception, Dr. Hankins said. Obese women who become pregnant face a higher risk of developing gestational diabetes and of having a large baby and a difficult delivery.
While doctors have been recommending preconception care for many years, it has never really caught on. Only one in six health care providers said they had provided preconception care to patients, one study found, and most health plans do not cover it. Medicaid, the government health plan for the poor, often only covers women after they are pregnant.
Rochelle Carr, 31, a Bronx mother, sought preconception counseling because she worried that her asthma medications might harm a developing fetus. Ms. Carr was also concerned because she had suffered a life-threatening pulmonary embolism, or blood clot to the lung, when she was 29.
Ms. Carr’s doctor referred her to a maternal fetal medicine specialist at Montefiore Medical Center. Dr. Ashlesha Dayal reviewed Ms. Carr’s medications and advised her to stop taking an asthma drug linked to birth defects and to start taking folic acid daily.
Once Ms. Carr became pregnant, Dr. Dayal prescribed an anticoagulant because Ms. Carr was at high risk for developing another blood clot. The doctor also explained the risks of taking the anticoagulant. “She really put my mind at ease,” said Ms. Carr, who delivered a healthy baby, Joshua, on Nov. 29, 2005.
Doctors say that planning pregnancies and using reliable contraception are part and parcel of preconception care, and they are encouraging all health providers — not just obstetricians but emergency room doctors, primary care physicians, cardiologists and endocrinologists — to counsel women of childbearing age about the possibility of pregnancy. “What we’re actually talking about,” Dr. Atrash said, “is women’s health.”
Prenatal Tests:
More Information, Less Risk
By Jane E. Brody : NY Times : July 27, 2004
At age 35, Angelica decided to start a family. Knowing that her age was associated with an increased risk of bearing a child with a chromosomal defect, at 18 weeks of pregnancy she underwent amniocentesis, an analysis of fetal cells from amniotic fluid extracted by a large needle inserted into the womb through the abdomen.
The test revealed a fetus with the extra chromosome that causes Down syndrome, and a distraught Angelica chose to end the pregnancy.
A year and a half later she was pregnant again. This time she did not want to wait until the fourth month to find out if the fetus had a chromosomal problem, so at 10 weeks she underwent chorionic villus sampling, or C.V.S., an analysis of fetal cells extracted from the placenta. No chromosomal abnormality was found, and six and a half months later she gave birth to a healthy boy.
Now 39, Angelica is pregnant once more. Based on her age, her risk of bearing a child with Down syndrome is 1 in 80. But this time there is to be no amniocentesis or C.V.S., for both tests are costly and invasive, with a small but not insignificant risk of miscarriage or fetal damage.
Instead, she underwent a series of simple blood tests plus a detailed sonogram at 12 weeks. These tests revealed that there was only a 1 in 981 chance that her child would have a chromosomal abnormality or neural tube defect, about the same risk as that faced by a woman of 29.
Measuring the Hazards
More women are having babies later in their reproductive lives, at ages when the chance of conceiving a child with a major chromosomal defect rises precipitously. The American College of Obstetricians and Gynecologists and the American College of Medical Genetics recommend that prenatal diagnosis by amniocentesis or C.V.S. be offered to all pregnant women 35 and older, as well as to younger women with positive results on screening blood tests.
But using age as the sole criterion has resulted in rising numbers of the invasive and expensive tests, as well as an increase in miscarriages of what are often hard-won pregnancies among older women. And so experts in obstetrics and fetal medicine have devised a series of simple blood tests that, when factored together with a woman's age and often with the results of a sonogram, are greatly reducing the numbers of women undergoing the more involved tests without compromising the chances of detecting serious fetal abnormalities.
A new study, published in the June issue of Obstetrics & Gynecology, illustrates this trend. According to the study, the number of women in Connecticut who had amniocentesis or C.V.S. declined 50 percent from 1991 to 2002, while the share of Down syndrome births did not increase even though more women were becoming pregnant at ''an advanced maternal age.''
Dr. Peter A. Benn, a geneticist at the University of Connecticut Health Center in Farmington, where the study was done, said fewer women had the procedures because more of them had blood tests and sonograms to screen for abnormalities.
Before September 1991, Dr. Benn said, women at his center were identified as facing a high risk of a chromosomally abnormal fetus based on their age or family history, or based on their having a low level of alpha-fetoprotein, a substance in blood. That month, though, the center began screening for Down syndrome in the second trimester of pregnancy using maternal blood levels of three substances -- alpha-fetoprotein plus human chorionic gonadotropin and estriol -- and combining those levels with the woman's age to obtain a risk estimate.
In 1996, structural abnormalities visible on a sonogram were used to modify the blood-test risk estimate. In 1999, the center added a fourth substance in blood, inhibin-A, to the risk calculation.
In 1991, there were 48,566 live births there, with 6,082, or 12 percent, to women 35 or older at delivery. In 2002, the number of live births declined to 41,690, but the number born to women 35 and older rose to 9,040, 21.7 percent of the total.
Despite the 58 percent increase in the share of women 35 and older at delivery, referrals to the center for an invasive test based on age alone declined 68 percent as those receiving the prenatal blood and ultrasound tests grew.
''Using age as the sole criterion for an invasive test is not an efficient use of resources,'' Dr. Benn said in an interview. He added that reducing the number of invasive tests did not result in a failure to detect affected pregnancies.
''We're getting at least as many, if not more,'' he said, at a much lower cost and with minimal trauma to the woman and her unborn child. An amniocentesis or C.V.S. costs $2,000 or more, while the blood tests and sonogram cost about $300.
In some areas of the country, blood tests plus the sonogram, which among other things measures a translucent area at the back of the fetal neck, are being performed in the first trimester, as was done in Angelica's case. This approach relieves overall maternal anxiety, because the overwhelming majority of tested pregnancies give a low-risk result. It also permits abortion of an affected pregnancy before other people know the woman is pregnant.
First-trimester screening has been used in Europe for several years but is only now becoming part of American obstetrical practice, Dr. Benn said.
Understanding the Data
Doctors, midwives and nurses can estimate the risk of having a baby with chromosomal abnormalities, but each woman must decide herself what to do with that information. In a report in the May/June issue of The Journal of Midwifery & Women's Health, Dr. Elena A. Gates, an obstetrician-gynecologist at the University of California, San Francisco, explored the factors influencing a woman's perception of risk.
''We toss numbers around but don't appreciate the difficulties people have in understanding the figures,'' Dr. Gates said in an interview.
She added that among the factors influencing a woman's perception of risk are her ideas ''when she walks in the door -- what she's read or heard from her friends, and how familiar she is with the condition, whether a friend, neighbor or family member had an affected child or she had a prior affected pregnancy.''
Also important, she said, is how the information is presented. ''Do you say you have a 5 percent chance of Down syndrome,'' she asked, ''or a 95 percent chance that the baby is not affected?''
In reviewing studies of how women perceive risk, Dr. Gates said, she discovered that it was much harder for most women to understand greater or lesser risk when proportions were used -- say, 1 in 384 versus 1 in 112 -- than when the same risks were expressed as a rate, like 2.6 per 1,000 versus 8.9 per 1,000.
It takes time to explain risk estimates to pregnant women and their partners, and to be sure they grasp the full meaning of the numbers within the context of personal experience and knowledge.
''Providers should bear in mind that a woman's individual values are much more important to optimizing decision-making than are her risks of any particular outcome,'' Dr. Gates concluded.
But she added a cautionary note: because of economics, lack of access to doctors and clinics, or simply a delay in receiving care, only about half of all pregnant women in this country receive prenatal diagnostic tests early enough to abort an affected pregnancy or prepare for the birth of an affected child.
More Information, Less Risk
By Jane E. Brody : NY Times : July 27, 2004
At age 35, Angelica decided to start a family. Knowing that her age was associated with an increased risk of bearing a child with a chromosomal defect, at 18 weeks of pregnancy she underwent amniocentesis, an analysis of fetal cells from amniotic fluid extracted by a large needle inserted into the womb through the abdomen.
The test revealed a fetus with the extra chromosome that causes Down syndrome, and a distraught Angelica chose to end the pregnancy.
A year and a half later she was pregnant again. This time she did not want to wait until the fourth month to find out if the fetus had a chromosomal problem, so at 10 weeks she underwent chorionic villus sampling, or C.V.S., an analysis of fetal cells extracted from the placenta. No chromosomal abnormality was found, and six and a half months later she gave birth to a healthy boy.
Now 39, Angelica is pregnant once more. Based on her age, her risk of bearing a child with Down syndrome is 1 in 80. But this time there is to be no amniocentesis or C.V.S., for both tests are costly and invasive, with a small but not insignificant risk of miscarriage or fetal damage.
Instead, she underwent a series of simple blood tests plus a detailed sonogram at 12 weeks. These tests revealed that there was only a 1 in 981 chance that her child would have a chromosomal abnormality or neural tube defect, about the same risk as that faced by a woman of 29.
Measuring the Hazards
More women are having babies later in their reproductive lives, at ages when the chance of conceiving a child with a major chromosomal defect rises precipitously. The American College of Obstetricians and Gynecologists and the American College of Medical Genetics recommend that prenatal diagnosis by amniocentesis or C.V.S. be offered to all pregnant women 35 and older, as well as to younger women with positive results on screening blood tests.
But using age as the sole criterion has resulted in rising numbers of the invasive and expensive tests, as well as an increase in miscarriages of what are often hard-won pregnancies among older women. And so experts in obstetrics and fetal medicine have devised a series of simple blood tests that, when factored together with a woman's age and often with the results of a sonogram, are greatly reducing the numbers of women undergoing the more involved tests without compromising the chances of detecting serious fetal abnormalities.
A new study, published in the June issue of Obstetrics & Gynecology, illustrates this trend. According to the study, the number of women in Connecticut who had amniocentesis or C.V.S. declined 50 percent from 1991 to 2002, while the share of Down syndrome births did not increase even though more women were becoming pregnant at ''an advanced maternal age.''
Dr. Peter A. Benn, a geneticist at the University of Connecticut Health Center in Farmington, where the study was done, said fewer women had the procedures because more of them had blood tests and sonograms to screen for abnormalities.
Before September 1991, Dr. Benn said, women at his center were identified as facing a high risk of a chromosomally abnormal fetus based on their age or family history, or based on their having a low level of alpha-fetoprotein, a substance in blood. That month, though, the center began screening for Down syndrome in the second trimester of pregnancy using maternal blood levels of three substances -- alpha-fetoprotein plus human chorionic gonadotropin and estriol -- and combining those levels with the woman's age to obtain a risk estimate.
In 1996, structural abnormalities visible on a sonogram were used to modify the blood-test risk estimate. In 1999, the center added a fourth substance in blood, inhibin-A, to the risk calculation.
In 1991, there were 48,566 live births there, with 6,082, or 12 percent, to women 35 or older at delivery. In 2002, the number of live births declined to 41,690, but the number born to women 35 and older rose to 9,040, 21.7 percent of the total.
Despite the 58 percent increase in the share of women 35 and older at delivery, referrals to the center for an invasive test based on age alone declined 68 percent as those receiving the prenatal blood and ultrasound tests grew.
''Using age as the sole criterion for an invasive test is not an efficient use of resources,'' Dr. Benn said in an interview. He added that reducing the number of invasive tests did not result in a failure to detect affected pregnancies.
''We're getting at least as many, if not more,'' he said, at a much lower cost and with minimal trauma to the woman and her unborn child. An amniocentesis or C.V.S. costs $2,000 or more, while the blood tests and sonogram cost about $300.
In some areas of the country, blood tests plus the sonogram, which among other things measures a translucent area at the back of the fetal neck, are being performed in the first trimester, as was done in Angelica's case. This approach relieves overall maternal anxiety, because the overwhelming majority of tested pregnancies give a low-risk result. It also permits abortion of an affected pregnancy before other people know the woman is pregnant.
First-trimester screening has been used in Europe for several years but is only now becoming part of American obstetrical practice, Dr. Benn said.
Understanding the Data
Doctors, midwives and nurses can estimate the risk of having a baby with chromosomal abnormalities, but each woman must decide herself what to do with that information. In a report in the May/June issue of The Journal of Midwifery & Women's Health, Dr. Elena A. Gates, an obstetrician-gynecologist at the University of California, San Francisco, explored the factors influencing a woman's perception of risk.
''We toss numbers around but don't appreciate the difficulties people have in understanding the figures,'' Dr. Gates said in an interview.
She added that among the factors influencing a woman's perception of risk are her ideas ''when she walks in the door -- what she's read or heard from her friends, and how familiar she is with the condition, whether a friend, neighbor or family member had an affected child or she had a prior affected pregnancy.''
Also important, she said, is how the information is presented. ''Do you say you have a 5 percent chance of Down syndrome,'' she asked, ''or a 95 percent chance that the baby is not affected?''
In reviewing studies of how women perceive risk, Dr. Gates said, she discovered that it was much harder for most women to understand greater or lesser risk when proportions were used -- say, 1 in 384 versus 1 in 112 -- than when the same risks were expressed as a rate, like 2.6 per 1,000 versus 8.9 per 1,000.
It takes time to explain risk estimates to pregnant women and their partners, and to be sure they grasp the full meaning of the numbers within the context of personal experience and knowledge.
''Providers should bear in mind that a woman's individual values are much more important to optimizing decision-making than are her risks of any particular outcome,'' Dr. Gates concluded.
But she added a cautionary note: because of economics, lack of access to doctors and clinics, or simply a delay in receiving care, only about half of all pregnant women in this country receive prenatal diagnostic tests early enough to abort an affected pregnancy or prepare for the birth of an affected child.
Alcohol's Toll On Fetuses:
Even Worse Than Thought
By Linda Carroll : NY Times : November 4, 2003
Thirty years ago, scientists linked prenatal alcohol exposure with a perplexing pattern of birth defects including neurological problems, low birth weight, mental retardation and a set of facial malformations.
Up to that time, many doctors had assumed that alcohol was so harmless that it was sometimes administered intravenously to women who were thought to be at risk of losing their pregnancies.
But in recent decades, scientists have discovered that alcohol can be remarkably toxic -- more than any other abused drug -- to developing fetuses. New research with imaging techniques is helping experts uncover which parts of the developing brain are damaged by alcohol exposure.
By pinpointing the damaged areas, they are beginning to understand the origins of the problem behaviors and learning disabilities linked to alcohol.
Scientists are also homing in on a protein important to the developing brain that is affected by alcohol. It is possible, they say, that a medication can be created to protect the brains of developing fetuses, even if pregnant women cannot quit drinking.
It is not surprising that it has taken researchers so long to tease out the link between alcohol exposure and birth defects. For one thing, the effects of alcohol exposure seem to vary widely.
Some fetuses seem to escape unscathed, even when their mothers drink heavily, while others are severely damaged. No one knows why.
''It's not like thalidomide, where anyone who took it had an affected child,'' said Dr. Sandra W. Jacobson, a professor at Wayne State School of Medicine in Detroit, referring to the morning-sickness drug linked to birth defects in the late 1950's and early 1960's. ''There's a range with alcohol. You might get the full-blown syndrome in 4 out of 100 heavy drinkers.''
There are also many babies who are affected, but not severely enough for the syndrome to be diagnosed. Some with fetal alcohol effects may appear relatively normal but have behavioral problems and learning deficits like those with the syndrome.
Further complicating matters is the question of how much alcohol it takes to cause harm. In the past few years, successive studies have shown an effect at increasingly lower levels. One study, published last year, found a small but significant effect on average in children born to women who consumed just a drink and a half a week.
''We were surprised by this,'' said the lead author, Dr. Nancy Day, a professor of psychiatry at the Western Psychiatric Institute and Clinic in Pittsburgh. The women in the study were recruited from a prenatal clinic between May 1983 and July 1985.
''The children were in the normal range of growth,'' Dr. Day said, ''but if you compare them to children whose mothers didn't drink at all, they weighed less, were shorter and had smaller head circumferences.''
The effect of low levels of alcohol appears to be subtle, said Dr. James R. West, head of the department of anatomy and neurobiology at the Texas A&M medical school.
''Perhaps instead of having an I.Q. of 120, you might end up with 115,'' he said. ''You might seem perfectly normal, but not have the motor skills to make the high school football team.''
Another factor making it difficult to tease out the impact of alcohol is its widespread effects on the developing brain and body.
''Alcohol is a dirty drug,'' Dr. West added. ''It affects a number of different neurotransmitters, and all cells can take it up.'' Compare this with cocaine, Dr. West said, which is taken up by only one neurotransmitter.
It is also difficult to identify the effects of alcohol because a woman's drinking habits seem to make a big difference. Experts say it matters when a pregnant woman drinks, how often she drinks and what her pattern of drinking is: whether she drinks small amounts daily or periodically binges.
Drinking in the first trimester can lead to facial malformations, while in the second it can interrupt nerve formation in the brain, Dr. West said. During the third, it can kill existing neurons and interfere with nervous system development, he added.
Researchers have also determined that babies are more likely to be affected if mothers drink in a binge pattern, like five drinks one day rather than a single drink daily, Dr. Jacobson of Wayne State said.
Because alcohol affects so many sites in the brain, researchers have come to believe that alcohol is far worse for the developing fetus than any other abused drug.
Dr. Jacobson's study included cocaine users who also used varying quantities of alcohol. ''We found more serious cognitive impairment in relation to alcohol than cocaine or other drugs, including marijuana and smoking,'' Dr. Jacobson said.
The damage done to fetuses often has been wrongly connected to cocaine, many experts say.
''The consensus, I think, at this point is that most of the adverse effects that had been reported due to cocaine and crack use were from alcohol use,'' said Dr. Kenneth R. Warren, the director of the office of scientific affairs at the National Institute on Alcohol Abuse and Alcoholism. ''It is the leading cause of birth defects due to an ingested environmental substance in this country.''
In 1973, researchers coined the phrase fetal alcohol syndrome to describe babies born with a certain pattern of neurologic and physiologic defects related to alcohol exposure in utero.
Early on, it was clear that exposed children were wired differently from normal ones and that they exhibited an array of disabilities.
Dr. Ann P. Streissguth, the director of the fetal alcohol and drug unit at the University of Washington and a professor at the medical school there, ticked off a list: ''These included attention problems, hyperactivity, learning problems -- particularly in arithmetic -- language problems, memory problems, fine and gross motor problems, poor impulse control, poor judgment, intellectual deficits and difficulty integrating past experience to plan and organize future behavior.''
Researchers wondered whether specific areas of the brain were being consistently harmed by alcohol exposure in utero. Poor judgment, for example, might point to damage to the frontal lobes. The lobes, as the control center of the brain, are involved in planning, organizing and inhibiting inappropriate responses, the researchers say.
Thirty years ago, the only way researchers could learn about the effects of alcohol on the brain was to study children who died shortly after birth.
''We knew from brain autopsies that in severe cases the brains were terribly disorganized,'' said Dr. Edward P. Riley, the director of the Center for Behavioral Teratology at San Diego State University. Now, researchers use imaging techniques like M.R.I.'s to look at the damage caused by alcohol. Several recent studies using magnetic resonance imaging have shown damage to the corpus callosum, a band of nerve fibers that connects the left and right sides of the brain.
A report published in 2002 compared the brain scans of adults and children who had severe or mild alcohol-related disabilities with the scans of healthy counterparts. The researchers found that the corpus callosa were abnormally shaped in 80 percent of those who had been exposed to alcohol in utero.
Another study found that the corpus callosum was smaller and shifted forward in children and young adults with the syndrome. Using a technique known as diffusion tensor imaging to look closer at the corpus callosum, researchers at Emory University have seen abnormalities in the myelin, the substance that insulates nerve cells.
When the myelin is damaged, signals do not carry as crisply through the cells, said Dr. Claire D. Coles, director of the Fetal Alcohol Center at the Marcus Institute and a professor of psychiatry and behavioral sciences at Emory.
Another study published in 2002 found that frontal lobe structures were smaller in teenagers and young adults who had been exposed to alcohol prenatally.
By pinpointing which sections of the brain are most likely to be damaged by alcohol, scientists may find a way to block its effects.
Researchers recently recognized that some of alcohol's effects were similar to those experienced by children born with defects in genes that control L1 adhesion cells. Fetal cells that are destined to grow into the brain and nervous system bind to one another with the help of adhesion molecules like L1, said Dr. Michael E. Charness, an associate professor of neurology at Harvard.
In laboratory experiments, Dr. Charness and his colleagues showed that alcohol could interfere with L1's stickiness, thus hampering crucial cell-to-cell attachments. In an article published in The Proceedings of the National Academy of Sciences in July, they showed that a protein, NAP, could block alcohol's effect on L1. When NAP was given to mice exposed to alcohol, the protein appeared to stave off neurological effects.
''The idea of giving drugs to pregnant women is controversial,'' Dr. Charness said. ''Drugs may have their own risks.''
But, he said, there are areas of the world where fetal alcohol syndrome is a huge problem. In parts of South Africa, the incidence of the syndrome in first graders is around 4.5 percent, he said. ''The rate of drinking is high,'' Dr. Charness added. ''And the women won't stop drinking despite interventions. It might be reasonable to give them a drug that can prevent the more serious effects of alcohol.''
Even Worse Than Thought
By Linda Carroll : NY Times : November 4, 2003
Thirty years ago, scientists linked prenatal alcohol exposure with a perplexing pattern of birth defects including neurological problems, low birth weight, mental retardation and a set of facial malformations.
Up to that time, many doctors had assumed that alcohol was so harmless that it was sometimes administered intravenously to women who were thought to be at risk of losing their pregnancies.
But in recent decades, scientists have discovered that alcohol can be remarkably toxic -- more than any other abused drug -- to developing fetuses. New research with imaging techniques is helping experts uncover which parts of the developing brain are damaged by alcohol exposure.
By pinpointing the damaged areas, they are beginning to understand the origins of the problem behaviors and learning disabilities linked to alcohol.
Scientists are also homing in on a protein important to the developing brain that is affected by alcohol. It is possible, they say, that a medication can be created to protect the brains of developing fetuses, even if pregnant women cannot quit drinking.
It is not surprising that it has taken researchers so long to tease out the link between alcohol exposure and birth defects. For one thing, the effects of alcohol exposure seem to vary widely.
Some fetuses seem to escape unscathed, even when their mothers drink heavily, while others are severely damaged. No one knows why.
''It's not like thalidomide, where anyone who took it had an affected child,'' said Dr. Sandra W. Jacobson, a professor at Wayne State School of Medicine in Detroit, referring to the morning-sickness drug linked to birth defects in the late 1950's and early 1960's. ''There's a range with alcohol. You might get the full-blown syndrome in 4 out of 100 heavy drinkers.''
There are also many babies who are affected, but not severely enough for the syndrome to be diagnosed. Some with fetal alcohol effects may appear relatively normal but have behavioral problems and learning deficits like those with the syndrome.
Further complicating matters is the question of how much alcohol it takes to cause harm. In the past few years, successive studies have shown an effect at increasingly lower levels. One study, published last year, found a small but significant effect on average in children born to women who consumed just a drink and a half a week.
''We were surprised by this,'' said the lead author, Dr. Nancy Day, a professor of psychiatry at the Western Psychiatric Institute and Clinic in Pittsburgh. The women in the study were recruited from a prenatal clinic between May 1983 and July 1985.
''The children were in the normal range of growth,'' Dr. Day said, ''but if you compare them to children whose mothers didn't drink at all, they weighed less, were shorter and had smaller head circumferences.''
The effect of low levels of alcohol appears to be subtle, said Dr. James R. West, head of the department of anatomy and neurobiology at the Texas A&M medical school.
''Perhaps instead of having an I.Q. of 120, you might end up with 115,'' he said. ''You might seem perfectly normal, but not have the motor skills to make the high school football team.''
Another factor making it difficult to tease out the impact of alcohol is its widespread effects on the developing brain and body.
''Alcohol is a dirty drug,'' Dr. West added. ''It affects a number of different neurotransmitters, and all cells can take it up.'' Compare this with cocaine, Dr. West said, which is taken up by only one neurotransmitter.
It is also difficult to identify the effects of alcohol because a woman's drinking habits seem to make a big difference. Experts say it matters when a pregnant woman drinks, how often she drinks and what her pattern of drinking is: whether she drinks small amounts daily or periodically binges.
Drinking in the first trimester can lead to facial malformations, while in the second it can interrupt nerve formation in the brain, Dr. West said. During the third, it can kill existing neurons and interfere with nervous system development, he added.
Researchers have also determined that babies are more likely to be affected if mothers drink in a binge pattern, like five drinks one day rather than a single drink daily, Dr. Jacobson of Wayne State said.
Because alcohol affects so many sites in the brain, researchers have come to believe that alcohol is far worse for the developing fetus than any other abused drug.
Dr. Jacobson's study included cocaine users who also used varying quantities of alcohol. ''We found more serious cognitive impairment in relation to alcohol than cocaine or other drugs, including marijuana and smoking,'' Dr. Jacobson said.
The damage done to fetuses often has been wrongly connected to cocaine, many experts say.
''The consensus, I think, at this point is that most of the adverse effects that had been reported due to cocaine and crack use were from alcohol use,'' said Dr. Kenneth R. Warren, the director of the office of scientific affairs at the National Institute on Alcohol Abuse and Alcoholism. ''It is the leading cause of birth defects due to an ingested environmental substance in this country.''
In 1973, researchers coined the phrase fetal alcohol syndrome to describe babies born with a certain pattern of neurologic and physiologic defects related to alcohol exposure in utero.
Early on, it was clear that exposed children were wired differently from normal ones and that they exhibited an array of disabilities.
Dr. Ann P. Streissguth, the director of the fetal alcohol and drug unit at the University of Washington and a professor at the medical school there, ticked off a list: ''These included attention problems, hyperactivity, learning problems -- particularly in arithmetic -- language problems, memory problems, fine and gross motor problems, poor impulse control, poor judgment, intellectual deficits and difficulty integrating past experience to plan and organize future behavior.''
Researchers wondered whether specific areas of the brain were being consistently harmed by alcohol exposure in utero. Poor judgment, for example, might point to damage to the frontal lobes. The lobes, as the control center of the brain, are involved in planning, organizing and inhibiting inappropriate responses, the researchers say.
Thirty years ago, the only way researchers could learn about the effects of alcohol on the brain was to study children who died shortly after birth.
''We knew from brain autopsies that in severe cases the brains were terribly disorganized,'' said Dr. Edward P. Riley, the director of the Center for Behavioral Teratology at San Diego State University. Now, researchers use imaging techniques like M.R.I.'s to look at the damage caused by alcohol. Several recent studies using magnetic resonance imaging have shown damage to the corpus callosum, a band of nerve fibers that connects the left and right sides of the brain.
A report published in 2002 compared the brain scans of adults and children who had severe or mild alcohol-related disabilities with the scans of healthy counterparts. The researchers found that the corpus callosa were abnormally shaped in 80 percent of those who had been exposed to alcohol in utero.
Another study found that the corpus callosum was smaller and shifted forward in children and young adults with the syndrome. Using a technique known as diffusion tensor imaging to look closer at the corpus callosum, researchers at Emory University have seen abnormalities in the myelin, the substance that insulates nerve cells.
When the myelin is damaged, signals do not carry as crisply through the cells, said Dr. Claire D. Coles, director of the Fetal Alcohol Center at the Marcus Institute and a professor of psychiatry and behavioral sciences at Emory.
Another study published in 2002 found that frontal lobe structures were smaller in teenagers and young adults who had been exposed to alcohol prenatally.
By pinpointing which sections of the brain are most likely to be damaged by alcohol, scientists may find a way to block its effects.
Researchers recently recognized that some of alcohol's effects were similar to those experienced by children born with defects in genes that control L1 adhesion cells. Fetal cells that are destined to grow into the brain and nervous system bind to one another with the help of adhesion molecules like L1, said Dr. Michael E. Charness, an associate professor of neurology at Harvard.
In laboratory experiments, Dr. Charness and his colleagues showed that alcohol could interfere with L1's stickiness, thus hampering crucial cell-to-cell attachments. In an article published in The Proceedings of the National Academy of Sciences in July, they showed that a protein, NAP, could block alcohol's effect on L1. When NAP was given to mice exposed to alcohol, the protein appeared to stave off neurological effects.
''The idea of giving drugs to pregnant women is controversial,'' Dr. Charness said. ''Drugs may have their own risks.''
But, he said, there are areas of the world where fetal alcohol syndrome is a huge problem. In parts of South Africa, the incidence of the syndrome in first graders is around 4.5 percent, he said. ''The rate of drinking is high,'' Dr. Charness added. ''And the women won't stop drinking despite interventions. It might be reasonable to give them a drug that can prevent the more serious effects of alcohol.''
Fertility : For Conception, Early Is Best
By Eric Nagourney : NY Times : December 31, 2002
Couples who are trying to have a baby should focus their efforts on the days leading up to ovulation, not on the day of ovulation itself, a new report advises.
The article, in this month's issue of Obstetrics & Gynecology, suggests that the best time to have intercourse may be the day before a woman ovulates. Repeated intercourse in the five days before ovulation will probably increase the odds of conception, the article said.
Researchers have known for some time that women are most fertile before ovulation, when an egg is released from the ovary and travels into the fallopian tube, said the lead author of the study, Dr. Joseph B. Stanford of the University of Utah. But many people trying to conceive are following the old theory that having intercourse on the day of ovulation is crucial, he said.
But by then, he added, it may be too late.
''A single act of intercourse during the fertile window that occurs on the day of ovulation may by chance occur sufficiently late in the 24-hour period that the ovum may have already lost its ability to become fertilized,'' the report said.
More than 10 percent of the couples in the United States have had trouble conceiving, the researchers said. While most of them will need medical help to have a baby, perhaps a quarter may be able to conceive with the timing right, Dr. Stanford said. ''This may be all they need,'' he said.
As for figuring out when ovulation will occur, the article said that the calendar and basal temperature techniques used by many people were of little use. More useful, it said, are some of the commercially available kits designed to predict ovulation.
By Eric Nagourney : NY Times : December 31, 2002
Couples who are trying to have a baby should focus their efforts on the days leading up to ovulation, not on the day of ovulation itself, a new report advises.
The article, in this month's issue of Obstetrics & Gynecology, suggests that the best time to have intercourse may be the day before a woman ovulates. Repeated intercourse in the five days before ovulation will probably increase the odds of conception, the article said.
Researchers have known for some time that women are most fertile before ovulation, when an egg is released from the ovary and travels into the fallopian tube, said the lead author of the study, Dr. Joseph B. Stanford of the University of Utah. But many people trying to conceive are following the old theory that having intercourse on the day of ovulation is crucial, he said.
But by then, he added, it may be too late.
''A single act of intercourse during the fertile window that occurs on the day of ovulation may by chance occur sufficiently late in the 24-hour period that the ovum may have already lost its ability to become fertilized,'' the report said.
More than 10 percent of the couples in the United States have had trouble conceiving, the researchers said. While most of them will need medical help to have a baby, perhaps a quarter may be able to conceive with the timing right, Dr. Stanford said. ''This may be all they need,'' he said.
As for figuring out when ovulation will occur, the article said that the calendar and basal temperature techniques used by many people were of little use. More useful, it said, are some of the commercially available kits designed to predict ovulation.
What Women Must Know About Fertility
By Jane E. Brody : NY Times : January 1, 2002
Childbearing has changed a lot in recent decades. As more career opportunities have opened for women, more women have chosen to delay starting a family, often waiting until ages when fertility is naturally in sharp decline.
While the probability of having a baby decreases by 3 percent to 5 percent a year after age 30 and even faster after age 40, one woman in five in the United States now has her first child after age 35. Since the mid-1970's the proportion of women in this country who have their first babies at age 30 and older has increased fourfold.
At the same time, threats to a woman's fertility have risen with the loosening of sexual mores and the switch from condoms and diaphragms to nonbarrier methods of contraception. The changes have increased the risk that a sexually transmitted disease will compromise the ability to conceive and bear a child.
Yet, as a recent Internet survey by the American Infertility Association indicated, women are woefully misinformed about their fertility and about what and when to do something to help matters along. Only one woman in 12,382 who completed the survey was able to correctly answer all 15 questions about reproduction. More than half the multiple-choice questions were answered incorrectly.
For example, 28 percent of women underestimated the risk of infertility, believing that it is one in 50 when actually one woman in 10 has great difficulty in conceiving a child. And 88 percent of the women overestimated by 5 to 10 years the age at which a woman's fertility began to decline (correct answer: in the late 20's). The chances of becoming pregnant in any one month, at 20 percent to 30 percent for women in their 30's, decrease to a mere 5 percent for women 40 and older who are trying to conceive.
Of course, being able to conceive is only part of the problem. As a woman ages, so does her chance of conceiving a child with a chromosomal abnormality, along with the risks of miscarriage, stillbirth or premature delivery.
While nearly every woman knows that modern medicine has developed techniques to help women with compromised fertility and complicated pregnancies, relatively few seem to be aware of the challenges -- financial, emotional and medical -- associated with these treatments, or with their often limited chance of success. Many couples readily talk about their childbearing success after in vitro fertilization, for example, but few who fail to have a child by medical intervention openly discuss the stress and costs associated with the failure.
Understanding Fertility
The goal of the American Infertility Association is not to encourage women to abandon careers or to start families before they are emotionally and financially ready. Rather, the association wants all women to be accurately informed about their reproductive cycle, when they are most likely to conceive, what they can do on their own to help matters along and how long they should wait before seeking professional assistance.
There are two crucial steps in conceiving a child. A woman must ovulate -- release a mature egg from one of her two ovaries -- and her partner must ejaculate tens of millions of mature, motile sperm. While sperm form throughout a man's reproductive life, a woman is born with all the eggs she will ever have. Over the years, her supply is depleted (of about seven million eggs present at birth, only 400 make it to ovulation) and the remaining eggs age, diminishing their reproductive capacity.
Next, one of those sperm must be able to reach and penetrate the egg as it travels from the ovary to the uterus. This fertilized egg must then be able to divide many times, implant in the uterus and form a placenta that is its lifeline until birth. If a woman's fallopian tubes have been damaged by a pelvic infection, or if she has suffered from severe endometriosis (misplaced growth of the uterine lining), fertilization or implantation may not be possible.
While a man can release sperm capable of fertilizing an egg at any time and sperm can live in a woman's body for several days, a woman with a normal menstrual cycle releases an egg once a month, and that egg can survive up to 24 hours.
Most couples trying to become pregnant would prefer to let nature take its course. But a woman past 30 for whom nature has been uncooperative for, say, three to six months, might want to think about helping nature along.
There are several approaches. The simplest is to chart the woman's menstrual cycle on a calendar. A woman is most likely to be fertile 10 to 14 days after the start of menstruation.
She can improve detection of ovulation by recording her basal body temperature. Using a special thermometer (available at pharmacies), she must take her temperature each morning after waking, before doing anything else (including going to the bathroom) and record the reading on a chart that comes with the thermometer. When she ovulates, her basal body temperature rises about one degree and remains elevated until her next period.
He Should Be Tested, Too
Other techniques include sampling the cervical mucus, which thins at ovulation to aid in transporting sperm, and measuring hormonal changes in urine -- estrogen levels rise at the start of a woman's most fertile period, and a rise in luteinizing hormone (L.H.) indicates that ovulation will most likely occur within 24 to 36 hours. Ovulation predictor kits, costing about $40, and reusable hormonal fertility monitors, about $100, are sold in pharmacies.
Of course, if a woman is regularly fertile but her partner is not, conception is likely to be compromised. Before a couple spends much time and money trying to conceive -- and certainly before a woman submits to medical tests of her fertility -- it is wise to have her partner's fertility tested. This can be done simply by delivering a semen sample to a reliable laboratory or male fertility specialist within two hours of ejaculation.
Sperm quality often declines in men over 50, and an age-associated drop in testosterone may lower libido and reduce attempts at copulation. A common problem in infertile men is a varicocele, or varicose vein in the testicles, that interferes with sperm development. Surgery can correct this problem in more than half of the cases.
How long should a couple wait to seek professional help in having a baby?
The infertility association recommends that for women under 35, the use of ovulation timing methods should be limited to a year, and those over 35 should not wait more than six months before consulting a physician who is expert in fertility matters.
By Jane E. Brody : NY Times : January 1, 2002
Childbearing has changed a lot in recent decades. As more career opportunities have opened for women, more women have chosen to delay starting a family, often waiting until ages when fertility is naturally in sharp decline.
While the probability of having a baby decreases by 3 percent to 5 percent a year after age 30 and even faster after age 40, one woman in five in the United States now has her first child after age 35. Since the mid-1970's the proportion of women in this country who have their first babies at age 30 and older has increased fourfold.
At the same time, threats to a woman's fertility have risen with the loosening of sexual mores and the switch from condoms and diaphragms to nonbarrier methods of contraception. The changes have increased the risk that a sexually transmitted disease will compromise the ability to conceive and bear a child.
Yet, as a recent Internet survey by the American Infertility Association indicated, women are woefully misinformed about their fertility and about what and when to do something to help matters along. Only one woman in 12,382 who completed the survey was able to correctly answer all 15 questions about reproduction. More than half the multiple-choice questions were answered incorrectly.
For example, 28 percent of women underestimated the risk of infertility, believing that it is one in 50 when actually one woman in 10 has great difficulty in conceiving a child. And 88 percent of the women overestimated by 5 to 10 years the age at which a woman's fertility began to decline (correct answer: in the late 20's). The chances of becoming pregnant in any one month, at 20 percent to 30 percent for women in their 30's, decrease to a mere 5 percent for women 40 and older who are trying to conceive.
Of course, being able to conceive is only part of the problem. As a woman ages, so does her chance of conceiving a child with a chromosomal abnormality, along with the risks of miscarriage, stillbirth or premature delivery.
While nearly every woman knows that modern medicine has developed techniques to help women with compromised fertility and complicated pregnancies, relatively few seem to be aware of the challenges -- financial, emotional and medical -- associated with these treatments, or with their often limited chance of success. Many couples readily talk about their childbearing success after in vitro fertilization, for example, but few who fail to have a child by medical intervention openly discuss the stress and costs associated with the failure.
Understanding Fertility
The goal of the American Infertility Association is not to encourage women to abandon careers or to start families before they are emotionally and financially ready. Rather, the association wants all women to be accurately informed about their reproductive cycle, when they are most likely to conceive, what they can do on their own to help matters along and how long they should wait before seeking professional assistance.
There are two crucial steps in conceiving a child. A woman must ovulate -- release a mature egg from one of her two ovaries -- and her partner must ejaculate tens of millions of mature, motile sperm. While sperm form throughout a man's reproductive life, a woman is born with all the eggs she will ever have. Over the years, her supply is depleted (of about seven million eggs present at birth, only 400 make it to ovulation) and the remaining eggs age, diminishing their reproductive capacity.
Next, one of those sperm must be able to reach and penetrate the egg as it travels from the ovary to the uterus. This fertilized egg must then be able to divide many times, implant in the uterus and form a placenta that is its lifeline until birth. If a woman's fallopian tubes have been damaged by a pelvic infection, or if she has suffered from severe endometriosis (misplaced growth of the uterine lining), fertilization or implantation may not be possible.
While a man can release sperm capable of fertilizing an egg at any time and sperm can live in a woman's body for several days, a woman with a normal menstrual cycle releases an egg once a month, and that egg can survive up to 24 hours.
Most couples trying to become pregnant would prefer to let nature take its course. But a woman past 30 for whom nature has been uncooperative for, say, three to six months, might want to think about helping nature along.
There are several approaches. The simplest is to chart the woman's menstrual cycle on a calendar. A woman is most likely to be fertile 10 to 14 days after the start of menstruation.
She can improve detection of ovulation by recording her basal body temperature. Using a special thermometer (available at pharmacies), she must take her temperature each morning after waking, before doing anything else (including going to the bathroom) and record the reading on a chart that comes with the thermometer. When she ovulates, her basal body temperature rises about one degree and remains elevated until her next period.
He Should Be Tested, Too
Other techniques include sampling the cervical mucus, which thins at ovulation to aid in transporting sperm, and measuring hormonal changes in urine -- estrogen levels rise at the start of a woman's most fertile period, and a rise in luteinizing hormone (L.H.) indicates that ovulation will most likely occur within 24 to 36 hours. Ovulation predictor kits, costing about $40, and reusable hormonal fertility monitors, about $100, are sold in pharmacies.
Of course, if a woman is regularly fertile but her partner is not, conception is likely to be compromised. Before a couple spends much time and money trying to conceive -- and certainly before a woman submits to medical tests of her fertility -- it is wise to have her partner's fertility tested. This can be done simply by delivering a semen sample to a reliable laboratory or male fertility specialist within two hours of ejaculation.
Sperm quality often declines in men over 50, and an age-associated drop in testosterone may lower libido and reduce attempts at copulation. A common problem in infertile men is a varicocele, or varicose vein in the testicles, that interferes with sperm development. Surgery can correct this problem in more than half of the cases.
How long should a couple wait to seek professional help in having a baby?
The infertility association recommends that for women under 35, the use of ovulation timing methods should be limited to a year, and those over 35 should not wait more than six months before consulting a physician who is expert in fertility matters.
Too Many Pills in Pregnancy
By Jane E. Body : NY Times : February 25, 2013
The thalidomide disaster of the early 1960s left thousands of babies with deformed limbs because their mothers innocently took a sleeping pill thought to be safe during pregnancy,
In its well-publicized wake, countless pregnant women avoided all medications, fearing that any drug they took could jeopardize their babies’ development.
I was terrified in December 1968 when, during the first weeks of my pregnancy, I developed double pneumonia and was treated with antibiotics and codeine. Before swallowing a single dose, I called my obstetrician, who told me to take what was prescribed, “reassuring” me that if I died of pneumonia I wouldn’t have a baby at all.
In the decades that followed, pregnancy-related hazards were linked to many medicinal substances: prescription and over-the-counter drugs and herbal remedies, as well as abused drugs and even some vitamins.
Now, however, the latest findings about drug use during pregnancy have ignited new concerns among experts who monitor the effects of medications on the developing fetus and pregnancy itself.
During the last 30 years, the use of prescription drugs during the first trimester of pregnancy, when fetal organs are forming, has grown by more than 60 percent.
About 90 percent of pregnant women take at least one medication, and 70 percent take at least one prescription drug.
Since the late 1970s, the proportion of pregnant women taking four or more medications has more than doubled.
Nearly one woman in 10 takes an herbal remedy during the first trimester.
A growing number of pregnant women, naïvely assuming safety, self-medicate with over-the-counter drugs that were once sold only by prescription.
While many commonly taken medications are considered safe for unborn babies, the Food and Drug Administration estimates that 10 percent or more of birth defects result from medications taken during pregnancy. “We seem to have forgotten as a society that drugs pose risks,” Dr. Allen A. Mitchell, professor of epidemiology and pediatrics at Boston University Schools of Public Health and Medicine, said in an interview. “Many over-the-counter drugs were grandfathered in with no studies of their possible effects during pregnancy.”
Medical progress has contributed to the rising use of medications during pregnancy, Dr. Mitchell said. Various conditions, like depression, are now recognized as diseases that warrant treatment; drugs have been developed to treat conditions for which no treatment was previously available, and some conditions, like Type 2 diabetes and hypertension, have become more prevalent.
Misled by the Web
Now a new concern has surfaced: Bypassing their doctors, more and more women are using the Internet to determine whether the medication they are taking or are about to take is safe for an unborn baby.
A study, published online last month in Pharmacoepidemiology and Drug Safety, of so-called “safe lists for medications in pregnancy” found at 25 Web sites revealed glaring inconsistencies and sometimes false reassurances or alarms based on “inadequate evidence.”
The report was prepared by Cheryl S. Broussard of the Centers for Disease Control and Prevention with co-authors from Emory, Georgia State University, the University of British Columbia and the Food and Drug Administration.
“Among medications approved for use in the U.S.A. from 2000 to 2010, over 79% had no published human data on which to assess teratogenic risk (potential to cause birth defects), and 98% had insufficient published data to characterize such risk,” the authors wrote.
But that did not stop the 25 Web sites from characterizing 245 medications as “safe” for use by pregnant women, which “might encourage use of medications during pregnancy even when they are not necessary,” the authors suggested.
Furthermore, the information found online was sometimes contradictory. “Twenty-two of the products listed as safe by one or more sites were stated not to be safe by one or more of the other sites,” the study found.
The question of timing was often ignored. A drug that could interfere with fetal organ development might be safe to take later in pregnancy. Or one (for example, ibuprofen) that is safe early in pregnancy could become a hazard later if it raises the risk of excessive bleeding or premature delivery.
Fewer than half the sites advised taking medication only when necessary, and only 13 sites encouraged pregnant women to consult their doctors before stopping or starting a medication.
Doctors, too, are often poorly informed about pregnancy-related hazards of various medications, the authors noted. One woman I know was advised to wean off an antidepressant before she became pregnant, but another was told to continue taking the same drug throughout her pregnancy.
“In many instances the best bet is for mom to stay on her medication,” said Dr. Siobhan M. Dolan, an obstetrician and geneticist at Albert Einstein College of Medicine. She said that if a woman is depressed during pregnancy, her risk of postpartum depression is greater and she may have difficulty bonding with her baby.
Dr. Dolan, who is author, with Alice Lesch Kelly, of the March of Dimes’ newest book, “Healthy Mom Healthy Baby,” emphasized the importance of weighing benefits and risks in deciding whether to take medication during pregnancy and which drugs to take.
“In anticipation of pregnancy, a woman taking more than one drug to treat her condition should try to get down to a single agent,” Dr. Dolan said in an interview. “Of the various medications available to treat a condition, is there a best choice — one least likely to cause a problem for either the baby or the mother?”
She cautioned against sharing medications prescribed for someone else and assuming that a remedy labeled “natural” or “herbal” is safe. Virtually none have been tested for safety in pregnancy.
Among medications a woman should be certain to avoid, in some cases starting three months before becoming pregnant, are isotretinoin (Accutane and others) for acne; valproic acid for seizure disorders; lithium for bipolar disorder; tetracycline for infections, and angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor antagonists for hypertension, Dr. Dolan said.
“Many medications that are not recommended during pregnancy can be replaced with low-risk alternatives,” she wrote.
Dr. Broussard, who did the “safe lists” study, said in an interview, “We’ve heard about women seeing medications on these lists and deciding on their own that it’s O.K. to take them. “Women who are pregnant or even thinking about getting pregnant should talk directly to their doctors before taking anything. They should be sure they’re taking only what’s necessary for their health condition.”
A reliable online resource for both women and their doctors, Dr. Mitchell said, are fact sheets prepared by OTIS, the Organization of Teratology Information Specialists, which are continually updated as new facts become available: http://www.otispregnancy.org.
By Jane E. Body : NY Times : February 25, 2013
The thalidomide disaster of the early 1960s left thousands of babies with deformed limbs because their mothers innocently took a sleeping pill thought to be safe during pregnancy,
In its well-publicized wake, countless pregnant women avoided all medications, fearing that any drug they took could jeopardize their babies’ development.
I was terrified in December 1968 when, during the first weeks of my pregnancy, I developed double pneumonia and was treated with antibiotics and codeine. Before swallowing a single dose, I called my obstetrician, who told me to take what was prescribed, “reassuring” me that if I died of pneumonia I wouldn’t have a baby at all.
In the decades that followed, pregnancy-related hazards were linked to many medicinal substances: prescription and over-the-counter drugs and herbal remedies, as well as abused drugs and even some vitamins.
Now, however, the latest findings about drug use during pregnancy have ignited new concerns among experts who monitor the effects of medications on the developing fetus and pregnancy itself.
During the last 30 years, the use of prescription drugs during the first trimester of pregnancy, when fetal organs are forming, has grown by more than 60 percent.
About 90 percent of pregnant women take at least one medication, and 70 percent take at least one prescription drug.
Since the late 1970s, the proportion of pregnant women taking four or more medications has more than doubled.
Nearly one woman in 10 takes an herbal remedy during the first trimester.
A growing number of pregnant women, naïvely assuming safety, self-medicate with over-the-counter drugs that were once sold only by prescription.
While many commonly taken medications are considered safe for unborn babies, the Food and Drug Administration estimates that 10 percent or more of birth defects result from medications taken during pregnancy. “We seem to have forgotten as a society that drugs pose risks,” Dr. Allen A. Mitchell, professor of epidemiology and pediatrics at Boston University Schools of Public Health and Medicine, said in an interview. “Many over-the-counter drugs were grandfathered in with no studies of their possible effects during pregnancy.”
Medical progress has contributed to the rising use of medications during pregnancy, Dr. Mitchell said. Various conditions, like depression, are now recognized as diseases that warrant treatment; drugs have been developed to treat conditions for which no treatment was previously available, and some conditions, like Type 2 diabetes and hypertension, have become more prevalent.
Misled by the Web
Now a new concern has surfaced: Bypassing their doctors, more and more women are using the Internet to determine whether the medication they are taking or are about to take is safe for an unborn baby.
A study, published online last month in Pharmacoepidemiology and Drug Safety, of so-called “safe lists for medications in pregnancy” found at 25 Web sites revealed glaring inconsistencies and sometimes false reassurances or alarms based on “inadequate evidence.”
The report was prepared by Cheryl S. Broussard of the Centers for Disease Control and Prevention with co-authors from Emory, Georgia State University, the University of British Columbia and the Food and Drug Administration.
“Among medications approved for use in the U.S.A. from 2000 to 2010, over 79% had no published human data on which to assess teratogenic risk (potential to cause birth defects), and 98% had insufficient published data to characterize such risk,” the authors wrote.
But that did not stop the 25 Web sites from characterizing 245 medications as “safe” for use by pregnant women, which “might encourage use of medications during pregnancy even when they are not necessary,” the authors suggested.
Furthermore, the information found online was sometimes contradictory. “Twenty-two of the products listed as safe by one or more sites were stated not to be safe by one or more of the other sites,” the study found.
The question of timing was often ignored. A drug that could interfere with fetal organ development might be safe to take later in pregnancy. Or one (for example, ibuprofen) that is safe early in pregnancy could become a hazard later if it raises the risk of excessive bleeding or premature delivery.
Fewer than half the sites advised taking medication only when necessary, and only 13 sites encouraged pregnant women to consult their doctors before stopping or starting a medication.
Doctors, too, are often poorly informed about pregnancy-related hazards of various medications, the authors noted. One woman I know was advised to wean off an antidepressant before she became pregnant, but another was told to continue taking the same drug throughout her pregnancy.
“In many instances the best bet is for mom to stay on her medication,” said Dr. Siobhan M. Dolan, an obstetrician and geneticist at Albert Einstein College of Medicine. She said that if a woman is depressed during pregnancy, her risk of postpartum depression is greater and she may have difficulty bonding with her baby.
Dr. Dolan, who is author, with Alice Lesch Kelly, of the March of Dimes’ newest book, “Healthy Mom Healthy Baby,” emphasized the importance of weighing benefits and risks in deciding whether to take medication during pregnancy and which drugs to take.
“In anticipation of pregnancy, a woman taking more than one drug to treat her condition should try to get down to a single agent,” Dr. Dolan said in an interview. “Of the various medications available to treat a condition, is there a best choice — one least likely to cause a problem for either the baby or the mother?”
She cautioned against sharing medications prescribed for someone else and assuming that a remedy labeled “natural” or “herbal” is safe. Virtually none have been tested for safety in pregnancy.
Among medications a woman should be certain to avoid, in some cases starting three months before becoming pregnant, are isotretinoin (Accutane and others) for acne; valproic acid for seizure disorders; lithium for bipolar disorder; tetracycline for infections, and angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor antagonists for hypertension, Dr. Dolan said.
“Many medications that are not recommended during pregnancy can be replaced with low-risk alternatives,” she wrote.
Dr. Broussard, who did the “safe lists” study, said in an interview, “We’ve heard about women seeing medications on these lists and deciding on their own that it’s O.K. to take them. “Women who are pregnant or even thinking about getting pregnant should talk directly to their doctors before taking anything. They should be sure they’re taking only what’s necessary for their health condition.”
A reliable online resource for both women and their doctors, Dr. Mitchell said, are fact sheets prepared by OTIS, the Organization of Teratology Information Specialists, which are continually updated as new facts become available: http://www.otispregnancy.org.
Can Mom's Medicine Hurt the Baby?
Few Studies Detail Prescription Drugs' Risk to Pregnant, Breast-Feeding Women
By Melinda Beck : WSJ : March 29, 2011
The list of medications that women shouldn't take in pregnancy keeps getting longer.
Earlier this month, the Food and Drug Administration strengthened warnings that expectant mothers who take topiramate (brand name Topamax), for migraines or to control seizures, have an increased risk of giving birth to babies with cleft lips or cleft palates.
The list of medications women shouldn't take when pregnant keeps getting longer. Kelsey Hubbard talks with WSJ's Melinda Beck about what drugs pose risks to expectant mothers and the hurdles to medical research in this field.
Last month, the FDA advised doctors that babies whose mothers took antipsychotic drugs such as Haldol, Zyprexa, Seroquel and Abilify, could suffer withdrawal symptoms such as agitation and difficulty breathing and feeding for hours or days after birth. It also warned that terbutaline, an asthma drug also used to halt preterm labor, should not be used by pregnant women due to the potential for maternal heart problems or death.
Also last month, the Centers for Disease Control and Prevention warned that taking pain relievers containing opioids, such as Vicodin, OxyContin and Tylenol with codeine, just before or in early pregnancy increased the risk of congenital heart defects, glaucoma and other problems.
Ever since the 1960s when thalidomide, a sleep aid and morning-sickness drug, was linked to more than 10,000 babies born with missing or shrunken limbs, it has been known that medications a pregnant woman takes can cross the placenta and affect her unborn child.
But determining what the impact might be for tens of thousands of medications is a Herculean task. The labels on most medicines have little or no information on how they might affect the mother or the fetus, other than advising to check with her doctor. Physicians are often baffled too, since conclusive data on safety in pregnancy don't exist for the majority of prescription medications.
There is not much more known about the safety of over-the-counter drugs. Most experts believe that acetaminophen (Tylenol) is safe to use in all trimesters. But many advise pregnant women not to take aspirin, ibuprofen and some other nonsteroidal anti-inflammatory drugs (NSAIDs), particularly in the third trimester, due to the potential for excess bleeding and other labor complications. Meanwhile, small studies have linked pseudoephedrine, a common ingredient in decongestants and other cold remedies, with a higher risk of gastroschisis, in which the baby's intestines grow outside the abdominal wall. Antacids are generally safe, although sodium bicarbonate is absorbed into the bloodstream and can raise a woman's sodium level.
There's so little safety information because it is considered unethical to expose pregnant women and unborn babies to potential risks in randomized-controlled clinical trials used to test drug safety. Yet millions of pregnant women take medications. Studies show that 64% use at least one prescription drug during pregnancy and, on average, women use three to five.
Experts agree that chronic conditions such as asthma, epilepsy, high blood pressure and depression can't go untreated for nine months without posing risks to both mothers and fetuses. For example, if a mother has a severe asthma attack or prolonged seizure, the fetus could be starved for oxygen; untreated hypertension in a mother could stunt her baby's growth or cause preterm labor.
So doctors must carefully weigh the benefits of a medication to both mother and baby against the often uncertain risk that it might interfere with fetal development. Many of the most serious medication risks occur when a baby's vital organs are forming in the first trimester, often before a woman knows she's pregnant.
To manage the uncertainty, the FDA in 1979 set up a system rating drugs' safety in pregnancy based on what data exist. Very few drugs are in category A, meaning that there are large, well-controlled studies demonstrating safety for human fetuses. Those in category B are believed safe but have less evidence. More than 60% of drugs are in category C, with no information on the risk to humans. Drugs in category D have been shown to pose some harm to human fetuses, but the potential benefits may outweigh to risks. Drugs in category X have either such a clear risk of harm or so little benefit to pregnant women that there is no justification for their use.
The rating system has been criticized for years as open to misinterpretation. "You may have drugs with no evidence of reproductive toxicity at all, and drugs where a few animal offspring showed some malformations and drugs where studies showed the same malformations in three different species, and they're all lumped together in category C," says Karen Feibus, a lead medical officer at the FDA. The agency in 2008 proposed eliminating the categories and requiring drug labels to include a summary of the drug's known risks in pregnancy, along with clinical considerations for doctors. That rule is now being finalized.
The FDA is also drafting new guidelines to help drug makers find ways to include pregnant women in clinical trials. "Pregnant women get sick, and sick women get pregnant. This is a reality," says Dr. Feibus.
In the meantime, the FDA has encouraged drug companies and other groups to set up registries to monitor how pregnant women who do opt to take prescription medications and their babies fare. More than 40 such registries are up and running, and some have alerted the FDA to some dangers drugs pose to fetal development.
Even so, the absolute risk that a mother taking topiramate would have a baby with cleft issues remains very small: 1.4% of babies exposed to topiramate in the womb was born with an oral cleft, compared with 0.38% to 0.55% of those whose mothers took other antiseizure drugs and .07% of those whose mother didn't have epilepsy.
In some cases, mothers and doctors can opt for a substitute medication for the condition that's thought to pose less risk. There is a wide variety of antidepressants, for example, with different associated risks. The popular category called serotonin-reuptake inhibitors (SSRIs) is generally considered safe, although some studies have linked a few of them to a higher risk of congential heart defects when taken in the first trimester, and infants suffering withdrawal symptoms such as irritability and seizures for more than a week after birth.
All this information creates some hard choices for mothers-to-be and their health-care providers. Sarah Lieberman Weisz, 36, of Chicago, who takes Wellbutrin, a category C drug for depression, talked it over with her midwife before her first pregnancy. Even though several other antidepressants are considered to be safer during pregnancy, Ms. Weisz had tried others and was reluctant to switch. They found some small-scale studies showing no adverse effects on human fetuses, and no large studies contradicting them. "To me, that was enough. We decided that the risk of switching and suffering more depression or new side effects was greater than a possible risk to the baby," says Ms. Weisz, who had a healthy baby boy in 21 months ago and a healthy, baby girl last month.
Few Studies Detail Prescription Drugs' Risk to Pregnant, Breast-Feeding Women
By Melinda Beck : WSJ : March 29, 2011
The list of medications that women shouldn't take in pregnancy keeps getting longer.
Earlier this month, the Food and Drug Administration strengthened warnings that expectant mothers who take topiramate (brand name Topamax), for migraines or to control seizures, have an increased risk of giving birth to babies with cleft lips or cleft palates.
The list of medications women shouldn't take when pregnant keeps getting longer. Kelsey Hubbard talks with WSJ's Melinda Beck about what drugs pose risks to expectant mothers and the hurdles to medical research in this field.
Last month, the FDA advised doctors that babies whose mothers took antipsychotic drugs such as Haldol, Zyprexa, Seroquel and Abilify, could suffer withdrawal symptoms such as agitation and difficulty breathing and feeding for hours or days after birth. It also warned that terbutaline, an asthma drug also used to halt preterm labor, should not be used by pregnant women due to the potential for maternal heart problems or death.
Also last month, the Centers for Disease Control and Prevention warned that taking pain relievers containing opioids, such as Vicodin, OxyContin and Tylenol with codeine, just before or in early pregnancy increased the risk of congenital heart defects, glaucoma and other problems.
Ever since the 1960s when thalidomide, a sleep aid and morning-sickness drug, was linked to more than 10,000 babies born with missing or shrunken limbs, it has been known that medications a pregnant woman takes can cross the placenta and affect her unborn child.
But determining what the impact might be for tens of thousands of medications is a Herculean task. The labels on most medicines have little or no information on how they might affect the mother or the fetus, other than advising to check with her doctor. Physicians are often baffled too, since conclusive data on safety in pregnancy don't exist for the majority of prescription medications.
There is not much more known about the safety of over-the-counter drugs. Most experts believe that acetaminophen (Tylenol) is safe to use in all trimesters. But many advise pregnant women not to take aspirin, ibuprofen and some other nonsteroidal anti-inflammatory drugs (NSAIDs), particularly in the third trimester, due to the potential for excess bleeding and other labor complications. Meanwhile, small studies have linked pseudoephedrine, a common ingredient in decongestants and other cold remedies, with a higher risk of gastroschisis, in which the baby's intestines grow outside the abdominal wall. Antacids are generally safe, although sodium bicarbonate is absorbed into the bloodstream and can raise a woman's sodium level.
There's so little safety information because it is considered unethical to expose pregnant women and unborn babies to potential risks in randomized-controlled clinical trials used to test drug safety. Yet millions of pregnant women take medications. Studies show that 64% use at least one prescription drug during pregnancy and, on average, women use three to five.
Experts agree that chronic conditions such as asthma, epilepsy, high blood pressure and depression can't go untreated for nine months without posing risks to both mothers and fetuses. For example, if a mother has a severe asthma attack or prolonged seizure, the fetus could be starved for oxygen; untreated hypertension in a mother could stunt her baby's growth or cause preterm labor.
So doctors must carefully weigh the benefits of a medication to both mother and baby against the often uncertain risk that it might interfere with fetal development. Many of the most serious medication risks occur when a baby's vital organs are forming in the first trimester, often before a woman knows she's pregnant.
To manage the uncertainty, the FDA in 1979 set up a system rating drugs' safety in pregnancy based on what data exist. Very few drugs are in category A, meaning that there are large, well-controlled studies demonstrating safety for human fetuses. Those in category B are believed safe but have less evidence. More than 60% of drugs are in category C, with no information on the risk to humans. Drugs in category D have been shown to pose some harm to human fetuses, but the potential benefits may outweigh to risks. Drugs in category X have either such a clear risk of harm or so little benefit to pregnant women that there is no justification for their use.
The rating system has been criticized for years as open to misinterpretation. "You may have drugs with no evidence of reproductive toxicity at all, and drugs where a few animal offspring showed some malformations and drugs where studies showed the same malformations in three different species, and they're all lumped together in category C," says Karen Feibus, a lead medical officer at the FDA. The agency in 2008 proposed eliminating the categories and requiring drug labels to include a summary of the drug's known risks in pregnancy, along with clinical considerations for doctors. That rule is now being finalized.
The FDA is also drafting new guidelines to help drug makers find ways to include pregnant women in clinical trials. "Pregnant women get sick, and sick women get pregnant. This is a reality," says Dr. Feibus.
In the meantime, the FDA has encouraged drug companies and other groups to set up registries to monitor how pregnant women who do opt to take prescription medications and their babies fare. More than 40 such registries are up and running, and some have alerted the FDA to some dangers drugs pose to fetal development.
Even so, the absolute risk that a mother taking topiramate would have a baby with cleft issues remains very small: 1.4% of babies exposed to topiramate in the womb was born with an oral cleft, compared with 0.38% to 0.55% of those whose mothers took other antiseizure drugs and .07% of those whose mother didn't have epilepsy.
In some cases, mothers and doctors can opt for a substitute medication for the condition that's thought to pose less risk. There is a wide variety of antidepressants, for example, with different associated risks. The popular category called serotonin-reuptake inhibitors (SSRIs) is generally considered safe, although some studies have linked a few of them to a higher risk of congential heart defects when taken in the first trimester, and infants suffering withdrawal symptoms such as irritability and seizures for more than a week after birth.
All this information creates some hard choices for mothers-to-be and their health-care providers. Sarah Lieberman Weisz, 36, of Chicago, who takes Wellbutrin, a category C drug for depression, talked it over with her midwife before her first pregnancy. Even though several other antidepressants are considered to be safer during pregnancy, Ms. Weisz had tried others and was reluctant to switch. They found some small-scale studies showing no adverse effects on human fetuses, and no large studies contradicting them. "To me, that was enough. We decided that the risk of switching and suffering more depression or new side effects was greater than a possible risk to the baby," says Ms. Weisz, who had a healthy baby boy in 21 months ago and a healthy, baby girl last month.
The Risks and Demands of Pregnancy
After 20
By Jane E. Brody : NY Times : May 11, 2004
Biologically speaking, the ideal age at which to have a baby is between 18 and 20. That is when pregnancy is most likely to produce a healthy full-term child with the least risk to the health of the mother. Considered from an evolutionary perspective, this makes sense too, since a child born to an 18-year-old would reach independence when the mother was 36. That mother would then live another 10 or so years to help out with the grandchildren, fostering the perpetuation of the species.
Today, however, millions of American women are postponing marriage and childbearing until their mid- to late-30's, the age at which our forebears became grandparents. Currently in this country, one in five women has her first child after 35.
Unfortunately, one-third of women who wait until then to try to become pregnant are finding themselves infertile. With each passing year beyond 20, in fact, the likelihood of a successful pregnancy declines. Among women over 40, half will require medical assistance if they want to conceive.
Even then, conception does not guarantee a happy outcome for several reasons. Older women are more likely to suffer pregnancy complications; genetic abnormalities are more common in their fetuses; and the miscarriage rate rises as the fertility rate falls.
The effect of age on men's fertility is less clear. There is a small decline in sperm numbers and motility -- the ability of sperm to swim to an egg -- in men over 45. But even though these characteristics are less robust than in younger men, they usually remain within normal limits until about age 70. However, men over 40 are more likely to produce genetically damaged sperm and can transmit these defects, which cannot always be found through amniocentesis, to their offspring.
Why Does Fertility Decline?
For decades, the difficulty older women faced in becoming pregnant was attributed primarily to two factors: the declining frequency of intercourse among older couples and the aging and depletion of a woman's eggs, all of which were believed to be present when a girl is born. Experts no longer believe that coital frequency is a factor, and a new study in mice by researchers in Boston suggests that female mammals are capable of making new eggs throughout their reproductive lives.
What this means to an older woman's fertility potential is not yet known, but what is known is that the supply of healthy eggs is only one factor -- and perhaps not the most important one -- influencing the ability of a woman to conceive and deliver a healthy child in her waning reproductive years.
Writing in the current issue of the journal Contemporary Ob/Gyn, Dr. Shirley Fong and Dr. Peter McGovern review what recent studies have revealed to explain why a woman's fertility declines steadily after age 20 and precipitously after age 35. Dr. Fong is a fellow and Dr. McGovern is director of reproductive endocrinology and infertility at the Department of Obstetrics, Gynecology and Women's Health at the University of Medicine and Dentistry of New Jersey in Newark.
Even if a woman turns out to be capable of producing new eggs throughout her reproductive life span, older eggs remain a factor, the experts stated. An older egg is readily fertilized, but the resulting embryo has a harder time implanting in the uterus, where a placenta must form to provide a circulatory connection to the mother that nourishes and supports the fetus during its development. The placenta also produces hormones necessary for a successful pregnancy.
Older women have a higher incidence of uterine fibroids, benign tumors that can interfere with the attachment of the embryo to the uterine lining. Also, the lining of the uterus in older women appears to be less receptive to an embryo, possibly because their fertilized eggs produce an insufficient amount of the hormone progesterone, needed to maintain an early pregnancy until placenta production of progesterone takes over at about eight weeks. Implantation rates decline at age 30, and by age 40 are half that of a young woman. Older women receiving donor eggs are commonly treated with progesterone to improve implantation rates.
Older eggs, once fertilized, also are more likely to divide abnormally, resulting in a genetically damaged embryo. Studies of embryos formed through in vitro fertilization showed that those of older women are five times more likely to have chromosomal disorders. The overwhelming problem is errors made when the chromosomes in the egg fail to separate properly during cell division.
Higher Miscarriage Rates
A result of all these problems is a dramatic rise in miscarriage rates in older women. Miscarriage occurs in 10 percent of women under 30 but in a third of women in their early 40's, with the greatest increase occurring after 35.
To reduce the rate of pregnancy loss among women undergoing I.V.F., preimplantation genetic analysis is now frequently performed on the early embryos formed from the eggs of older women. Sometimes all the embryos in an I.V.F. cycle are found to be affected, which means none are suitable for implantation. However, this technique has significantly reduced miscarriage rates and increased the probability that a woman undergoing I.V.F. will give birth to a genetically healthy baby.
Studies of infertile women who receive donor eggs show that problems with genetic abnormalities and miscarriage are related to the age of the egg. Most donor eggs come from women in their 20's, and the rates of miscarriage and chromosome errors match those of the donor, not the recipient. In fact, up to the late 40's, the Society of Reproductive Technology has reported, pregnancy rates are not affected by the age of a woman who conceives through egg donation. Not until age 50 and above are the rates of implantation, pregnancy and delivery significantly reduced in women receiving donor eggs.
Pregnancy is an assault on a woman's body, and the older a woman, the less resilient her body is likely to be at meeting the many demands on it to support fetal growth and development. The fetus, after all, is a true parasite, taking everything it needs from its host.
The demands on a woman's body are further increased by a multiple pregnancy. Even without assisted reproduction, older women are more likely to conceive fraternal twins because, as women age, their ovarian follicles tend to release more than one egg at a time, Drs. Fong and McGovern explained.
Pregnancy in older women is associated with higher rates of three maternal health problems: gestational diabetes, pre-eclampsia (high blood pressure in pregnancy) and thrombophlebitis, the formation of blood clots. These problems can threaten the well-being and even the life of the mother and her fetus. They are not related to an older woman's older eggs because they occur with equal frequency in older women who become pregnant with a donated egg.
The risk of developing one or more of these obstetrical complications rises when a women is pregnant with two or more fetuses, as might occur naturally in older women and as occurs often in women having I.V.F.
None of this means that an older woman should not try to become pregnant. But she should be aware of the risks involved and be emotionally prepared and strong enough to withstand the disappointment should the effort fail.
After 20
By Jane E. Brody : NY Times : May 11, 2004
Biologically speaking, the ideal age at which to have a baby is between 18 and 20. That is when pregnancy is most likely to produce a healthy full-term child with the least risk to the health of the mother. Considered from an evolutionary perspective, this makes sense too, since a child born to an 18-year-old would reach independence when the mother was 36. That mother would then live another 10 or so years to help out with the grandchildren, fostering the perpetuation of the species.
Today, however, millions of American women are postponing marriage and childbearing until their mid- to late-30's, the age at which our forebears became grandparents. Currently in this country, one in five women has her first child after 35.
Unfortunately, one-third of women who wait until then to try to become pregnant are finding themselves infertile. With each passing year beyond 20, in fact, the likelihood of a successful pregnancy declines. Among women over 40, half will require medical assistance if they want to conceive.
Even then, conception does not guarantee a happy outcome for several reasons. Older women are more likely to suffer pregnancy complications; genetic abnormalities are more common in their fetuses; and the miscarriage rate rises as the fertility rate falls.
The effect of age on men's fertility is less clear. There is a small decline in sperm numbers and motility -- the ability of sperm to swim to an egg -- in men over 45. But even though these characteristics are less robust than in younger men, they usually remain within normal limits until about age 70. However, men over 40 are more likely to produce genetically damaged sperm and can transmit these defects, which cannot always be found through amniocentesis, to their offspring.
Why Does Fertility Decline?
For decades, the difficulty older women faced in becoming pregnant was attributed primarily to two factors: the declining frequency of intercourse among older couples and the aging and depletion of a woman's eggs, all of which were believed to be present when a girl is born. Experts no longer believe that coital frequency is a factor, and a new study in mice by researchers in Boston suggests that female mammals are capable of making new eggs throughout their reproductive lives.
What this means to an older woman's fertility potential is not yet known, but what is known is that the supply of healthy eggs is only one factor -- and perhaps not the most important one -- influencing the ability of a woman to conceive and deliver a healthy child in her waning reproductive years.
Writing in the current issue of the journal Contemporary Ob/Gyn, Dr. Shirley Fong and Dr. Peter McGovern review what recent studies have revealed to explain why a woman's fertility declines steadily after age 20 and precipitously after age 35. Dr. Fong is a fellow and Dr. McGovern is director of reproductive endocrinology and infertility at the Department of Obstetrics, Gynecology and Women's Health at the University of Medicine and Dentistry of New Jersey in Newark.
Even if a woman turns out to be capable of producing new eggs throughout her reproductive life span, older eggs remain a factor, the experts stated. An older egg is readily fertilized, but the resulting embryo has a harder time implanting in the uterus, where a placenta must form to provide a circulatory connection to the mother that nourishes and supports the fetus during its development. The placenta also produces hormones necessary for a successful pregnancy.
Older women have a higher incidence of uterine fibroids, benign tumors that can interfere with the attachment of the embryo to the uterine lining. Also, the lining of the uterus in older women appears to be less receptive to an embryo, possibly because their fertilized eggs produce an insufficient amount of the hormone progesterone, needed to maintain an early pregnancy until placenta production of progesterone takes over at about eight weeks. Implantation rates decline at age 30, and by age 40 are half that of a young woman. Older women receiving donor eggs are commonly treated with progesterone to improve implantation rates.
Older eggs, once fertilized, also are more likely to divide abnormally, resulting in a genetically damaged embryo. Studies of embryos formed through in vitro fertilization showed that those of older women are five times more likely to have chromosomal disorders. The overwhelming problem is errors made when the chromosomes in the egg fail to separate properly during cell division.
Higher Miscarriage Rates
A result of all these problems is a dramatic rise in miscarriage rates in older women. Miscarriage occurs in 10 percent of women under 30 but in a third of women in their early 40's, with the greatest increase occurring after 35.
To reduce the rate of pregnancy loss among women undergoing I.V.F., preimplantation genetic analysis is now frequently performed on the early embryos formed from the eggs of older women. Sometimes all the embryos in an I.V.F. cycle are found to be affected, which means none are suitable for implantation. However, this technique has significantly reduced miscarriage rates and increased the probability that a woman undergoing I.V.F. will give birth to a genetically healthy baby.
Studies of infertile women who receive donor eggs show that problems with genetic abnormalities and miscarriage are related to the age of the egg. Most donor eggs come from women in their 20's, and the rates of miscarriage and chromosome errors match those of the donor, not the recipient. In fact, up to the late 40's, the Society of Reproductive Technology has reported, pregnancy rates are not affected by the age of a woman who conceives through egg donation. Not until age 50 and above are the rates of implantation, pregnancy and delivery significantly reduced in women receiving donor eggs.
Pregnancy is an assault on a woman's body, and the older a woman, the less resilient her body is likely to be at meeting the many demands on it to support fetal growth and development. The fetus, after all, is a true parasite, taking everything it needs from its host.
The demands on a woman's body are further increased by a multiple pregnancy. Even without assisted reproduction, older women are more likely to conceive fraternal twins because, as women age, their ovarian follicles tend to release more than one egg at a time, Drs. Fong and McGovern explained.
Pregnancy in older women is associated with higher rates of three maternal health problems: gestational diabetes, pre-eclampsia (high blood pressure in pregnancy) and thrombophlebitis, the formation of blood clots. These problems can threaten the well-being and even the life of the mother and her fetus. They are not related to an older woman's older eggs because they occur with equal frequency in older women who become pregnant with a donated egg.
The risk of developing one or more of these obstetrical complications rises when a women is pregnant with two or more fetuses, as might occur naturally in older women and as occurs often in women having I.V.F.
None of this means that an older woman should not try to become pregnant. But she should be aware of the risks involved and be emotionally prepared and strong enough to withstand the disappointment should the effort fail.
35 and Pregnant?
Assessing Risk Becomes Easier
By Jane E. Brody : NY Times : December 27, 2005
Dawn will be 35 when her first child is born in April. Based on her age alone, she has 1 chance in 270 that her fetus has Down syndrome, a genetic defect caused by an extra chromosome that results in mental retardation and other problems.
In recent decades, many thousands of older women have been offered the option of having an invasive test - amniocentesis, or more recently chorionic villus sampling, known as C.V.S. - to find out for sure whether their babies would be born with the syndrome. The tests are costly and can sometimes result in miscarriage, not a happy outcome for any woman who wants a baby, let alone an older woman who may have tried for years to become pregnant.
But Dawn, who lives in Brooklyn, did not have to rely on age alone to decide whether to have an invasive test to determine the likelihood that her baby would be free of this serious abnormality.
Testing Blood and Sound
Instead, in the first 12 weeks of her pregnancy, she had three noninvasive tests, an ultrasound of the fetus and two blood tests. A third blood test, in the second trimester, showed a drastically reduced risk of Down syndrome, 1 in 9,000.
"With such a low risk, I'm not going to have amniocentesis," Dawn said.
For older pregnant women who would consider aborting a fetus with Down syndrome, noninvasive screening is fast becoming standard care in gynecological practices. And it now appears that such screening can be completed with great accuracy in the first trimester, before anyone other than the woman, her partner and her physician need know that she is pregnant.
Based on a newly published study of more than 38,000 pregnant women, 117 of whom had a fetus with Down syndrome, a combination of three noninvasive tests conducted at 11 to 13 weeks of gestation was 87 percent accurate in predicting the presence of the syndrome in the fetus.
The tests are an ultrasound evaluation of the thickness of the fetal neck, called nuchal translucency, and two blood tests, pregnancy-associated plasma protein A, or PAPP-A, and beta human chorionic gonadotropin, or H.C.G. Adding a second ultrasound of the fetal nasal bone may push the accuracy of these tests even higher, according to an editorial accompanying a report last month in The New England Journal of Medicine.
These are indeed exciting findings, especially since many more women are now delaying pregnancy into their mid-30's and beyond, when the risk of Down syndrome increases exponentially. For those women who would consider aborting an affected fetus, the opportunity to assess the risk of Down by noninvasive tests early in pregnancy can be so reassuring that most would willingly forgo the riskier invasive procedures.
In the editorial, Dr. Joe Leigh Simpson of the departments of obstetrics and gynecology and molecular and human genetics at Baylor College of Medicine in Houston recounted the progress in prenatal diagnosis of Down syndrome.
In the 1970's, all that was available for prenatal screening was amniocentesis, a procedure done at about 18 weeks gestation in which a small sample of amniotic fluid surrounding the fetus is removed by a large needle inserted through the woman's abdomen. Fetal cells in the fluid are then analyzed for a possible chromosomal abnormality, a process that takes up to two weeks.
A Second-Trimester Decision
If an abnormality is found, the woman can choose to have a second-trimester abortion, which is physically and emotionally more traumatic than one performed earlier in pregnancy.
In the 1980's, researchers established that certain blood tests in the second trimester could predict the risk of Down syndrome in the fetus and thus enable many women to avoid having amniocentesis. These tests measured alpha-fetoprotein, or AFP; a hormone called unconjugated estriol; and H.C.G. in a woman's blood. Later, a fourth blood test for inhibin A improved the ability to predict the presence of the syndrome. Taken together, the results of these tests provided a risk estimate that could be higher or lower, often much lower, than that based solely on a woman's age.
But the goal was earlier determination of risk and, as Dr. Simpson wrote, "a dazzling series of noninvasive screening options for trisomy 21," the extra chromosome causing the defect, emerged. In the first trimester, an ultrasound exam that measured fetal nuchal translucency and maternal blood tests for PAPP-A and H.C.G. were shown to be effective in estimating the risk of Down syndrome. Detection rates above 80 percent of affected fetuses were demonstrated using these first-trimester tests.
One major study of 44,613 pregnancies, directed by Dr. K. H. Nicolaides and published last year in The American Journal of Obstetrics & Gynecology, found a detection rate of 87 percent using measures of nuchal translucency, PAPP-A and H.C.G. Adding the absence or presence of the fetal nasal bone increased the detection rate to 97 percent, with 5 percent of the women undergoing an invasive procedure.
More Effective Testing
The new study compared the accuracy of first-trimester screening with that of second-trimester screening and a combination of both. It found that screening at 11 weeks of gestation was 87 percent accurate, and more accurate than screening one or two weeks later. The most accurate prediction, 96 percent, occurred when the tests at 11 weeks were combined with four noninvasive tests in the second trimester.
Thus, the detection rate associated with tests in the second trimester was really no better than what Dr. Nicolaides and others found with first-trimester screening, which can result in many fewer invasive tests and allow for safer, earlier terminations of affected pregnancies.
Of course, for a woman who wants to know for sure in her first trimester that her fetus is free of the syndrome, chorionic villus sampling can be done at about 10 or 11 weeks of gestation or, if she is further along in her pregnancy, she can have amniocentesis at 16 weeks.
As Dr. Simpson said, "In experienced hands, neither procedure seems to be as risky as once thought." So, women whose risk of having a child with Down syndrome is high based on the noninvasive tests - as well as those seeking certainty about the absence of this genetic defect regardless of their risk- can be less concerned about miscarriages resulting from C.V.S. or amniocentesis.
There are even better options on the horizon, Dr. Simpson said. Under study now is the ability to examine the fetal chromosomes in cells found in the woman's blood or in fetal cells shed into her cervix. Such studies would provide definitive evidence of the presence or absence not only of Down, but also of other genetic disorders that might run in the family. Such determinations could be made from only one noninvasive test and without having to do a single invasive one.
As a result of such progress, women who will be 35 or older when their babies are born and who are willing to consider abortion could obtain a high level of reassurance by having noninvasive tests in their first trimester.
Most important to the accuracy of this risk assessment is having the ultrasound exam done with the most modern equipment by a highly skilled sonographer who is experienced at measuring nuchal translucency. Even better would be a sonographer who could reliably determine the presence of a nasal bone in the fetus.
Assessing Risk Becomes Easier
By Jane E. Brody : NY Times : December 27, 2005
Dawn will be 35 when her first child is born in April. Based on her age alone, she has 1 chance in 270 that her fetus has Down syndrome, a genetic defect caused by an extra chromosome that results in mental retardation and other problems.
In recent decades, many thousands of older women have been offered the option of having an invasive test - amniocentesis, or more recently chorionic villus sampling, known as C.V.S. - to find out for sure whether their babies would be born with the syndrome. The tests are costly and can sometimes result in miscarriage, not a happy outcome for any woman who wants a baby, let alone an older woman who may have tried for years to become pregnant.
But Dawn, who lives in Brooklyn, did not have to rely on age alone to decide whether to have an invasive test to determine the likelihood that her baby would be free of this serious abnormality.
Testing Blood and Sound
Instead, in the first 12 weeks of her pregnancy, she had three noninvasive tests, an ultrasound of the fetus and two blood tests. A third blood test, in the second trimester, showed a drastically reduced risk of Down syndrome, 1 in 9,000.
"With such a low risk, I'm not going to have amniocentesis," Dawn said.
For older pregnant women who would consider aborting a fetus with Down syndrome, noninvasive screening is fast becoming standard care in gynecological practices. And it now appears that such screening can be completed with great accuracy in the first trimester, before anyone other than the woman, her partner and her physician need know that she is pregnant.
Based on a newly published study of more than 38,000 pregnant women, 117 of whom had a fetus with Down syndrome, a combination of three noninvasive tests conducted at 11 to 13 weeks of gestation was 87 percent accurate in predicting the presence of the syndrome in the fetus.
The tests are an ultrasound evaluation of the thickness of the fetal neck, called nuchal translucency, and two blood tests, pregnancy-associated plasma protein A, or PAPP-A, and beta human chorionic gonadotropin, or H.C.G. Adding a second ultrasound of the fetal nasal bone may push the accuracy of these tests even higher, according to an editorial accompanying a report last month in The New England Journal of Medicine.
These are indeed exciting findings, especially since many more women are now delaying pregnancy into their mid-30's and beyond, when the risk of Down syndrome increases exponentially. For those women who would consider aborting an affected fetus, the opportunity to assess the risk of Down by noninvasive tests early in pregnancy can be so reassuring that most would willingly forgo the riskier invasive procedures.
In the editorial, Dr. Joe Leigh Simpson of the departments of obstetrics and gynecology and molecular and human genetics at Baylor College of Medicine in Houston recounted the progress in prenatal diagnosis of Down syndrome.
In the 1970's, all that was available for prenatal screening was amniocentesis, a procedure done at about 18 weeks gestation in which a small sample of amniotic fluid surrounding the fetus is removed by a large needle inserted through the woman's abdomen. Fetal cells in the fluid are then analyzed for a possible chromosomal abnormality, a process that takes up to two weeks.
A Second-Trimester Decision
If an abnormality is found, the woman can choose to have a second-trimester abortion, which is physically and emotionally more traumatic than one performed earlier in pregnancy.
In the 1980's, researchers established that certain blood tests in the second trimester could predict the risk of Down syndrome in the fetus and thus enable many women to avoid having amniocentesis. These tests measured alpha-fetoprotein, or AFP; a hormone called unconjugated estriol; and H.C.G. in a woman's blood. Later, a fourth blood test for inhibin A improved the ability to predict the presence of the syndrome. Taken together, the results of these tests provided a risk estimate that could be higher or lower, often much lower, than that based solely on a woman's age.
But the goal was earlier determination of risk and, as Dr. Simpson wrote, "a dazzling series of noninvasive screening options for trisomy 21," the extra chromosome causing the defect, emerged. In the first trimester, an ultrasound exam that measured fetal nuchal translucency and maternal blood tests for PAPP-A and H.C.G. were shown to be effective in estimating the risk of Down syndrome. Detection rates above 80 percent of affected fetuses were demonstrated using these first-trimester tests.
One major study of 44,613 pregnancies, directed by Dr. K. H. Nicolaides and published last year in The American Journal of Obstetrics & Gynecology, found a detection rate of 87 percent using measures of nuchal translucency, PAPP-A and H.C.G. Adding the absence or presence of the fetal nasal bone increased the detection rate to 97 percent, with 5 percent of the women undergoing an invasive procedure.
More Effective Testing
The new study compared the accuracy of first-trimester screening with that of second-trimester screening and a combination of both. It found that screening at 11 weeks of gestation was 87 percent accurate, and more accurate than screening one or two weeks later. The most accurate prediction, 96 percent, occurred when the tests at 11 weeks were combined with four noninvasive tests in the second trimester.
Thus, the detection rate associated with tests in the second trimester was really no better than what Dr. Nicolaides and others found with first-trimester screening, which can result in many fewer invasive tests and allow for safer, earlier terminations of affected pregnancies.
Of course, for a woman who wants to know for sure in her first trimester that her fetus is free of the syndrome, chorionic villus sampling can be done at about 10 or 11 weeks of gestation or, if she is further along in her pregnancy, she can have amniocentesis at 16 weeks.
As Dr. Simpson said, "In experienced hands, neither procedure seems to be as risky as once thought." So, women whose risk of having a child with Down syndrome is high based on the noninvasive tests - as well as those seeking certainty about the absence of this genetic defect regardless of their risk- can be less concerned about miscarriages resulting from C.V.S. or amniocentesis.
There are even better options on the horizon, Dr. Simpson said. Under study now is the ability to examine the fetal chromosomes in cells found in the woman's blood or in fetal cells shed into her cervix. Such studies would provide definitive evidence of the presence or absence not only of Down, but also of other genetic disorders that might run in the family. Such determinations could be made from only one noninvasive test and without having to do a single invasive one.
As a result of such progress, women who will be 35 or older when their babies are born and who are willing to consider abortion could obtain a high level of reassurance by having noninvasive tests in their first trimester.
Most important to the accuracy of this risk assessment is having the ultrasound exam done with the most modern equipment by a highly skilled sonographer who is experienced at measuring nuchal translucency. Even better would be a sonographer who could reliably determine the presence of a nasal bone in the fetus.
Dispelling Pregnancy Myths: Eating for 1.5
By Jane E. Brody : NY Times : July 24, 2007
Ivy had been eating tuna sushi almost every day. But before becoming pregnant, she wisely had a checkup, which revealed high levels of mercury in her blood that could damage a fetus. Shocked, she stopped eating tuna and postponed pregnancy until the mercury had cleared her system. Last month she gave birth to a full-term healthy boy.
Mercury from eating certain kinds of seafood is just one of many nutrition-related hazards that can confront a pregnant woman or one who wishes to become pregnant. At the same time, some pregnant women worry needlessly about nonexistent nutritional risks.
The March of Dimes, which strives to make every pregnancy as well-planned and successful as Ivy’s, is making a new push to dispel nutritional misinformation and replace it with advice based on solid scientific evidence. Some of the advice may come as a distressing surprise to women, who may be fond of foods or drinks that could endanger their pregnancy.
For example, pregnant women are advised to steer clear of deli meats, including sliced turkey, unless they are fully cooked again before being eaten. But the March of Dimes, among other experts, suggests that it is safe to drink one or two cups of caffeinated coffee a day during pregnancy, whereas consuming too much herbal tea (and three or more cups of coffee a day) can be risky and may result in a miscarriage.
A Healthy Diet
The organization is also concerned about the current notion among some women that it is O.K. to gain 40 or more pounds when pregnant with one baby. Excessive weight gain in pregnancy not only makes it harder to shed the extra pounds after childbirth. It also increases the risk to the mother of gestational diabetes, dangerous rises in blood pressure (pre-eclampsia), the need for a Caesarean delivery and postpartum infection. For the baby, a mother’s excessive weight gain raises the risk of neural tube defects, birth trauma and fetal death near term.
Studies of tens of thousands of pregnancies showed that how much a pregnant woman should gain for the best chance of a healthy outcome for both mother and baby depends on how much she weighed before becoming pregnant.
Accordingly, the March of Dimes suggests that normal-weight women should gain 25 to 35 pounds; overweight women 15 to 25 pounds, and underweight women 28 to 40 pounds. But a woman having a multiple birth should gain more, depending on how many babies she is carrying.
When a woman is eating for two, or better yet, when she is contemplating getting pregnant, is an ideal time to learn the principles of good nutrition and put them into practice. The basics of a healthy diet during pregnancy are the same as what everyone should eat at any time of life:
¶Whole grains, like brown rice, whole wheat bread or whole oat cereal: 6 to 11 servings a day
¶Dairy products, like low-fat or nonfat milk, yogurt or hard cheese: 3 to 4 servings a day
¶Protein, like meat, poultry, fish, beans, nuts or eggs: 3 to 4 servings a day
¶Vegetables, like broccoli, carrots, green beans, tomatoes or beets: 3 to 5 servings a day
¶Fruits, like oranges, bananas or apples: 2 to 4 servings a day
The trick is to know what a portion means because “eating for two” does not mean a woman should double her caloric intake. Only 300 additional calories a day are needed to sustain a healthy pregnancy, provided those calories come from nutritious foods.
Here are some examples of a single serving: one slice of bread, a half-cup of rice or pasta, one cup cold cereal; one cup milk or yogurt, two one-inch cubes of cheese; two ounces of cooked meat, poultry or fish, a half-cup of cooked dried beans, two tablespoons peanut butter; a half-cup of cooked or cut-up vegetables, one cup salad greens, three-quarters cup of vegetable juice; one apple, banana or orange, a half-cup of cut-up fruit, three-quarters cup of fruit juice.
Be sure, too, to drink plenty of water — up to 64 ounces a day — and get regular exercise. Pregnant women can walk, dance, swim and do yoga, but should avoid high-risk activities like scuba diving and skiing.
Foods to Avoid
Many popular foods are potentially dangerous during pregnancy. Pregnant women should refrain from the following:
Raw fish and shellfish, a possible source of the parasite Toxoplasma that can cause fetal blindness and brain damage.
Large predatory fish like swordfish, shark, king mackerel and albacore tuna (fresh or canned), which can contain risky levels of mercury. The Food and Drug Administration says to limit albacore tuna to 6 ounces a week, but it is acceptable to eat up to 12 ounces a week of chunk light tuna, shrimp, salmon, pollock and catfish.
Undercooked or raw meat, poultry and seafood. Use a meat thermometer and cook pork and ground beef to 160 degrees; beef, veal and lamb to 145 degrees; whole poultry to 180 degrees; and chicken breasts to 170 degrees.
Unpasteurized milk and soft cheeses — feta, Brie, Camembert, Roquefort, queso blanco, queso fresco and Panela, unless the label says “made with pasteurized milk.” They may contain the food-poisoning bacteria Listeria that can cause miscarriage, premature birth, stillbirth or fatal newborn illness.
Hot dogs and deli meats, unless cooked until steaming hot. These can become contaminated with Listeria after processing.
Refrigerated pâtés, meat spreads and smoked seafood (unless it is cooked before you eat it). Canned versions are safe.
Soft-scrambled eggs and foods like homemade salad dressing and eggnog made with raw or lightly cooked eggs. Cook eggs until the white and yolk are firm to avoid salmonella poisoning.
Raw sprouts, including alfalfa, clover, radish and mung bean.
Herbal teas and supplements. Their safety in pregnancy is unstudied. Some, like black cohosh or large amounts of chamomile tea, can raise the risk of miscarriage or premature birth.
Alcohol, which can cause fetal damage, including mental retardation and abnormal behavior. Although an occasional drink may be all right, no safe amount has been established.
Extra Vitamins Needed
Pregnant women and those contemplating pregnancy are advised to take a daily prenatal vitamin that contains 400 micrograms to 600 micrograms of folic acid to help prevent neural tube defects, as well as 18 milligrams to 27 milligrams of iron to prevent iron-deficiency anemia, linked to premature birth and low birth weight babies.
But prenatal supplements do not contain enough calcium; 1,000 milligrams a day are needed to protect a pregnant woman’s bones and build strong bones and teeth in her baby. Be sure to eat enough calcium-rich foods, like milk, cheese and leafy greens, or take a calcium supplement daily.
By Jane E. Brody : NY Times : July 24, 2007
Ivy had been eating tuna sushi almost every day. But before becoming pregnant, she wisely had a checkup, which revealed high levels of mercury in her blood that could damage a fetus. Shocked, she stopped eating tuna and postponed pregnancy until the mercury had cleared her system. Last month she gave birth to a full-term healthy boy.
Mercury from eating certain kinds of seafood is just one of many nutrition-related hazards that can confront a pregnant woman or one who wishes to become pregnant. At the same time, some pregnant women worry needlessly about nonexistent nutritional risks.
The March of Dimes, which strives to make every pregnancy as well-planned and successful as Ivy’s, is making a new push to dispel nutritional misinformation and replace it with advice based on solid scientific evidence. Some of the advice may come as a distressing surprise to women, who may be fond of foods or drinks that could endanger their pregnancy.
For example, pregnant women are advised to steer clear of deli meats, including sliced turkey, unless they are fully cooked again before being eaten. But the March of Dimes, among other experts, suggests that it is safe to drink one or two cups of caffeinated coffee a day during pregnancy, whereas consuming too much herbal tea (and three or more cups of coffee a day) can be risky and may result in a miscarriage.
A Healthy Diet
The organization is also concerned about the current notion among some women that it is O.K. to gain 40 or more pounds when pregnant with one baby. Excessive weight gain in pregnancy not only makes it harder to shed the extra pounds after childbirth. It also increases the risk to the mother of gestational diabetes, dangerous rises in blood pressure (pre-eclampsia), the need for a Caesarean delivery and postpartum infection. For the baby, a mother’s excessive weight gain raises the risk of neural tube defects, birth trauma and fetal death near term.
Studies of tens of thousands of pregnancies showed that how much a pregnant woman should gain for the best chance of a healthy outcome for both mother and baby depends on how much she weighed before becoming pregnant.
Accordingly, the March of Dimes suggests that normal-weight women should gain 25 to 35 pounds; overweight women 15 to 25 pounds, and underweight women 28 to 40 pounds. But a woman having a multiple birth should gain more, depending on how many babies she is carrying.
When a woman is eating for two, or better yet, when she is contemplating getting pregnant, is an ideal time to learn the principles of good nutrition and put them into practice. The basics of a healthy diet during pregnancy are the same as what everyone should eat at any time of life:
¶Whole grains, like brown rice, whole wheat bread or whole oat cereal: 6 to 11 servings a day
¶Dairy products, like low-fat or nonfat milk, yogurt or hard cheese: 3 to 4 servings a day
¶Protein, like meat, poultry, fish, beans, nuts or eggs: 3 to 4 servings a day
¶Vegetables, like broccoli, carrots, green beans, tomatoes or beets: 3 to 5 servings a day
¶Fruits, like oranges, bananas or apples: 2 to 4 servings a day
The trick is to know what a portion means because “eating for two” does not mean a woman should double her caloric intake. Only 300 additional calories a day are needed to sustain a healthy pregnancy, provided those calories come from nutritious foods.
Here are some examples of a single serving: one slice of bread, a half-cup of rice or pasta, one cup cold cereal; one cup milk or yogurt, two one-inch cubes of cheese; two ounces of cooked meat, poultry or fish, a half-cup of cooked dried beans, two tablespoons peanut butter; a half-cup of cooked or cut-up vegetables, one cup salad greens, three-quarters cup of vegetable juice; one apple, banana or orange, a half-cup of cut-up fruit, three-quarters cup of fruit juice.
Be sure, too, to drink plenty of water — up to 64 ounces a day — and get regular exercise. Pregnant women can walk, dance, swim and do yoga, but should avoid high-risk activities like scuba diving and skiing.
Foods to Avoid
Many popular foods are potentially dangerous during pregnancy. Pregnant women should refrain from the following:
Raw fish and shellfish, a possible source of the parasite Toxoplasma that can cause fetal blindness and brain damage.
Large predatory fish like swordfish, shark, king mackerel and albacore tuna (fresh or canned), which can contain risky levels of mercury. The Food and Drug Administration says to limit albacore tuna to 6 ounces a week, but it is acceptable to eat up to 12 ounces a week of chunk light tuna, shrimp, salmon, pollock and catfish.
Undercooked or raw meat, poultry and seafood. Use a meat thermometer and cook pork and ground beef to 160 degrees; beef, veal and lamb to 145 degrees; whole poultry to 180 degrees; and chicken breasts to 170 degrees.
Unpasteurized milk and soft cheeses — feta, Brie, Camembert, Roquefort, queso blanco, queso fresco and Panela, unless the label says “made with pasteurized milk.” They may contain the food-poisoning bacteria Listeria that can cause miscarriage, premature birth, stillbirth or fatal newborn illness.
Hot dogs and deli meats, unless cooked until steaming hot. These can become contaminated with Listeria after processing.
Refrigerated pâtés, meat spreads and smoked seafood (unless it is cooked before you eat it). Canned versions are safe.
Soft-scrambled eggs and foods like homemade salad dressing and eggnog made with raw or lightly cooked eggs. Cook eggs until the white and yolk are firm to avoid salmonella poisoning.
Raw sprouts, including alfalfa, clover, radish and mung bean.
Herbal teas and supplements. Their safety in pregnancy is unstudied. Some, like black cohosh or large amounts of chamomile tea, can raise the risk of miscarriage or premature birth.
Alcohol, which can cause fetal damage, including mental retardation and abnormal behavior. Although an occasional drink may be all right, no safe amount has been established.
Extra Vitamins Needed
Pregnant women and those contemplating pregnancy are advised to take a daily prenatal vitamin that contains 400 micrograms to 600 micrograms of folic acid to help prevent neural tube defects, as well as 18 milligrams to 27 milligrams of iron to prevent iron-deficiency anemia, linked to premature birth and low birth weight babies.
But prenatal supplements do not contain enough calcium; 1,000 milligrams a day are needed to protect a pregnant woman’s bones and build strong bones and teeth in her baby. Be sure to eat enough calcium-rich foods, like milk, cheese and leafy greens, or take a calcium supplement daily.
PCOS: An Infertility Issue That Is Little Understood
Jane E. Brody : NY Times : November 24, 2014
Sometimes medical syndromes are named long before they are fully understood.
Take polycystic ovarian syndrome, or PCOS, which affects as many as 10 percent of women of childbearing age, often impairing their fertility.
But not all of these women have polycystic ovaries, a fact that can result in misdiagnosis. As it turns out, cysts — sacs of fluid on the ovaries — are just one manifestation of a complex hormonal condition.
First described in 1935, PCOS was initially called Stein-Leventhal syndrome, for the two American gynecologists who identified it, Dr. Irving F. Stein Sr. and Dr. Michael L. Leventhal. They recognized that ovarian cysts can interrupt ovulation and cause infertility in significant numbers of women.
Irregular menstrual cycles and difficulty conceiving are among the most common symptoms, the result of ovarian follicles that fail to mature fully and to release eggs. Affected women often have enlarged ovaries and, when menses does occur, prolonged bleeding.
Over time more cysts — swollen follicles, really — may form. On an ultrasound exam, they resemble a string of pearls stretched over the surface of the ovary. Yet some experts believe cysts are a result, rather than the cause, of the syndrome.
“Whether the condition starts in the ovaries is not certain,” Dr. R. Scott Lucidi, an expert on PCOS at Virginia Commonwealth University, said in an interview.
Indeed, women with few or no ovarian cysts may be diagnosed with PCOS. According to the so-called Rotterdam criteria, a woman with any two of the following conditions may have the condition:
■ Symptoms of elevated levels of androgens, or male sex hormones, which can include acne, excessive hairiness and sometimes male-pattern hair loss.
■ Irregular menses, with prolonged periods between cycles.
■ Twelve or more follicular cysts on the ovaries, as seen on an ultrasound.
Dr. Lucidi and others have suggested that insulin resistance could be the underlying factor responsible for the disparate symptoms of PCOS.
In people resistant to insulin, the hormone does not effectively transfer glucose from blood to body cells to be used for energy. As blood levels of glucose build, more insulin is produced to try to lower it.
Excess insulin promotes fat storage and can result in weight gain and obesity. About half of American women with PCOS are obese. Insulin also can stimulate the ovaries to produce androgens.
But just as some young women with a lot of ovarian cysts do not have PCOS, some women with metabolic syndrome and insulin resistance are thin.
PCOS tends to cluster in families, with predisposing genes passed from either parent to both daughters and sons. In affected males, early balding or excessive hairiness can be a sign that the genes have been inherited. In women, symptoms can vary from being very mild to extensive.
Some experts believe that the fundamental defect may not be insulin resistance, but hormonal dysregulation by or of the hypothalamus. This small region at the base of the brain produces hormones that stimulate the pituitary gland, which in turn affects organs throughout the body.
In most women with PCOS, the pituitary gland produces excessive amounts of luteinizing hormone, which, like insulin, can stimulate the ovaries to secrete androgens, according to a practice guideline written by Dr. Robert L. Barbieri, head of obstetrics and gynecology at Brigham and Women’s Hospital in Boston.
When ovarian follicles are enlarging, women with PCOS also produce high levels of estradiol but low levels of progesterone, resulting in a thick uterine lining and over time an increased risk of endometrial cancer.
There is no cure for PCOS, and the best approach to treatment is individualized, depending on the goals of each patient, Dr. Lucidi said.
For women with prolonged intervals between menses or excessive hairiness, or both, contraceptives containing estrogen and progestin are used to regulate the menstrual cycle and suppress the production of androgens.
Often, the blood pressure drug spironolactone is also given to counteract androgen-caused acne or hirsutism in adult women.
For a woman trying to become pregnant, a different regimen is needed. Two drugs, clomiphene and letrozole, are commonly prescribed to stimulate ovulation. Both these drugs prompt the pituitary to secrete follicle-stimulating hormone (FSH), which enhances the growth of small follicles and thus can trigger ovulation.
Dr. Barbieri noted that “most women with PCOS who undergo ovulation induction go on to conceive and bear children.” Perhaps the most challenging therapy involves weight reduction. Losing 10 percent of body weight can result in more regular menstrual cycles and reduced levels of testosterone, Dr. Barbieri wrote.
For women with PCOS, the most effective diet for achieving and maintaining weight loss is low in carbohydrates, rather than low in fat.
Without being extreme, women with PCOS should reduce their carbohydrate intake overall and in particular avoid sugars and refined carbohydrates (white bread, white rice and anything stripped of its natural fiber or made with refined white flour).
They should instead select foods high in fiber made from whole grains, as unprocessed as possible. They are also advised to avoid eating carbohydrate-rich foods by themselves, and space them out during the day to keep insulin levels from spiking. Consuming four or more small meals instead of a few large ones each day is also helpful.
Regular moderate or vigorous exercise done five or more times a week is an important part of the regimen.
Jane E. Brody : NY Times : November 24, 2014
Sometimes medical syndromes are named long before they are fully understood.
Take polycystic ovarian syndrome, or PCOS, which affects as many as 10 percent of women of childbearing age, often impairing their fertility.
But not all of these women have polycystic ovaries, a fact that can result in misdiagnosis. As it turns out, cysts — sacs of fluid on the ovaries — are just one manifestation of a complex hormonal condition.
First described in 1935, PCOS was initially called Stein-Leventhal syndrome, for the two American gynecologists who identified it, Dr. Irving F. Stein Sr. and Dr. Michael L. Leventhal. They recognized that ovarian cysts can interrupt ovulation and cause infertility in significant numbers of women.
Irregular menstrual cycles and difficulty conceiving are among the most common symptoms, the result of ovarian follicles that fail to mature fully and to release eggs. Affected women often have enlarged ovaries and, when menses does occur, prolonged bleeding.
Over time more cysts — swollen follicles, really — may form. On an ultrasound exam, they resemble a string of pearls stretched over the surface of the ovary. Yet some experts believe cysts are a result, rather than the cause, of the syndrome.
“Whether the condition starts in the ovaries is not certain,” Dr. R. Scott Lucidi, an expert on PCOS at Virginia Commonwealth University, said in an interview.
Indeed, women with few or no ovarian cysts may be diagnosed with PCOS. According to the so-called Rotterdam criteria, a woman with any two of the following conditions may have the condition:
■ Symptoms of elevated levels of androgens, or male sex hormones, which can include acne, excessive hairiness and sometimes male-pattern hair loss.
■ Irregular menses, with prolonged periods between cycles.
■ Twelve or more follicular cysts on the ovaries, as seen on an ultrasound.
Dr. Lucidi and others have suggested that insulin resistance could be the underlying factor responsible for the disparate symptoms of PCOS.
In people resistant to insulin, the hormone does not effectively transfer glucose from blood to body cells to be used for energy. As blood levels of glucose build, more insulin is produced to try to lower it.
Excess insulin promotes fat storage and can result in weight gain and obesity. About half of American women with PCOS are obese. Insulin also can stimulate the ovaries to produce androgens.
But just as some young women with a lot of ovarian cysts do not have PCOS, some women with metabolic syndrome and insulin resistance are thin.
PCOS tends to cluster in families, with predisposing genes passed from either parent to both daughters and sons. In affected males, early balding or excessive hairiness can be a sign that the genes have been inherited. In women, symptoms can vary from being very mild to extensive.
Some experts believe that the fundamental defect may not be insulin resistance, but hormonal dysregulation by or of the hypothalamus. This small region at the base of the brain produces hormones that stimulate the pituitary gland, which in turn affects organs throughout the body.
In most women with PCOS, the pituitary gland produces excessive amounts of luteinizing hormone, which, like insulin, can stimulate the ovaries to secrete androgens, according to a practice guideline written by Dr. Robert L. Barbieri, head of obstetrics and gynecology at Brigham and Women’s Hospital in Boston.
When ovarian follicles are enlarging, women with PCOS also produce high levels of estradiol but low levels of progesterone, resulting in a thick uterine lining and over time an increased risk of endometrial cancer.
There is no cure for PCOS, and the best approach to treatment is individualized, depending on the goals of each patient, Dr. Lucidi said.
For women with prolonged intervals between menses or excessive hairiness, or both, contraceptives containing estrogen and progestin are used to regulate the menstrual cycle and suppress the production of androgens.
Often, the blood pressure drug spironolactone is also given to counteract androgen-caused acne or hirsutism in adult women.
For a woman trying to become pregnant, a different regimen is needed. Two drugs, clomiphene and letrozole, are commonly prescribed to stimulate ovulation. Both these drugs prompt the pituitary to secrete follicle-stimulating hormone (FSH), which enhances the growth of small follicles and thus can trigger ovulation.
Dr. Barbieri noted that “most women with PCOS who undergo ovulation induction go on to conceive and bear children.” Perhaps the most challenging therapy involves weight reduction. Losing 10 percent of body weight can result in more regular menstrual cycles and reduced levels of testosterone, Dr. Barbieri wrote.
For women with PCOS, the most effective diet for achieving and maintaining weight loss is low in carbohydrates, rather than low in fat.
Without being extreme, women with PCOS should reduce their carbohydrate intake overall and in particular avoid sugars and refined carbohydrates (white bread, white rice and anything stripped of its natural fiber or made with refined white flour).
They should instead select foods high in fiber made from whole grains, as unprocessed as possible. They are also advised to avoid eating carbohydrate-rich foods by themselves, and space them out during the day to keep insulin levels from spiking. Consuming four or more small meals instead of a few large ones each day is also helpful.
Regular moderate or vigorous exercise done five or more times a week is an important part of the regimen.
Nausea? There’s No Need to Suffer in Silence
By Jane E. Brody : NY Times : October 24, 2006
Anyone who has ever been nauseated knows what an awful feeling it is. Yet for millions of Americans, nausea and its frequent aftermath, vomiting, are facts of life that occur periodically over many months.
Although there are now safe and effective ways to prevent and to treat predictable cases, like those involving pregnant women and cancer patients, many people who could benefit fail to receive adequate treatment, if any treatment at all.
Common in Pregnancy
In the 1960’s, a friend of mine spent her two pregnancies nauseated and vomiting. By the time her sons were born, she looked like a poorly nourished scarecrow. Fortunately, both babies, true to their role as parasites, were hale and hearty at birth. Another friend soon to give birth to twins was so sick during her first trimester that she hardly left the house, and she lost weight instead of gaining it.
Infants of those severely afflicted through their pregnancies — the condition is known medically as hyperemesis gravidarum — typically have lower than normal birth weights for their gestational age. Up to 2 percent of pregnant women experience such severe and protracted vomiting that hospitalization is necessary to keep them from becoming dangerously dehydrated and to keep their weight up.
Nausea and vomiting affects 70 to 85 percent of pregnant women for varying lengths of time. Half of pregnant women have both nausea and vomiting, a quarter have nausea only and the remaining quarter are spared. For many women, nausea and vomiting is their first indication that they are pregnant. Typically, the distress dissipates after about 12 weeks, and women who experience it are often reassured by friends and relatives that it is an indication of a healthy pregnancy. Indeed, there is a lower rate of miscarriage among women with nausea and vomiting of any severity; even hyperemesis gravidarum most often results in a good outcome.
Alas, for large numbers of pregnant women, so-called morning sickness, although it can occur at any and all hours of the day, is often minimized by their physicians and thus undertreated, according to a report in 2004 from the American College of Obstetricians and Gynecologists.
In a clinical guidance bulletin for obstetrician-gynecologists, the college wrote that an investigator found that among women who called a help line for those with nausea and vomiting during pregnancy and who subsequently terminated pregnancy because of these afflictions, fewer than 50 percent were offered anti-emetic therapy.
“Of those offered treatment, 90 percent were offered regimens that were not likely to be effective,” the bulletin says. “Furthermore, some women do not seek treatment because of concerns about safety.”
It is true that most women today are terrified of taking any medication during pregnancy. Some may remember the voluntary withdrawal of the drug Bendectin by Merrell Dow after a barrage of lawsuits amid claims that it caused birth defects. At the time, Bendectin (doxylamine) was being used by about a quarter of pregnant women to relieve nausea and vomiting.
Since then multiple studies have exonerated the drug and found it to be safe and effective. In the hierarchy of remedies for nausea and vomiting due to pregnancy, the practice bulletin ranks a combination of doxylamine and vitamin B6 among “first-line therapies.” The drug combination can be legally prescribed and prepared by compounding pharmacies upon request.
Other drugs deemed safe and effective include phenothiazines and trimethobenzamide.
Before going the drug route, however, there are lifestyle and diet options that are effective for many women, according to the March of Dimes. Most important:
¶Eat frequent small meals, five or six a day. Hence the classic advice to keep crackers at the bedside and to consume several before getting up in the morning.
¶Get up slowly in the morning, sitting on the bed for a few minutes before standing up.
¶Eat snacks high in protein, like nuts and peanut butter.
¶Drink fluids often during the day, including broth, cola and a sports drink like Gatorade.
¶Get plenty of fresh air.
¶Avoid smells that you find unpleasant and foods that are hard to digest, like fatty foods.
¶Avoid drinking citrus juice, milk, coffee and tea with meals.
Capsules of powdered ginger have been found in a few studies to reduce episodes of nausea and vomiting in pregnant women.
Effect of Cancer Therapy
Several of the most effective drugs used to treat cancer, as well as radiation therapy involving the digestive tract, cause nausea and vomiting for up to 75 percent of people treated, and it is the side effect most feared by cancer patients.
If untreated, nausea and vomiting caused by cancer therapy can result in dehydration, fatigue, difficulty concentrating, slow healing of wounds and loss of appetite, according to a bulletin produced by the American Cancer Society and National Comprehensive Cancer Network.
Many cancer patients insist that marijuana is the best remedy for this problem. But the United States Supreme Court has refused efforts to legalize marijuana as a medical treatment.
Even without marijuana, however, most patients do not have to suffer. There are now quite a few legal remedies that can treat and even prevent nausea and vomiting. Most often, the anti-nausea remedy is started before the chemotherapy is administered.
The treatments selected are determined by how likely the therapy is to cause nausea and vomiting. For example, for chemotherapy low on the nausea scale, Compazine may be used.
Using Drugs in Combination
For therapies more likely to cause nausea and vomiting, two anti-nausea drugs may be used in combination. One such remedy recently approved by the Food and Drug Administration is Emend, by Merck. Taking one capsule a day for three days starting before chemotherapy can help prevent nausea and vomiting. Emend may be combined with another drug when chemotherapy, for example high-dosage cisplatin, is highly likely to cause nausea and vomiting.
Other helpful measures include acupuncture, biofeedback and relaxation techniques.
The cancer bulletin recommends the following: eat frequent small meals; eat at least an hour before your treatment; avoid fried and fatty foods; restrict fluids with meals; eat foods cold or at room temperature; have someone else prepare meals if you feel nauseated; limit exposure to sounds, sights and smells that cause nausea; avoid favorite foods when nauseated; wear loose-fitting clothes; and freshen the air with a fan or open window. Make sure, too, to let your health care team know if the remedies you try do not control your nausea.
Free copies of the bulletin, Nausea and Vomiting Treatment Guidelines for Patients With Cancer, can be ordered through the Web sites www.nccn.org and www.cancer.org, or by calling 1-888-909-NCCN or 1-800-ACS-2345.
By Jane E. Brody : NY Times : October 24, 2006
Anyone who has ever been nauseated knows what an awful feeling it is. Yet for millions of Americans, nausea and its frequent aftermath, vomiting, are facts of life that occur periodically over many months.
Although there are now safe and effective ways to prevent and to treat predictable cases, like those involving pregnant women and cancer patients, many people who could benefit fail to receive adequate treatment, if any treatment at all.
Common in Pregnancy
In the 1960’s, a friend of mine spent her two pregnancies nauseated and vomiting. By the time her sons were born, she looked like a poorly nourished scarecrow. Fortunately, both babies, true to their role as parasites, were hale and hearty at birth. Another friend soon to give birth to twins was so sick during her first trimester that she hardly left the house, and she lost weight instead of gaining it.
Infants of those severely afflicted through their pregnancies — the condition is known medically as hyperemesis gravidarum — typically have lower than normal birth weights for their gestational age. Up to 2 percent of pregnant women experience such severe and protracted vomiting that hospitalization is necessary to keep them from becoming dangerously dehydrated and to keep their weight up.
Nausea and vomiting affects 70 to 85 percent of pregnant women for varying lengths of time. Half of pregnant women have both nausea and vomiting, a quarter have nausea only and the remaining quarter are spared. For many women, nausea and vomiting is their first indication that they are pregnant. Typically, the distress dissipates after about 12 weeks, and women who experience it are often reassured by friends and relatives that it is an indication of a healthy pregnancy. Indeed, there is a lower rate of miscarriage among women with nausea and vomiting of any severity; even hyperemesis gravidarum most often results in a good outcome.
Alas, for large numbers of pregnant women, so-called morning sickness, although it can occur at any and all hours of the day, is often minimized by their physicians and thus undertreated, according to a report in 2004 from the American College of Obstetricians and Gynecologists.
In a clinical guidance bulletin for obstetrician-gynecologists, the college wrote that an investigator found that among women who called a help line for those with nausea and vomiting during pregnancy and who subsequently terminated pregnancy because of these afflictions, fewer than 50 percent were offered anti-emetic therapy.
“Of those offered treatment, 90 percent were offered regimens that were not likely to be effective,” the bulletin says. “Furthermore, some women do not seek treatment because of concerns about safety.”
It is true that most women today are terrified of taking any medication during pregnancy. Some may remember the voluntary withdrawal of the drug Bendectin by Merrell Dow after a barrage of lawsuits amid claims that it caused birth defects. At the time, Bendectin (doxylamine) was being used by about a quarter of pregnant women to relieve nausea and vomiting.
Since then multiple studies have exonerated the drug and found it to be safe and effective. In the hierarchy of remedies for nausea and vomiting due to pregnancy, the practice bulletin ranks a combination of doxylamine and vitamin B6 among “first-line therapies.” The drug combination can be legally prescribed and prepared by compounding pharmacies upon request.
Other drugs deemed safe and effective include phenothiazines and trimethobenzamide.
Before going the drug route, however, there are lifestyle and diet options that are effective for many women, according to the March of Dimes. Most important:
¶Eat frequent small meals, five or six a day. Hence the classic advice to keep crackers at the bedside and to consume several before getting up in the morning.
¶Get up slowly in the morning, sitting on the bed for a few minutes before standing up.
¶Eat snacks high in protein, like nuts and peanut butter.
¶Drink fluids often during the day, including broth, cola and a sports drink like Gatorade.
¶Get plenty of fresh air.
¶Avoid smells that you find unpleasant and foods that are hard to digest, like fatty foods.
¶Avoid drinking citrus juice, milk, coffee and tea with meals.
Capsules of powdered ginger have been found in a few studies to reduce episodes of nausea and vomiting in pregnant women.
Effect of Cancer Therapy
Several of the most effective drugs used to treat cancer, as well as radiation therapy involving the digestive tract, cause nausea and vomiting for up to 75 percent of people treated, and it is the side effect most feared by cancer patients.
If untreated, nausea and vomiting caused by cancer therapy can result in dehydration, fatigue, difficulty concentrating, slow healing of wounds and loss of appetite, according to a bulletin produced by the American Cancer Society and National Comprehensive Cancer Network.
Many cancer patients insist that marijuana is the best remedy for this problem. But the United States Supreme Court has refused efforts to legalize marijuana as a medical treatment.
Even without marijuana, however, most patients do not have to suffer. There are now quite a few legal remedies that can treat and even prevent nausea and vomiting. Most often, the anti-nausea remedy is started before the chemotherapy is administered.
The treatments selected are determined by how likely the therapy is to cause nausea and vomiting. For example, for chemotherapy low on the nausea scale, Compazine may be used.
Using Drugs in Combination
For therapies more likely to cause nausea and vomiting, two anti-nausea drugs may be used in combination. One such remedy recently approved by the Food and Drug Administration is Emend, by Merck. Taking one capsule a day for three days starting before chemotherapy can help prevent nausea and vomiting. Emend may be combined with another drug when chemotherapy, for example high-dosage cisplatin, is highly likely to cause nausea and vomiting.
Other helpful measures include acupuncture, biofeedback and relaxation techniques.
The cancer bulletin recommends the following: eat frequent small meals; eat at least an hour before your treatment; avoid fried and fatty foods; restrict fluids with meals; eat foods cold or at room temperature; have someone else prepare meals if you feel nauseated; limit exposure to sounds, sights and smells that cause nausea; avoid favorite foods when nauseated; wear loose-fitting clothes; and freshen the air with a fan or open window. Make sure, too, to let your health care team know if the remedies you try do not control your nausea.
Free copies of the bulletin, Nausea and Vomiting Treatment Guidelines for Patients With Cancer, can be ordered through the Web sites www.nccn.org and www.cancer.org, or by calling 1-888-909-NCCN or 1-800-ACS-2345.
For Mother and Child, a Lurking Danger
By Jane E. Brody : NY Times : November 23, 2004
Obstetric researchers have done much in recent years to increase the safety and success of pregnancies among all women of reproductive age, even those approaching the end of their ability to conceive.
But in one important area - a disorder called preeclampsia -no significant improvement has occurred, even though its incidence has risen by nearly a third in the last decade.
Preeclampsia, formerly called toxemia of pregnancy, now affects about 5 to 8 percent of pregnant women and involves a dangerous increase in blood pressure, excessive swelling and excretion of protein in the urine as a result of kidney damage.
It typically starts after the 20th week of pregnancy and, if it progresses, can cause serious damage and even threaten the lives of mother and baby. The only known way to "cure" it is to deliver the baby, however prematurely.
Monitoring for early signs of preeclampsia is one reason that it is so important for all women to obtain prenatal care and keep their scheduled appointments. At every visit, the doctor or midwife should check the blood pressure and test the urine for protein.
In one famous case, the Pulitzer Prize-winning playwright Wendy Wasserstein, who was 48 when she became pregnant with the help of a fertility doctor, was hospitalized with preeclampsia in the sixth month. Sixteen days later, doctors had to perform a Caesarean section to deliver Lucy Jane at 1 pound 12 ounces. The baby spent two months in the neonatal intensive care unit.
Who Is at Risk?
Although there are no proven ways to prevent preeclampsia, certain conditions are known to increase a woman's chances of developing it.
Pregnancies late in life and those that involve two or more fetuses are the most prominent risk factors, and they account for the increasing incidence of preeclampsia.
A third common factor, also on the rise, is obesity before a woman becomes pregnant. Among other ill effects, obesity is often associated with high blood pressure and Type 2 diabetes, each increasing the risk of preeclampsia.
Women who become pregnant before they turn 20 also face a higher than average chance of developing preeclampsia. But it is primarily pregnancy among older women that is the current focus of concern.
By the end of the last century, the National Center for Health Statistics reports, birth rates among women ages 30 to 44 and the number of births to women 45 and older were at their highest levels ever.
Many of these late-in-reproductive-life pregnancies and a growing number of others among younger women with fertility problems, are aided by ovulation-stimulating drugs or in vitro fertilization, which often result in multiple fetuses.
From 1980 to 1998, for example, the rate of twin births in the United States rose by 50 percent overall, and by 1,000 percent among women 45 to 49. The rate of triplet and other higher-order multiple births increased by 400 percent overall and 1,000 percent among women in their 40's.
Regardless of a woman's age, if she is carrying two or more babies, her chances of developing preeclampsia in the second or third trimester rise significantly.
This is one reason that obstetricians often encourage women pregnant with triplets or more to undergo fetal reduction - destruction of one fetus or more very early in the pregnancy - to give those remaining a better chance of a healthy survival.
Other established risk factors for preeclampsia include chronic or poorly controlled hypertension before pregnancy, a history of having developed high blood pressure or preeclampsia in a previous pregnancy and the presence of health problems like kidney disease, rheumatoid arthritis, lupus or scleroderma.
The risk is also higher for women who conceive in the summer, according to a study in the November issue of Obstetrics & Gynecology.
If you have high blood pressure, you should do your best to get it under control before becoming pregnant.
Limit salt intake, get regular exercise and, if you are overweight, lose at least 10 percent of your weight. If these measures fail to bring down pressure to normal, about 120 over 80 or less, ask your doctor about medication.
Note, however, that experts advise against taking angiotensin converting enzyme (ACE) inhibitors and angiotensin II (AII) receptor antagonists in pregnancy. A simple diuretic may do the job with the recommended changes in daily living.
What Happens?
Rising blood pressure is just a symptom of preeclampsia. The underlying problem involves a defect in the way blood vessels respond to the presence of a fetus.
Normally, chemical signals from the fetus stimulate an expansion of maternal blood vessels, especially those supplying the placenta. By setting up a good blood supply to the placenta, the developing fetus is assured of adequate nutrition and oxygen.
But in preeclampsia, instead of expanding, the maternal vessels constrict, diminishing blood flow to the fetus and to the mother's internal organs.
An increased tendency of the mother's blood to clot adds to the problem by further impairing blood flow to the fetus. Some evidence suggests that genetic factors are to blame for improper fetal-maternal signaling.
As you may suspect, when blood flow through the placenta diminishes, the baby cannot grow normally. Also, if preeclampsia worsens, it can develop into eclampsia and cause the deaths of both mother and baby.
Although such deaths are rare in this country, eclampsia remains the second leading cause of maternal deaths after pulmonary embolism.
Every pregnant woman should know the symptoms of preeclampsia and be sure to call her doctor without delay if any develop midpregnancy.
They include severe headaches, excessive swelling of the feet and hands (some swelling in pregnancy is normal), excessive nausea or vomiting, reduced amount of urine, rapid heartbeat, dizziness, abdominal pain, ringing or buzzing in the ears, fever, drowsiness, double or blurred vision or sudden blindness, or an abrupt gain of five or more pounds.
Mild preeclampsia is diagnosed when a woman's blood pressure rises to about 140 over 90 with some protein in her urine and unusual swelling of the hands and feet.
Placing the woman on bed rest and treating her high blood pressure are the first steps a doctor is likely to take when the early stages of preeclampsia are detected. Not infrequently, the woman will be hospitalized and monitored closely to be sure that the situation does not worsen.
Some obstetricians suggest taking aspirin, to counter blood clots, and calcium supplements, to help control blood pressure, though definitive evidence for the effectiveness of these remedies is lacking.
Women are also advised to lie on their left sides when resting to prevent the weight of the abdomen from further diminishing blood flow to the fetus. Salt reduction in pregnancy, however, is not recommended because normal intakes of salt and water are needed to maintain body fluids.
If conservative measures fail to control preeclampsia, a doctor may have no choice but to deliver the baby prematurely. If possible, the delivery will be delayed until the baby's lungs have a chance to mature, a process hastened with two injections of a corticosteroid.
In many cases of preeclampsia, however, delivery by Caesarean will be necessary to protect the health of the mother and baby.
By Jane E. Brody : NY Times : November 23, 2004
Obstetric researchers have done much in recent years to increase the safety and success of pregnancies among all women of reproductive age, even those approaching the end of their ability to conceive.
But in one important area - a disorder called preeclampsia -no significant improvement has occurred, even though its incidence has risen by nearly a third in the last decade.
Preeclampsia, formerly called toxemia of pregnancy, now affects about 5 to 8 percent of pregnant women and involves a dangerous increase in blood pressure, excessive swelling and excretion of protein in the urine as a result of kidney damage.
It typically starts after the 20th week of pregnancy and, if it progresses, can cause serious damage and even threaten the lives of mother and baby. The only known way to "cure" it is to deliver the baby, however prematurely.
Monitoring for early signs of preeclampsia is one reason that it is so important for all women to obtain prenatal care and keep their scheduled appointments. At every visit, the doctor or midwife should check the blood pressure and test the urine for protein.
In one famous case, the Pulitzer Prize-winning playwright Wendy Wasserstein, who was 48 when she became pregnant with the help of a fertility doctor, was hospitalized with preeclampsia in the sixth month. Sixteen days later, doctors had to perform a Caesarean section to deliver Lucy Jane at 1 pound 12 ounces. The baby spent two months in the neonatal intensive care unit.
Who Is at Risk?
Although there are no proven ways to prevent preeclampsia, certain conditions are known to increase a woman's chances of developing it.
Pregnancies late in life and those that involve two or more fetuses are the most prominent risk factors, and they account for the increasing incidence of preeclampsia.
A third common factor, also on the rise, is obesity before a woman becomes pregnant. Among other ill effects, obesity is often associated with high blood pressure and Type 2 diabetes, each increasing the risk of preeclampsia.
Women who become pregnant before they turn 20 also face a higher than average chance of developing preeclampsia. But it is primarily pregnancy among older women that is the current focus of concern.
By the end of the last century, the National Center for Health Statistics reports, birth rates among women ages 30 to 44 and the number of births to women 45 and older were at their highest levels ever.
Many of these late-in-reproductive-life pregnancies and a growing number of others among younger women with fertility problems, are aided by ovulation-stimulating drugs or in vitro fertilization, which often result in multiple fetuses.
From 1980 to 1998, for example, the rate of twin births in the United States rose by 50 percent overall, and by 1,000 percent among women 45 to 49. The rate of triplet and other higher-order multiple births increased by 400 percent overall and 1,000 percent among women in their 40's.
Regardless of a woman's age, if she is carrying two or more babies, her chances of developing preeclampsia in the second or third trimester rise significantly.
This is one reason that obstetricians often encourage women pregnant with triplets or more to undergo fetal reduction - destruction of one fetus or more very early in the pregnancy - to give those remaining a better chance of a healthy survival.
Other established risk factors for preeclampsia include chronic or poorly controlled hypertension before pregnancy, a history of having developed high blood pressure or preeclampsia in a previous pregnancy and the presence of health problems like kidney disease, rheumatoid arthritis, lupus or scleroderma.
The risk is also higher for women who conceive in the summer, according to a study in the November issue of Obstetrics & Gynecology.
If you have high blood pressure, you should do your best to get it under control before becoming pregnant.
Limit salt intake, get regular exercise and, if you are overweight, lose at least 10 percent of your weight. If these measures fail to bring down pressure to normal, about 120 over 80 or less, ask your doctor about medication.
Note, however, that experts advise against taking angiotensin converting enzyme (ACE) inhibitors and angiotensin II (AII) receptor antagonists in pregnancy. A simple diuretic may do the job with the recommended changes in daily living.
What Happens?
Rising blood pressure is just a symptom of preeclampsia. The underlying problem involves a defect in the way blood vessels respond to the presence of a fetus.
Normally, chemical signals from the fetus stimulate an expansion of maternal blood vessels, especially those supplying the placenta. By setting up a good blood supply to the placenta, the developing fetus is assured of adequate nutrition and oxygen.
But in preeclampsia, instead of expanding, the maternal vessels constrict, diminishing blood flow to the fetus and to the mother's internal organs.
An increased tendency of the mother's blood to clot adds to the problem by further impairing blood flow to the fetus. Some evidence suggests that genetic factors are to blame for improper fetal-maternal signaling.
As you may suspect, when blood flow through the placenta diminishes, the baby cannot grow normally. Also, if preeclampsia worsens, it can develop into eclampsia and cause the deaths of both mother and baby.
Although such deaths are rare in this country, eclampsia remains the second leading cause of maternal deaths after pulmonary embolism.
Every pregnant woman should know the symptoms of preeclampsia and be sure to call her doctor without delay if any develop midpregnancy.
They include severe headaches, excessive swelling of the feet and hands (some swelling in pregnancy is normal), excessive nausea or vomiting, reduced amount of urine, rapid heartbeat, dizziness, abdominal pain, ringing or buzzing in the ears, fever, drowsiness, double or blurred vision or sudden blindness, or an abrupt gain of five or more pounds.
Mild preeclampsia is diagnosed when a woman's blood pressure rises to about 140 over 90 with some protein in her urine and unusual swelling of the hands and feet.
Placing the woman on bed rest and treating her high blood pressure are the first steps a doctor is likely to take when the early stages of preeclampsia are detected. Not infrequently, the woman will be hospitalized and monitored closely to be sure that the situation does not worsen.
Some obstetricians suggest taking aspirin, to counter blood clots, and calcium supplements, to help control blood pressure, though definitive evidence for the effectiveness of these remedies is lacking.
Women are also advised to lie on their left sides when resting to prevent the weight of the abdomen from further diminishing blood flow to the fetus. Salt reduction in pregnancy, however, is not recommended because normal intakes of salt and water are needed to maintain body fluids.
If conservative measures fail to control preeclampsia, a doctor may have no choice but to deliver the baby prematurely. If possible, the delivery will be delayed until the baby's lungs have a chance to mature, a process hastened with two injections of a corticosteroid.
In many cases of preeclampsia, however, delivery by Caesarean will be necessary to protect the health of the mother and baby.