- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Diabetes Management
Also check the American Diabetes Association website for more detailed information and advice
- a consultation with a dietician*. Remember to avoid those sugar rich "foods": cookies, cake, candy, chocolates, regular sodas. Try to follow a low carbohydrate diet. Also remember that fruit drinks are loaded with fructose "fruit sugar". Try to drink more water.
- THE FACTS [NY Times : May 6, 2013 : Anahad O'Connor]
Americans as a whole consume too much sugar, that much seems to be clear. But where is most of the sugar in our diets coming from?
Pinning the blame on liquid calories like soda and other sweetened beverages seems easy enough. Since the 1970s, the average percentage of daily calories that comes from sugary drinks has more than doubled.
But new data from the Centers for Disease Control and Prevention shows that most of the added sugar in the American diet comes not from beverages, but from food. In its latest National Health and Nutrition Examination Survey, the agency reported that although soda and sugary drinks are obvious targets for public health campaigns, they make up on average a third of the calories from added sugars that Americans consume in a typical day — a significant amount, but not the lion’s share.
Nearly 70 percent of the calories from added sugars that Americans eat on a daily basis come from processed foods like breads, jams, cakes and ice cream. Added sugars can also be found in things like tomato sauce, condiments and salad dressings, and multigrain crackers and cereals.
Ingredients on food labels are usually listed in descending order by weight. So one way to spot a food product with high quantities of sugar is to look at whether sugar, in one form or another, is listed as one of the first few ingredients.
The government data showed slight differences in consumption based on age and gender. Women get more of their daily calories from added sugar than men, but not by much: 13.2 percent compared with 12.7 percent. And as people get older, their sugar intake, at least as a percentage of daily calories, tends to fall.
THE BOTTOM LINE - Most of the added sugar the average American consumes in a typical day comes from food, not drinks.
- I use the Nutrition Counseling at Mt Auburn Hospital at 617-499-5189
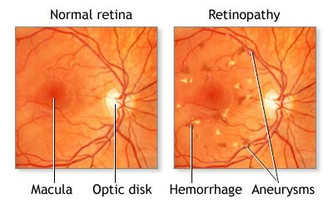
- an annual visit to an ophthalmologist. The following symptoms should be heeded and should be a reason to see your eye specialist: Blurry vision; trouble reading signs or books; seeing double; one or both eyes hurt; eyes get red and stay that way; pressure in your eye; seeing spots or floaters; straight lines no longer look straight; your side vision has changed.
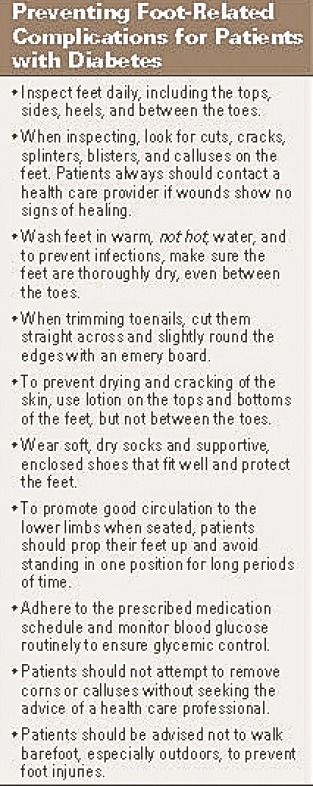
- at least two visits a year to a podiatrist
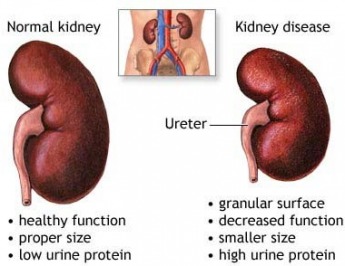
- annual checking of the urine for micro albumin (protein) to check for evidence of kidney involvement
- aggressive lowering of cholesterol in an attempt to get the LDL "bad cholesterol" <75 using one of the "statins"
- tight control of blood pressure in an attempt to get the systolic BP to <130
- the addition when ever possible of an ACE inhibitor or an angiotensin receptor blocker (ARB) to protect the kidneys from the effects of diabetes and hypertension
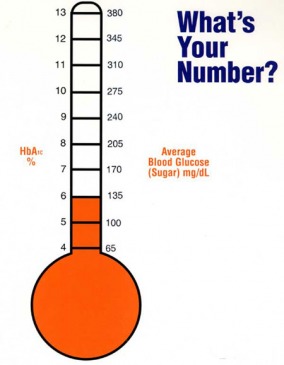
- consistently tight control of the blood glucose employing diet and medication in an attempt to get the hemoglobin A1c level down to <7%. This should be checked every 2 - 3 month
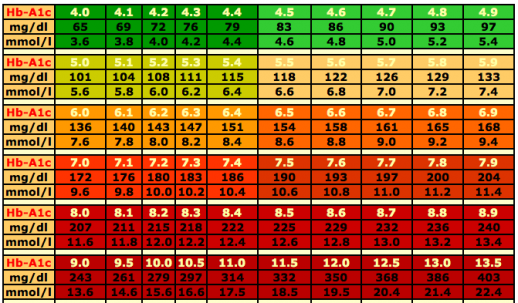
Your HbA1c value can tell you what your average blood sugar has been for approximately the previous three months. The chart above shows the approximate relationship between HbA1c and average blood sugar values.
- encouragement of the patient to monitor their own blood sugar levels on a regular basis
- strong advice and encouragement about quitting smoking
- try to keep active by walking daily
- take a multivitamin daily
- we used to tell patients to take adult low dose aspirin [81mg] if there was no medical contra-indication. No benefit for aspirin in diabetic patients without symptomatic cardiovascular disease has been demonstrated. However, diabetic patients with established cardiovascular disease should still take aspirin for secondary prevention.
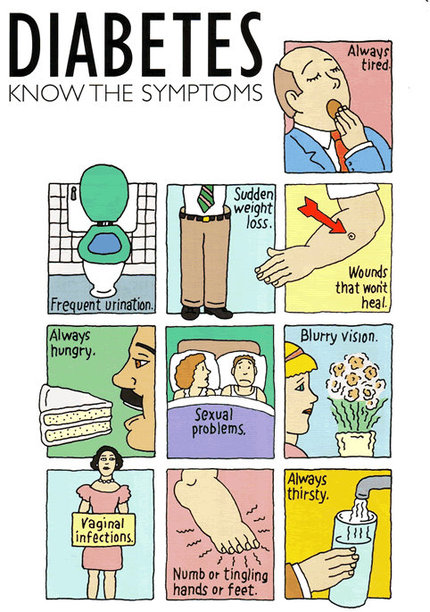
- Frequent urination
- Excessive thirst
- Extreme hunger
- Unusual weight loss
- Increased fatigue
- Irritability
- Blurry vision
Hidden Risk: Millions of People Don't Know They Are Diabetic
By Melinda Beck : WSJ Article : May 19, 2009
One of the most troubling statistics in health care is this: Twenty-three million Americans have diabetes, and one-quarter of them don't realize it.
Experts know these people exist -- even if they don't know themselves -- by extrapolating from big government health surveys that include blood tests. A surprising number of adults have elevated blood-sugar levels that meet the criteria for diabetes but have never had symptoms or ignored them. The numbers would no doubt be higher if they included children, since Type 2 diabetes is being found at ages as young as 4.
Are You Vulnerable?
The American Diabetes Association recommends:
Age 45 and older, you should be screened every 3 years and more often if you have any of the following:
- Family history of diabetes
- BMI of 25 or more
- Inactive lifestyle
- High blood pressure
- High cholesterol and/or high triglycerides
- Gestational diabetes
- African-American, Hispanic, Asian, Native American or Pacific Island heritage
- Polycystic ovary syndrome
The danger of undiagnosed diabetes is that, left untreated, it raises the risk of heart disease and stroke and can escalate into blindness, kidney failure, loss of limbs and death.
Yet fear of such complications is a key reason it often goes undiagnosed. "Many people know of elderly relatives who died or had these complications, and they don't get it checked out because they're terrified," says Robin Goland, co-director of the Naomi Berrie Diabetes Center at Columbia University Medical Center in New York. "But it doesn't have to be that way. We know how to manage it."
Some people fail to get tested because Type 2 diabetes is often associated with being overweight and sedentary. "People think it's their fault, but that's not true," Dr. Goland says. Roughly 20% of the people with Type 2 diabetes are thin, and 75% of obese people never get it.
The biggest risk factor is a family history. The more relatives you have with the disease, the higher your own risk is. Being overweight seems to activate the genetic predisposition in many cases, but not always. "People with a lot of genetic loading can get it at a younger age and a lower body weight," Dr. Goland says.
Diabetes is technically an imbalance between sugar, or glucose, and insulin. When the body ingests glucose, the pancreas secretes insulin to convert it into energy. With diabetes, the body doesn't get enough insulin, either because the pancreas can't make it (Type 1) or because the body becomes resistant to the insulin (Type 2). With Type 2, the pancreas churns out ever more insulin, but it has little effect, leaving too much glucose in the blood stream. Eventually, the insulin-making beta cells in the pancreas may give out.
The first symptoms -- including fatigue, excessive thirst and frequent urination -- often don't appear until the excess sugar has been damaging blood vessels for 10 years or more.
"I felt absolutely fine," says Charles Gallagher, an attorney in Jersey City, N.J., and his doctor agreed. But his father and 10 of his 11 aunts and uncles had "sugar," as it was often called in years past, and his daughter, an endocrinologist, persuaded him to check further. He was diagnosed with diabetes at the Naomi Berrie center in November at age 63. He has since lost 15 pounds and lowered his blood sugar considerably.
Standard physical exams often include a blood-glucose test, but experts say doctors at times don't take the results seriously enough. "They'll tell patients, 'Oh, your blood sugar is a little high. We'll check it again next year,' " says R. Paul Robertson, president for medicine and science of the American Diabetes Association. "That's the wrong thing to say. You want to make the diagnosis as soon as possible."
A fasting-glucose level below 100 milligrams per deciliter is normal. From 100 to 125 mg/dl is considered "prediabetes," and above 125 is diabetes. Some experts think "prediabetes" should be dubbed full diabetes so that patients pay attention sooner. Some also recommend that a different test, the hemoglobin A1C, be used for screening, since the results are more clear-cut.
Treating elevated blood sugar isn't as draconian as some people fear. In one study, 58% of subjects with prediabetes were able to prevent Type 2 diabetes by cutting down on carbohydrates, which reduces the glucose the body has to handle, and adding exercise, which helps insulin work more efficiently. For those who need more help, many medications are available.
"Losing just a little weight, and exercising just a little more can make a huge difference," Dr. Goland says. "People can still eat in restaurants and eat foods they love, in moderation, with diabetes. They just can't ignore it."
Diabetes - Underrated, Insidious and Deadly
By Tara Parker- Pope : NY Times Article : July 1, 2008
In a set of recent focus groups, participants were asked to rank the severity of various health problems, including cancer, heart disease and diabetes.
On a scale of 1 to 10, cancer and heart disease consistently ranked as 9s and 10s. But diabetes scored only 4s and 5s.
“The general consensus seems to be, ‘There’s medication,’ ‘Look how good people look with diabetes’ or ‘I’ve never heard of anybody dying of diabetes,’ ” said Larry Hausner, chief executive of the American Diabetes Association, which held the focus groups. “There was so little understanding about everything that dealt with diabetes.”
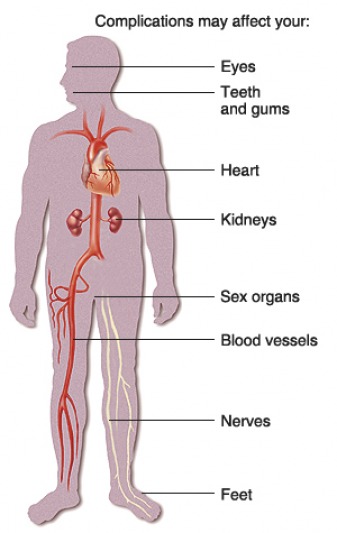
But diabetes is anything but minor. It wreaks havoc on the entire body, affecting everything from hearing and vision to sexual function, mental health and sleep. It is the leading cause of blindness, amputations and kidney failure, and it can triple the risk for heart attack and stroke.
“It is a disease that does have the ability to eat you alive,” said Dr. John B. Buse, a professor at the University of North Carolina School of Medicine who is the diabetes association’s president for medicine and science. “It can be just awful — it’s almost unimaginable how bad it can be.”
Diabetes results when the body cannot use blood sugar as energy, either because it has too little insulin or because it cannot use insulin. Type 2 diabetes, which accounts for 90 to 95 percent of cases, typically develops later in life and is associated with obesity and lack of exercise. Type 1 diabetes, which is often diagnosed in children, occurs when the immune system mistakenly destroys cells that make the insulin.
The disconnect between perception and reality is particularly worrisome at a time when national diabetes rates are surging. Just last week, the Centers for Disease Control and Prevention announced that the number of Americans with diabetes had grown to about 24 million, or 8 percent of the population. Almost 25 percent of those aged 60 and older had diabetes in 2007. And the C.D.C. estimates that 57 million people have abnormal blood sugar levels that qualify as pre-diabetes.
To be sure, diabetes is treatable, and an array of new medications and monitoring tools have dramatically improved the quality of care. But keeping the illness in check requires constant vigilance and expensive care, along with lifestyle changes like losing weight, exercising regularly and watching your carbohydrates.
Dr. Buse says patients who are focused on their disease and who have access to regular medical care have a good chance of living out a normal life span without developing a diabetes-related disability.
But some patients say they are too busy to take better care of themselves, and many low-income patients can’t afford regular care. Even people with health insurance struggle to keep up with the co-payments for frequent doctor visits and multiple medications.
And to make matters worse, diabetes is associated with numerous other health problems. Last week, for example, The Journal of the American Medical Association reported that people with depression were at higher risk for Type 2 diabetes, and vice versa.
That is not surprising: according to data published last year in the journal Diabetes Care, depression tends to interfere with a patient’s self-care, which requires glucose monitoring, medications, dietary changes and exercise.
Ultimately, diabetes can take a toll from head to toe. In the brain, it raises the risk not only for depression but also for sleep problems and stroke. It endangers vision and dental health. This month, The Annals of Internal Medicine is reporting that the disease more than doubles the risk of hearing loss.
Moving down the body, diabetes can lead to liver and kidney disease, along with serious gastrointestinal complications like paralysis of the stomach and loss of bowel control. Last year the journal Diabetes Care reported that in a sample of nearly 3,000 patients with diabetes, 70 percent had nonalcohol fatty liver disease.
Poor circulation and a loss of feeling in the extremities, called neuropathy, can lead to severe ulcers and infections; each year in the United States, there are about 86,000 diabetes-related amputations.
Diabetes can also take a toll on relationships. By some estimates, 50 percent to 80 percent of men with diabetes suffer from erectile dysfunction. Experts say women with diabetes often lose their libidos or suffer from vaginal dryness.
The challenge for doctors is to convince patients that diabetes is a major health threat. For years, the message from the American Diabetes Association has been one of reassurance that the disease is treatable. Now, beginning in 2009, the association plans to reframe its message to better communicate the seriousness of the disease.
“Our communication strategy is going to be that diabetes has deadly consequences, and that the A.D.A. is here to change the future of diabetes,” said Mr. Hausner, a former executive with the Leukemia and Lymphoma Society who came to the association 10 months ago. “It’s the word ‘deadly’ that was the potentially controversial word for the organization. In the past, people said, ‘We don’t want to get anybody scared.’ ”
The new strategy is not a scare tactic, he added. Prevention and hope will still be part of the message.
“It’s not that we don’t want people to have hope,” he said. “We want people to understand this is serious.”
Finding Whether Diabetes Lurks
Denise Grady : NY Times article : May 1, 2007
More than six million Americans are walking around with no idea that they have an insidious disease with the potential to wreak havoc throughout the body.
The disease is diabetes, and it causes high blood sugar levels that can damage arteries and lead to heart disease, strokes, kidney failure, amputations and blindness. It is the sixth-leading cause of death in the United States.
The idea of so many people — roughly 30 percent of the 21 million Americans who have the disease — going without treatment is disturbing because diabetes can do so much damage. But in its early stages, people often do not realize they are ill, because the symptoms — if there are any — may creep up gradually or be attributed to overwork or aging.
“Certain signs are important,” said Dr. F. Xavier Pi-Sunyer, chief of endocrinology, diabetes and nutrition at St. Luke’s-Roosevelt Hospital in Manhattan. “If you have to get up a couple of times to urinate at night, and you didn’t before, that’s a suggestive sign. Also, vision blurring of any kind, suddenly beginning to lose a significant amount of weight without trying, frequent skin infections or vaginal infections. And this is nonspecific, but if you’re getting headaches and feeling kind of fatigued.”
Any of those symptoms should prompt testing for diabetes, Dr. Pi-Sunyer said. So should certain risk factors, especially if there are more than one. Aging and obesity increase the odds that a person will develop Type 2, or adult-onset diabetes, the most common form. Weight is a particular risk factor, especially if it is mostly in the belly — a waist over 40 inches in men or 35 inches in women. Blacks, Native Americans and Hispanics have a higher-than-average risk, as do people with a family history of the disease. Being sedentary may also increase the risk, though not all researchers agree about that.
People who appear healthy but have risk factors should be tested for diabetes every three years, Dr. Pi-Sunyer said.
The simplest means for earlier detection is a blood sugar test, measured after a person has fasted for at least eight hours. Readings above 126 milligrams of glucose per tenth of a liter of blood indicate diabetes; anything below 100 is considered normal. Intermediate levels reflect impaired glucose metabolism or “pre-diabetes.” People in this category need yearly testing, because up to 8 percent of them will become diabetic each year. About 54 million Americans are pre-diabetic.
Though many doctors in the United States like the fasting blood sugar test because it is quick and easy, some use another test, one that may pick up diabetes at an even earlier stage. This is a glucose tolerance test, in which the patient is given a fasting blood sugar test, drinks a glucose solution and then has another blood sugar test two hours later. People who test positive for Type 2 diabetes are generally advised to lose weight and exercise more, and some may also need drugs to help lower blood sugar. They will also usually be tested for conditions that often go along with Type 2 diabetes, like high blood pressure and high cholesterol and triglyceride levels.
A major study of people with impaired glucose metabolism found that among those who did moderate exercise, like walking for just 30 minutes a day, and who lost 5 to 10 percent of their body weight, there were 58 percent fewer new cases of diabetes than in a similar group of people who did not exercise or lose weight.
The study also found that a commonly used diabetes drug, metformin, could help lower the risk of the disease in pre-diabetics. But the drug did not work as well as weight loss and exercise, and it is approved only for diabetes, not for pre-diabetes.
In April a genetic test was introduced that can also identify people with an increased risk of developing Type 2 diabetes. The $500 test by DeCode Genetics cannot predict diabetes definitively, but it might motivate people with a high risk to exercise and lose weight. It can be ordered by doctors or from a company called DNA Direct.
Diabetes : Looking past blood sugar
By Gina Kolata : NY Times Article : August 20, 2007
Dave Smith found out he had Type 2 diabetes by accident, after a urine test.
“Whoa, look at the sugar in here,” his doctor told him. Mr. Smith’s blood sugar level was sky high and glucose was spilling into his urine.
That was about nine years ago, and from then on Mr. Smith, like so many with diabetes, became fixated on his blood sugar. His doctor warned him to control it or the consequences could be dire — he could end up blind or lose a leg. His kidneys could fail.
Mr. Smith, a 43-year-old pastor in Fairmont, Minn., tried hard. When dieting did not work, he began counting carbohydrates, taking pills to lower his blood sugar and pricking his finger several times a day to measure his sugar levels. They remained high, so he agreed to add insulin to his already complicated regimen. Blood sugar was always on his mind.
But in focusing entirely on blood sugar, Mr. Smith ended up neglecting the most important treatment for saving lives — lowering the cholesterol level. That protects against heart disease, which eventually kills nearly everyone with diabetes.
He also was missing a second treatment that protects diabetes patients from heart attacks — controlling blood pressure. Mr. Smith assumed everything would be taken care of if he could just lower his blood sugar level.
Blood sugar control is important in diabetes, specialists say. It can help prevent dreaded complications like blindness, amputations and kidney failure. But controlling blood sugar is not enough.
Nearly 73,000 Americans die from diabetes annually, more than from any disease except heart disease, cancer, stroke and pulmonary disease.
Yet, largely because of a misunderstanding of the proper treatment, most patients are not doing even close to what they should to protect themselves. In fact, according to the federal Centers for Disease Control and Prevention, just 7 percent are getting all the treatments they need.
“That, to me, is mind-boggling,” said Dr. Michael Brownlee, director of the JDRF International Center for Diabetic Complications Research at the Albert Einstein College of Medicine in New York. “It makes me ask, What is going on? I can only conclude that people are not aware of their risks and what could be done about them.”
In part, the fault for the missed opportunities to prevent complications and deaths lies with the medical system. Most people who have diabetes are treated by primary care doctors who had just a few hours of instruction on diabetes, while they were in medical school. Then the doctors typically spend just 10 minutes with diabetes patients, far too little for such a complex disease, specialists say.
In part it is the fault of proliferating advertisements for diabetes drugs that emphasize blood sugar control, which is difficult and expensive and has not been proven to save lives.
And in part it is the fault of public health campaigns that give the impression that diabetes is a matter of an out-of-control diet and sedentary lifestyle and the most important way to deal with it is to lose weight.
Most diabetes patients try hard but are unable to control their disease in this way, and most of the time it progresses as years go by, no matter what patients do.
Mr. Smith, like 90 percent of diabetes patients, has Type 2 diabetes, the form that usually arises in adulthood when the insulin-secreting cells of the pancreas cannot keep up with the body’s demand for the hormone. The other form of diabetes, Type 1, is far less common and usually arises in childhood or adolescence when insulin-secreting pancreas cells die.
And, like many diabetes patients, Mr. Smith ended up paying the price for his misconceptions about diabetes. Last year, he had a life-threatening heart attack.
The Heart Disease
Just after returning from church last October, Mr. Smith had a discomforting sensation. Deciding to focus on something else, he went to a local newspaper office where he was weekend editor. But the strange feeling persisted and intensified.
“I felt a pain in my chest,” Mr. Smith recalled. “It wasn’t sharp — it was more of a kind of pressure, a feeling like something is contracting.”
The pain spread, to his neck, along his shoulder, down to his biceps. Mr. Smith, alone and frightened, looked up heart attack symptoms on the American Heart Association’s Web site. They were exactly what he was experiencing.
An hour later, Mr. Smith was at the Mayo Clinic in Rochester, Minn., in the throes of a major heart attack, transported by helicopter while his wife and two young sons frantically drove two and a half hours to be with him. A main artery to his heart was 90 percent blocked. If he had waited to seek help or if his local hospital and doctor had not acted quickly and sent him to the Mayo Clinic, he probably would have died.
Mr. Smith thought his biggest risk from diabetes was blindness or amputations. He never thought about heart disease and had no idea how important it was to control cholesterol levels and blood pressure. He said his doctor had not advised him to take a cholesterol-lowering or blood pressure drug and he did not think he needed them.
Most people with diabetes are equally unaware of the danger that heart disease poses for them.
A recent survey by the American Diabetes Association conducted by RoperASW found that only 18 percent of people with diabetes believed that they were at increased risk for cardiovascular disease.
Yet, said Dr. David Nathan, director of the Diabetes Center at Massachusetts General Hospital, “when you think about it, it’s not the diabetes that kills you, it’s the diabetes causing cardiovascular disease that kills you.”
Dr. Brownlee said he was stunned by the results of the diabetes association poll. “If you are one of those 82 percent who don’t think you are at increased risk,” he said, “finding out that you are and that you can decrease that risk substantially could literally change your life.”
The science is clear on the huge benefits for people with diabetes of lowering cholesterol and controlling blood pressure. After multiple studies, costing hundreds of millions of dollars and involving tens of thousands of subjects, national guidelines were rewritten to reflect the new data, and professional organizations issued recommendations for diabetes care.
With cholesterol, the guidelines say that levels of LDL cholesterol, the form that increases heart disease risk, should be below 100 milligrams per deciliter and, if possible, 70 to 80. Yet, Dr. Brownlee said, diabetes patients with LDL cholesterol levels of 100 to 139 often are told that their levels — ideal for a healthy person without diabetes — are terrific.
“Many practicing doctors just don’t know that an LDL cholesterol number that is normal for someone without diabetes is not normal for someone with diabetes,” he said.
Mr. Smith found all that out too late. The heart attack, he said, “really blindsided me.”
He also did not know the other measures proven to prevent complications in diabetes. He was correct that high blood sugar is dangerous. It can damage the small blood vessels in the eyes, leading to blindness; the nerves in the feet, leading to amputations; and the kidneys, leading to kidney failure.
But no matter how carefully patients try to control their blood sugar, they can never get it perfect — no drugs can substitute for the body’s normal sugar regulation. So while controlling blood sugar can be important, other measures also are needed to prevent blindness, amputations, kidney failure and stroke. Mr. Smith was doing none of them.
He also made the common assumption that Type 2 diabetes is simply a consequence of being fat. And that losing weight will help cure it.
Obesity does increase the risk of developing diabetes, but the disease involves more than being obese. Only 5 percent to 10 percent of obese people have diabetes, and many with diabetes are not obese. To a large extent, Type 2 diabetes is genetically determined — if one identical twin has it, the other has an 80 percent chance of having it too. In many cases, weight loss can help, but, as Mr. Smith has learned, most who lose weight are not cured of the disease. He lost 40 pounds but still has diabetes.
“Everybody in the act of losing weight will have a pretty dramatic improvement pretty quickly,” said Dr. C. Ronald Kahn, a diabetes researcher and professor of medicine at Harvard Medical School. Blood sugar levels drop precipitously and the disease seems to be under control. But that is because the metabolic process of weight loss lessens diabetes. Once weight is lost, he added, and people stabilize at a lower weight, their diabetes may remain.
When it comes to weight loss, Dr. Kahn said, “there is a range of susceptibilities in how people react.”
Complex Regimens
Before he left the hospital, Mr. Smith’s doctors told him about his new diabetes regimen: a statin to drive his cholesterol level very low, two drugs to lower his blood pressure, an aspirin, insulin and two drugs to reduce his blood sugar levels. That new list of drugs was what he should have been taking all along.
Mr. Smith is taking them now, terrified that his heart disease will progress.
“I’ll never be out of the woods,” he said. “I’ve got to face that.”
Diabetes researchers say stories like Mr. Smith’s are all too familiar.
The statistics are grim: A quarter to a third of all heart attack patients have diabetes, even though diabetes patients constitute just 9.3 percent of the population. Another 25 percent of heart attack patients are verging on diabetes with abnormally high blood sugar levels.
Most worrisome are diabetes patients who already have symptoms of heart disease, like chest pains or a previous heart attack. “That is a terrible situation,” said Dr. James Cleeman, coordinator of the National Cholesterol Education Program at the National Institutes of Health. Those patients, Dr. Cleeman said, are set up for a fatal heart attack and should be stringently controlling their cholesterol and blood pressure.
And it is not just that many diabetes patients are overweight, as people with Type 1 diabetes, who often are thin, also have a high risk of heart disease. There is something about diabetes itself, researchers say, that leads to high levels of LDL cholesterol and a form of LDL cholesterol particles that is particularly dangerous. Diabetes also leads to increased levels of triglycerides, which are fats in the blood that increase heart disease risk, and in diabetes is linked to high blood pressure.
Being obese or overweight, in contrast, are “weak contributors to heart attack risk,” Dr. Nathan said.
Type 2 diabetes “does not exist in isolation,” Dr. Nathan said. “Underlying diabetes are all these cardiovascular risk factors.”
Somehow, though, it has taken quite a while for the alarm bells to go off.
One reason might be that it was heart disease researchers, not diabetes researchers, who conducted the seminal studies.
The key to saving lives is to reduce levels of LDL cholesterol to below 100 and also control other risk factors like blood pressure and smoking. The cholesterol reduction alone can reduce the very high risk of heart attacks and death from cardiovascular disease in people with diabetes by 30 percent to 40 percent, Dr. Cleeman said. And clinical trials have found that LDL levels of 70 to 80 are even better for people with diabetes who already have overt heart disease.
Studies of blood sugar control have been more problematic than those of cholesterol lowering.
In Type 2 diabetes, the most ambitious effort was a huge study in Britain. It found that rigorous blood sugar control could lower the risk of complications that involved damage to small blood vessels, a list that includes blindness, nerve damage and kidney damage. But there was no effect on the overall death rate. There was a small decrease in the number of heart attacks but it was not statistically significant, meaning it could have occurred by chance.
The National Institutes of Health is trying again, with a larger study of blood sugar control that includes enough patients to detect more subtle effects on the heart attack rate if they exist. For now, though, the answer simply is not known.
In Type 1 diabetes, a large federal study did find evidence that rigorous blood sugar control could reduce heart disease risk. But the effect emerged 12 years after the study ended and most of the patients, in those years, had not been able to sustain the blood sugar control that they had had during the study. Did the short period of rigorous control exert a delayed effect on heart disease or was the effect caused by some other factor during the study or afterward, some asked? While most think it was caused by blood sugar control, it is impossible to know for sure.
The result, notes Dr. John Buse, president-elect for science and medicine at the American Diabetes Association, is that for people with Type 1 and, especially, for those with Type 2 diabetes, there are still questions about whether and to what extent blood sugar control protects against heart disease and saves lives.
That leaves cholesterol lowering, for patients with Type 1 and Type 2 diabetes, as the most effective and easiest way by far to reduce the risk of heart disease and the only treatment proven to save lives. But doctors say achieving the recommended cholesterol levels usually means taking a statin. Some patients resist, wary of intense drug company marketing to patients and afraid of side effects like muscle or liver damage which, although extremely rare, have frightened many away from the drugs, Dr. Brownlee and other diabetes specialists said. (Dr. Brownlee said he had no financial ties to statin makers.)
Others point to drug company advertising itself.
Statin advertising, said Dr. Irl B. Hirsch, a professor of medicine and director of the diabetes clinic at the University of Washington, is all about heart disease, and the advertisements do not mention diabetes. The diabetes advertisements are all about blood sugar. Dr. Hirsch has seen few that put the two together.
Yet lowering cholesterol with statins, Dr. Hirsch and others said, is much simpler than anything else diabetes patients are asked to do. And, he added, the drugs are among the best studied and the safest on the market. (Dr. Hirsch said he had no financial ties to statin makers.)
Dr. Hirsch has a message for diabetes patients: If he had to rate the different regimens for a typical middle-age person with Type 2 diabetes, the first priority would be to take a statin and lower the LDL cholesterol level.
Dr. Brownlee agreed, but added that the two other measures to protect against heart disease, blood pressure control and taking an aspirin to prevent blood clots, should not be neglected.
“Right now, without waiting for lots of exciting things that are almost in the pipeline or in the pipeline, starting tomorrow, if everyone did these things — taking a statin, taking a blood pressure medication, and maybe taking an aspirin — you would reduce the heart attack rate by half.”
The Burnout
Even when patients do take the right steps to control diabetes, the grueling process can simply wear them down.
Virgil Umbarger learned that he had Type 2 diabetes when he was 39 and had a medical exam for a life insurance policy.
That was 25 years ago, and the start of a journey that diabetes specialists say ends up fundamentally changing a person’s world. Unlike Mr. Smith, who has just awakened to the danger he is in, Mr. Umbarger, a funeral director in Yakima, Wash., has lived with diabetes and its increasingly complex regimen for decades. And, as happens with most diabetes patients eventually, he feels he is reaching a point where he just cannot continue to do all that he should to protect his health.
In a sense, Mr. Umbarger said, he was not completely surprised when he learned he had diabetes, because it runs in his family. But he never thought it would happen to him. At 6 feet tall and 195 pounds, he was not heavy.
Still, Mr. Umbarger’s first thought was to lose weight. “I starved myself,” he said, and lost 15 pounds. But he still had diabetes and the pounds crept back on.
Dr. Buse said his patients knew how important it was to diet and exercise, but most could not do it enough to make a difference, and some were also thwarted by medications to control blood sugar that make patients gain weight.
In the end, Mr. Umbarger decided to seek care from a diabetes specialist. He chose Dr. Hirsch, even though it meant driving nearly three hours each way for an office visit. There was no one nearby with that kind of expertise, Mr. Umbarger said.
On his first visit, Dr. Hirsch gave him a fistful of prescriptions, including a statin, blood pressure medications and one for the drug Mr. Umbarger dreaded — insulin. He also told Mr. Umbarger to have regular checks for eye, nerve and kidney damage. And he has to watch what he eats and count carbohydrates.
Dr. Hirsch and other diabetes specialists say they are well aware of how daunting the program can be.
“Many come here once or twice and walk away saying, ‘I don’t want to do this,’ ” Dr. Hirsch said.
Not Mr. Umbarger. For years, he tried to do all that was required. He can cope with the medications and the long drives to see Dr. Hirsch. The problem for him, as for most diabetes patients eventually, is the blood sugar monitoring. He is supposed to prick his finger six or more times a day to measure his glucose levels and adjust his insulin dose accordingly.
Every time he checks his blood sugar is like getting a report card — was he eating too many carbohydrates? Did he get the insulin dose right?
“I don’t want to look,” he said.
“Pricking your finger, seeing that number day after day, it wears on you,” Mr. Umbarger said. “It’s like a ball and chain.” He confesses that he has only been checking his blood sugar once or twice a day, guessing at many of his insulin doses. His blood sugar levels have been rising and guilt hangs over him.
Meanwhile, no matter what they do, most people with Type 2 diabetes get worse as the years go by. Patients make less and less insulin and their cells become less and less able to use the insulin they do produce.
“That is why it is not uncommon to start initially with diet therapy, then after a few years we need to add a drug that improves insulin sensitivity,” Dr. Kahn said. “Then when that drug isn’t enough, we add a second drug that improves insulin sensitivity by a different mechanism. Then we add a drug that stimulates that pancreas to make more insulin.”
Then, he added, patients with Type 2 diabetes may need insulin itself, but when that happens they have to take even more than a person with Type 1 diabetes — two or even three times as much — because their cells no longer respond adequately to the hormone.
While it is not easy to re-energize burned-out patients, Dr. Hirsch said, at the very least, doctors and patients should know what is important.
“We already have the miracle pills” — statins and blood pressure medications, he said. And they are available for pennies a day, as generics.
“We need patient education and physician training that this stuff is out there and this is what we should be focusing on to make a difference in lives.”
Things to Know : Tips to Help Patients Manage Their Care
From NY Times : August 20, 2007
Dr. John Buse, director of the Diabetes Care Center at the University of North Carolina, Chapel Hill, is president-elect for science and medicine at the American Diabetes Association and a principal investigator in a federal study asking whether blood sugar control can protect against heart disease in people with Type 2 diabetes.
“Diabetes is underdiagnosed, undertreated and underappreciated as a cause of death and disability,” Dr. Buse said. “Despite the fact that almost 20 percent of all health care dollars are spent on the management of people with diabetes, the diabetes epidemic and its associated pain and suffering grow and grow.” Here, he says, are
Five things that everyone with diabetes should know:
- 1. If you are overweight, get screened for diabetes with a fasting glucose test, starting at puberty, at least every three years. If you are not, start at age 45. A normal result is less than 100 mg/dl.
- 2. If you have diabetes or prediabetes, engage in moderate-intensity exercise like brisk walking for at least 30 minutes at least five days a week. If you are overweight, reduce calories with a goal of losing at least 5 percent of body weight (10 pounds if you weigh 200 pounds). Working with a dietitian can be extremely helpful.
- 3. If you have diabetes, make sure to have an A1C test, which measures glucose levels, at least twice a year, regular blood pressure checks and annual cholesterol checks. The A1C should be less than 7 percent, blood pressure less than 130 over 80 and LDL cholesterol under 100 mg/dl. If you are not reaching all three goals, ask for a referral to a diabetes education program, start a new drug, see a specialist and keep working toward getting what is known as your ABC’s (for A1C, blood pressure and cholesterol) under control. If you are over 21, discuss taking low-dose aspirin with your doctor. Do not smoke.
- 4. If you have diabetes, have annual checkups for complications including a dilated eye exam by an eye-care professional, a urine microalbumin-to-creatinine ratio and a comprehensive foot exam including testing with a 10-gram filament. If the results are not normal, you will need additional treatment to avoid disability. Make sure you get it.
- 5. People with diabetes who work with their health care team to do the best they can to control diabetes, its related disorders and its complications should expect to live a long and healthy life.
Statins for all diabetics urged
People with diabetes should receive cholesterol-busting drugs regardless of whether they have signs of heart disease, UK researchers say.
Statins cut the risk of heart attack, stroke and death in diabetic people even in those with low cholesterol levels, analysis of 14 trials shows.
It means hundreds of thousands more people could benefit from treatment, the Lancet report said.
There are 2.5 million people diagnosed with diabetes in the UK.
Many more do not realise they have the condition and statins are "underused" in people with diabetes the researchers said.
Guidance from the National Institute of Clinical and Health Excellence (NICE) in England and Wales issued in 2006 estimated around 3.3 million people are eligible for treatment with statins.
This includes people with diabetes who have a 20% risk of developing cardiovascular disease in the next 10 years.
Benefits
A team of researchers at Oxford University reviewed studies of more than 90,000 people - 19,000 with diabetes - and found that many more would benefit from statins than previously realised.
They found that standard daily treatment with statins would prevent about one third of heart attacks and strokes in people with diabetes.
The benefits were seen regardless of age, sex and whether patients were already showing signs of cardiovascular disease.
After five years, 42 fewer people with diabetes had major problems, such as heart attacks or stroke, for every 1,000 treated with statins.
The only exceptions for treatment should be those with exceptionally low risk, such as children or those who cannot take the drugs for other reasons, such as pregnant women.
Study leader Professor Colin Baigent said there had been some debate about whether statins would have the same benefits in people with diabetes as those with heart disease in general.
"People with diabetes are a clearly defined group of people at an increased risk of cardiovascular disease.
"What we're saying is statins are clearly effective in every type of person with diabetes."
Diabetes UK estimates 60% of all diabetics currently receive statins. That would mean the vast majority of the remaining 40% could also benefit from these drugs, according to the researchers.
However, Douglas Smallwood, chief executive of Diabetes UK, recommended statins for people with diabetes over the age of 40 or diabetics younger than 40 with another risk factor.
"Diabetes UK also strongly recommends that good diabetes management should rely not only on medication, but also on a healthy lifestyle and diet," he added.
Eating to Keep Diabetes in Check
By Peter Jaret : NY Times Article : May 24, 2008
In Brief:
One in four people born today are expected to develop Type 2 diabetes during their lifetimes.
Shedding excess weight and exercising more can cut Type 2 diabetes risk by 58 percent.
Favoring foods in their unrefined state -- brown rice and whole grains, for instance -- can help keep blood sugar levels from spiking.
Exercise improves blood sugar control by increasing insulin sensitivity.
As rates of Type 2 diabetes continue to rise around the world, experts say we mostly have ourselves to blame. Genes certainly play a role in determining risk. But the surge of new cases of this debilitating disease is caused mostly by poor diets and lack of physical activity.
By all rights, the prescription should be simple: lose weight if you are overweight, and get more exercise.
Easy? Of course not. Experts have yet to come up with anything close to a surefire approach to help people shed pounds. And dietary recommendations to prevent or slow diabetes have often been contradictory and confusing. Nearly 30 years after the American Diabetes Association recommended a low-fat, high-carbohydrate diet to control diabetes, overturning the high-fat, low-carbohydrate approach of earlier decades, controversy still swirls around the amount and types of carbohydrates to eat.
Much of the debate focuses on the glycemic index, a measure of how carbohydrate-rich foods affect blood sugar, and whether these effects play a significant role in the progression of Type 2 diabetes. Foods high on the glycemic index, like sugared beverages, cake and white rice, are known to send blood sugar levels up sharply after a meal. Foods low on the index, like broccoli, lettuce, brown rice and whole grains, on the other hand, take longer to digest and hence keep blood sugar levels on a more even keel.
The American Diabetes Association has decided that patients should not be counseled to take the glycemic index into account when choosing foods. “Although it is clear that carbohydrates do have differing glycemic responses,” its policy statement declares, “the data reveal no clear trend in outcome benefits.”
That’s a mistake, says Dr. David Ludwig, an endocrinologist at Children’s Hospital in Boston and an associate professor at Harvard Medical School. “High-glycemic foods like refined grains raise blood sugar levels two to three times higher than unprocessed foods with a low glycemic index,” he said. When blood sugar levels spike, the body must churn out insulin to move glucose out of the bloodstream and into cells, where it is used for energy.
“If you’re eating high-glycemic foods meal after meal, snack after snack, day after day, that’s going to put a lot of stress on the system that produces insulin,” Dr. Ludwig said. “If the system is already compromised due to a family history of diabetes, those rapid swings of blood sugar could make a difference between remaining healthy or decompensating into Type 2 diabetes.”
Dr. Ludwig cites a study he conducted in which rats fed foods high on the glycemic index lost lean muscle mass, gained body fat and began to lose their ability to control blood sugar.
“A high percentage of insulin-producing cells in the high-glycemic rats were undergoing a process of destruction, disruptions in their architecture and scarring,” Dr. Ludwig said. The same thing, he suspects, happens in people.
But so far, evidence from human studies has been sketchy. In one recent Canadian study, there were no differences in blood sugar control among 162 volunteers assigned to one of three very different diets for a year: a low-carbohydrate regimen; a high-carbohydrate, low-glycemic-index diet; or foods high on the glycemic scale. Fasting glucose, a test widely used to monitor diabetes risk, actually rose in the group eating the low-glycemic foods.
A second study of 1,898 people found that risk of Type 2 diabetes was the same whether people reported eating foods high or low on the glycemic index.
“The notion that glycemic index matters makes intuitive sense,” said Dr. John M. Miles, a diabetes expert at the Mayo Clinic. “A lot of people have strong feelings on the subject. But the evidence just isn’t there.”
Dr. Xavier Pi-Sunyer, an endocrinologist and diabetes expert at St Luke’s-Roosevelt Hospital in New York, agreed. Given the new findings, “It seems unwise at this point to burden Type 2 diabetes patients with trying to pick and choose among different high- and low-glycemic-index foods,” he wrote in a recent review of the evidence.
But Dr. Thomas Wolever, a University of Toronto researcher who led the Canadian trial, noted that those who ate low-glycemic-index foods showed improvements in blood sugar control after meals, which may be a more important measure of glucose control than the fasting glucose test. They also had reductions in levels of C-reactive protein, a marker for inflammation that also appears to be linked to diabetes risk.
Low-glycemic diets may have another crucial advantage, Dr. Wolever suggested: they help some people shed pounds. “I’ve had people tell me it’s the only way they’ve been able to lose weight,” he said.
While no single diet works for everyone, losing weight may be the single most effective way to lower Type 2 diabetes risk. Evidence for that comes from a major trial sponsored by the National Institutes of Health, in which a randomly assigned group of overweight volunteers with early signs of diabetes were encouraged to lose about 7 percent of their body weight and engage in 150 minutes of moderate exercise weekly.
Over the next three years, only 5 percent of the lifestyle intervention group went on to develop diabetes each year, compared with 11 percent of volunteers in a control group. Weight loss and exercise proved more effective than a leading diabetes medication in preventing Type 2 diabetes.
“There’s no question that if we can get people to lose 5 or 10 pounds, we’ll be doing them a world of good,” Dr. Wolever said. The confounding question remains how.
High Carbohydrate Food with Resistant Starches are Back
Resistant starches, found naturally in foods such as navy beans, green bananas and whole-grain breads, can contribute to colon health. They may also aid in lowering cholesterol and weight.
By Susan Bowerman : Special to The Times : June 23, 2008
The Atkins craze is pretty much behind us -- my neighborhood low-carb food store recently shuttered its doors -- so now it's time to circle back with some good news about carbohydrates.
High-carb foods such as beans, bananas and whole-grain breads might have gotten the cold shoulder in recent years. But of late, some in the food industry have begun touting the health benefits of "resistant starch" -- a form of fiber that delivers some of the health benefits of soluble and insoluble fibers.
Starches are simply long chains of sugar molecules that must be broken apart by amylase, an enzyme in the saliva and small intestine, releasing the individual sugars so that they can be absorbed.
But resistant starches defy digestion: They contain more of a tight-packing form of starch that amylase doesn't easily attack. They continue unscathed through the digestive tract to the large intestine, where bacteria feed on them, fermenting them and producing fatty acids.
These fatty acids (acetate, propionate and butyrate) contribute to colon health. They make the environment more acidic and less hospitable to bacteria that can cause illness. Absorption of potentially toxic or carcinogenic compounds is lowered too.
Like insoluble fibers such as cellulose, resistant starch traps water and adds bulk to the stool, which helps with regularity. And it appears to share properties with soluble fibers that help to control blood sugar and cholesterol.
In a Korean study published in 2004 in the Journal of Nutritional Science and Vitaminology, overweight subjects who ate resistant starch every day for three weeks had significant drops (about 50 points, on average) in their cholesterol levels. The placebo group, who ate regular starch, showed no such change. But the subjects in this study ate a lot of resistant starch -- nearly five times the estimated 5 grams Americans eat daily via whole foods.
More modest intakes of resistant starch have been shown in a few studies to help blunt rapid rises in blood sugar after a carbohydrate-rich meal. In a Japanese report, for example, blood sugar levels in subjects with borderline diabetes rose 20% less after they ate bread laced with 6 grams of resistant starch than after a meal of bread without resistant starch.
Foods high in resistant starch may help with weight loss too. In a 2006 study from Louisiana State University published in the journal Obesity, rats fed chow supplemented with resistant starch lost body fat -- but not because the fiber filled them up. Instead, resistant starch stimulated genes that contain the blueprint for two hormones, PYY and GLP-1, that make us feel full and send signals to stop eating.
A small study at the University of Colorado, published in 2004 in Nutrition & Metabolism, looked at the effects of resistant starch on fat metabolism in people after eating a single meal. The fat in the meal was chemically labeled so that the end product of its metabolism -- carbon dioxide released in the breath -- could be traced over a six-hour period.
Fat burning was 23% higher in those who ate 5 grams of resistant starch in the meal than in those who didn't: More fat was burned for fuel and less was available to store away. The subjects in this study were of normal weight and they ate the starch once. Longer studies of intake in overweight people would be needed to see if weight loss would occur.
Resistant starches exist naturally in underripe bananas, navy beans, lentils, barley and whole-grain breads -- but in relatively small amounts. One review of the literature estimated that 6 to 12 grams of resistant starch at a meal can exert beneficial effects on blood sugar, but that daily intakes in the range of 20 grams might be needed to provide the bulk to promote digestive health. Even if you like your bananas green, a single fruit -- one of the richest natural sources -- will provide just less than 5 grams.
Food manufacturers are on top of this story, though. Forget low-carb breads and candy bars, so popular a few years ago. Corn-derived resistant starch is making its way into breads, cereals and pastas -- coming to a store near you.