- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Dizziness, Vertigo and Tinnitus
Getting Specific About Dizziness
By Jane E. Brody : NY Times : Feb. 6, 2017
Dizziness is not a disease but rather a symptom that can result from a huge variety of underlying disorders or, in some cases, no disorder at all. Readily determining its cause and how best to treat it — or whether to let it resolve on its own — can depend on how well patients are able to describe exactly how they feel during a dizziness episode and the circumstances under which it usually occurs.
For example, I recently experienced a rather frightening attack of dizziness, accompanied by nausea, at a food and beverage tasting event where I ate much more than I usually do. Suddenly feeling that I might faint at any moment, I lay down on a concrete balcony for about 10 minutes until the disconcerting sensations passed, after which I felt completely normal.
The next morning I checked the internet for my symptom — dizziness after eating — and discovered the condition had a name: Postprandial hypotension, a sudden drop in blood pressure when too much blood is diverted to the digestive tract, leaving the brain relatively deprived. The condition most often affects older adults who may have an associated disorder like diabetes, hypertension or Parkinson’s disease that impedes the body’s ability to maintain a normal blood pressure. Fortunately, I am thus far spared any disorder linked to this symptom, but I’m now careful to avoid overeating lest it happen again.
“An essential problem is that almost every disease can cause dizziness,” say two medical experts who wrote a comprehensive new book, “Dizziness: Why You Feel Dizzy and What Will Help You Feel Better.” Although the vast majority of patients seen at dizziness clinics do not have a serious health problem, the authors, Dr. Gregory T. Whitman and Dr. Robert W. Baloh, emphasize that doctors must always “be on the alert for a serious disease presenting as ‘dizziness,’” like “stroke, transient ischemic attacks, multiple sclerosis and brain tumors.”
Benign paroxysmal positional vertigo can be caused by a blow to the head or be a result of aging. “Approximately one in five people in their 80s will develop B.P.P.V.,” the authors wrote. It can also affect younger people, particularly those who already have, or will develop, migraine headaches, they noted.Dr. Kevin A. Kerber, a neurotologist at the University of Michigan Health System, told me that dizziness is one of the most common symptoms that primary care and emergency department doctors see, as common as back pain and headache. He cited a nationally representative health survey conducted by the Centers for Disease Control and Prevention in 2008 in which 10 percent of adults said they had felt dizzy within the past year and had been referred to or seen by a health care specialist because of the symptom.
Typically, those reporting dizziness in the survey indicated they each had experienced three of the following different types: a spinning or vertigo sensation, including a rocking of yourself or your surroundings; a floating, spacey or tilting sensation; feeling lightheaded, without a sense of motion; feeling as if you are going to pass out or faint; blurring of your vision when you move your head; or feeling off-balance or unsteady.
As you can see, reporting a symptom simply as dizziness does not give a doctor much to go on. A major problem, Dr. Kerber said, is that the examining doctor has to decide on the type of dizziness and determine whether there may be a “particularly dangerous cause” like a heart attack or stroke based on “often unreliable” descriptions by patients.
People use the word dizziness when referring to lightheadedness, unsteadiness, motion intolerance, imbalance, floating or a tilting sensation. Vertigo, a subtype of dizziness, is an illusion of movement caused by uneven input to the inner ear’s vestibular system that provides a sense of balance and orientation in space. In 2011, an estimated 3.9 million people visited emergency departments with symptoms of dizziness or vertigo.
“Patients are generally nonspecific in describing their symptoms,” Dr. Kerber said. “They should spend time thinking about their symptoms before they see the doctor.” Factors to consider, he said, include “timing — does the dizziness occur episodically or is it constant? What seems to set it off — certain positions or particular foods? How long does the symptom last? And what happens over time — does it get worse, stay the same or get better?”
Note, too, whether the feelings get worse when you walk, stand up or move your head. Are the episodes accompanied by nausea, and do they occur so suddenly and severely that they force you to sit or lie down?
Family members or friends who pay attention to the affected individual’s complaints “can help contribute to a rapid and correct diagnosis,” according to the authors of the new book. Dr. Whitman is an otoneurology specialist at Massachusetts Eye and Ear Infirmary, and Dr. Baloh is director of the neurotology clinic and testing laboratory at the medical center of the University of California, Los Angeles.
Two of the most common causes of dizziness are triggered by changes in position. One is called orthostatic hypotension — a reduced flow of blood to the brain that occurs when a person gets up from a sitting or lying position and goes away when the person lies down.
The second, called benign paroxysmal positional vertigo, or B.P.P.V., is not exactly benign to those affected, Dr. Kerber said. It is triggered by a change in head position, for example, when lying down, turning over in bed, or bending the head backward while sitting or standing (called “top shelf vertigo”), the authors of “Dizziness” wrote. The person may feel that the world is moving or spinning or that an object in the room is jumping up and down rhythmically.
Vertigo is one of the most disabling causes of dizziness. It arises when tiny calcium particles in the inner ear become dislodged from the balance organ and get stuck in the semicircular canal, where “they cause havoc,” Dr. Kerber explained. When the head is moved, the particles shift and set off a sensitive nerve wired to the eyes, making them jerk and causing dizziness. When the particles settle down, the eyes stop jerking and the dizziness goes away.
Vertigo can be a disabling condition that lasts for weeks, months or even years. Those affected are often unable to work, drive or walk around without falling.
However, B.P.P.V. usually responds to a treatment like the Epley maneuver, a sequence of movements that re-positions the head and gets the errant particles to go back to where they belong. The maneuver is often performed by a health professional, but patients can learn to do it on their own if the vertigo recurs.
Symptom: Dizziness.
Cause: Often Baffling.
By Richard Saltus : NY Times Article : September 6, 2005
On the Fourth of July, a 63-year-old man was taken by wheelchair into the emergency room of a suburban Virginia hospital, overwhelmed with dizziness and nausea and gripped by sweat-inducing anxiety.
"I felt dim and lightheaded, like I was just going to fade out," said John Farquhar, a semiretired consultant in Washington. "I said, 'I'm going to die.' "
His wife, Lou, a nurse, had driven him to the hospital, taking big curves gingerly because the motion of a sweeping turn "made me feel like I was pulling 30 G's like a fighter pilot," said Mr. Farquhar, who otherwise was healthy and fit.
The attacks had begun the previous day, out of the blue, while he was playing with the couple's dog, Sascha.
Lifting her high in the air, "I snapped my head back, and suddenly it seemed that my body was turning, and the room was spinning around," Mr. Farquhar recounted. "I felt profoundly dizzy and nauseated."
The episode passed, but the queasiness returned not long afterward, set off by the on-screen action on a DVD. When Mr. Farquhar got out of bed the next day, the world was spinning so violently that he crumpled to his knees, and he could barely make his way to the bathroom, where he vomited, leading to the trip to the E.R.
Dizziness is one of the most miserable of sensations, and it can be disabling.
The technical term for the false sensation that you and the world are spinning is vertigo. (In Alfred Hitchcock's film "Vertigo," the James Stewart character actually suffers from acrophobia, or fear of heights.)
There are many causes of vertigo, most of them temporary and treatable, but sometimes the condition signals a serious problem, like a tumor \nor a stroke. Dizziness and lightheadedness are among the most frequent complaints that cause people to seek medical help.
Although doctors often see patients with the symptom, its cause can be a challenge to determine, said Dr. Jonathan Olshaker, chief of the emergency department at Boston Medical Center, who has written a textbook chapter on vertigo.
"The staff has a concern that they're not going to be able to figure out what it is, or that the person is a difficult-to-treat patient," Dr. Olshaker said. In fact, a vast majority of patients have a specific, identifiable cause for their dizziness, he said.
Even when the cause is probably not serious, doctors generally are cautious, ordering a number of tests and sometimes consulting with neurologists to make sure the cause of the vertigo is not life-threatening.
Ruling out life-threatening causes, the doctors told Mr. Farquhar that he was most likely suffering from benign paroxysmal positional vertigo.
The problem accounts for perhaps 25 to 40 percent of patients seeking medical attention for dizziness. "Paroxysmal" refers to the episodic pattern of vertigo attacks, and "positional" means that the spinning sensations are brought on by certain movements.
Tilting the head back to look upward is a typical trigger. The disorder has been nicknamed "top-shelf vertigo," and hair salon customers sometimes experience it when leaning back for a shampoo, as do patients sitting in dental chairs.
The diagnosis and treatment of vertigo have markedly improved in the last two decades. The cause of most benign positional vertigo is now believed to be calcium debris that has dislodged from a part of the inner ear and strayed into one of the fluid-filled semicircular canals of the sensitive vestibular system.
The system is a cluster of structures that keeps the brain updated on the body's orientation and movement in space.
These microscopic flecks of calcium debris do not in themselves lead to problems, but sometimes in their meandering they brush against delicate, hairlike cells, sending misinformation to the brain.
When those signals conflict with more accurate signals from other nerves, the brain responds with disorientation and vertigo.
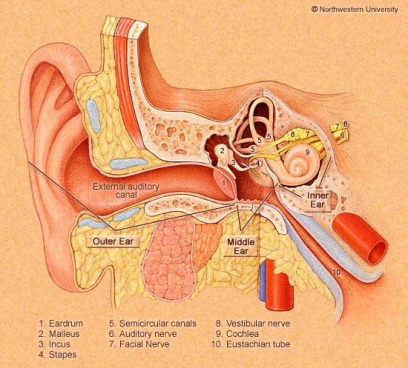
The three semicircular canals of the inner ear loop out - more or less at right angles, like three edges of a box meeting at the corner - from a chamber called the vestibule.
The slight fluid movements in these canals in response to head movements and gravity activate the hair-trigger cells that relay positional information to the brain.
Inside the vestibule, scores of tiny "stones" called otoliths are attached to \na membrane, and when the head turns in any direction, the slight force imparted to the otoliths is translated into nerve messages about motion and orientation. B.P.P.V., a common cause of dizziness caused by a malfunction of the inner ear's balance mechanism.
The problem accounts for perhaps 25 to 40 percent of patients seeking medical attention for dizziness. "Paroxysmal" refers to the episodic pattern of vertigo attacks, and "positional" means that the spinning sensations are brought on by certain movements.
The diagnosis and treatment of vertigo have markedly improved in the last two decades. The cause of most benign positional vertigo is now believed to be calcium debris that has dislodged from a part of the inner ear and strayed into one of the fluid-filled semicircular canals of the sensitive vestibular system.
The maneuvers involve moving the head into four different positions sequentially, taking advantage of gravity to roll the calcium flecks out of the sensitive part of the canal to a place where they cause less trouble.
In cases like Mr. Farquhar, the Epley maneuvers are repeated, the patient sits up, and the treatment is complete. For the next 48 hours, Mr. Farquhar was cautioned to avoid a variety of movements that could send the debris tumbling back into the canal.
Most doctors who do this say that 80 percent of patients have their symptoms alleviated in one set of treatments," Dr. Fitzgerald says.
The remaining 20 percent, he added, need repeated treatments, and the overall recurrence rate is 25 percent to 30 percent, though the episodes may not come back for months or years.
Within a few days, Mr. Farquhar was much improved and was able to walk several blocks and go into his office to work. Two months later, he continued to be free of nearly all his symptoms, except a brief lingering feeling of unease just after waking up in the morning.
For all but the most intractable cases, which occasionally require surgery, the simple and low-tech Epley maneuvers rank among the most effective and certainly the least costly of treatments for such a common and disabling source \nof misery.
"Vertigo is a horrible feeling," said Dr. Olshaker, the Boston emergency room chief. "The physician does need to have empathy for these patients. And in recent time, we're seeing more awareness of the condition and the Epley maneuvers, both in the E.R. and the primary care clinic."
A Stable Life, Despite Persistent Dizziness
By Jane E. Brody : NY Times Article : January 15, 2008
On the subway, children twirl themselves around the poles in the cars until they are so dizzy I’m ready to catch them. The young seem to delight in making the world spin out of control for a few moments, causing them to flop about like drunks. But when dizziness, vertigo or loss of balance is neither self-imposed nor short lived, it is anything but fun. It can throw one’s whole life out of kilter, literally and figuratively.This is what befell Cheryl Schiltz in 1997, when long treatment with the antibiotic gentamicin permanently damaged the vestibular apparatus in her inner ear. For three years, said Ms. Schiltz, of Madison, Wis., her world seemed to be made of Jell-O. Lacking a sense of balance, she wobbled with every step, and everything she looked at jiggled and tilted.Unable to work, Ms. Schiltz became increasingly isolated and struggled to perform the simplest household tasks.
Lisa Haven, executive director of the Vestibular Disorders Association, reports that “the risk of falling is two to three times greater in people with chronic imbalance or dizziness.” Nearly 9 percent of Americans 65 and older have balance problems, the prevalence of which is likely to increase as the 78 million baby boomers age.
Four Types of Dizziness :
The job of the vestibular system is to integrate sensory stimuli and movement for the brain and keep objects in visual focus as the body moves. When the head moves, signals are sent to the inner ear, an organ consisting of three semicircular canals surrounded by fluid. It in turn sends movement information to the vestibular nerve, which carries it to the brainstem and cerebellum, which control balance and posture and coordinate movement. Disruption of any part of the system can result in dizziness.
These are four types of dizziness, all of which are more common with increasing age:
What to Tell the Doctor:
About 40 percent of people experience at least one of these forms of dizziness at some time during their lives. When dizziness persists, medical care is essential, and so is the ability to provide a detailed description of the symptoms and what provokes them.
For example, for benign paroxysmal positional vertigo, a simple head-turning maneuver that repositions crystals in the inner ear may bring lasting relief. If ministrokes are the cause, the treatment may involve anticlotting drugs or opening a blocked artery with a stent. If medication is the problem, adjusting the dose or changing the drug can relieve dizziness. If dizziness persists despite treatment, lifestyle adjustments can help like avoiding sudden movements, keeping often-used items within easy reach, standing up slowly and clenching hands and flexing feet before standing. Physical therapy can help, as can exercises that strengthen muscles and that combine eye, head and body movements.Ms. Schiltz, whose vestibular system was damaged a decade ago, said she was told that nothing could be done about it. Nothing, that is, until she became the first patient to be treated with a device called a BrainPort invented by the late Dr. Paul Bach-y-Rita, a neurobiologist and rehabilitation medicine specialist, and his colleagues at the University of Wisconsin. The device takes advantage of the acute sensitivity of the tongue and sends balance signals directly to the brain from the tongue, bypassing the ear’s vestibular apparatus. At first, she used it a few minutes at a time, but soon found longer use kept her in balance for hours, then days, then weeks and months. Eventually, all that was needed was 20 minutes twice a day to train her brain, and she now uses it just occasionally.She is among more than 100 study participants who have used the BrainPort, including patients with multiple sclerosis, Parkinson’s disease and stroke. The device is available commercially in Canada and is awaiting approval by the Food and Drug Administration in the United States.Dr. Norman Doidge of the research faculty at the Columbia University Psychoanalytic Center and the University of Toronto describes Ms. Schiltz’s dramatic recovery in his new book about the plasticity of the brain, “The Brain That Changes Itself.” (Her case was also described in Science Times in November 2004.) With her sense of balance intact, Ms. Schiltz was able to return to school and on Dec. 20 received a degree in rehabilitation psychology.“I feel like a restored, even enhanced, person,” she said in an interview. “I’m living proof that the brain can be retrained. My goal now is to help people with acquired disabilities gain increased independence.”
New Views of Motion Sickness
Travel-Related Nausea Puzzles Scientists Amid Search for a Better Remedy; Ginger Root or a Nasal Spray?
Sumathi Reddy : WSJ : June 18, 2013
Researchers from the Navy, the National Aeronautics and Space Administration and academia are studying causes and potential treatments of motion sickness, hoping to formulate better products for situations that range from the extreme (space!) to the mundane (road trip to Grandma's, anyone?).
There's nothing quite like motion sickness to ruin summer travel, with symptoms including dizziness, headache, nausea and most unfortunately, vomiting. Some 25% to 40% of the population suffers from some degree of motion sickness, depending on the mode of transportation.
At Siena College, in Loudonville, N.Y., researchers have studied the effectiveness of ginger capsules, facial cooling and listening to music as a distraction for lessening symptoms and physiological responses to motion sickness.
NASA and the Navy are collaborating with pharmaceutical company Epiomed Therapeutics, of Irvine, Calif., to develop a nasal spray containing scopolamine, a drug currently used in a prescription-only patch for those prone to seasickness. Researchers say the drug's strong possible side effects, such as drowsiness and dry mouth, would be significantly reduced with a nasal spray.
Part of the difficulty with devising treatments is that experts don't know exactly what causes motion sickness. The prevailing belief is it is caused by a sensory mismatch between the visual and vestibular systems. The vestibular system, which is part of the inner ear, monitors movement and helps control balance.
In other words, our inner ear tells our brain that we are moving, but our eyes tell us we aren't, or vice versa. "When one of these is telling you you're in motion and the other one is telling you you're sitting, the brain gets confused with the mixed signals, and it causes this sense of sickness," says Abinash Virk, director of the travel and tropical medicine clinic at Mayo Clinic in Rochester, Minn.
What remain unknown are the reasons why the mismatch causes some individuals to react adversely. One long-standing theory is that the reactions are triggered by the brain's false identification of a toxin in the body, with nausea and vomiting a protective response to get rid of it.
Another theory is that body sway, or the change in a person's movements over short time intervals, can explain a propensity to get motion sickness. In Tom Stoffregen's lab at the University of Minnesota, the kinesiology professor measures each subject's body sway over a short period. He has found that individuals who are more susceptible have a more-erratic sway during and even before they are exposed to any stimulation.
Dr. Stoffregen uses a force plate, a glorified bathroom scale with pressure sensors, to take measurements of body movement as often as 200 times a second. He studies people both in a lab simulator and on ships.
In a forthcoming study to be published in the online journal PLOS ONE, Dr. Stoffregen tested the body sway of 35 cruise passengers aboard a ship in the Caribbean before departure. Passengers then reported the intensity of their seasickness. He found a link: Those who reported getting more sea sickness had more body sway at the dock.
"There may be sort of a general classification that people who are susceptible to motion sickness have," Dr. Stoffregen said. "Maybe they just move differently in general."
Max Levine, an associate professor of psychology at Siena College, studies behavioral and alternative motion-sickness treatments. In a recent experiment on about 50 individuals, half received capsules with ginger root and the remainder got a placebo. Then the individuals were seated in a chamber and exposed to a rotating device called an optokinetic drum that induces motion sickness.
"The folks who got ginger beforehand ended up doing much better both in terms of the symptoms they developed and in terms of the physiological reaction that they had in the stomach," he said.
Recent behavioral experiments have found that cool compresses or gel packs placed on the forehead are somewhat effective at controlling physiological changes, such as abnormal rhythmic stomach activity that generally accompanies nausea, but didn't significantly reduce nausea. Listening to one's favorite music as a distraction showed improvements in symptoms including nausea, as well as in physiological changes, Dr. Levine said. Now, Dr. Levine is studying how deep breathing and relaxation may aid in motion sickness.
Doctors say a common misperception is that traveling on an empty stomach helps. Wrong. It's better to eat a light meal beforehand, especially one high in protein.
In a 2004 study in Alimentary Pharmacology & Therapeutics, 18 individuals completed three trials. In one, they had a protein drink before exposure to a device that induces motion sickness. In a second trial, they had a carbohydrate drink, and the third time they had nothing. They fared best after the protein drink. Protein "really tends to get the stomach into that slow normal rhythmic activity more so than fats and carbohydrates," Dr. Levine said.
Children over age 2 seem more prone to motion sickness than adults. Some experts think children's extra-sharp senses may make them aware of even a slight mismatch. Adults in their golden years seem to experience motion sickness less often—perhaps because of habituation.
Women have a greater tendency than men to get motion sickness. Some experts believe this is because women also are more prone to getting migraines, and migraine sufferers have a higher rate of motion sickness. Or women may simply report motion sickness symptoms more often.
Doctors say prescription drugs and over-the-counter options like Dramamine are the best treatment option, though some can cause side effects. Such drugs work by suppressing the central nervous system's response to nausea-producing stimuli. They reduce symptoms for many people but aren't universally effective.
Some travelers rely on homeopathic remedies such as ginger or acupressure wrist bands. Sujana Chandrasekhar, director of New York Otology in New York City, said they aren't universally effective, but are "worth trying."
There are behavioral tips for preventing or minimizing symptoms. Cynthia Ryan knows them all. The 45-year-old Portland, Ore., resident has suffered from motion sickness since she was a child commuting to school along winding roads, her barf bag in hand. Now the executive director of the Vestibular Disorders Association, Ms. Ryan says individuals with vestibular disorders are prone to motion sickness.
Her rule of thumb is to always be the driver. "I almost never let somebody else drive," she said. "And if I do, I sit in the passenger seat." Even when sitting as the front passenger, Ms. Ryan says she does deep-breathing exercises and tries to focus on a fixed point on the road in front of her. "I can't participate in conversations," she said. "I can't read. Sometimes someone will pass me a smartphone and say, 'Can you read me the directions?' And I'll say, 'Not unless you want me to throw up in your car.' "
Watching television TV or reading in a car is a no-no. "Face forward in the vehicle to be as alert to what's happening outside the vehicle as the driver would be," Dr. Chandrasekhar said. "You want to try to match your eyes to what's going on and to what your inner ear is feeling." Experts say: Just close your eyes and sleep.
Living With a Sound You Can’t Turn Off
By Jane E. Brody : NY Times : December 3, 2012
Shortly after my 70th birthday, a high-pitched hum began in my left ear. I noticed it only during quiet times but soon realized that it never went away.
An ear, nose and throat specialist (otolaryngologist) examined my ears and took a thorough medical history that included questions about noise exposure and drugs I take. An audiologist checked my hearing.
Diagnosis: tinnitus, with a mild hearing loss in the upper range that closely matched the pitch of the hum.
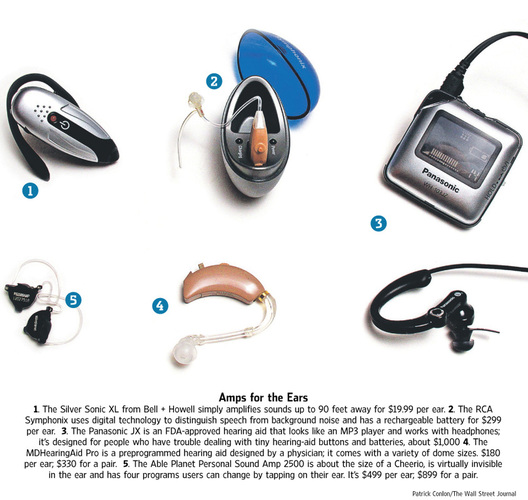
Although the hum was not particularly disturbing, I asked what might be done if it should get loud enough to interfere with my life and ability to hear speech clearly (about 85 percent of tinnitus cases are accompanied by hearing loss). The answer was that I could be fitted with a hearing aid.
But since my tinnitus is still mild, no mention was made of anything that might relieve the constant noise in my head.
Tinnitus is a chronic noise of varying intensity, loudness and pitch that has no external source. Rather, it seems to come from within a person's head. It is most apparent to the sufferer when all is quiet and may not be noticed when the person is otherwise distracted - while participating in physical activity, for example, or listening to music.
There is currently no cure for tinnitus, a potentially life-disrupting condition that affects about 10 to 20 percent of people, mostly those over age 65, but also many veterans of the wars in Iraq and Afghanistan. Among possible causes are head and neck injuries, drugs that damage the ear, blood vessel disease, autoimmune disorders, ear conditions and disorders of the temporomandibular joint.
Until recently, no treatment had been shown to have lasting effectiveness in controlled clinical trials, despite a host of remedies variously endorsed by hearing specialists and commercial interests.
In addition to a hearing aid, the most commonly prescribed remedy is a so-called masking device, a white-noise machine that introduces natural or artificial sound into the sufferer's ears in an attempt to suppress the perceived ringing. But eventually the noise of the masker can become as disruptive as the tinnitus.
"When patients respond poorly to the masking device, they are often told they haven't used it long or consistently enough," said Rilana F. F. Cima, a psychologist and researcher in the Netherlands.
Fear and Anxiety
Dr. Cima said in an interview that, like me, most people with tinnitus function fairly well. But for about 3 percent of people with the condition, it is extremely disabling, causing intense distress, fear and anxiety, and leaving them unable to function.
"Patients say the sound is driving them crazy," Dr. Cima said. "Their negative reaction to not wanting to hear it creates daily life impairment." She said patients would do almost anything to avoid hearing the sound in their heads and the feelings of fear and anxiety that result.
Recently Dr. Cima's team demonstrated the effectiveness of a multidisciplinary, psychology-based approach to this problem. The technique, published last spring in The Lancet, does not make the ringing go away, but it does show that now there is real hope for relief for people whose tinnitus impairs their ability to work, sleep and enjoy life.
In an accompanying editorial, Dr. Berthold Langguth of the University of Regensburg in Germany, an international authority on tinnitus, said the team's findings "overcome the idea that nothing can be done to treat tinnitus" and provide "a clear statement against therapeutic nihilism."
James Henry, a specialist in auditory rehabilitation at the Veterans Administration Medical Center in Portland, Ore., where many veterans with traumatic brain injuries are treated for tinnitus, said that Dr. Cima had done "probably the best study to date, a good job that is advancing the field."
An Improved Approach
The three-month treatment developed and carefully tested by the Dutch team is based on cognitive behavioral therapy and relies on principles of exposure therapy long proven effective to treat phobias. While the use of cognitive behavioral therapy for tinnitus is not new, the team's demonstration of a scientifically validated, comprehensive approach to the problem offers a therapeutic blueprint that others can use.
Unlike the use of a tinnitus masker, the treatment is simple, relatively brief and does not require patients to purchase or use devices to gain relief. If necessary, patients who "relapse" can return for a brief therapeutic brush-up.
Dr. Cima's team enrolled 492 patients with varying degrees of tinnitus and randomly assigned them to receive either usual care or "specialized" care. Usual care, in the Netherlands as well as in the United States, involves a medical exam and hearing test, typically followed by a prescription for a hearing aid and/or masking device.
Patients may also be given antidepressants, anti-anxiety drugs, sleep aids or other medication to relieve emotional distress and other disabling symptoms.
The Dutch treatment relies solely on psychological techniques. Following an education session about tinnitus and lessons in deep relaxation, patients are gradually exposed to an external source of the very ringing they hear in their heads. After 10 or 12 sessions, they become habituated to it and no longer find it threatening.
It is not the noise itself but "patients' extremely negative reaction to it that creates daily life impairment," Dr. Cima explained. "Patients are continuously stressed and fearful of it. It becomes a sign of a danger from which they must escape."
She likened the approach to helping people overcome their fear of spiders by inducing deep relaxation and gradually introducing them to increasingly realistic objects of their fear.
"They may never learn to love spiders, but they can live with them more comfortably," Dr. Cima said.
Dr. Henry of the veterans medical center, who has been involved in tinnitus research for a quarter century, said his team uses a similar approach with five treatment sessions, which "takes care of about 95 percent of cases," he said.
"Lots of veterans get tinnitus in association with traumatic brain injuries, but the tinnitus is often permanent even after these other injuries are resolved," Dr. Henry said. "We teach them skills that enable them to manage their tinnitus. They learn to reframe the problem in a more positive way. It's not a cure - nobody has a cure - but we're able to help most veterans and enable them to live a normal life."
A cure may emerge from findings of changes in the brains of tinnitus patients that are being revealed through sophisticated imaging techniques.
New Therapies Fight Phantom Noises of Tinnitus
By Kate Murphy : NY Times Article : April 1, 2008
Modern life is loud. The jolting buzz of an alarm clock awakens the ears to a daily din of trucks idling, sirens blaring, televisions droning, computers pinging and phones ringing — not to mention refrigerators humming and air-conditioners thrumming. But for the 12 million Americans who suffer from severe tinnitus, the phantom tones inside their head are louder than anything else.
By Jane E. Brody : NY Times : Feb. 6, 2017
Dizziness is not a disease but rather a symptom that can result from a huge variety of underlying disorders or, in some cases, no disorder at all. Readily determining its cause and how best to treat it — or whether to let it resolve on its own — can depend on how well patients are able to describe exactly how they feel during a dizziness episode and the circumstances under which it usually occurs.
For example, I recently experienced a rather frightening attack of dizziness, accompanied by nausea, at a food and beverage tasting event where I ate much more than I usually do. Suddenly feeling that I might faint at any moment, I lay down on a concrete balcony for about 10 minutes until the disconcerting sensations passed, after which I felt completely normal.
The next morning I checked the internet for my symptom — dizziness after eating — and discovered the condition had a name: Postprandial hypotension, a sudden drop in blood pressure when too much blood is diverted to the digestive tract, leaving the brain relatively deprived. The condition most often affects older adults who may have an associated disorder like diabetes, hypertension or Parkinson’s disease that impedes the body’s ability to maintain a normal blood pressure. Fortunately, I am thus far spared any disorder linked to this symptom, but I’m now careful to avoid overeating lest it happen again.
“An essential problem is that almost every disease can cause dizziness,” say two medical experts who wrote a comprehensive new book, “Dizziness: Why You Feel Dizzy and What Will Help You Feel Better.” Although the vast majority of patients seen at dizziness clinics do not have a serious health problem, the authors, Dr. Gregory T. Whitman and Dr. Robert W. Baloh, emphasize that doctors must always “be on the alert for a serious disease presenting as ‘dizziness,’” like “stroke, transient ischemic attacks, multiple sclerosis and brain tumors.”
Benign paroxysmal positional vertigo can be caused by a blow to the head or be a result of aging. “Approximately one in five people in their 80s will develop B.P.P.V.,” the authors wrote. It can also affect younger people, particularly those who already have, or will develop, migraine headaches, they noted.Dr. Kevin A. Kerber, a neurotologist at the University of Michigan Health System, told me that dizziness is one of the most common symptoms that primary care and emergency department doctors see, as common as back pain and headache. He cited a nationally representative health survey conducted by the Centers for Disease Control and Prevention in 2008 in which 10 percent of adults said they had felt dizzy within the past year and had been referred to or seen by a health care specialist because of the symptom.
Typically, those reporting dizziness in the survey indicated they each had experienced three of the following different types: a spinning or vertigo sensation, including a rocking of yourself or your surroundings; a floating, spacey or tilting sensation; feeling lightheaded, without a sense of motion; feeling as if you are going to pass out or faint; blurring of your vision when you move your head; or feeling off-balance or unsteady.
As you can see, reporting a symptom simply as dizziness does not give a doctor much to go on. A major problem, Dr. Kerber said, is that the examining doctor has to decide on the type of dizziness and determine whether there may be a “particularly dangerous cause” like a heart attack or stroke based on “often unreliable” descriptions by patients.
People use the word dizziness when referring to lightheadedness, unsteadiness, motion intolerance, imbalance, floating or a tilting sensation. Vertigo, a subtype of dizziness, is an illusion of movement caused by uneven input to the inner ear’s vestibular system that provides a sense of balance and orientation in space. In 2011, an estimated 3.9 million people visited emergency departments with symptoms of dizziness or vertigo.
“Patients are generally nonspecific in describing their symptoms,” Dr. Kerber said. “They should spend time thinking about their symptoms before they see the doctor.” Factors to consider, he said, include “timing — does the dizziness occur episodically or is it constant? What seems to set it off — certain positions or particular foods? How long does the symptom last? And what happens over time — does it get worse, stay the same or get better?”
Note, too, whether the feelings get worse when you walk, stand up or move your head. Are the episodes accompanied by nausea, and do they occur so suddenly and severely that they force you to sit or lie down?
Family members or friends who pay attention to the affected individual’s complaints “can help contribute to a rapid and correct diagnosis,” according to the authors of the new book. Dr. Whitman is an otoneurology specialist at Massachusetts Eye and Ear Infirmary, and Dr. Baloh is director of the neurotology clinic and testing laboratory at the medical center of the University of California, Los Angeles.
Two of the most common causes of dizziness are triggered by changes in position. One is called orthostatic hypotension — a reduced flow of blood to the brain that occurs when a person gets up from a sitting or lying position and goes away when the person lies down.
The second, called benign paroxysmal positional vertigo, or B.P.P.V., is not exactly benign to those affected, Dr. Kerber said. It is triggered by a change in head position, for example, when lying down, turning over in bed, or bending the head backward while sitting or standing (called “top shelf vertigo”), the authors of “Dizziness” wrote. The person may feel that the world is moving or spinning or that an object in the room is jumping up and down rhythmically.
Vertigo is one of the most disabling causes of dizziness. It arises when tiny calcium particles in the inner ear become dislodged from the balance organ and get stuck in the semicircular canal, where “they cause havoc,” Dr. Kerber explained. When the head is moved, the particles shift and set off a sensitive nerve wired to the eyes, making them jerk and causing dizziness. When the particles settle down, the eyes stop jerking and the dizziness goes away.
Vertigo can be a disabling condition that lasts for weeks, months or even years. Those affected are often unable to work, drive or walk around without falling.
However, B.P.P.V. usually responds to a treatment like the Epley maneuver, a sequence of movements that re-positions the head and gets the errant particles to go back to where they belong. The maneuver is often performed by a health professional, but patients can learn to do it on their own if the vertigo recurs.
Symptom: Dizziness.
Cause: Often Baffling.
By Richard Saltus : NY Times Article : September 6, 2005
On the Fourth of July, a 63-year-old man was taken by wheelchair into the emergency room of a suburban Virginia hospital, overwhelmed with dizziness and nausea and gripped by sweat-inducing anxiety.
"I felt dim and lightheaded, like I was just going to fade out," said John Farquhar, a semiretired consultant in Washington. "I said, 'I'm going to die.' "
His wife, Lou, a nurse, had driven him to the hospital, taking big curves gingerly because the motion of a sweeping turn "made me feel like I was pulling 30 G's like a fighter pilot," said Mr. Farquhar, who otherwise was healthy and fit.
The attacks had begun the previous day, out of the blue, while he was playing with the couple's dog, Sascha.
Lifting her high in the air, "I snapped my head back, and suddenly it seemed that my body was turning, and the room was spinning around," Mr. Farquhar recounted. "I felt profoundly dizzy and nauseated."
The episode passed, but the queasiness returned not long afterward, set off by the on-screen action on a DVD. When Mr. Farquhar got out of bed the next day, the world was spinning so violently that he crumpled to his knees, and he could barely make his way to the bathroom, where he vomited, leading to the trip to the E.R.
Dizziness is one of the most miserable of sensations, and it can be disabling.
The technical term for the false sensation that you and the world are spinning is vertigo. (In Alfred Hitchcock's film "Vertigo," the James Stewart character actually suffers from acrophobia, or fear of heights.)
There are many causes of vertigo, most of them temporary and treatable, but sometimes the condition signals a serious problem, like a tumor \nor a stroke. Dizziness and lightheadedness are among the most frequent complaints that cause people to seek medical help.
Although doctors often see patients with the symptom, its cause can be a challenge to determine, said Dr. Jonathan Olshaker, chief of the emergency department at Boston Medical Center, who has written a textbook chapter on vertigo.
"The staff has a concern that they're not going to be able to figure out what it is, or that the person is a difficult-to-treat patient," Dr. Olshaker said. In fact, a vast majority of patients have a specific, identifiable cause for their dizziness, he said.
Even when the cause is probably not serious, doctors generally are cautious, ordering a number of tests and sometimes consulting with neurologists to make sure the cause of the vertigo is not life-threatening.
Ruling out life-threatening causes, the doctors told Mr. Farquhar that he was most likely suffering from benign paroxysmal positional vertigo.
The problem accounts for perhaps 25 to 40 percent of patients seeking medical attention for dizziness. "Paroxysmal" refers to the episodic pattern of vertigo attacks, and "positional" means that the spinning sensations are brought on by certain movements.
Tilting the head back to look upward is a typical trigger. The disorder has been nicknamed "top-shelf vertigo," and hair salon customers sometimes experience it when leaning back for a shampoo, as do patients sitting in dental chairs.
The diagnosis and treatment of vertigo have markedly improved in the last two decades. The cause of most benign positional vertigo is now believed to be calcium debris that has dislodged from a part of the inner ear and strayed into one of the fluid-filled semicircular canals of the sensitive vestibular system.
The system is a cluster of structures that keeps the brain updated on the body's orientation and movement in space.
These microscopic flecks of calcium debris do not in themselves lead to problems, but sometimes in their meandering they brush against delicate, hairlike cells, sending misinformation to the brain.
When those signals conflict with more accurate signals from other nerves, the brain responds with disorientation and vertigo.
The three semicircular canals of the inner ear loop out - more or less at right angles, like three edges of a box meeting at the corner - from a chamber called the vestibule.
The slight fluid movements in these canals in response to head movements and gravity activate the hair-trigger cells that relay positional information to the brain.
Inside the vestibule, scores of tiny "stones" called otoliths are attached to \na membrane, and when the head turns in any direction, the slight force imparted to the otoliths is translated into nerve messages about motion and orientation. B.P.P.V., a common cause of dizziness caused by a malfunction of the inner ear's balance mechanism.
The problem accounts for perhaps 25 to 40 percent of patients seeking medical attention for dizziness. "Paroxysmal" refers to the episodic pattern of vertigo attacks, and "positional" means that the spinning sensations are brought on by certain movements.
The diagnosis and treatment of vertigo have markedly improved in the last two decades. The cause of most benign positional vertigo is now believed to be calcium debris that has dislodged from a part of the inner ear and strayed into one of the fluid-filled semicircular canals of the sensitive vestibular system.
The maneuvers involve moving the head into four different positions sequentially, taking advantage of gravity to roll the calcium flecks out of the sensitive part of the canal to a place where they cause less trouble.
In cases like Mr. Farquhar, the Epley maneuvers are repeated, the patient sits up, and the treatment is complete. For the next 48 hours, Mr. Farquhar was cautioned to avoid a variety of movements that could send the debris tumbling back into the canal.
Most doctors who do this say that 80 percent of patients have their symptoms alleviated in one set of treatments," Dr. Fitzgerald says.
The remaining 20 percent, he added, need repeated treatments, and the overall recurrence rate is 25 percent to 30 percent, though the episodes may not come back for months or years.
Within a few days, Mr. Farquhar was much improved and was able to walk several blocks and go into his office to work. Two months later, he continued to be free of nearly all his symptoms, except a brief lingering feeling of unease just after waking up in the morning.
For all but the most intractable cases, which occasionally require surgery, the simple and low-tech Epley maneuvers rank among the most effective and certainly the least costly of treatments for such a common and disabling source \nof misery.
"Vertigo is a horrible feeling," said Dr. Olshaker, the Boston emergency room chief. "The physician does need to have empathy for these patients. And in recent time, we're seeing more awareness of the condition and the Epley maneuvers, both in the E.R. and the primary care clinic."
A Stable Life, Despite Persistent Dizziness
By Jane E. Brody : NY Times Article : January 15, 2008
On the subway, children twirl themselves around the poles in the cars until they are so dizzy I’m ready to catch them. The young seem to delight in making the world spin out of control for a few moments, causing them to flop about like drunks. But when dizziness, vertigo or loss of balance is neither self-imposed nor short lived, it is anything but fun. It can throw one’s whole life out of kilter, literally and figuratively.This is what befell Cheryl Schiltz in 1997, when long treatment with the antibiotic gentamicin permanently damaged the vestibular apparatus in her inner ear. For three years, said Ms. Schiltz, of Madison, Wis., her world seemed to be made of Jell-O. Lacking a sense of balance, she wobbled with every step, and everything she looked at jiggled and tilted.Unable to work, Ms. Schiltz became increasingly isolated and struggled to perform the simplest household tasks.
Lisa Haven, executive director of the Vestibular Disorders Association, reports that “the risk of falling is two to three times greater in people with chronic imbalance or dizziness.” Nearly 9 percent of Americans 65 and older have balance problems, the prevalence of which is likely to increase as the 78 million baby boomers age.
Four Types of Dizziness :
The job of the vestibular system is to integrate sensory stimuli and movement for the brain and keep objects in visual focus as the body moves. When the head moves, signals are sent to the inner ear, an organ consisting of three semicircular canals surrounded by fluid. It in turn sends movement information to the vestibular nerve, which carries it to the brainstem and cerebellum, which control balance and posture and coordinate movement. Disruption of any part of the system can result in dizziness.
These are four types of dizziness, all of which are more common with increasing age:
- Faintness
- Loss of balance, feeling unsteady
- Vertigo
- Vague lightheadedness
What to Tell the Doctor:
About 40 percent of people experience at least one of these forms of dizziness at some time during their lives. When dizziness persists, medical care is essential, and so is the ability to provide a detailed description of the symptoms and what provokes them.
- What does the dizziness feel like — faintness, loss of balance, lightheadedness, a sensation that you or your surroundings are spinning or moving?
- When did the symptoms begin?
- How long do they last?
- What provokes or relieves them?
- What other symptoms like headache, ringing in the ears, impaired vision, difficulty walking, weakness or hearing loss accompany the dizziness?
- trying to reproduce the symptoms. For example, by rapidly standing and sitting, standing after lying down or lying on a tilt table while changes in blood pressure are measured.
- The doctor may test heart function with an electrocardiogram or an echocardiogram, an exercise stress test or a Holter monitor to detect abnormal rhythms.
- Vision tests may be performed, along with tests to evaluate balance and gait and
- C.T. or M.R.I. scans of the head, including noninvasive tests that check for narrowed or blocked arteries to the brain.
- If no physical explanation for dizziness is found, the patient may be checked for psychological disorders like depression, panic attacks or dissociation from the world.
For example, for benign paroxysmal positional vertigo, a simple head-turning maneuver that repositions crystals in the inner ear may bring lasting relief. If ministrokes are the cause, the treatment may involve anticlotting drugs or opening a blocked artery with a stent. If medication is the problem, adjusting the dose or changing the drug can relieve dizziness. If dizziness persists despite treatment, lifestyle adjustments can help like avoiding sudden movements, keeping often-used items within easy reach, standing up slowly and clenching hands and flexing feet before standing. Physical therapy can help, as can exercises that strengthen muscles and that combine eye, head and body movements.Ms. Schiltz, whose vestibular system was damaged a decade ago, said she was told that nothing could be done about it. Nothing, that is, until she became the first patient to be treated with a device called a BrainPort invented by the late Dr. Paul Bach-y-Rita, a neurobiologist and rehabilitation medicine specialist, and his colleagues at the University of Wisconsin. The device takes advantage of the acute sensitivity of the tongue and sends balance signals directly to the brain from the tongue, bypassing the ear’s vestibular apparatus. At first, she used it a few minutes at a time, but soon found longer use kept her in balance for hours, then days, then weeks and months. Eventually, all that was needed was 20 minutes twice a day to train her brain, and she now uses it just occasionally.She is among more than 100 study participants who have used the BrainPort, including patients with multiple sclerosis, Parkinson’s disease and stroke. The device is available commercially in Canada and is awaiting approval by the Food and Drug Administration in the United States.Dr. Norman Doidge of the research faculty at the Columbia University Psychoanalytic Center and the University of Toronto describes Ms. Schiltz’s dramatic recovery in his new book about the plasticity of the brain, “The Brain That Changes Itself.” (Her case was also described in Science Times in November 2004.) With her sense of balance intact, Ms. Schiltz was able to return to school and on Dec. 20 received a degree in rehabilitation psychology.“I feel like a restored, even enhanced, person,” she said in an interview. “I’m living proof that the brain can be retrained. My goal now is to help people with acquired disabilities gain increased independence.”
New Views of Motion Sickness
Travel-Related Nausea Puzzles Scientists Amid Search for a Better Remedy; Ginger Root or a Nasal Spray?
Sumathi Reddy : WSJ : June 18, 2013
Researchers from the Navy, the National Aeronautics and Space Administration and academia are studying causes and potential treatments of motion sickness, hoping to formulate better products for situations that range from the extreme (space!) to the mundane (road trip to Grandma's, anyone?).
There's nothing quite like motion sickness to ruin summer travel, with symptoms including dizziness, headache, nausea and most unfortunately, vomiting. Some 25% to 40% of the population suffers from some degree of motion sickness, depending on the mode of transportation.
At Siena College, in Loudonville, N.Y., researchers have studied the effectiveness of ginger capsules, facial cooling and listening to music as a distraction for lessening symptoms and physiological responses to motion sickness.
NASA and the Navy are collaborating with pharmaceutical company Epiomed Therapeutics, of Irvine, Calif., to develop a nasal spray containing scopolamine, a drug currently used in a prescription-only patch for those prone to seasickness. Researchers say the drug's strong possible side effects, such as drowsiness and dry mouth, would be significantly reduced with a nasal spray.
Part of the difficulty with devising treatments is that experts don't know exactly what causes motion sickness. The prevailing belief is it is caused by a sensory mismatch between the visual and vestibular systems. The vestibular system, which is part of the inner ear, monitors movement and helps control balance.
In other words, our inner ear tells our brain that we are moving, but our eyes tell us we aren't, or vice versa. "When one of these is telling you you're in motion and the other one is telling you you're sitting, the brain gets confused with the mixed signals, and it causes this sense of sickness," says Abinash Virk, director of the travel and tropical medicine clinic at Mayo Clinic in Rochester, Minn.
What remain unknown are the reasons why the mismatch causes some individuals to react adversely. One long-standing theory is that the reactions are triggered by the brain's false identification of a toxin in the body, with nausea and vomiting a protective response to get rid of it.
Another theory is that body sway, or the change in a person's movements over short time intervals, can explain a propensity to get motion sickness. In Tom Stoffregen's lab at the University of Minnesota, the kinesiology professor measures each subject's body sway over a short period. He has found that individuals who are more susceptible have a more-erratic sway during and even before they are exposed to any stimulation.
Dr. Stoffregen uses a force plate, a glorified bathroom scale with pressure sensors, to take measurements of body movement as often as 200 times a second. He studies people both in a lab simulator and on ships.
In a forthcoming study to be published in the online journal PLOS ONE, Dr. Stoffregen tested the body sway of 35 cruise passengers aboard a ship in the Caribbean before departure. Passengers then reported the intensity of their seasickness. He found a link: Those who reported getting more sea sickness had more body sway at the dock.
"There may be sort of a general classification that people who are susceptible to motion sickness have," Dr. Stoffregen said. "Maybe they just move differently in general."
Max Levine, an associate professor of psychology at Siena College, studies behavioral and alternative motion-sickness treatments. In a recent experiment on about 50 individuals, half received capsules with ginger root and the remainder got a placebo. Then the individuals were seated in a chamber and exposed to a rotating device called an optokinetic drum that induces motion sickness.
"The folks who got ginger beforehand ended up doing much better both in terms of the symptoms they developed and in terms of the physiological reaction that they had in the stomach," he said.
Recent behavioral experiments have found that cool compresses or gel packs placed on the forehead are somewhat effective at controlling physiological changes, such as abnormal rhythmic stomach activity that generally accompanies nausea, but didn't significantly reduce nausea. Listening to one's favorite music as a distraction showed improvements in symptoms including nausea, as well as in physiological changes, Dr. Levine said. Now, Dr. Levine is studying how deep breathing and relaxation may aid in motion sickness.
Doctors say a common misperception is that traveling on an empty stomach helps. Wrong. It's better to eat a light meal beforehand, especially one high in protein.
In a 2004 study in Alimentary Pharmacology & Therapeutics, 18 individuals completed three trials. In one, they had a protein drink before exposure to a device that induces motion sickness. In a second trial, they had a carbohydrate drink, and the third time they had nothing. They fared best after the protein drink. Protein "really tends to get the stomach into that slow normal rhythmic activity more so than fats and carbohydrates," Dr. Levine said.
Children over age 2 seem more prone to motion sickness than adults. Some experts think children's extra-sharp senses may make them aware of even a slight mismatch. Adults in their golden years seem to experience motion sickness less often—perhaps because of habituation.
Women have a greater tendency than men to get motion sickness. Some experts believe this is because women also are more prone to getting migraines, and migraine sufferers have a higher rate of motion sickness. Or women may simply report motion sickness symptoms more often.
Doctors say prescription drugs and over-the-counter options like Dramamine are the best treatment option, though some can cause side effects. Such drugs work by suppressing the central nervous system's response to nausea-producing stimuli. They reduce symptoms for many people but aren't universally effective.
Some travelers rely on homeopathic remedies such as ginger or acupressure wrist bands. Sujana Chandrasekhar, director of New York Otology in New York City, said they aren't universally effective, but are "worth trying."
There are behavioral tips for preventing or minimizing symptoms. Cynthia Ryan knows them all. The 45-year-old Portland, Ore., resident has suffered from motion sickness since she was a child commuting to school along winding roads, her barf bag in hand. Now the executive director of the Vestibular Disorders Association, Ms. Ryan says individuals with vestibular disorders are prone to motion sickness.
Her rule of thumb is to always be the driver. "I almost never let somebody else drive," she said. "And if I do, I sit in the passenger seat." Even when sitting as the front passenger, Ms. Ryan says she does deep-breathing exercises and tries to focus on a fixed point on the road in front of her. "I can't participate in conversations," she said. "I can't read. Sometimes someone will pass me a smartphone and say, 'Can you read me the directions?' And I'll say, 'Not unless you want me to throw up in your car.' "
Watching television TV or reading in a car is a no-no. "Face forward in the vehicle to be as alert to what's happening outside the vehicle as the driver would be," Dr. Chandrasekhar said. "You want to try to match your eyes to what's going on and to what your inner ear is feeling." Experts say: Just close your eyes and sleep.
Living With a Sound You Can’t Turn Off
By Jane E. Brody : NY Times : December 3, 2012
Shortly after my 70th birthday, a high-pitched hum began in my left ear. I noticed it only during quiet times but soon realized that it never went away.
An ear, nose and throat specialist (otolaryngologist) examined my ears and took a thorough medical history that included questions about noise exposure and drugs I take. An audiologist checked my hearing.
Diagnosis: tinnitus, with a mild hearing loss in the upper range that closely matched the pitch of the hum.
Although the hum was not particularly disturbing, I asked what might be done if it should get loud enough to interfere with my life and ability to hear speech clearly (about 85 percent of tinnitus cases are accompanied by hearing loss). The answer was that I could be fitted with a hearing aid.
But since my tinnitus is still mild, no mention was made of anything that might relieve the constant noise in my head.
Tinnitus is a chronic noise of varying intensity, loudness and pitch that has no external source. Rather, it seems to come from within a person's head. It is most apparent to the sufferer when all is quiet and may not be noticed when the person is otherwise distracted - while participating in physical activity, for example, or listening to music.
There is currently no cure for tinnitus, a potentially life-disrupting condition that affects about 10 to 20 percent of people, mostly those over age 65, but also many veterans of the wars in Iraq and Afghanistan. Among possible causes are head and neck injuries, drugs that damage the ear, blood vessel disease, autoimmune disorders, ear conditions and disorders of the temporomandibular joint.
Until recently, no treatment had been shown to have lasting effectiveness in controlled clinical trials, despite a host of remedies variously endorsed by hearing specialists and commercial interests.
In addition to a hearing aid, the most commonly prescribed remedy is a so-called masking device, a white-noise machine that introduces natural or artificial sound into the sufferer's ears in an attempt to suppress the perceived ringing. But eventually the noise of the masker can become as disruptive as the tinnitus.
"When patients respond poorly to the masking device, they are often told they haven't used it long or consistently enough," said Rilana F. F. Cima, a psychologist and researcher in the Netherlands.
Fear and Anxiety
Dr. Cima said in an interview that, like me, most people with tinnitus function fairly well. But for about 3 percent of people with the condition, it is extremely disabling, causing intense distress, fear and anxiety, and leaving them unable to function.
"Patients say the sound is driving them crazy," Dr. Cima said. "Their negative reaction to not wanting to hear it creates daily life impairment." She said patients would do almost anything to avoid hearing the sound in their heads and the feelings of fear and anxiety that result.
Recently Dr. Cima's team demonstrated the effectiveness of a multidisciplinary, psychology-based approach to this problem. The technique, published last spring in The Lancet, does not make the ringing go away, but it does show that now there is real hope for relief for people whose tinnitus impairs their ability to work, sleep and enjoy life.
In an accompanying editorial, Dr. Berthold Langguth of the University of Regensburg in Germany, an international authority on tinnitus, said the team's findings "overcome the idea that nothing can be done to treat tinnitus" and provide "a clear statement against therapeutic nihilism."
James Henry, a specialist in auditory rehabilitation at the Veterans Administration Medical Center in Portland, Ore., where many veterans with traumatic brain injuries are treated for tinnitus, said that Dr. Cima had done "probably the best study to date, a good job that is advancing the field."
An Improved Approach
The three-month treatment developed and carefully tested by the Dutch team is based on cognitive behavioral therapy and relies on principles of exposure therapy long proven effective to treat phobias. While the use of cognitive behavioral therapy for tinnitus is not new, the team's demonstration of a scientifically validated, comprehensive approach to the problem offers a therapeutic blueprint that others can use.
Unlike the use of a tinnitus masker, the treatment is simple, relatively brief and does not require patients to purchase or use devices to gain relief. If necessary, patients who "relapse" can return for a brief therapeutic brush-up.
Dr. Cima's team enrolled 492 patients with varying degrees of tinnitus and randomly assigned them to receive either usual care or "specialized" care. Usual care, in the Netherlands as well as in the United States, involves a medical exam and hearing test, typically followed by a prescription for a hearing aid and/or masking device.
Patients may also be given antidepressants, anti-anxiety drugs, sleep aids or other medication to relieve emotional distress and other disabling symptoms.
The Dutch treatment relies solely on psychological techniques. Following an education session about tinnitus and lessons in deep relaxation, patients are gradually exposed to an external source of the very ringing they hear in their heads. After 10 or 12 sessions, they become habituated to it and no longer find it threatening.
It is not the noise itself but "patients' extremely negative reaction to it that creates daily life impairment," Dr. Cima explained. "Patients are continuously stressed and fearful of it. It becomes a sign of a danger from which they must escape."
She likened the approach to helping people overcome their fear of spiders by inducing deep relaxation and gradually introducing them to increasingly realistic objects of their fear.
"They may never learn to love spiders, but they can live with them more comfortably," Dr. Cima said.
Dr. Henry of the veterans medical center, who has been involved in tinnitus research for a quarter century, said his team uses a similar approach with five treatment sessions, which "takes care of about 95 percent of cases," he said.
"Lots of veterans get tinnitus in association with traumatic brain injuries, but the tinnitus is often permanent even after these other injuries are resolved," Dr. Henry said. "We teach them skills that enable them to manage their tinnitus. They learn to reframe the problem in a more positive way. It's not a cure - nobody has a cure - but we're able to help most veterans and enable them to live a normal life."
A cure may emerge from findings of changes in the brains of tinnitus patients that are being revealed through sophisticated imaging techniques.
New Therapies Fight Phantom Noises of Tinnitus
By Kate Murphy : NY Times Article : April 1, 2008
Modern life is loud. The jolting buzz of an alarm clock awakens the ears to a daily din of trucks idling, sirens blaring, televisions droning, computers pinging and phones ringing — not to mention refrigerators humming and air-conditioners thrumming. But for the 12 million Americans who suffer from severe tinnitus, the phantom tones inside their head are louder than anything else.
Often caused by prolonged or sudden exposure to loud noises, tinnitus (pronounced tin-NIGHT-us or TIN-nit-us) is becoming an increasingly common complaint, particularly among soldiers returning from combat, users of portable music players, and aging baby boomers reared on rock ’n’ roll. (Other causes include stress, some kinds of chemotherapy, head and neck trauma, sinus infections, and multiple sclerosis.)
Although there is no cure, researchers say they have never had a better understanding of the cascade of physiological and psychological mechanisms responsible for tinnitus. As a result, new treatments under investigation — some of them already on the market — show promise in helping patients manage the ringing, pinging and hissing that otherwise drives them to distraction.
The most promising therapies, experts say, are based on discoveries made in the last five years about the brain activity of people with tinnitus. With brain-scanning equipment like functional magnetic resonance imaging, researchers in the United States and Europe have independently discovered that the brain areas responsible for interpreting sound and producing fearful emotions are exceptionally active in people who complain of tinnitus.
“We’ve discovered that tinnitus is not so much ringing in the ears as ringing in the brain,” said Thomas J. Brozoski, a tinnitus researcher at Southern Illinois University School of Medicine in Springfield.
Indeed, tinnitus can be intense in people with hearing loss and even those whose auditory nerves have been completely severed. In the absence of normal auditory stimulation, the brain is like a driver trying to tune in to a radio station that is out of range. It turns up the volume trying but gets only annoying static. Richard Salvi, director of the Center for Hearing and Deafness at the State University of New York at Buffalo, said the static could be “neural noise” — the sound of nerves firing. Or, he said, it could be a leftover sound memory.
Adam Edwards, a 34-year-old co-owner of a wheel repair shop in Dallas, said he developed tinnitus four years ago after target shooting with a pistol. “I had all the risk factors,” he said. “I grew up hunting, I played drums in a band, I went to loud concerts, I have a loud work environment — everything but living next to a missile launch site.” His tinnitus, which he described as a “computer beeping” sound, was so intense and persistent that he needed sedatives to sleep at night.
Mr. Edwards says he has gotten relief from a device developed by an Australian audiologist, which became widely available in the United States last year. Manufactured by Neuromonics Inc. of Bethlehem, Pa., it looks like an MP3 player and delivers sound spanning the full auditory spectrum, digitally embedded in soothing music.
Similar to white noise, the broadband sound, tailored to each patient’s hearing ability, masks the tinnitus. (The music is intended to ease the anxiety that often accompanies the disorder.) Patients wear the $5,000 device, which is usually not covered by health insurance, for a minimum of two hours a day for six months. Since completing the treatment regimen last year, Mr. Edwards said his tinnitus had “become sort of like Muzak at a department store — you hear it if you think about it, but otherwise you don’t really notice.”
A small, company-financed study in the journal Ear & Hearing in April 2007 indicated that the Neuromonics method was 90 percent successful at reducing tinnitus. A larger study is under way to determine its long-term effectiveness.
Anne Howell, an audiologist at the Callier Center for Communication Disorders at the University of Texas at Dallas, said the Neuromonics device was a big improvement over older sound therapies that required wearing something that looked like a hearing aid all the time and took 18 to 24 months.
“The length of time was discouraging for many patients,” she said. “And a lot of them told me that wearing something that looks like a hearing aid would cause a problem in their professional life.”
Other treatments showing promise include surgically implanted electrodes and noninvasive magnetic stimulation, both intended to disrupt and possibly reset the faulty brain signals responsible for tinnitus. Using functional M.R.I. to guide them, neurosurgeons in Belgium have performed the implant procedure on several patients in the last year and say it has suppressed tinnitus entirely.
But the treatment is controversial. “It’s a radical option and not proven yet,” said Jennifer R. Melcher, an assistant professor of otology and laryngology at Harvard Medical School.
The magnetic therapy, similar to treatments used for depression and chronic pain, involves holding a magnet in the shape of a figure eight over the skull. Clinicians use functional M.R.I. to aim the magnetic pulses so they reach regions of the brain responsible for interpreting sound. Patients receive a pulse every second for about 20 minutes. “It works for some people but not for others,” said Anthony Cacace, professor of communication science and nerve disorders at Wayne State University in Detroit. Since tinnitus has so many causes, Dr. Cacace said, the challenge now is to find out which “subsets of patients benefit from this treatment.”
Researchers in Brazil have published a study indicating that a treatment called cranial-sacral trigger point therapy can relieve tinnitus in some head and neck trauma cases by releasing muscles that constrict hearing and neural pathways.
And drugs intended to treat alcoholism, epilepsy, Alzheimer’s and depression that alter levels of various neurotransmitters in the brain like serotonin, dopamine and gamma-aminobutyric acid have quieted tinnitus in some published animal and human studies.
“We’ve never been so hopeful,” said Dr. Salvi, of SUNY Buffalo, “of finding treatments for a disorder that haunts people and follows them everywhere they go.”
That Buzzing Sound : The mystery of tinnitus.
by Jerome Groopman, MD
The New Yorker : February 9, 2009
Tinnitus is one of the most common clinical conditions in the United States.
I noticed the sound one evening about a year ago. At first, I thought an alarm had been set off. Then I realized that the noise—a high-pitched drone—was mainly in my right ear. It has been with me ever since. The tone varies, from a soft whoosh like a shower to a piercing screech resembling a dental drill. When I am engaged in work at the hospital or in the laboratory, it seems distant. But in idle moments it gets louder and more annoying, once even jarring me from a dream.
Tinnitus—the false perception of sound in the absence of an acoustic stimulus, a phantom noise—is one of the most common clinical syndromes in the United States, affecting twelve per cent of men and almost fourteen per cent of women who are sixty-five and older. It only rarely afflicts the young, with one significant exception: those serving in the armed forces. Tinnitus affects nearly half the soldiers exposed to blasts in Iraq and Afghanistan.
This past August, I visited the University of Buffalo, which houses one of the major clinical and research centers for the evaluation and study of tinnitus. After filling out a detailed questionnaire, I met with Christina Stocking of the Speech-Language and Hearing Clinic, who has a doctorate in audiology and specializes in the condition. Stocking thought that I might have suffered noise trauma during a youth spent on the New York City subways. Sitting in the first row of a rock concert exposes you to between a hundred and ten and a hundred and twenty decibels; the screech of the New York subways can reach about a hundred and fifteen decibels. Moreover, since much of the New York subway system is underground, the noise reverberates in the tunnels, unlike in Boston, where many of the trains are above ground and noise dissipates, or in Paris, where several metro lines run on rubber wheels.
Normally, the outer ear, known as the pinna, collects sound waves and directs them into the ear canal, which carries the sound waves to the eardrum. In turn, the eardrum vibrates, and these tremors are picked up by the three tiny bones in the middle ear: the malleus (resembling a club), the incus (shaped like an anvil), and the stapes (similar to a stirrup). These bones amplify the sound vibrations and transmit them to the inner ear, where the cochlea converts the vibrations into electrical impulses, which travel from the acoustic nerve to the part of the brain that processes sound, the auditory cortex. Tinnitus can be temporary, caused by excess wax, an infection of the inner ear, or the toxic effects of drugs like aspirin (which appears to weaken the neural signals from the ear to the brain) or those used to treat cancer. Some people with normal hearing develop spontaneous tinnitus when placed in total silence; this is believed to be a response of the auditory cortex to the abnormal absence of all ambient sounds. But the majority of people with chronic symptoms develop them in conjunction with hearing loss. With the recent proliferation of MP3 players, rates of hearing loss and tinnitus may rise sharply in the coming years. A recent European Union study has projected that as many as ten million Europeans may be at risk of developing severe hearing loss as they age; and, according to the American Academy of Audiology, noise-induced hearing loss affects about one out of every eight children in the United States.
The range of tinnitus’s severity is as wide as the ways of describing the syndrome. Martin Amis, in “Money,” characterizes the tinnitus that his character John Self suffers as “jet take-offs, breaking glass, ice scratched from the tray.” In “A Pair of Blue Eyes,” Thomas Hardy’s William Worm complains of “people frying fish: fry, fry, fry, all day long in my poor head.” Some patients also suffer from hyperacusis, in which certain sounds are amplified in a painful way. As part of a standard evaluation, patients are given a series of tests: a tympanogram, to determine how the eardrums respond to air pressure; an assessment of the cochlea’s response to sound; and a standard audiogram, to test the frequency and intensity of sounds that define the span of hearing. Although my eardrums functioned well, Stocking said, the last two tests showed signs common to hearing loss at high frequencies, usually owing to age and noise trauma.
The audiologists at the Buffalo clinic see between a hundred and fifty and two hundred tinnitus patients a year, nearly all of them referred by physicians because the noise is disrupting their lives. Last May, David Nowak, a sixty-four-year-old retired machine repairman, had an ear infection that his doctor treated with antibiotics. Shortly thereafter, he heard a loud horn in the street, and has been plagued by tinnitus ever since. “It’s so loud that I can’t drown it out,” he told me. “It is a high-pitched squeal most of the time.” Nowak said that, before the tinnitus, “I didn’t have a care in the world—I cut the grass and I played with my granddaughter.” Now, he said, “My life has come to a halt. I can’t do anything. I can’t concentrate.” One Sunday, he told me, he went out and stood by a metal flagpole during a storm, hoping that lightning would strike, and that he had gone to the cemetery and “begged my mother to take me. I wish I would pass away.”
Tinnitus may have been described as early as the Seventeenth Dynasty, in Egypt (1650-1532 B.C.): an ancient Egyptian text, the Medical Book from Crocodilopolis (circa 150 B.C.), contains references to a “humming in the ear.” Treatment involved pouring herbs, oil, frankincense, tree sap, and soil into the ear using a reed stalk. The earliest undisputed description of the condition comes from Hippocrates, who used three words to describe the problem: echos, meaning sound; bombos, denoting buzzing; and psophos, indicating a slight sound. (Our word “tinnitus” derives from the Latin tinnire, meaning to ring.) The Greco-Roman therapy ranged from holding one’s breath in an effort to expel offending humors from the ear to placing honey, vinegar, cucumber juice, and radish extract in the ear. Hippocrates did make an observation that serves as the foundation for modern therapy: “Why is it that the buzzing in the ear ceases if one makes a sound? Is it because the greater sound drives out the less?”
In the modern era, people with tinnitus were thought to be suffering from anxiety or delusion, or to be subject to the transmission of spontaneous impulses from the nerve within the ear. Researchers have only recently begun to explore the neurological basis for tinnitus. Richard Salvi, a professor at the University of Buffalo, is one of the leading experts in the field. As a graduate student at Upstate Medical Center, in Syracuse, Salvi had set out to identify the “neurological signature” for tinnitus by treating rats and mice with drugs that injured the auditory nerve; conventional wisdom held that, after damage to the hearing apparatus in the inner ear, increased output from the cochlea would create the constant ringing or buzzing sound perceived as tinnitus. Salvi recalled, “Instead of seeing hyperactivity, which was the prevailing opinion about tinnitus, it was just the opposite. Output would actually slow down. You had a severely deafened animal, and nothing coming out of the inner ear—no spontaneous activity at all.”
Salvi moved to the University of Buffalo in 1987. He had begun to consider a new theory, in which hyperactivity originated in the central nervous system rather than in the inner ear. He collaborated with Dr. Alan Lockwood, a neurologist at the University of Buffalo. “Initially, we were going to do images of the brains of people who are normal and people with tinnitus,” Salvi recalled. “But when you are doing any sort of brain-imaging project what you have is all the other confounding variables”—such as age, gender, and head size. Shortly after Salvi’s arrival, he met with a group of local residents who had formed a tinnitus support group. One person, Salvi recalled, got up and said, “ ‘Dr. Salvi, I stick my tongue out and my tinnitus gets louder.’ I looked at the person, and my eyes started to wobble around in my head, and I thought, What’s going on with this person?” Then a second person got up and said, “When I clench my jaw, my tinnitus gets quieter.” Salvi told me, “A light bulb went off in my head. It seemed like what we should be doing with imaging studies was not comparing normal people to those with tinnitus but, rather, having these people come in and get scanned when their tinnitus was quiet, and then again while doing something like sticking out their tongue, which made it louder. In the same patient we can determine what part of the brain was changing.”
The first PET-scan results were unexpected. Whereas a real sound will activate areas on both sides of the brain, “we found a big increase in activity in just one side of the brain,” Salvi told me. If the origins of tinnitus were in the ear, it would activate both sides of the brain; when only one side appeared active, it suggested that the tinnitus originated in the central nervous system. The brain became hyperactive in an effort to compensate for the reduced input, generating phantom sounds. This conclusion, which was published in the journal Neurology in 1998, began to change the way that researchers approached tinnitus. Still, there is no convincing explanation for why only one side of the brain shows activity in people with tinnitus, particularly since it doesn’t appear consistently on either the right or the left side.
Another oddity is a type of tinnitus called “gaze-evoked,” in which ringing in the ears is occasioned or worsened by moving one’s eyes to the right or left, or up or down. Case studies reported gaze-evoked tinnitus in patients who had had a tumor on the auditory nerve which was surgically removed. “The patient goes completely deaf in that ear, and then he starts hearing the phantom sound of tinnitus in the ear which is deaf,” Salvi explained. “The ear isn’t even connected to the brain anymore.” When patients with gaze-evoked tinnitus were given PET scans, some showed activity in the angular gyrus, an area of the brain near the auditory cortex; others had activity in the brain stem. “The bottom line was that you perceive tinnitus in your deaf ear but there is no nerve there, no input,” he went on. “So it has to come from various parts of the brain.”
Jean-Luc Puel, a professor of neuroscience in Montpellier, France, is not convinced that tinnitus always originates as a phantom sound in the brain. He has studied rats and guinea pigs that were treated with high doses of aspirin or exposed to noise trauma. Puel believes that glutamate, a neurotransmitter, is inappropriately processed in the cochlea, which causes abnormal impulses from the acoustic nerve, and that by infusing the animal’s ear with a drug that blocks the action of glutamate he can reduce the tinnitus. More broadly, Puel argues that the disorder may have multiple causes. “This conflict between peripheral and central origin of tinnitus is simplistic,” he said. “To have perception of tinnitus, which is subjective, you need a brain.” Puel allows that his view is contrarian, adding, “I like to arrive at scientific meetings and disturb people.” But he also believes that different causes of tinnitus may reflect differences in biology. “There is no one type of tinnitus,” he told me.
When I visited Salvi’s laboratories, Edward Lobarinas, a researcher, was conducting experiments on rats that had been subjected to acoustic trauma. Lobarinas showed me a Plexiglas platform with an embedded pressure sensor attached to a computer. On top of the Plexiglas was a metal mesh canopy. First, a normal rat that served as a control was caged under the canopy and the entire apparatus was placed inside an acoustic chamber, into which Lobarinas delivered a steady noise with a narrow frequency range. “It’s a continual sound in the background, a sort of sh-h-h,” he said. This was interrupted by a loud bang. “The animal startles,” he said, and this sent a measurement of the movement through the pressure sensor to the computer screen, which showed a sharp spike.
In the next step, the sudden bang was preceded by a silent gap in the noise. This time, the rat had a much smaller startle reflex, seen on the computer as a low peak. “When you have a silent gap before the loud noise, you’re less startled,” Lobarinas said. “It’s like when it’s dark and you’re in your room and a bogeyman jumps out at you. You have a maximum startle. But if, before the bogeyman jumps out, the door is slowly creaking open, you sort of know the bogeyman is going to come out, and that decreases your startle.”
When a rat with induced hearing loss underwent the same experiment, it had a robust startle reflex even when the loud noise was preceded by silence. “The rat has tinnitus,” Lobarinas said. “It can’t tell us, of course, but it has constant buzzing in the ear, and we know that although it hears, it doesn’t perceive the silent gap because of tinnitus. So its startle reflex is not attenuated. It doesn’t hear the door slowly creaking open, just the bogeyman.”
Total funding for tinnitus research in the United States has recently been little more than three million dollars. “People don’t realize how complicated tinnitus really is,” Salvi said. “It’s in the same league as epilepsy and many neurological disorders. But so little money is spent on it, so there is almost no scientific database you can build on.”
Perry Jefferies, now a forty-eight-year-old retired Army first sergeant, entered Iraq with the 4th Infantry Division in April, 2003, as part of the initial invasion of Operation Iraqi Freedom. “We moved from Kuwait to Baghdad,” he told me, when we spoke by phone, “and then went up to Tikrit, until we were posted at the Iran border.” Jefferies escorted and resupplied units moving into battle. After one firefight, as his convoy was evacuating an injured Iraqi soldier, U.S. helicopters fired missiles into enemy ammunition bunkers. “We were right there at the explosions,” he said. Later, as his convoy was resupplying a unit near the border with Iran, a massive explosion at a nearby Iraqi fort rocked his Humvee. “We think that looters set it off,” he said. “It fried the fort.”
Although hearing trauma was most intense in combat, Jefferies said, he had been exposed to repeated noise during his many years in the military. During basic training, while on the weapons range, “we only wore one earplug, so you could hear the instructor when he yelled at you.” While learning how to fire a .50-calibre gun from an armored personnel carrier, he recalled, “we had no hearing protection. Afterwards, blood was coming out of one of my ears.” He had ruptured his right eardrum. Even so, the close-range explosion at the fort was different from anything he had experienced before. “I felt like I was under water for a few minutes,” he said. Since that time, he has been afflicted with tinnitus. “It is a high, steady electronic tone,” he told me. “And my ears feel heavy and blocked.”
As a first sergeant, Jefferies acted as an adviser to soldiers during their deployment. “One of my jobs was to try to find answers,” he said. “But I don’t remember any discussion about hearing protection.” The soldiers in his unit were required to carry earplugs, but many of them would simply attach the case to the front of their protective vests. “I had to listen sometimes to three different radios in the Humvee and respond,” Jefferies went on. No one, he told me, wore hearing protection, even when machine guns were test-fired on the base. In 2004, Jefferies retired from active service and was awarded the Bronze Star and the Legion of Merit.
Jefferies’s hearing fluctuates, at times diminishing to thirty-five per cent below normal, and he is now receiving ten-per-cent disability compensation for tinnitus. He is active in the Iraq and Afghanistan Veterans of America and works as a blood-donor recruiter at Robertson Blood Center, at Fort Hood, in Texas. “It is hard to hear in a bar or restaurant, hard to discern certain words, and I have to turn up the TV,” he told me. At times, the high-pitched drone of his tinnitus wakes him in the middle of the night.
A recent report from the Department of Veterans Affairs estimated that nearly seventy thousand of the 1.3 million soldiers who have served in Iraq and Afghanistan are collecting disability for tinnitus, and more than fifty-eight thousand are on disability for hearing loss. In 2006, the V.A. reportedly spent five hundred and thirty-nine million dollars on payments to veterans with tinnitus. A survey of more than a hundred and forty-one thousand Army active-duty, reserve, and Guard members who were examined in audiology clinics from April, 2003, through March, 2004, showed that tinnitus accounted for more than thirty per cent of post-deployment-related diagnoses. The study, from the U.S. Army Center for Health Promotion and Preventive Medicine, concluded, “There were not adequate supplies of earplugs to fit all deploying soldiers. There was also failure of an Army medical readiness automation system . . . to provide unit commanders with information regarding troops having adequate hearing protection. . . . Finally, there is evidence . . . that soldiers having blast injuries may not have been referred to audiology for adequate evaluation and treatment.” As with body armor and protective shielding on Humvees, the Pentagon had failed to anticipate the kind of hearing-protection devices that were needed. Even soldiers who were provided with earplugs were given insufficient instruction in their use; mistakenly believing that the earplugs could interfere with low-frequency sounds, like whispered commands during search-and-destroy operations, many chose not to use them.
Theresa Schulz, an audiologist who served in the military for twenty-one years, told me that hearing loss accompanying tinnitus is now the No. 1 cause of disability among veterans of the conflicts in Afghanistan and Iraq. “I think it’s probably because of the nature of urban warfare,” she said, given that gunfire and mortar and grenade explosions occur in relatively confined and often closed areas. After Schulz left the military, she worked for the National Institute for Occupational Safety and Health, in the field of hearing conservation among workers, and she is now employed in the private sector, developing devices that can protect against noise trauma. For civilians, Schulz noted, extraordinary noise like construction blasts or jackhammering can often be anticipated and protected against, but “in the military that’s not the case. It can come up anytime.”
In the fall of 2004, in an article for Hearing Health titled “Troops Return with Alarming Rates of Hearing Loss,” Schulz wrote, “Unfortunately, the resources required to accomplish the hearing conservation mission throughout the armed forces are diminishing just as the problem worsens.” Positions for active-duty audiologists, Schulz noted, were quickly being eliminated; since 1990, these positions had dwindled from seventy-three to twenty-five, with six more posts expected to be eliminated in the coming years. Meanwhile, Schulz wrote, “In the Army . . . only forty-six per cent of those soldiers who require an annual hearing evaluation—because they are exposed to hazardous noise as a part of their routine duties—received one last year.”
The military has attempted to make hearing protection more widely available. The combat-arms earplug currently in use was originally developed in France, in the late nineteen-nineties, and contains a unique acoustic filter that is about the size of a grain of rice. The filter creates acoustic friction to capture potentially harmful sound waves and turn them around, so that the noise doesn’t send signals into the ear canal. Schulz described it as low-end, explaining, “It’s basically just a fairly traditional earplug that has a filter in it, that allows through most of the sounds that you would normally hear,” while blocking sharper noises, like gunfire. A more sophisticated device, called QuietPro, is a lightweight digital tactical-communication headset with high-level hearing protection. Continuous low-frequency rumbling noises above eighty-five decibels, such as those produced by helicopters and armored vehicles, are attenuated by more than thirty decibels. Outer microphones amplify surrounding sound, but very loud impact noises from I.E.D.s are instantly blocked by a digital processor; normal amplification is restored immediately after the impact sound has passed. “It’s essentially a hearing aid and a hearing protector in one,” Schulz said. “It’s a device that allows you to turn up the sound so that you can hear what’s on the other side of a door, what’s around the corner. . . . It basically shuts down and protects you during the blast and then comes back on so that you can hear what’s going on after the blast.” The Marines have adopted the QuietPro, but the Army and the Air Force, Schulz said, are taking a “wait-and-see approach,” particularly since each QuietPro unit costs about a thousand dollars. But, Schulz noted, hearing loss and tinnitus can prevent soldiers from being redeployed and qualifies as a disability. “It’s one of those pay-me-now, pay-me-later” situations, Schulz said. “Pay-me-now is really less.”
Colonel Kathy Gates, the director of the Army Audiology and Speech Center in Washington, D.C., serves as the audiology consultant to the Army Surgeon General, working to redesign the hearing program in that branch of the service. In 2004, Gates instituted an annual surveillance hearing test for soldiers about to be deployed, and last year mandated a similar evaluation of those returning from service. All soldiers must now be instructed in the use of the combat-arms earplugs. Gates has helped develop a strategy for persuading Army personnel to wear the earplugs in combat by linking their use to success in battle rather than to long-term health. “A soldier with hearing loss is impaired in battle,” Gates said. “We are linking hearing not to quality of life per se but to survivability and completion of the mission.” Gates said that QuietPro is being field-tested in Iraq and Afghanistan, and that the Army had increased the number of positions for audiologists in the battle theatre and in regional hospitals in Iraq. Even so, recruitment was slow, and the military is not yet fully staffed despite the restoration of funding for the hearing program.
The efforts to provide proper training and equipment have had some success. Specialist Joseph McLosky, who is twenty-four, is a member of the military-police reserve; in September, 2006, his unit was sent to Fort Dix to prepare for urban combat, and he was issued the newly requisitioned combat-arms earplugs. Two-sided and color-coded (the green side for use when actively shooting—on a range, for instance—and the yellow side for missions), the earplugs, McLosky said, were to be used in addition to the radio headsets that soldiers wear in convoys. “A lot of guys thought it was ridiculous to use both,” he told me, when we spoke in September.
In December, 2006, McLosky was deployed to the city of Bayji, between Baghdad and Mosul, in the north of the country, to train Iraqi police recruits in the use of firearms, surveillance missions, and the pursuit of insurgents. “We went from police station to police station along the same roads, spending eight to sixteen hours a day in the convoy,” he said. They encountered about one I.E.D. a week. In June, 2007, his squad was passing a checkpoint when a car bomb exploded. “Dirt and smoke and debris were flying past my head,” he went on. “We had been up all night, and I thought I was dreaming.” Although he was only a few yards away from the explosion, McLosky said, “My ears weren’t ringing.” In October, an I.E.D. detonated underneath McLosky’s truck. “I was ejected from the vehicle,” he said. “It broke my pelvis, left leg, and ankle. I had to have my left foot amputated.” Despite the severity of his injuries, McLosky emerged with his hearing intact; he now plans to become a physical therapist. Throughout his deployment, McLosky told me, it had been easy to tell which soldiers weren’t wearing their earplugs. “They were the ones saying, ‘What? What?’ ”
Tinnitus patients desperate for relief sometimes turn to folk remedies. Christina Stocking routinely hears of patients using herbal supplements like ginkgo biloba or high doses of Vitamin B, neither of which has been proved effective in large controlled studies. Antioxidants are commonly recommended—because the aging process is believed to be related in part to oxidized damage to tissues, including the auditory nerve—although no practical benefit has been documented. Some of the more extreme approaches that Stocking has encountered include the neti pot, a device that resembles a teapot with a long spout; the device is filled with warm salt water and used to irrigate the nasal passages. “You get yourself into a position to pour up one nostril, and it gets up to your sinus and drains out the other side,” Stocking explained. Another is “ear candling,” she told me. “People actually take wax paper, roll it up, stick one end into the ear canal, and light the other end.”
Stocking trained under Pawel Jastreboff, now a professor at Emory University, who developed a treatment plan called tinnitus retraining therapy. It combines counselling, to reduce the anxiety caused by the phantom sounds, with sound therapy, using a neutral background noise. Stocking first determined the decibel level of my tinnitus, then transmitted a noise similar to rushing water to both ears through headphones. For the first time in a year, I couldn’t hear the dental drill even when I tried.
The device currently approved by the F.D.A. for tinnitus treatment, produced by a company called Neuromonics, resembles an MP3 player. I put the earbuds in and listened to a soothing piece of classical music. “That is meant to induce relaxation,” Stocking explained, a key component of the tinnitus management strategy. Then I noticed a soft white noise that was programmed to mask my own tinnitus. Again, within moments, the tinnitus was gone. The theory, elaborated by Jastreboff, is that when more sounds are fed to the brain sensitivity and spontaneous activity decline—the effect Hippocrates remarked upon.
A simple hearing aid may reduce some tinnitus by amplifying background noises, but other strategies include using sounds in the environment, like soft background music from a stereo or more directed sounds that come from a fan or a small desktop sound machine. Similarly, a device called a sound generator, which is worn on the ear, can supply a white noise that partially interferes with the tinnitus. “It really provides a sense of relief and control over the tinnitus,” Stocking said. “Patients feel they are able to do something about it. And, by providing additional sound, it seems to bring down the sensitivity of the auditory system.”
Recently, I met with Dr. David Vernick, an ear-nose-and-throat specialist at my hospital, Beth Israel Deaconess. He reviewed the tests done in Buffalo and concurred that I needed hearing aids. “They will certainly help you with what you are missing now,” he said. “It’s hard to know how much benefit you will get with regard to your tinnitus.” He added that hearing aids often act simply as a placebo.
Ann Stockwell, an audiologist in Vernick’s office, entered the data from my audiogram into a computer, then used earbuds to transmit sounds generated by the computer—in essence, programming the hearing aids. I listened to a range of tones, which Stockwell compared with the data provided by the audiogram. Once the hearing aids were fitted, she asked me to turn my back. From about sixteen feet away, she spoke in a normal voice that I heard with no difficulty. “The aids will amplify background sounds, like the noise from the refrigerator or a heater,” she said. “Initially, there will be increased sensory awareness, and then you will adapt. I like to say that we are entering the auditory closet and throwing out what the brain can’t hear. We will fill the closet with a new set of sounds. And, hopefully, your brain will change so that there is less tinnitus.”
The hearing aids aren’t a cure: in a quiet room, my tinnitus is as persistent as ever. But when I returned to my office, with the hearing aids in place, I could hear the noise of the air vents, which previously had been inaudible. I tried to catch the high-pitched drone that has accompanied me in the past year. I couldn’t hear it. ♦
The Epley Maneuvers
Start sitting on a bed and turn your head 45° to the right. Place a pillow behind you so that on lying back it will be under your shoulders.
Lie back quickly with shoulders on the pillow and head reclined onto the bed. Wait for 30 seconds.
Turn your head 90° to the left (without raising it) and wait again for 30 seconds.
Turn your body and head another 90° to the left and wait for another 30 seconds.
Sit up on the left side.
This maneuver should be carried out three times a day. Repeat this daily until you are free from positional vertigo for 24 hours
Turn Off the Ringing Sound
Researchers Explore New Treatments to Silence the Persistent Din of Tinnitus
Melinda Beck : WSJ Article : December 14, 2010
Some people hear a high-pitched buzzing sound. Others describe it as a ringing, roaring, hissing, chirping, whooshing or wheezing. It can be high or low, single or multi-toned, an occasional mild annoyance or a constant personal din. Tinnitus—whose Latin root means "to jingle"—is defined as the perception of sound when no external sound is present. It usually accompanies hearing loss, and while no one knows for sure what causes it, many experts believe that when people lose the ability to hear in certain frequencies, the brain fills the void with imaginary or remembered noise—like phantom limb pain for sound.
"Those auditory centers are just craving input," says Rebecca Price, an audiologist who treats tinnitus at Duke University Health Systems in Durham, N.C.
Some 50 million Americans at least occasionally experience tinnitus, pronounced tin-EYE-tus or TIN-i-tus. And 16 million U.S. adults had it frequently in the past year, according to a new study by the Centers for Disease Control and Prevention. Some two million find it so disturbing that it interferes with sleep, work, concentration and family relationships.
The incidence is rising these days along with the aging population and personal music players cranked up high. "Now we have 12-year-olds complaining of tinnitus. We never had that previously," says Jennifer Born, a spokeswoman for the American Tinnitus Association, a nonprofit education and advocacy group.
Tinnitus is also the No. 1 service-related disability among veterans from Afghanistan and Iraq, due to brain injuries from explosive devices.
While many sufferers are told there is no cure for their tinnitus, treatment options are proliferating. And brain-imaging studies are shedding new light on how some peoples' brains are wired with unusual connections between the auditory cortex that governs hearing and the centers for attention, emotion and executive function.
"We have always wondered why some people find tinnitus so distressing. Now we can see it," says Jay Piccirillo, an otolaryngologist at Washington University in St. Louis who is studying a new treatment for tinnitus that targets magnetic pulses at patients' brains to redirect abnormal connections.
The first step in treating tinnitus is usually to determine if a patient has hearing loss and to identify the cause, which can run the gamut from ear-wax buildup to infections, accidents, aging, medication side effects and noise exposure.
"At least half of the time, if we can reduce the hearing loss, we can dramatically reduce the tinnitus or make it so that the patient doesn't care," says Sujana Chandrasekhar, an otolaryngologist in New York and chairman-elect of the American Academy of Otolaryngology-Head and Neck Surgery.
Surgery may be helpful in some cases. Frank Scalera, a 42-year-old pipefitter in New York, had tinnitus ever since a firecracker blew out his eardrum at age 15. Ten surgeries have helped restore his hearing and reduce the ringing he's heard for 30 years.
About 40% of tinnitus sufferers find relief with a regular hearing aid that restores sound in lost frequencies, so the brain doesn't need to fill in the void. But some also have hyperacusis—in which normal sounds seem unbearably loud—so a hearing aid may be uncomfortable.
A variety of tinnitus treatments use sound therapy—soothing external sounds to drown out the ringing from within. Some people find relief by running a fan, a humidifier, a machine that mimics waves or waterfalls or even a radio tuned to static, especially at night when tinnitus is often most noticeable and frequently disrupts sleep.
Several brands of hearing aids also mix in soft "shhhsssing" tones to mask tinnitus sounds and help users relax. As with other hearing aids, they are rarely covered by insurance and can cost $2,500 or more per ear.
Another variation is the Oasis device by Neuromonics Inc., which looks like an MP3 player but plays baroque and new age music customized to provide more auditory stimulation in patients' lost frequencies as well as a "shower" sound to relieve the tinnitus. Users listen to the program for two hours daily for two months, then the shower sound is withdrawn for four more months of treatment, gradually training the brain to filter out the internal noise, according to the company.
"You get used to hearing the music and then your brain fills in with sounds that aren't as irritating," explains Michael Gillespie, a Duke University political science professor who found the device helpful after an ear infection left him with tinnitus.
Dr. Price says she has used Neuromonics treatment with 30 patients, and 90% have had at least a partial reduction in their tinnitus awareness, similar to the company's published data.
Cleared by the Food and Drug Administration in 2005, the Neuromonics device has been used by 4,500 patients in the U.S., Australia, New Zealand and Singapore. The cost—roughly $4,500—is rarely covered by insurance.
For some patients, it's not the noise itself that's so distressing, but the anxiety that comes along with it. Researchers long theorized—and have now seen on brain scans—that the limbic system, the brain's primitive fight-or-flight response, is highly activated in some tinnitus sufferers. Patients often have generalized anxiety disorder or depression and a few become suicidal; but it's unclear which came first.
Some patients find that antidepressants or anti-anxiety drugs can bring some tinnitus relief. Many find their tinnitus is worse during times of stress, so yoga, acupuncture, deep breathing, biofeedback or exercise—may also be helpful.
Ginkgo, zinc, magnesium and other supplements are often marketed for tinnitus relief, along with a bevy of over-the-counter products, but few have been evaluated scientifically. "There are a lot of people out there trying to capitalize on the desperation of tinnitus patients," Ms. Born says.
The new magnetic pulse treatment—called repetitive Transcranial Magnetic Stimulation (rTMS)—seeks to break the tinnitus cycle in a different way. Researchers first conduct scans of patients' brains. In people with severe tinnitus, "We notice that communication between parts of the brain responsible for hearing and maintaining attention are abnormal," says Dr. Piccirillo. A magnetic coil placed over auditory cortex outside the head sends pulses through the skull and attempts to disrupt the faulty communications. Dr. Piccirillo likens it to shaking an Etch-a-Sketch to erase an old picture. "We hypothesize that given half a chance, the brain can establish more normal connections," he says.
RTMS has been used for years with severely depressed patients, some of whom found that it also stopped the ringing in their ears. To patients, it feels like a mild tapping on the head and brings no harmful effects. One early study found that it had little benefit either compared to a placebo when used for 40 minutes, five times a week for two weeks. Dr. Piccirillo and colleagues are now studying whether using four-week rTMS sessions and higher energy is more effective. With a Defense Department grant, they are also scanning the brains of U.S. solders before and after deployment to see if those who develop tinnitus had unusual brain wiring that made them especially vulnerable.
One of the most effective treatments is cognitive behavioral therapy, which treats patients' emotional reactions to tinnitus, not the noise itself. "The goal is to make your tinnitus like your socks and shoes—you're wearing them, but you're not actively thinking about them," says Dr. Chandrasekhar.
Michelle Pearce, a psychologist at Duke University Medical Center, says she starts by getting patients to identify the automatic negative thoughts they have about their tinnitus. "Some patients say things like, 'My life is over now.' I had one who was convinced no one would want to marry her because of her tinnitus," says Dr. Pearce. "Our work together was to realize that her life didn't resolve around tinnitus; it was just part of her life."
Indeed, some patients say learning to ignore the sound in their head is ultimately the most effective thing to do.
"It's like living near an airport. After you've lived there for awhile, you don't pay attention to the planes," says Mark Church, an entrepreneur and investor who has tried multiple treatments for tinnitus that started 11 years ago. Still, he says, his favorite place is his shower, where he can't hear it at all.
Researchers Explore New Treatments to Silence the Persistent Din of Tinnitus
Melinda Beck : WSJ Article : December 14, 2010
Some people hear a high-pitched buzzing sound. Others describe it as a ringing, roaring, hissing, chirping, whooshing or wheezing. It can be high or low, single or multi-toned, an occasional mild annoyance or a constant personal din. Tinnitus—whose Latin root means "to jingle"—is defined as the perception of sound when no external sound is present. It usually accompanies hearing loss, and while no one knows for sure what causes it, many experts believe that when people lose the ability to hear in certain frequencies, the brain fills the void with imaginary or remembered noise—like phantom limb pain for sound.
"Those auditory centers are just craving input," says Rebecca Price, an audiologist who treats tinnitus at Duke University Health Systems in Durham, N.C.
Some 50 million Americans at least occasionally experience tinnitus, pronounced tin-EYE-tus or TIN-i-tus. And 16 million U.S. adults had it frequently in the past year, according to a new study by the Centers for Disease Control and Prevention. Some two million find it so disturbing that it interferes with sleep, work, concentration and family relationships.
The incidence is rising these days along with the aging population and personal music players cranked up high. "Now we have 12-year-olds complaining of tinnitus. We never had that previously," says Jennifer Born, a spokeswoman for the American Tinnitus Association, a nonprofit education and advocacy group.
Tinnitus is also the No. 1 service-related disability among veterans from Afghanistan and Iraq, due to brain injuries from explosive devices.
While many sufferers are told there is no cure for their tinnitus, treatment options are proliferating. And brain-imaging studies are shedding new light on how some peoples' brains are wired with unusual connections between the auditory cortex that governs hearing and the centers for attention, emotion and executive function.
"We have always wondered why some people find tinnitus so distressing. Now we can see it," says Jay Piccirillo, an otolaryngologist at Washington University in St. Louis who is studying a new treatment for tinnitus that targets magnetic pulses at patients' brains to redirect abnormal connections.
The first step in treating tinnitus is usually to determine if a patient has hearing loss and to identify the cause, which can run the gamut from ear-wax buildup to infections, accidents, aging, medication side effects and noise exposure.
"At least half of the time, if we can reduce the hearing loss, we can dramatically reduce the tinnitus or make it so that the patient doesn't care," says Sujana Chandrasekhar, an otolaryngologist in New York and chairman-elect of the American Academy of Otolaryngology-Head and Neck Surgery.
Surgery may be helpful in some cases. Frank Scalera, a 42-year-old pipefitter in New York, had tinnitus ever since a firecracker blew out his eardrum at age 15. Ten surgeries have helped restore his hearing and reduce the ringing he's heard for 30 years.
About 40% of tinnitus sufferers find relief with a regular hearing aid that restores sound in lost frequencies, so the brain doesn't need to fill in the void. But some also have hyperacusis—in which normal sounds seem unbearably loud—so a hearing aid may be uncomfortable.
A variety of tinnitus treatments use sound therapy—soothing external sounds to drown out the ringing from within. Some people find relief by running a fan, a humidifier, a machine that mimics waves or waterfalls or even a radio tuned to static, especially at night when tinnitus is often most noticeable and frequently disrupts sleep.
Several brands of hearing aids also mix in soft "shhhsssing" tones to mask tinnitus sounds and help users relax. As with other hearing aids, they are rarely covered by insurance and can cost $2,500 or more per ear.
Another variation is the Oasis device by Neuromonics Inc., which looks like an MP3 player but plays baroque and new age music customized to provide more auditory stimulation in patients' lost frequencies as well as a "shower" sound to relieve the tinnitus. Users listen to the program for two hours daily for two months, then the shower sound is withdrawn for four more months of treatment, gradually training the brain to filter out the internal noise, according to the company.
"You get used to hearing the music and then your brain fills in with sounds that aren't as irritating," explains Michael Gillespie, a Duke University political science professor who found the device helpful after an ear infection left him with tinnitus.
Dr. Price says she has used Neuromonics treatment with 30 patients, and 90% have had at least a partial reduction in their tinnitus awareness, similar to the company's published data.
Cleared by the Food and Drug Administration in 2005, the Neuromonics device has been used by 4,500 patients in the U.S., Australia, New Zealand and Singapore. The cost—roughly $4,500—is rarely covered by insurance.
For some patients, it's not the noise itself that's so distressing, but the anxiety that comes along with it. Researchers long theorized—and have now seen on brain scans—that the limbic system, the brain's primitive fight-or-flight response, is highly activated in some tinnitus sufferers. Patients often have generalized anxiety disorder or depression and a few become suicidal; but it's unclear which came first.
Some patients find that antidepressants or anti-anxiety drugs can bring some tinnitus relief. Many find their tinnitus is worse during times of stress, so yoga, acupuncture, deep breathing, biofeedback or exercise—may also be helpful.
Ginkgo, zinc, magnesium and other supplements are often marketed for tinnitus relief, along with a bevy of over-the-counter products, but few have been evaluated scientifically. "There are a lot of people out there trying to capitalize on the desperation of tinnitus patients," Ms. Born says.
The new magnetic pulse treatment—called repetitive Transcranial Magnetic Stimulation (rTMS)—seeks to break the tinnitus cycle in a different way. Researchers first conduct scans of patients' brains. In people with severe tinnitus, "We notice that communication between parts of the brain responsible for hearing and maintaining attention are abnormal," says Dr. Piccirillo. A magnetic coil placed over auditory cortex outside the head sends pulses through the skull and attempts to disrupt the faulty communications. Dr. Piccirillo likens it to shaking an Etch-a-Sketch to erase an old picture. "We hypothesize that given half a chance, the brain can establish more normal connections," he says.
RTMS has been used for years with severely depressed patients, some of whom found that it also stopped the ringing in their ears. To patients, it feels like a mild tapping on the head and brings no harmful effects. One early study found that it had little benefit either compared to a placebo when used for 40 minutes, five times a week for two weeks. Dr. Piccirillo and colleagues are now studying whether using four-week rTMS sessions and higher energy is more effective. With a Defense Department grant, they are also scanning the brains of U.S. solders before and after deployment to see if those who develop tinnitus had unusual brain wiring that made them especially vulnerable.
One of the most effective treatments is cognitive behavioral therapy, which treats patients' emotional reactions to tinnitus, not the noise itself. "The goal is to make your tinnitus like your socks and shoes—you're wearing them, but you're not actively thinking about them," says Dr. Chandrasekhar.
Michelle Pearce, a psychologist at Duke University Medical Center, says she starts by getting patients to identify the automatic negative thoughts they have about their tinnitus. "Some patients say things like, 'My life is over now.' I had one who was convinced no one would want to marry her because of her tinnitus," says Dr. Pearce. "Our work together was to realize that her life didn't resolve around tinnitus; it was just part of her life."
Indeed, some patients say learning to ignore the sound in their head is ultimately the most effective thing to do.
"It's like living near an airport. After you've lived there for awhile, you don't pay attention to the planes," says Mark Church, an entrepreneur and investor who has tried multiple treatments for tinnitus that started 11 years ago. Still, he says, his favorite place is his shower, where he can't hear it at all.
What Causes Hearing Loss
By Jane E. Brody : NY Times : March 25, 2013
Noise, not age is the leading cause of hearing loss. Unless you take steps now to protect to your ears, sooner or later many of you — and your children — will have difficulty understanding even ordinary speech.
Tens of millions of Americans, including 12 percent to 15 percent of school-age children, already have permanent hearing loss caused by the everyday noise that we take for granted as a fact of life.
“The sad truth is that many of us are responsible for our own hearing loss,” writes Katherine Bouton in her new book, “Shouting Won’t Help: Why I — and 50 Million Other Americans — Can’t Hear You.” The cause, she explains, is “the noise we blithely subject ourselves to day after day.”
While there are myriad regulations to protect people who work in noisy environments, there are relatively few governing repeated exposure to noise outside the workplace, from portable music devices, rock concerts, hair dryers, sirens, lawn mowers, leaf blowers, vacuum cleaners, car alarms and countless other sources.
We live in a noisy world, and every year it seems to get noisier. Ms. Bouton notes that the noise level inside Allen Fieldhouse at the University of Kansas often exceeds that of a chain saw.
After poor service, noise is the second leading complaint about restaurants. Proprietors believe that people spend more on food and drink in bustling eateries, and many have created new venues or retrofitted old ones to maximize sound levels.
When I’m told about a new restaurant, my first question is, “Is it noisy?” My friends and I will never return to one in which the racket makes it impossible to converse with tablemates. Perhaps the young diners the restaurateurs covet “talk” by texting.
The ears are fragile instruments. When sound waves enter the ear, they cause the eardrum to vibrate. The vibrations are transmitted to the cochlea, in the inner ear, where fluid carries them to neatly organized rows of hair cells. These in turn stimulate auditory nerve fibers, each attuned to a different frequency. These impulses travel via the auditory nerve to the brain, where they are interpreted as, say, words, music or an approaching vehicle.
Damage to this delicate apparatus results from both volume and length of exposure to sound. Very loud noises, or chronic exposure to sound even when it is not particularly loud, can wreak havoc on hair cells, causing them to become disarranged and to degenerate.
We are born with a fixed number of hair cells; once they are dead, they cannot be replaced, and auditory sensitivity is permanently lost. Usually, sensitivity to high-frequency sounds is first to go, followed by an inability to hear the frequencies of speech.
Furthermore, the effects of noise exposure are cumulative, as Robert V. Harrison, an auditory specialist at the University of Toronto, noted recently in the International Journal of Pediatrics. Although we start out with a redundancy of hair cells, with repeated noisy insults, enough are destroyed to impair hearing. Thus, damage to hair cells incurred early in life, as has happened to many rock musicians and rock concert aficionados, can show up in midlife as difficulty understanding speech.
Sound volume is measured in decibels (dB), and the level at which noise can cause permanent hearing loss begins at about 85 dB, typical of a hair dryer, food processor or kitchen blender.
Dr. Michael D. Seidman, the director of otolaryngology at Henry Ford West Bloomfield Hospital in Michigan, told me to use ear plugs when I dry my hair or mow my lawn with a gas-powered mower, and to cover my ears when an emergency vehicle passes with siren blasting. Ear protection is a must for people who shoot guns as well as those who ride motorcycles or use snow blowers, leaf blowers, hand or pneumatic drills or chain saws.
But even noisier than many of these is the maximum output of some portable music players, which can exceed occupational safety levels and produce sound levels in the ear on a par with that of a jet taking off. If you listen to music with earbuds or headphones at levels that block out normal discourse, you are in effect dealing lethal blows to the hair cells in your ears, Dr. Seidman said.
A national study in 2006 by the American Speech-Language-Hearing Association found that among users of portable music devices, 35 percent of adults and up to 59 percent of teenagers reported listening at loud volumes.
Dr. Harrison urges purchasers of such “personal entertainment devices” to read and heed the warnings and practical advice on package inserts. Too often people turn up the volume to overcome surrounding noise. A better plan is to set a maximum volume while in a quiet environment and never go above that.
In general, if other people can hear what you’re listening to, the volume is turned up too high. Many times I’ve had to change my seat on the subway or bus because the rider next to me was using a music player as if it were a boombox.
Some portable listening devices come with the ability to set a maximum volume, which may be worth the added cost to parents concerned about protecting their children’s ears.
At a given volume level, earbuds deliver higher noise levels than over-the-ear headphones. If earbuds are used, Dr. Harrison suggests selecting ones that fit loosely and never inserting them tightly into the ear canal. Alternatively, when you are alone and not at risk of missing important environmental cues, like an approaching vehicle, consider using noise-canceling over-the-ear headphones that block out background noise and enable you to listen at a lower volume.
Even toys meant for young children can generate ear-damaging levels of noise. The American Speech-Language-Hearing Association lists as potential hazards cap guns, talking dolls, vehicles with horns and sirens, walkie-talkies, rubber squeaky toys, musical instruments and toys with cranks. According to the association, some toy sirens and squeaky rubber toys can emit sounds of 90 decibels, as loud as a lawn mower.
It suggests that parents with normal hearing test new toys before giving them to a child. “If the toy sounds loud, don’t buy it,” is the recommendation. For noisy toys already bought, consider removing the batteries or taping over the speaker.
What Should Be Done About Hearing Loss?
By NY Times Article : February 27, 2013
Judging purely by the responses to Ask an Expert, hearing problems are an enormous concern for baby boomers, rivaled only by worries about memory. More than 200 people wroteto this week’s expert on hearing, Neil J. DiSarno. Dr. DiSarno is chief staff officer for audiology at the American Speech-Language-Hearing Association, and from 1998 to 2012 was chairman of the department of communication sciences and disorders at Missouri State University.
Dr. DiSarno’s first set of answers follows.
As is quite evident from the number of comments readers sent in, hearing loss affects large numbers of baby boomers. Although I would like to have the time to answer each question individually, that is not possible. Those of you who have read the comments, however, see that they fall pretty neatly into seven or eight categories. I will address the questions by topic area.
First I would like to point out that although the effects of hearing loss differ as a result of type and degree of impairment, one important aspect to be mindful of is that the use of hearing aids is only part of a plan of treatment. Although it is a prime component, amplification in the form of hearing aids only brings sounds closer to the individual. How the individual’s auditory system processes that information differs considerably among those with impaired hearing. This is one reason some individuals benefit greatly from the use of hearing aids and others somewhat less.
The treatment following the fitting of hearing aids includes extensive counseling that is tailored to the degree of impairment as well as the lifestyle of the individual user. Hearing aid users must establish realistic expectations with regard to the benefit they can expect. Although hearing aids have become more technologically advanced in recent years, it must be kept in mind that the auditory system is the most complex organ in the human body. When it becomes altered, either through the process of normal aging, or other health-related factors, it can leave the individual with limitations ranging from an inability to hear soft speech which is easily addressed by hearing aids, to complete inability to understand any speech information, even when using very powerful hearing aids.
Another factor to consider is the change that occurs in how the brain processes speech. Consider this example. A twenty-something and a sixty-something both have their hearing checked and learn that hearing is within normal limits. Each individual receives a cellphone call while dining in a very noisy restaurant. If you are me, you are amazed that the twenty-something appears to have no difficulty at all understanding the conversation. The sixty-something on the other hand can barely understand who they are speaking with, much less what is being said. Remember, each had quite good hearing on a hearing test.
The brain’s ability to understand speech in background noise undergoes changes and this imposes limitations on how the aging auditory system processes speech under those circumstances. Now, add a bit of hearing loss or a foreign accent to the cell phone situation and you can imagine, or probably already live with that frustration. Help can be found for many of the limitations impaired hearing imposes on an individual; however, appropriate counseling and realistic expectations are key to successful rehabilitation.
Please understand that any advice in this section is provided without the benefit of seeing you as a patient. It is only with the knowledge of a complete medical history and a thorough audiological evaluation that accurate information can be provided. Please allow this to serve as a stepping-off point to allow you to research your condition further and to seek professional consultation.
BACKGROUND NOISE
Q. After thorough testing, the Mayo Clinic told me that I had a slight hearing loss, but my difficulty separating sounds (as in a noisy restaurant) is caused by a brain function that can’t be alleviated by audiology modifications. What is the name of this disability, and are people being sold hearing aids that can’t deal with it very successfully? — George B., Creve Coeur, Mo.
Q. I only have hearing problems in certain situations, e.g., at movies, crowded restaurants. If I got a hearing aid, would there be any problem wearing it in just those situations? — John Fisher, Winston-Salem, N.C.
A. Without seeing audiological test results from either George B. or John Fisher it is difficult to provide consultation as to whether hearing aids would help. An important fact to keep in mind is that most hearing loss occurs in the high-frequency range. This is the part of the hearing organ that typically produces awareness of sounds such as “s”, “f”, “th”, “p”, and “t”. An inability to hear these consonant sounds can cause considerable confusion when listening to speech. When listening in the presence of background noise, the damaged high-frequency portion of your hearing organ cannot provide you with accurate high-frequency speech information. You may easily confuse the word shoot with shoe, or hit with hip. Your inability to hear these high-frequency consonant sounds can certainly send your brain an inaccurate message.
The fortunate part of this condition is that these high-frequency sounds are some of the most visible sounds on a person’s lips. So, if you are able to see the speaker’s face, your brain can often fill in what your ears may have misunderstood. Positioning yourself in restaurants, at family dinners, or group settings where you are able to see the speaker’s face can improve your ability to follow conversation.
Can hearing aids help as well? A properly fit hearing aid may boost up the damaged region of your hearing, in most cases this is the high-frequency portion. Depending on the degree of the damage, the boosted high-frequency sounds can fill in where your damaged hearing organ is lacking. The extent of the benefit you may receive is dependent upon several factors. Certainly you must give your brain a chance to get used to utilizing this new amplified information. A trial period of at least one month of consistent hearing aid use often times will provide you with the answer.
TINNITUS
Q. I’ve had tinnitus on my left ear since August 2011 but it was not annoying at first. Hearing tests show mild to moderate hearing loss on my left ear; however, for some inexplicable reason my tinnitus got very loud in October 2012. I suspect it was emotional stress. I have tried many things to lessen the sound and its effects on my mood and reaction including a hearing aid but nothing seems to help. I am only 25 and the hissing continues. The sound is destroying my life day by day! It is not life anymore it is torture. Can you please recommend something a college student like me can do to improve this unfortunate situation? And do you have any further knowledge on acoustic neuromodulation treatment offered in the U.K.? Thank you. — Henry, Sacramento
Q. Following surgery to repair a ruptured eardrum about five years ago, I experienced a catastrophic loss of high-frequency hearing in one ear. I wear a hearing aid in that ear and can get by except in the presence of high background noise (cocktail party effect). However, I’ve never completely adjusted to the tinnitus, which is not only intrusive and distracting but wakes me up at night. What are the latest developments in overcoming tinnitus? And is there anything on the horizon as far as hair cell regeneration? — Liza, Connecticut
Tinnitus refers to “ringing in the ears” or “head noises” when no other sound is present. Tinnitus can sound like hissing, roaring, pulsing, whooshing, chirping, whistling or clicking. Tinnitus can occur in one ear or both ears. It is a symptom common to many problems. While the exact cause of tinnitus is unknown, it may be a symptom of other problems like hearing loss, exposure to loud noise, ototoxic medications, allergies or even too much wax in the ear canal. If you have tinnitus, chances are the cause will remain a mystery. The American Speech-Language-Hearing Association has more about commonly asked questions about tinnitus.
Both Henry and Liza as well as many others who have written are experiencing the effects of tinnitus to the point where it is disruptive to their lives, and both asked about the latest treatments. An advocacy group for tinnitus suffers is the American Tinnitus Association, and this link provides information about the latest research on tinnitus treatment, including neuromodulation treatment. With regard to hair cell regeneration to replenish the damaged sensory hair cells, a critical component to the hearing process, the National Institutes of Healthprovides information regarding recent advances in this area. Successes dealing with hair cell regeneration have so far been limited to animal studies. Some facts regarding tinnitus are:
¶One-third of all adults report experiencing tinnitus at some time in their lives. Ten to 15 percent of adults have prolonged tinnitus requiring medical/audiologic evaluation.
¶Up to 18 percent of the general population of industrialized countries is mildly affected by chronic tinnitus, and 0.5 percent report tinnitus having a severe effect on the ability to lead a normal life.
Tinnitus and hearing loss often go hand in hand. Contact an audiologist to find out if your tinnitus symptoms also include hearing loss. For a provider check here. If you have hearing loss as well as tinnitus, in some cases hearing aids can help.
Q. What is the latest research on tinnitus and treatments/cure? Congress is looking at this issue because so many of our returning military have tinnitus so hopefully that will mean more research dollars to benefit them as well as the rest of us who have tinnitus. — Anne Royal Oak, MI
A. New brain imaging techniques have led to insights about the connections between structures and function within the ear and in the cognitive process of the brain. These new imaging techniques suggest the possibility of more effective treatments for tinnitus and hyperacusis (oversensitivity to normal sounds; see question below). Imaging advances will also increase the knowledge about the plasticity of the brain and its ability to compensate for hearing dysfunction.
Q. Following surgery to repair a ruptured eardrum about five years ago, I experienced a catastrophic loss of high-frequency hearing in one ear (complicated story). I wear a hearing aid in that ear and can get by except in the presence of high background noise (cocktail party effect). However, I’ve never completely adjusted to the tinnitus, which is not only intrusive and distracting but wakes me up at night. What are the latest developments in overcoming tinnitus? And is there anything on the horizon as far as hair cell regeneration? – Liza, Connecticut
A. One area of exciting research involves inner ear hair cell regeneration with the use of stem cells. The discovery of both adult and embryonic stem cells in the inner ear and scientific evidence that they can be converted into hair cells raises hope for the development of stem-cell based treatments to regrow damaged hair cells.
Researchers are studying precisely how hearing may have been damaged from exposure to loud noise or ear-damaging medications, known as ototoxic medications. This research is looking at the biology of the ear structures and chemistry to understand the role of free radicals, highly reactive molecules in the body. Free radicals are a result of stress (oxidation) on the inner ear tissues and can lead to cell death. Several pharmaceutical interventions based on natural and synthetic antioxidants are being studied.
AGE-RELATED HEARING LOSS
Q. I am 63 years old. I blame my “hearing loss” on cell phones and poor audio quality of DVDs and inconsiderate people who talk from distant rooms, but my wife is not buying it. I can hear fine if someone speaks to me face to face, but . . . Is it me? — John, Memphis
Q. After thorough testing, Mayo Clinic told me I had slight hearing loss, but my difficulty separating sounds (as in a noisy restaurant) is caused by a brain function that can’t be alleviated by audiology modifications. What is the name of this disability, and are people being sold hearing “aids” that can’t deal with it very successfully? — George B., Creve Coeur, Missouri
A. Age-related hearing loss, or presbycusis, is increasing as the baby-boom generation grows older. Scientists are still trying to determine whether the age-related deficit is mostly due to loss of sensitivity in the inner ear. Increasingly, research suggests that other areas within the hearing system may be affected. For example, it has been found that the brain processes sound less quickly with advancing age. This suggests that a major contributor to poor speech understanding in older people is poor processing of sound in the brain. Thus, simple hearing aid strategies that only address damage in the inner ear by amplifying sound may not solve the communication problems often expressed by older hearing aid users.
An emerging area of research is looking at a link between noise exposure and the degree and rate of development of presbycusis. What we know now is that exposure to loud levels of noise over time will increase the ear’s vulnerability to the aging process.
PAINFULLY LOUD SOUNDS
Q. Would like to learn more about “recruitment.” Although I have a moderate to severe hearing loss, I notice that sounds that others can tolerate are painfully loud to me. This seem paradoxical; can you explain to me how and why this happens? — Jerry M., Little Rock, Ark.
Q. What is the latest information on helping people who have tinnitus and hyperacusis caused by having a bad case of the flu or a virus. This happened to me in 1991 and actually the hyperacusis is harder to deal with than the tinnitus, which never stops hissing and screaming. Have you seen any success with acupuncture treatment? — Chadds Ford, Pa.
A. Recruitment is a condition sometimes observed in people with known damage to the hair cells of the inner ear and/or the damaged auditory nerve cells to which they are connected. Although it seems paradoxical, consider this situation. An individual without hearing loss has a tone presented to one ear just barely above the level he can hear (his hearing threshold) and he responds that yes, he hears a very soft tone. An individual with impaired hearing is also presented with a tone that is just above his threshold of impaired hearing and he reports that yes, he hears a very soft tone. The level of the tone is brought up the same amount (e.g., 20 dB additional) for the normal hearing individual and he reports that the tone is a little louder. The same additional 20 dB of loudness is presented to the individual with impaired hearing and he reports that the new tone is much louder than the original tone and may be approaching a painfully loud level. The impaired ear is experiencing an abnormal growth of loudness. Recruitment is defined as an abnormal perception of loudness and is seen in some people with sensory and/or neural hearing loss.
Hyperacusis is a rare hearing disorder that causes sounds which would otherwise seem normal to most people to sound unbearably loud. People who suffer from hyperacusis may even find normal environmental sounds to be too loud. Hyperacusis is not discomfort around loud sounds. Individuals with hyperacusis may find a car engine, dishes clanking, rustling of paper or even loud conversation uncomfortable enough to avoid such situations.
Many people with hyperacusis have normal hearing. The disorder can occur in one or both ears and is often accompanied by tinnitus (ringing or buzzing in the ear). It is reported that 1 in 50,000 people has hyperacusis and that 1 in 1,000 people who have tinnitus will also have hyperacusis.
There are some diseases or disorders that are linked to hyperacusis, like Bell’s palsy, chronic fatigue syndrome, Lyme disease, Ménière's disease, post-traumatic stress disorder, depression and autism.
Additionally, hyperacusis is seen in patients who have experienced a head trauma, such as an air bag deployment, surgery to the jaw or face, or a viral infection of the inner ear.
One major cause of hyperacusis is loud noise exposure. It may be triggered by a single intense noise such as a gunshot, or it may develop gradually from listening to loud noise without hearing protection. People exposed to loud levels of noise through their occupation, whether as a machinist or a musician, should be protective of their hearing to avoid noise-induced hearing loss and other changes in their hearing such as tinnitus or hyperacusis.
Depending on the cause, hyperacusis may get better with time. Specifically, in cases of trauma to the brain or hearing system, there is a chance that the sensitivity to sounds will become more tolerable. In cases where the cause is not clear, however, relief may not come on its own. I do not have any personal experience with acupuncture as a successful treatment for hyperacusis.
Many people who suffer from hyperacusis get by in their everyday life by wearing earplugs or earmuffs to reduce incoming sound levels that may be bothersome or by withdrawing from social situations that may have uncomfortable sounds present. This is a logical response.
But these strategies may not work — hyperacusis sufferers may be furthering their poor tolerance to relatively soft sounds. Wearing earplugs or earmuffs may provide immediate relief from an environment that seems uncomfortably loud, but when the individual eventually removes the earplugs or earmuffs, that environment will seem even louder than it might have otherwise.
Additional resource: http://www.hyperacusis.org/
Hearing Loss Costs Far More Than Ability to Hear
By Jane E. Brody : NY Times : September 28, 2015
Mark Hammel’s hearing was damaged in his 20s by machine gun fire when he served in the Israeli Army. But not until decades later, at 57, did he receive his first hearing aids.
“It was very joyful, but also very sad, when I contemplated how much I had missed all those years,” Dr. Hammel, a psychologist in Kingston, N.Y., said in an interview. “I could hear well enough sitting face to face with someone in a quiet room, but in public, with background noise, I knew people were talking, but I had no idea what they were saying. I just stood there nodding my head and smiling.
“Eventually, I stopped going to social gatherings. Even driving, I couldn’t hear what my daughter was saying in the back seat. I live in the country, and I couldn’t hear the birds singing.
“People with hearing loss often don’t realize what they’re missing,” he said. “So much of what makes us human is social contact, interaction with other human beings. When that’s cut off, it comes with a very high cost.”
And the price people pay is much more than social. As Dr. Hammel now realizes, “the capacity to hear is so essential to overall health.”
Hearing loss is one of the most common conditions affecting adults, and the most common among older adults. An estimated 30 million to 48 million Americans have hearing loss that significantly diminishes the quality of their lives — academically, professionally and medically as well as socially.
One person in three older than 60 has life-diminishing hearing loss, but most older adults wait five to 15 years before they seek help, according to a 2012 report in Healthy Hearing magazine. And the longer the delay, the more one misses of life and the harder it can be to adjust to hearing aids.
As Dr. Hammel put it: “I had lost the habit of listening. After I got the aids, it took me a long time to get back into the habit of paying attention to what people were saying.”
The author of the Healthy Hearing report, Debbie Clason, pointed out that “the sooner you get help for your hearing impairment, the easier it will be for your brain to use the auditory pathways it’s developed for processing sound.”
The National Register of Health Service Psychologists states in an online continuing education course, “For the majority of people with hearing loss, the difficulties faced can wreak havoc in a person’s life.” Yet, the register added, “many people who have hearing loss are not aware of it, do not accept the fact of it, or are unwilling to discuss their hearing loss.”
In a large survey by the National Council on the Aging, two-thirds of older adults with untreated hearing loss explained their reluctance to get a hearing aid with statements like “my hearing is not bad enough” or “I can get along without one,” and one person in five said things like “it would make me feel old” or “I don’t like what others will think about me.”
However, those in the survey who had hearing aids were, on average, more socially active and less likely to be depressed, worried, paranoid or insecure, and their family members and friends were even more likely than they were to have noticed these benefits.
The findings of the survey, conducted among 2,096 hearing-impaired people and 1,710 of their family members and friends, and funded by the Hearing Industries Association, a trade group, were published in 1999, but experts say little has changed in people’s attitudes and treatment of hearing loss.
Many who are hard of hearing don’t realize how distressing it is to family members, who typically report feeling frustrated, annoyed and sad as a consequence of communication difficulties and misunderstandings.
For the hearing-impaired person, confusion, difficulty focusing and distracting thoughts are common cognitive impairments, Andrea Ciorba of the University Hospital of Ferrara in Italy and colleagues reported in Clinical Interventions in Aging. Other frequently reported problems include an inability to think straight and difficulty making decisions.
When people can’t hear what is being said, they may become anxious and even suspect that others are talking about them behind their backs or saying things others don’t want them to hear. Anger, embarrassment and a loss of self-esteem are common emotional fallout.
Links have also been found to an increased risk of dementia, which is not surprising given the diminished cognitive input among those with untreated hearing loss. In a 2013 study of 1,984 older adultsliving independently and followed for 11 years with repeated cognitive examinations, “rates of cognitive decline and the risk for incident cognitive impairment were linearly associated with the severity of an individual’s baseline hearing loss,” Dr. Frank R. Lin of the Johns Hopkins Center on Aging and Health and his colleagues in the Health ABC Study Group reported.
Untreated hearing loss can have physical consequences as well, including excessive fatigue, stress and headaches, which may result from trying so hard to hear and understand spoken language. One recent study found that moderate to severe hearing loss was associated with a 54 percent increased risk of death, and mild hearing loss with a 27 percent increased risk of death, compared with individuals with normal hearing. Affected individuals also report more problems with eating, sleeping and sex, according to Deborah Touchette, an audiologist in Paradise, Calif.
Working people with poor hearing are more likely to earn less than those with good hearing; they may even risk losing their jobs if the work depends on good communication.
“If the boss says, ‘Don’t go over $15,000 on that contract,’ and the employee hears $50,000, there is a potential for problems,” the national register wrote. A 2011 study by the Better Hearing Institute, the educational arm of the Hearing Industries Association, found that untreated hearing loss adversely affected productivity, performance and career success, and was associated with a loss in annual income that could reach $30,000. Those in the study with severe hearing loss were twice as likely to be unemployed as people with normal hearing and nearly twice as likely to be out of work as their peers who used hearing aids.
There are safety issues, too, for someone who may miss auditory signals important for survival, like alarms, car horns and shouts of warning, as well as the potential impact of missing sounds like the ringing of a telephone, doorbell or alarm clock.
By Jane E. Brody : NY Times : September 28, 2015
Mark Hammel’s hearing was damaged in his 20s by machine gun fire when he served in the Israeli Army. But not until decades later, at 57, did he receive his first hearing aids.
“It was very joyful, but also very sad, when I contemplated how much I had missed all those years,” Dr. Hammel, a psychologist in Kingston, N.Y., said in an interview. “I could hear well enough sitting face to face with someone in a quiet room, but in public, with background noise, I knew people were talking, but I had no idea what they were saying. I just stood there nodding my head and smiling.
“Eventually, I stopped going to social gatherings. Even driving, I couldn’t hear what my daughter was saying in the back seat. I live in the country, and I couldn’t hear the birds singing.
“People with hearing loss often don’t realize what they’re missing,” he said. “So much of what makes us human is social contact, interaction with other human beings. When that’s cut off, it comes with a very high cost.”
And the price people pay is much more than social. As Dr. Hammel now realizes, “the capacity to hear is so essential to overall health.”
Hearing loss is one of the most common conditions affecting adults, and the most common among older adults. An estimated 30 million to 48 million Americans have hearing loss that significantly diminishes the quality of their lives — academically, professionally and medically as well as socially.
One person in three older than 60 has life-diminishing hearing loss, but most older adults wait five to 15 years before they seek help, according to a 2012 report in Healthy Hearing magazine. And the longer the delay, the more one misses of life and the harder it can be to adjust to hearing aids.
As Dr. Hammel put it: “I had lost the habit of listening. After I got the aids, it took me a long time to get back into the habit of paying attention to what people were saying.”
The author of the Healthy Hearing report, Debbie Clason, pointed out that “the sooner you get help for your hearing impairment, the easier it will be for your brain to use the auditory pathways it’s developed for processing sound.”
The National Register of Health Service Psychologists states in an online continuing education course, “For the majority of people with hearing loss, the difficulties faced can wreak havoc in a person’s life.” Yet, the register added, “many people who have hearing loss are not aware of it, do not accept the fact of it, or are unwilling to discuss their hearing loss.”
In a large survey by the National Council on the Aging, two-thirds of older adults with untreated hearing loss explained their reluctance to get a hearing aid with statements like “my hearing is not bad enough” or “I can get along without one,” and one person in five said things like “it would make me feel old” or “I don’t like what others will think about me.”
However, those in the survey who had hearing aids were, on average, more socially active and less likely to be depressed, worried, paranoid or insecure, and their family members and friends were even more likely than they were to have noticed these benefits.
The findings of the survey, conducted among 2,096 hearing-impaired people and 1,710 of their family members and friends, and funded by the Hearing Industries Association, a trade group, were published in 1999, but experts say little has changed in people’s attitudes and treatment of hearing loss.
Many who are hard of hearing don’t realize how distressing it is to family members, who typically report feeling frustrated, annoyed and sad as a consequence of communication difficulties and misunderstandings.
For the hearing-impaired person, confusion, difficulty focusing and distracting thoughts are common cognitive impairments, Andrea Ciorba of the University Hospital of Ferrara in Italy and colleagues reported in Clinical Interventions in Aging. Other frequently reported problems include an inability to think straight and difficulty making decisions.
When people can’t hear what is being said, they may become anxious and even suspect that others are talking about them behind their backs or saying things others don’t want them to hear. Anger, embarrassment and a loss of self-esteem are common emotional fallout.
Links have also been found to an increased risk of dementia, which is not surprising given the diminished cognitive input among those with untreated hearing loss. In a 2013 study of 1,984 older adultsliving independently and followed for 11 years with repeated cognitive examinations, “rates of cognitive decline and the risk for incident cognitive impairment were linearly associated with the severity of an individual’s baseline hearing loss,” Dr. Frank R. Lin of the Johns Hopkins Center on Aging and Health and his colleagues in the Health ABC Study Group reported.
Untreated hearing loss can have physical consequences as well, including excessive fatigue, stress and headaches, which may result from trying so hard to hear and understand spoken language. One recent study found that moderate to severe hearing loss was associated with a 54 percent increased risk of death, and mild hearing loss with a 27 percent increased risk of death, compared with individuals with normal hearing. Affected individuals also report more problems with eating, sleeping and sex, according to Deborah Touchette, an audiologist in Paradise, Calif.
Working people with poor hearing are more likely to earn less than those with good hearing; they may even risk losing their jobs if the work depends on good communication.
“If the boss says, ‘Don’t go over $15,000 on that contract,’ and the employee hears $50,000, there is a potential for problems,” the national register wrote. A 2011 study by the Better Hearing Institute, the educational arm of the Hearing Industries Association, found that untreated hearing loss adversely affected productivity, performance and career success, and was associated with a loss in annual income that could reach $30,000. Those in the study with severe hearing loss were twice as likely to be unemployed as people with normal hearing and nearly twice as likely to be out of work as their peers who used hearing aids.
There are safety issues, too, for someone who may miss auditory signals important for survival, like alarms, car horns and shouts of warning, as well as the potential impact of missing sounds like the ringing of a telephone, doorbell or alarm clock.
Looking for the Right Solution to Hearing Problems
This is the second set of answers to reader questions from Neil J. DiSarno, chief staff officer for audiology at the American Speech-Language-Hearing Association, and a former chairman of the department of communication sciences and disorders at Missouri State University. Dr. DiSarno’s first set of answers can be found here. Because more than 200 people wrote in, not all questions can be answered individually; Dr. DiSarno selected representative questions on similar topics. This feature is closed to new questions.
HEARING AIDS
Many people wrote in with questions about hearing aids. Before answering a few individual questions, I’ll address the common topics of cost, technology, advancements and method of service delivery.
Cost. Hearing aids are medical devices regulated by the Food and Drug Administration. Like most medical devices in our country, they are expensive. Cost certainly is one reason why so many who would benefit from hearing aid use are not hearing aid users. Cost is also why so many people may have dentures instead of dental implants. Health care is expensive, and for those working to try to contain costs we wish you great success.
That said, a prospective hearing aid user does not need to purchase units that provide benefits greater than those needed by the individual patient. When discussing choices of models with your health care provider, your consultation should include information about your lifestyle and individual needs. If you are active and still in the work force, then the features you may most benefit from would be different from someone with a less active lifestyle. Additional features mean additional cost.
Also, learn what is included with the purchase of your hearing aids. Beyond the device, other services in the price of the hearing aid may include initial recommendations, fitting, verification of a correct fitting, orientation to the device and its features, ongoing counseling, repairs and modifications, reprogramming, and documentation. Accessories or batteries may also be included in the price. Walk-in office visits, warranties, and educational sessions may be included. Once you consider the amount of time, the one-on-one professional consultation and follow-up services, costs may be very similar to those of return visits to any health care provider until the benefit you receive is at the highest level possible.
Technology and advancements. One of the most common problems people with impaired hearing encounter is understanding speech in background noise. Hearing aid manufacturers spend large amounts of time and money researching ways to produce a device that can mimic the capabilities of the normal auditory system. What the hearing aid user needs is an improved signal-to-noise ratio — to have what is important to hear to be more distinct than the less important background noise. This research has led to the use of multiple microphone arrays, FM transmission, Bluetooth technology and sophisticated sound analysis and processing strategies, just to name a few. These advances have resulted in some success, and more is expected. Researchers are looking for ways to combine cellphone technology coupled with hearing aids to do more than just improve your ability to hear on the phone. We should keep in mind, however, that we are asking an electronic device to replicate the workings of one of the most complex organs in the human body. Also, remember that when hearing aid use is put off until later years, other health issues can limit whether an individual can take advantage of the accessories used to improve listening in noise.
Method of delivery. There are a number of ways you can go about being fit with hearing aids. You just need to open your newspaper to see the proliferation of advertisements. Do I have a bias? I have spent the past 35 years as a practicing audiologist and 20 of those years as an instructor of audiology students. Audiologists now need a total of eight years of college to deal with the wide array of hearing and balance issues presented by patients as young as 1 month of age to the elderly. That said, we all would like to consider ourselves savvy consumers who do not want to pay more for a service than is necessary. Understanding that the device (hearing aid) is a part of your rehabilitation plan, ask yourself what is it that you need. Are you a sophisticated, longtime user looking for replacement hearing aids? Or, are you exploring whether hearing aids will benefit you? Ask other people where they obtain services and if they are satisfied.
As you might expect, the Internet is now in the hearing aid dispensing business. Be wary and be warned. I do not recommend purchasing hearing aids online. The Internet offers many advantages for consumers looking for information and products. Online purchasing is convenient and private, and although it may offer cost savings for individuals, before you buy devices like hearing aids online, here are some things you should know:
¶A hearing aid is a complex medical device, not a simple sound amplifier.
¶Hearing aids have digital technology that can be set by an audiologist to meet your personal hearing needs.
¶Hearing aids bought online without a complete hearing test and other necessary hearing therapy/treatment services may not meet your needs.
¶Setting hearing aids for your needs requires specific computer software that audiologists may not have access to if the devices were bought online. For some online businesses, getting the hearing aid settings changed may only be possible by shipping the hearing aid back to the manufacturer, which means you will have to go without your hearing aid for a while.
¶Online hearing screens cannot tell you the cause of hearing loss — the cause may be something as minor as too much earwax or as serious as a brain tumor.
The F.D.A. strongly recommends that you see a physician to rule out medical causes of hearing loss before buying hearing aids. If your doctor determines your hearing loss is not medically treatable, ask to be referred to a licensed audiologist to see if you are a candidate for hearing aids.
Audiologists are professionals who can provide adjustment and programming of the devices, counseling, hearing training and support when you obtain hearing aids from them. Hearing aids bought online do not include these services.
Q. Hearing aids come in a wide range of prices. Many audiologists have ties to specific manufacturers and push their products. How do I find neutral advice to sort through what’s on the market to get what I need but no more? — John Adams, Canaan, N.Y.
Q. My husband has had two different hearing aids and wasn’t satisfied with either of them. The last pair he stopped wearing after losing one several years ago. His hearing has continued to deteriorate and is starting to think his mind is going because he’s often struggling so hard to hear words he can’t process meaning well enough. He is reluctant to try buying hearing aids again. What can he do or say when he goes through the process again — if I can coax him to — so that a new pair will work better for him? Shouldn’t an audiologist be able to explain how much help hearing aids should be in general for an individual patient? Why aren’t there support groups for those wearing hearing aids?
— Susie, Conn.
A. John, some audiologists may limit their offerings of hearing aids to two or three of the major hearing aid manufacturers. That is not necessarily a negative. Becoming extremely familiar with the complexities of a range of products that you know can meet the needs of your patients can actually result in better outcomes for the patient. Hearing aids do range in price and they also range in level of technology. Once your audiologist knows what listening situations are most difficult for you and has information regarding your lifestyle, hearing aids with an appropriate level of technology would be chosen for you to use on a 30- to 45-day trial basis. Be sure you are offered a trial and be sure you have a good understanding of the follow-up services you can expect.
Hearing aids are miniature computers with multiple parameters that can be adjusted based on patient-reported outcomes. Your audiologist should arrange to see you one to two weeks after the initial fitting and at least one or two more times before the end of your trial period. These visits provide opportunities for the patient to report their progress and for the audiologist to make changes to hearing aid properties to better meet your needs. You should expect your audiologist to administer a measure that verifies the appropriateness of the hearing aids chosen.
Keep in mind that you must establish realistic expectations. If your audiologist does not address realistic expectations based on the severity of your hearing impairment, you may likely be a disappointed hearing aid user. Patients expect that because there is a high cost involved in the purchase of hearing aids, the result should be somewhere near perfect. This is rarely the case because of the complex nature of the auditory system and the damage the individual’s auditory system has sustained.
Be sure your evaluation includes a test of speech recognition. You will be asked to repeat prerecorded speech presented to you under headphones. If your ability to repeat those words is very poor, then the benefit you may receive from the use of hearing aids may be limited. This does not mean that you should not use hearing aids. If you are unable to follow conversation unless it is amplified then you need hearing aids. What it does indicate is that in your case hearing aids are only a part of a plan of rehabilitation. You will also have to use a combination of other means to follow speech, like watching faces and becoming better at speech reading and letting others know how best to communicate with you.
With regard to support groups, it would be good for you to check the Web site of the Hearing Loss Association of America http://hearingloss.org/.
Q. Can hearing aids actually damage hearing or accelerate the rate of hearing loss? – Deeanne Westbrook
A. State-of-the-art, appropriately fit hearing aids do not damage hearing. I should emphasize that the fitting of hearing aids must follow a comprehensive diagnostic evaluation administered by an audiologist. Once accurate diagnostic information is available, hearing aids fitted by an experienced individual educated and licensed to fit hearing aids would not damage hearing. Depending upon the underlying cause of the hearing impairment, hearing may continue to decrease. But this would not be as a result of using hearing aids.
Q. Would ahearing aid only in certain situations (assuming it helped) be O.K.? —John Fisher
A. John, the short answer is that you would be the best person to answer your question. If there are situations in which you struggle to follow conversation or believe you are missing important speech information then it would be in your best interest to undergo a trial period using hearing aids. During that time you would have the opportunity to experience how appropriately fitted hearing aids may improve your listening situations. Your hearing health care provider can assist you in developing realistic expectations.
Q. All good information, but what I was hoping to find here was more cutting-edge information about new assistive technologies, e.g.: the future of using smart phones or tablets as bluetooth streamers for appropriately configured hearing aids, or advances in the development of speech-clarification algorithms in hearing aids. Perhaps in the next section? — David, Massachusetts
A. David, you have hit on many of the advances in hearing aid technology. Smart phone and tablet coupling with hearing aids is believed to be in development stages and will hopefully be available within the next year. Bluetooth streamers are already used successfully for many individuals who benefit from connectivity with their cell phones, automobile sound systems and televisions. Manufacturers keep a good deal of their upcoming innovations relatively quiet until they are just ready to hit the consumer market.
GENETIC CAUSES
Q. I’ve been diagnosed with hereditary “cookie bite” hearing loss. My mom only has 10 percent of her hearing left. Will hearing aids help prevent a loss like hers by keeping the synapses firing between ear/brain or is that just wishful thinking? Also, is there any other treatment for my type of loss? — Kristen Brakeman, Los Angeles
A. By “cookie bite” hearing loss I’m assuming you mean that the midrange of your hearing has sustained the greatest impairment, with your ability to hear low-frequency and high-frequency sounds being less affected. When hearing aids bring sound into an audible range for an individual with impaired hearing, the effects on the auditory system that would otherwise be deprived of sensory input are believed to be lessened. The auditory system requires a certain amount of communication between ear and brain to keep functioning. If the severity of your loss continues as you relate your mother’s has, cochlear implantation may be a treatment option. More information on cochlear implants is provided below. A comprehensive audiological evaluation will be required to determine treatment for your type of loss and can help to determine if hearing aid use would be beneficial.
Readers may find the following information regarding hereditary deafness helpful.
Genetic, or hereditary, factors are thought to cause more than 50 percent of all hearing loss.
In the most common hereditary pattern, accounting for about 70 percent of cases of genetic hearing loss, each parent carries both a normal gene and a defective gene that is recessive, meaning that it causes hearing loss only when paired with the same defective gene from the other parent. Parents are often surprised to discover their child has a hearing loss because their own hearing was unaffected and they were unaware that they carried a defective gene.
Another type of hearing loss, accounting for about 15 percent of genetic hearing loss, can occur when an abnormal gene from one parent is dominant, meaning it is able to cause hearing loss even though the matching gene from the other parent is normal. The parent who carries the dominant gene may also have hearing loss as well as other signs and symptoms that make up a genetic syndrome.
Other, rarer types of genetic hearing loss include X-linked (related to the sex chromosome) or mitochondrial inheritance patterns.
Genetic testing involves looking at a person’s DNA to see if certain mutations are present. Typically, DNA samples are obtained through a blood test or from a swab of the inside of the cheek. The GJB2 gene contains the instructions for a protein called Connexin 26; this protein plays an important role in the functioning of the cochlea, or inner ear. The cochlea is very complex and needs many instructions to guide its development and functioning. Inaccurate instructions from defective genes can result in hearing loss.
Possible benefits of genetic testing include:
¶Accurate determination of the cause of hearing loss.
¶Reduction and/or elimination of the need for further testing.
¶Prognostic information about future hearing and potential medical complications.
¶Guidance regarding treatment and long-term medical management.
¶Information regarding the chances of passing the condition on to children.
ASYMMETRICAL HEARING LOSS
Q. I am 52 and had a horrible ear infection about three months ago. I couldn’t hear a thing out of my right ear. It took four rounds of antibiotics to clear up the infection. Since that experience, I have a hard time distinguishing where the phone is when it’s ringing. Does this indicate that my hearing was permanently damaged? — Deck of Cards, MA
Q. Twenty years ago I was diagnosed by an ENT as having a serious “cookie bite” hearing loss in one ear where the middle range of hearing was essentially wiped out. He thought it was the result of a concussive martial arts injury I had experienced a few years earlier and called my condition “profound, progressive and irreversible.” The ENT went on to tell me that hearing aids would not help and I should learn to read lips. He was correct about the progression of my hearing loss, but I trust you may be able to prove him wrong about the hopelessness of my situation. — Selkie, CA
A. Each of these individuals describes what appears to be asymmetrical hearing loss, or hearing poorer for one ear than the other. One reason an individual may have a hard time distinguishing where the phone is when it rings is because sounds are heard first by the ear with the better hearing, and when your brain is provided with this information the tendency is to turn toward your more sensitive side. Individuals with asymmetrical or single-sided deafness have difficulty locating the source of sounds as well as increased difficulty understanding speech in background noise. A comprehensive audiological evaluation will provide information as to whether his hearing test results suggest permanent damage.
Selkie describes a condition of profound hearing loss in one ear. If he was told that hearing aids would not help, the hearing health care specialist may have been referring to use of a conventional hearing aid on the damaged ear. There exists a hearing aid fitting strategy where the damaged ear is fit with a microphone and the better ear fit with an amplifier (much like a traditional hearing aid). When sounds are presented to the impaired side, the microphone picks up that sound and sends it wirelessly to the better ear. The way the brain interprets the sounds from the impaired side allows the individual to learn to turn to that direction. This type of fitting is referred to a CROS (contralateral routing of off-side signals) fitting. Learning to adapt to such a fitting can be a challenge. As a cautionary note, I hope none of the readers will ever become comfortable diagnosing their own hearing deficits, especially when they occur on only one side of the body. Unilateral hearing loss may be a condition caused by a growth or tumor in the auditory pathway. Although the condition is rare, undergoing examination by hearing health care professionals is strongly advised.
ALCOHOL, MEDICINE AND HEARING PROTECTION
Q. I am 28 years old and I have sensory-neural hearing loss from birth. I cannot hear anything in my left ear and I have moderate loss in my right ear. What is the effect of coffee, alcohol and various foods and medicines on the hearing loss? How can I prevent further loss in my right ear? Are there any treatments to restore hearing? How can I get cheaper hearing aids? — vkm, Jersey City
A. Certain medications are known to cause or further hearing loss. Medications with properties known to damage hearing are prescribed to treat very serious illnesses and only when other, nontoxic medications would be ineffective. With regard to the effects of alcohol, it is believed that cumulative, lifelong consumption of large amounts of alcohol can inflict damage to the central auditory system, which is reflected as hearing loss. Protecting and preserving your remaining hearing is critical.
Wear hearing protection. Cotton in the ears will not work. Hearing protection, like earmuffs or earplugs, can be purchased at drugstores, hardware stores or sporting goods stores. Custom earmolds can be made to fit your ears and are available from audiologists or other hearing health care providers. Learn how to correctly insert the earplugs and earmolds for the best noise reduction. Earmuffs that fit completely over both ears can be used in combination with earplugs to achieve greater sound reduction.
Reduce the loudness of the sound. Keep personal listening devices set to no more than half volume. Earphones that fit snugly into your ear canals generally require less sound power. This is because the user does not have to turn them up high to overcome the effects of other noise in the environment.
Be a good consumer. Look for noise ratings on appliances, sporting equipment, power tools and hair dryers. Purchase quieter products. This is especially important when purchasing toys for children.
Be a local advocate. Some movie theaters, health clubs, dance clubs, bars and amusement centers are very noisy. Speak to managers and those in charge about the loud noise and the potential damage to hearing. Ask to have the noise lowered. More information about noise can be found here.
EAR PROTECTION
Q. I wear disposable soft foam earplugs with a 32db SNR for my work as a sculptor, and often keep them in as I navigate the subway or need to concentrate in a noisy situation and as a rule when I sleep. My ears feel fine and I am able to hear people speak with them in, but certainly there is a ringing in my ears when I have them in. I ignore the ringing, but wonder about the effects of wearing earplugs so much. — Djkoob, New York
A. I applaud you for your consistent use of hearing protection. Hearing protection devices with a 32 dB noise reduction rating should protect your hearing when sculpting, unless the amount of time you are exposed to the noise and the intensity of the sculpting noise exceeds known levels of safe exposure. If your ears are ringing when exposed to the sculpting noise, it is possible that you may be exceeding safe exposure times. I am unaware of any detrimental effects of using hearing protection long term.
AGE AND HEARING
Q. At what age would you recommend a screening test for hearing loss? When does Joe Average start to have diminished hearing? — Meg, Denver
Often your family physician will ask you about changes in your hearing. If you suspect decreased hearing sensitivity, this is an opportunity to speak to a professional regarding a referral for an audiological examination. Hearing loss can occur at any age, but of course there is a direct relationship between aging and decreases in hearing sensitivity. Asking others to repeat themselves, feeling that people are mumbling or having difficulty following rapid speech may be signs of decreased hearing.
COCHLEAR IMPLANTS
Q. Is there any point in a person with total hearing loss in one ear and reasonably good hearing in the other getting a cochlear implant, especially considering the recent link between deafness and dementia? — Mary, London
Q. What exactly are cochlear implants? Are they a useful substitute for hearing aids? — zb, Shippensburg, PA
Q. If there is a next installment, perhaps cochlear implants could be the topic. After 50 years of profound deafness, my wife recovered her hearing through such an implant. She now has binaural implants. While music is not really accessible for her, she is able to use the phone, watch television, watch movies, attend lectures, etc. She also employs assistive technologies like FM transceivers to improve sound quality in noisy environments. — vint cerf, Stockholm
A. A cochlear implant is a device that provides direct electrical stimulation to the auditory nerve in the inner ear. Children and adults with a severe to profound hearing loss who cannot be helped with hearing aids may be helped with cochlear implants.
This type of hearing loss is sensorineural, which means there is damage to the tiny hair cells in the part of the inner ear called the cochlea. Because of this damage, sound cannot reach the auditory nerve. With a cochlear implant, the damaged hair cells are bypassed, and the auditory nerve is stimulated directly.
The cochlear implant does not result in “restored” or “cured” hearing. It does, however, allow for the perception of the sensation of sound.
Implanted hearing devices including cochlear implants and bone-anchored hearing aids continue to advance after many years of experience, technical advances in design and improvement in programming strategies as well as changes in criteria for patient selection.
The benefits from a cochlear implant depend on many factors, including the age of the patient when he or she receives the implant; whether the hearing loss was present before or after the patient developed language skills; and the motivation of the patient and family.
An excellent resource for information about cochlear implants can be found on this F.D.A. Web page.
You may also find the linked article, “The Mind Hears: Tuning In With a Cochlear Implant,” by Susan Boswell, of interest.
More information on this topic can be found here in the Audiology Information Series by my organization, the American Speech-Language-Hearing Association.
Mary from London, thank you for asking about the use of a cochlear implant on the patient’s deaf side when he or she had near-normal hearing on the other. A recent study found that cochlear implantation improved hearing abilities in people with single-sided deafness and was found to be superior to the alternative treatment options. The researchers also determined that the use of the cochlear implant did not interfere with speech understanding in the normal hearing ear.
EAR WAX
Q. I am 64 and have minor hearing loss (high-pitched sounds) in one ear, while the other ear seems normal. My doctor has noted that I have wax accumulation in both ears, which I have tried to remove with over-the-counter wax removal kits for several years, with minimal success. The doctor says that he cannot remove the wax buildup, that I would need to go to a specialist to do so. Is it likely that this is worth the effort and expense of seeking out a specialist? — Dev Joslin, Monteverde, Costa Rica
A. If you have not been successful with over-the-counter treatments to remove ear wax, I would agree that you should see a specialist and have the wax removed professionally.
This is the second set of answers to reader questions from Neil J. DiSarno, chief staff officer for audiology at the American Speech-Language-Hearing Association, and a former chairman of the department of communication sciences and disorders at Missouri State University. Dr. DiSarno’s first set of answers can be found here. Because more than 200 people wrote in, not all questions can be answered individually; Dr. DiSarno selected representative questions on similar topics. This feature is closed to new questions.
HEARING AIDS
Many people wrote in with questions about hearing aids. Before answering a few individual questions, I’ll address the common topics of cost, technology, advancements and method of service delivery.
Cost. Hearing aids are medical devices regulated by the Food and Drug Administration. Like most medical devices in our country, they are expensive. Cost certainly is one reason why so many who would benefit from hearing aid use are not hearing aid users. Cost is also why so many people may have dentures instead of dental implants. Health care is expensive, and for those working to try to contain costs we wish you great success.
That said, a prospective hearing aid user does not need to purchase units that provide benefits greater than those needed by the individual patient. When discussing choices of models with your health care provider, your consultation should include information about your lifestyle and individual needs. If you are active and still in the work force, then the features you may most benefit from would be different from someone with a less active lifestyle. Additional features mean additional cost.
Also, learn what is included with the purchase of your hearing aids. Beyond the device, other services in the price of the hearing aid may include initial recommendations, fitting, verification of a correct fitting, orientation to the device and its features, ongoing counseling, repairs and modifications, reprogramming, and documentation. Accessories or batteries may also be included in the price. Walk-in office visits, warranties, and educational sessions may be included. Once you consider the amount of time, the one-on-one professional consultation and follow-up services, costs may be very similar to those of return visits to any health care provider until the benefit you receive is at the highest level possible.
Technology and advancements. One of the most common problems people with impaired hearing encounter is understanding speech in background noise. Hearing aid manufacturers spend large amounts of time and money researching ways to produce a device that can mimic the capabilities of the normal auditory system. What the hearing aid user needs is an improved signal-to-noise ratio — to have what is important to hear to be more distinct than the less important background noise. This research has led to the use of multiple microphone arrays, FM transmission, Bluetooth technology and sophisticated sound analysis and processing strategies, just to name a few. These advances have resulted in some success, and more is expected. Researchers are looking for ways to combine cellphone technology coupled with hearing aids to do more than just improve your ability to hear on the phone. We should keep in mind, however, that we are asking an electronic device to replicate the workings of one of the most complex organs in the human body. Also, remember that when hearing aid use is put off until later years, other health issues can limit whether an individual can take advantage of the accessories used to improve listening in noise.
Method of delivery. There are a number of ways you can go about being fit with hearing aids. You just need to open your newspaper to see the proliferation of advertisements. Do I have a bias? I have spent the past 35 years as a practicing audiologist and 20 of those years as an instructor of audiology students. Audiologists now need a total of eight years of college to deal with the wide array of hearing and balance issues presented by patients as young as 1 month of age to the elderly. That said, we all would like to consider ourselves savvy consumers who do not want to pay more for a service than is necessary. Understanding that the device (hearing aid) is a part of your rehabilitation plan, ask yourself what is it that you need. Are you a sophisticated, longtime user looking for replacement hearing aids? Or, are you exploring whether hearing aids will benefit you? Ask other people where they obtain services and if they are satisfied.
As you might expect, the Internet is now in the hearing aid dispensing business. Be wary and be warned. I do not recommend purchasing hearing aids online. The Internet offers many advantages for consumers looking for information and products. Online purchasing is convenient and private, and although it may offer cost savings for individuals, before you buy devices like hearing aids online, here are some things you should know:
¶A hearing aid is a complex medical device, not a simple sound amplifier.
¶Hearing aids have digital technology that can be set by an audiologist to meet your personal hearing needs.
¶Hearing aids bought online without a complete hearing test and other necessary hearing therapy/treatment services may not meet your needs.
¶Setting hearing aids for your needs requires specific computer software that audiologists may not have access to if the devices were bought online. For some online businesses, getting the hearing aid settings changed may only be possible by shipping the hearing aid back to the manufacturer, which means you will have to go without your hearing aid for a while.
¶Online hearing screens cannot tell you the cause of hearing loss — the cause may be something as minor as too much earwax or as serious as a brain tumor.
The F.D.A. strongly recommends that you see a physician to rule out medical causes of hearing loss before buying hearing aids. If your doctor determines your hearing loss is not medically treatable, ask to be referred to a licensed audiologist to see if you are a candidate for hearing aids.
Audiologists are professionals who can provide adjustment and programming of the devices, counseling, hearing training and support when you obtain hearing aids from them. Hearing aids bought online do not include these services.
Q. Hearing aids come in a wide range of prices. Many audiologists have ties to specific manufacturers and push their products. How do I find neutral advice to sort through what’s on the market to get what I need but no more? — John Adams, Canaan, N.Y.
Q. My husband has had two different hearing aids and wasn’t satisfied with either of them. The last pair he stopped wearing after losing one several years ago. His hearing has continued to deteriorate and is starting to think his mind is going because he’s often struggling so hard to hear words he can’t process meaning well enough. He is reluctant to try buying hearing aids again. What can he do or say when he goes through the process again — if I can coax him to — so that a new pair will work better for him? Shouldn’t an audiologist be able to explain how much help hearing aids should be in general for an individual patient? Why aren’t there support groups for those wearing hearing aids?
— Susie, Conn.
A. John, some audiologists may limit their offerings of hearing aids to two or three of the major hearing aid manufacturers. That is not necessarily a negative. Becoming extremely familiar with the complexities of a range of products that you know can meet the needs of your patients can actually result in better outcomes for the patient. Hearing aids do range in price and they also range in level of technology. Once your audiologist knows what listening situations are most difficult for you and has information regarding your lifestyle, hearing aids with an appropriate level of technology would be chosen for you to use on a 30- to 45-day trial basis. Be sure you are offered a trial and be sure you have a good understanding of the follow-up services you can expect.
Hearing aids are miniature computers with multiple parameters that can be adjusted based on patient-reported outcomes. Your audiologist should arrange to see you one to two weeks after the initial fitting and at least one or two more times before the end of your trial period. These visits provide opportunities for the patient to report their progress and for the audiologist to make changes to hearing aid properties to better meet your needs. You should expect your audiologist to administer a measure that verifies the appropriateness of the hearing aids chosen.
Keep in mind that you must establish realistic expectations. If your audiologist does not address realistic expectations based on the severity of your hearing impairment, you may likely be a disappointed hearing aid user. Patients expect that because there is a high cost involved in the purchase of hearing aids, the result should be somewhere near perfect. This is rarely the case because of the complex nature of the auditory system and the damage the individual’s auditory system has sustained.
Be sure your evaluation includes a test of speech recognition. You will be asked to repeat prerecorded speech presented to you under headphones. If your ability to repeat those words is very poor, then the benefit you may receive from the use of hearing aids may be limited. This does not mean that you should not use hearing aids. If you are unable to follow conversation unless it is amplified then you need hearing aids. What it does indicate is that in your case hearing aids are only a part of a plan of rehabilitation. You will also have to use a combination of other means to follow speech, like watching faces and becoming better at speech reading and letting others know how best to communicate with you.
With regard to support groups, it would be good for you to check the Web site of the Hearing Loss Association of America http://hearingloss.org/.
Q. Can hearing aids actually damage hearing or accelerate the rate of hearing loss? – Deeanne Westbrook
A. State-of-the-art, appropriately fit hearing aids do not damage hearing. I should emphasize that the fitting of hearing aids must follow a comprehensive diagnostic evaluation administered by an audiologist. Once accurate diagnostic information is available, hearing aids fitted by an experienced individual educated and licensed to fit hearing aids would not damage hearing. Depending upon the underlying cause of the hearing impairment, hearing may continue to decrease. But this would not be as a result of using hearing aids.
Q. Would ahearing aid only in certain situations (assuming it helped) be O.K.? —John Fisher
A. John, the short answer is that you would be the best person to answer your question. If there are situations in which you struggle to follow conversation or believe you are missing important speech information then it would be in your best interest to undergo a trial period using hearing aids. During that time you would have the opportunity to experience how appropriately fitted hearing aids may improve your listening situations. Your hearing health care provider can assist you in developing realistic expectations.
Q. All good information, but what I was hoping to find here was more cutting-edge information about new assistive technologies, e.g.: the future of using smart phones or tablets as bluetooth streamers for appropriately configured hearing aids, or advances in the development of speech-clarification algorithms in hearing aids. Perhaps in the next section? — David, Massachusetts
A. David, you have hit on many of the advances in hearing aid technology. Smart phone and tablet coupling with hearing aids is believed to be in development stages and will hopefully be available within the next year. Bluetooth streamers are already used successfully for many individuals who benefit from connectivity with their cell phones, automobile sound systems and televisions. Manufacturers keep a good deal of their upcoming innovations relatively quiet until they are just ready to hit the consumer market.
GENETIC CAUSES
Q. I’ve been diagnosed with hereditary “cookie bite” hearing loss. My mom only has 10 percent of her hearing left. Will hearing aids help prevent a loss like hers by keeping the synapses firing between ear/brain or is that just wishful thinking? Also, is there any other treatment for my type of loss? — Kristen Brakeman, Los Angeles
A. By “cookie bite” hearing loss I’m assuming you mean that the midrange of your hearing has sustained the greatest impairment, with your ability to hear low-frequency and high-frequency sounds being less affected. When hearing aids bring sound into an audible range for an individual with impaired hearing, the effects on the auditory system that would otherwise be deprived of sensory input are believed to be lessened. The auditory system requires a certain amount of communication between ear and brain to keep functioning. If the severity of your loss continues as you relate your mother’s has, cochlear implantation may be a treatment option. More information on cochlear implants is provided below. A comprehensive audiological evaluation will be required to determine treatment for your type of loss and can help to determine if hearing aid use would be beneficial.
Readers may find the following information regarding hereditary deafness helpful.
Genetic, or hereditary, factors are thought to cause more than 50 percent of all hearing loss.
In the most common hereditary pattern, accounting for about 70 percent of cases of genetic hearing loss, each parent carries both a normal gene and a defective gene that is recessive, meaning that it causes hearing loss only when paired with the same defective gene from the other parent. Parents are often surprised to discover their child has a hearing loss because their own hearing was unaffected and they were unaware that they carried a defective gene.
Another type of hearing loss, accounting for about 15 percent of genetic hearing loss, can occur when an abnormal gene from one parent is dominant, meaning it is able to cause hearing loss even though the matching gene from the other parent is normal. The parent who carries the dominant gene may also have hearing loss as well as other signs and symptoms that make up a genetic syndrome.
Other, rarer types of genetic hearing loss include X-linked (related to the sex chromosome) or mitochondrial inheritance patterns.
Genetic testing involves looking at a person’s DNA to see if certain mutations are present. Typically, DNA samples are obtained through a blood test or from a swab of the inside of the cheek. The GJB2 gene contains the instructions for a protein called Connexin 26; this protein plays an important role in the functioning of the cochlea, or inner ear. The cochlea is very complex and needs many instructions to guide its development and functioning. Inaccurate instructions from defective genes can result in hearing loss.
Possible benefits of genetic testing include:
¶Accurate determination of the cause of hearing loss.
¶Reduction and/or elimination of the need for further testing.
¶Prognostic information about future hearing and potential medical complications.
¶Guidance regarding treatment and long-term medical management.
¶Information regarding the chances of passing the condition on to children.
ASYMMETRICAL HEARING LOSS
Q. I am 52 and had a horrible ear infection about three months ago. I couldn’t hear a thing out of my right ear. It took four rounds of antibiotics to clear up the infection. Since that experience, I have a hard time distinguishing where the phone is when it’s ringing. Does this indicate that my hearing was permanently damaged? — Deck of Cards, MA
Q. Twenty years ago I was diagnosed by an ENT as having a serious “cookie bite” hearing loss in one ear where the middle range of hearing was essentially wiped out. He thought it was the result of a concussive martial arts injury I had experienced a few years earlier and called my condition “profound, progressive and irreversible.” The ENT went on to tell me that hearing aids would not help and I should learn to read lips. He was correct about the progression of my hearing loss, but I trust you may be able to prove him wrong about the hopelessness of my situation. — Selkie, CA
A. Each of these individuals describes what appears to be asymmetrical hearing loss, or hearing poorer for one ear than the other. One reason an individual may have a hard time distinguishing where the phone is when it rings is because sounds are heard first by the ear with the better hearing, and when your brain is provided with this information the tendency is to turn toward your more sensitive side. Individuals with asymmetrical or single-sided deafness have difficulty locating the source of sounds as well as increased difficulty understanding speech in background noise. A comprehensive audiological evaluation will provide information as to whether his hearing test results suggest permanent damage.
Selkie describes a condition of profound hearing loss in one ear. If he was told that hearing aids would not help, the hearing health care specialist may have been referring to use of a conventional hearing aid on the damaged ear. There exists a hearing aid fitting strategy where the damaged ear is fit with a microphone and the better ear fit with an amplifier (much like a traditional hearing aid). When sounds are presented to the impaired side, the microphone picks up that sound and sends it wirelessly to the better ear. The way the brain interprets the sounds from the impaired side allows the individual to learn to turn to that direction. This type of fitting is referred to a CROS (contralateral routing of off-side signals) fitting. Learning to adapt to such a fitting can be a challenge. As a cautionary note, I hope none of the readers will ever become comfortable diagnosing their own hearing deficits, especially when they occur on only one side of the body. Unilateral hearing loss may be a condition caused by a growth or tumor in the auditory pathway. Although the condition is rare, undergoing examination by hearing health care professionals is strongly advised.
ALCOHOL, MEDICINE AND HEARING PROTECTION
Q. I am 28 years old and I have sensory-neural hearing loss from birth. I cannot hear anything in my left ear and I have moderate loss in my right ear. What is the effect of coffee, alcohol and various foods and medicines on the hearing loss? How can I prevent further loss in my right ear? Are there any treatments to restore hearing? How can I get cheaper hearing aids? — vkm, Jersey City
A. Certain medications are known to cause or further hearing loss. Medications with properties known to damage hearing are prescribed to treat very serious illnesses and only when other, nontoxic medications would be ineffective. With regard to the effects of alcohol, it is believed that cumulative, lifelong consumption of large amounts of alcohol can inflict damage to the central auditory system, which is reflected as hearing loss. Protecting and preserving your remaining hearing is critical.
Wear hearing protection. Cotton in the ears will not work. Hearing protection, like earmuffs or earplugs, can be purchased at drugstores, hardware stores or sporting goods stores. Custom earmolds can be made to fit your ears and are available from audiologists or other hearing health care providers. Learn how to correctly insert the earplugs and earmolds for the best noise reduction. Earmuffs that fit completely over both ears can be used in combination with earplugs to achieve greater sound reduction.
Reduce the loudness of the sound. Keep personal listening devices set to no more than half volume. Earphones that fit snugly into your ear canals generally require less sound power. This is because the user does not have to turn them up high to overcome the effects of other noise in the environment.
Be a good consumer. Look for noise ratings on appliances, sporting equipment, power tools and hair dryers. Purchase quieter products. This is especially important when purchasing toys for children.
Be a local advocate. Some movie theaters, health clubs, dance clubs, bars and amusement centers are very noisy. Speak to managers and those in charge about the loud noise and the potential damage to hearing. Ask to have the noise lowered. More information about noise can be found here.
EAR PROTECTION
Q. I wear disposable soft foam earplugs with a 32db SNR for my work as a sculptor, and often keep them in as I navigate the subway or need to concentrate in a noisy situation and as a rule when I sleep. My ears feel fine and I am able to hear people speak with them in, but certainly there is a ringing in my ears when I have them in. I ignore the ringing, but wonder about the effects of wearing earplugs so much. — Djkoob, New York
A. I applaud you for your consistent use of hearing protection. Hearing protection devices with a 32 dB noise reduction rating should protect your hearing when sculpting, unless the amount of time you are exposed to the noise and the intensity of the sculpting noise exceeds known levels of safe exposure. If your ears are ringing when exposed to the sculpting noise, it is possible that you may be exceeding safe exposure times. I am unaware of any detrimental effects of using hearing protection long term.
AGE AND HEARING
Q. At what age would you recommend a screening test for hearing loss? When does Joe Average start to have diminished hearing? — Meg, Denver
Often your family physician will ask you about changes in your hearing. If you suspect decreased hearing sensitivity, this is an opportunity to speak to a professional regarding a referral for an audiological examination. Hearing loss can occur at any age, but of course there is a direct relationship between aging and decreases in hearing sensitivity. Asking others to repeat themselves, feeling that people are mumbling or having difficulty following rapid speech may be signs of decreased hearing.
COCHLEAR IMPLANTS
Q. Is there any point in a person with total hearing loss in one ear and reasonably good hearing in the other getting a cochlear implant, especially considering the recent link between deafness and dementia? — Mary, London
Q. What exactly are cochlear implants? Are they a useful substitute for hearing aids? — zb, Shippensburg, PA
Q. If there is a next installment, perhaps cochlear implants could be the topic. After 50 years of profound deafness, my wife recovered her hearing through such an implant. She now has binaural implants. While music is not really accessible for her, she is able to use the phone, watch television, watch movies, attend lectures, etc. She also employs assistive technologies like FM transceivers to improve sound quality in noisy environments. — vint cerf, Stockholm
A. A cochlear implant is a device that provides direct electrical stimulation to the auditory nerve in the inner ear. Children and adults with a severe to profound hearing loss who cannot be helped with hearing aids may be helped with cochlear implants.
This type of hearing loss is sensorineural, which means there is damage to the tiny hair cells in the part of the inner ear called the cochlea. Because of this damage, sound cannot reach the auditory nerve. With a cochlear implant, the damaged hair cells are bypassed, and the auditory nerve is stimulated directly.
The cochlear implant does not result in “restored” or “cured” hearing. It does, however, allow for the perception of the sensation of sound.
Implanted hearing devices including cochlear implants and bone-anchored hearing aids continue to advance after many years of experience, technical advances in design and improvement in programming strategies as well as changes in criteria for patient selection.
The benefits from a cochlear implant depend on many factors, including the age of the patient when he or she receives the implant; whether the hearing loss was present before or after the patient developed language skills; and the motivation of the patient and family.
An excellent resource for information about cochlear implants can be found on this F.D.A. Web page.
You may also find the linked article, “The Mind Hears: Tuning In With a Cochlear Implant,” by Susan Boswell, of interest.
More information on this topic can be found here in the Audiology Information Series by my organization, the American Speech-Language-Hearing Association.
Mary from London, thank you for asking about the use of a cochlear implant on the patient’s deaf side when he or she had near-normal hearing on the other. A recent study found that cochlear implantation improved hearing abilities in people with single-sided deafness and was found to be superior to the alternative treatment options. The researchers also determined that the use of the cochlear implant did not interfere with speech understanding in the normal hearing ear.
EAR WAX
Q. I am 64 and have minor hearing loss (high-pitched sounds) in one ear, while the other ear seems normal. My doctor has noted that I have wax accumulation in both ears, which I have tried to remove with over-the-counter wax removal kits for several years, with minimal success. The doctor says that he cannot remove the wax buildup, that I would need to go to a specialist to do so. Is it likely that this is worth the effort and expense of seeking out a specialist? — Dev Joslin, Monteverde, Costa Rica
A. If you have not been successful with over-the-counter treatments to remove ear wax, I would agree that you should see a specialist and have the wax removed professionally.
Why Won’t They Get Hearing Aids?
Susan Seliger : NY Times : April 6, 2012
While visiting my parents recently, I overheard a conversation between them that went something like this.
Mom, in the dining room: “Did you take out the trash?”
Dad, in the living room: “I have plenty of cash. What do you need money for?”
“What? I don’t want any money.” “Why did you ask for it?” “What did you say? You’re mumbling again.”
I felt as if I was in the middle of that Abbott and Costello routine. The only difference is that after a while, the daily misunderstandings and frustrations of having to repeat yourself become a lot less funny.
When I suggested to my parents that they might want to get their hearing tested, their first reaction (after exasperated sighs) was that they didn’t want to be bothered. Turns out, they’ve got a lot of company.
“The average person has been having trouble hearing for 7 to 10 years before they come in — they say it’s only been a few months, but we’ve found it’s years,” said Dr. Eric Hagberg, an audiologist in Youngstown, Ohio, and president of the Academy of Doctors of Audiology.
Of the 26.7 million people over age 50 with a hearing impairment, only one in seven, a meager 14 percent, use a hearing aid, said Dr. Frank Lin, assistant professor of otolaryngology and epidemiology at Johns Hopkins University. “If you think you have a hearing loss, you probably do,” he said.
Why so much resistance to getting hearing impairment diagnosed and treated? First, denial. Many older adults just don’t think they have a problem.
“The No. 1 thing I get from patients is ‘I hear what I want to hear,’ ” said Dr. Linda S. Remensnyder, an audiologist in Libertyville, Ill. “What they don’t understand is that in order to be fully engaged in life, you have to be fully engaged everywhere.”
The person with a hearing problem is often the last to notice it, because the change comes on gradually over years and starts subtly. Adults with hearing loss typically say, “I can hear just fine if people would just stop mumbling.”
They’re half right. It isn’t that they can’t hear — they can. The problem is that they can’t understand. The first clue to a hearing impairment is mixing up consonants. Age-related hearing loss often occurs in the high-frequency ranges that, in English, tend to carry the consonants.
And many older adults think it’s normal to lose some hearing ability. If a majority of older people have hearing loss – and 55 percent of those over age 70 do — then it can’t be that harmful, right?
Wrong. Because the ear plays a role in balance, hearing loss can lead to falls. “Even mild hearing loss can triple the risk of falling,” said Dr. Lin, citing his own research as well as a study of Finnish twins.
And then there is the mysterious link to dementia. Some studies have suggested that mild hearing loss is linked to a doubling of dementia risk, and that moderate hearing loss can triple it. With severe hearing loss, the risk can be five times as high, according to Dr. Lin’s 2011 study in Archives of Neurology and a report last month in The Journal of the American Medical Association.
It is possible that hearing loss leads to social isolation, itself a risk factor for dementia, said Dr. Lin.
In addition, few people realize that delayed treatment may make hearing loss worse. “If you don’t use it, you’ll lose it,” said Dr. Remensnyder. “I have a retired nurse, age 90, who has lived alone with no auditory stimulation for years. She doesn’t understand 50 percent of the words, and I can’t reverse that now.”
Even among the enlightened, hearing aids still carry a stigma. “Men think, ‘It’s a sign of weakness,’ and women think, ‘It’s showing my age,’ ” said Dr. Hagberg. Anyone over 60 remembers when the words “deaf and dumb” were always uttered together – and “dumb” was not used to mean “mute.”
Vanity, too, is still a deterrent. But that may be receding now that new hearing aids are smaller and less visible than ever. Besides, it’s increasingly commonplace to see young and old alike walking around with devices plugged into their ears. (A good thing, too, because the bigger, more noticeable devices tend to produce better sound.)
Money can also be a serious obstacle. Hearing aids can run from $1,800 to $6,800 or more per pair, according to Consumer Reports. They are not covered by Medicare or most insurance. (Caregivers should ask if the audiologist will set up a payment plan – many do.)
Bottom line: Caregivers have a lot of obstacles to overcome, but they also have a lot of ammunition to explain that the health pros in getting hearing help outweigh the cons.
Start with something simple. “Stop being a living hearing aid,” Dr. Hagberg advised. “Everybody has one — a seemingly helpful caregiver, husband or wife who feeds back the information so the other person doesn’t need to seek help.”
Second, “I tell patients who deny they have a problem, even after testing, to go home and pay attention to every time they say, ‘What?’ or they miss the punchline on TV or ask people to repeat something,” said Dr. Hagberg. “They usually come back in a week” – ready for a hearing aid.
Primary care doctors often fail to test for hearing loss. It helps to line up a certified audiologist who is patient and passionate about working with the elderly. Interview certified audiologists (listed here and here) until you find one you like.
Don’t be fooled by the misconception that hearing aids are plug-and-play. “There’s still an art to programming hearing aids,” said Dr. Remensnyder. “I spend 80 percent of my time making adjustments and showing patients how to use them properly.”
Caregivers and patients alike should be realistic about their expectations. Hearing aids won’t solve everything. “I am absolutely pro-hearing aids, but there is vast room for improvement in them,” said Richard Einhorn, whose use of hearing aids and other high-tech devices has enabled him to continue his successful career in New York as a classical composer. Mr. Einhorn pointed out that the sound quality can be especially disappointing in noisy restaurants, where the devices cannot filter out much of the background clatter.
Still, a majority of those who finally get hearing aids — and do the necessary follow-up visits with an audiologist — experience positive results.
“It’s thrilling,” said Barb Merry, age 68, from Appleton, Wis., describing life after she got hearing aids — especially the improvement in watching TV. She uses an additional device in the TV area that operates much the way metal induction loops installed in many theaters, concert halls and public institutions do – transmitting sound directly into a telecoil in her hearing aids.
“When I used to watch ‘Downton Abbey,’ that English series, my understanding was maybe 40 percent at best — I thought the problem was their English accents,” Mrs. Merry said. “But now I understand 95 percent. Only 5 percent is the English thing.”
She continued, “I want to talk to everyone I know and say, ‘Get over the shyness about hearing aids – life can be better.’ “
Susan Seliger : NY Times : April 6, 2012
While visiting my parents recently, I overheard a conversation between them that went something like this.
Mom, in the dining room: “Did you take out the trash?”
Dad, in the living room: “I have plenty of cash. What do you need money for?”
“What? I don’t want any money.” “Why did you ask for it?” “What did you say? You’re mumbling again.”
I felt as if I was in the middle of that Abbott and Costello routine. The only difference is that after a while, the daily misunderstandings and frustrations of having to repeat yourself become a lot less funny.
When I suggested to my parents that they might want to get their hearing tested, their first reaction (after exasperated sighs) was that they didn’t want to be bothered. Turns out, they’ve got a lot of company.
“The average person has been having trouble hearing for 7 to 10 years before they come in — they say it’s only been a few months, but we’ve found it’s years,” said Dr. Eric Hagberg, an audiologist in Youngstown, Ohio, and president of the Academy of Doctors of Audiology.
Of the 26.7 million people over age 50 with a hearing impairment, only one in seven, a meager 14 percent, use a hearing aid, said Dr. Frank Lin, assistant professor of otolaryngology and epidemiology at Johns Hopkins University. “If you think you have a hearing loss, you probably do,” he said.
Why so much resistance to getting hearing impairment diagnosed and treated? First, denial. Many older adults just don’t think they have a problem.
“The No. 1 thing I get from patients is ‘I hear what I want to hear,’ ” said Dr. Linda S. Remensnyder, an audiologist in Libertyville, Ill. “What they don’t understand is that in order to be fully engaged in life, you have to be fully engaged everywhere.”
The person with a hearing problem is often the last to notice it, because the change comes on gradually over years and starts subtly. Adults with hearing loss typically say, “I can hear just fine if people would just stop mumbling.”
They’re half right. It isn’t that they can’t hear — they can. The problem is that they can’t understand. The first clue to a hearing impairment is mixing up consonants. Age-related hearing loss often occurs in the high-frequency ranges that, in English, tend to carry the consonants.
And many older adults think it’s normal to lose some hearing ability. If a majority of older people have hearing loss – and 55 percent of those over age 70 do — then it can’t be that harmful, right?
Wrong. Because the ear plays a role in balance, hearing loss can lead to falls. “Even mild hearing loss can triple the risk of falling,” said Dr. Lin, citing his own research as well as a study of Finnish twins.
And then there is the mysterious link to dementia. Some studies have suggested that mild hearing loss is linked to a doubling of dementia risk, and that moderate hearing loss can triple it. With severe hearing loss, the risk can be five times as high, according to Dr. Lin’s 2011 study in Archives of Neurology and a report last month in The Journal of the American Medical Association.
It is possible that hearing loss leads to social isolation, itself a risk factor for dementia, said Dr. Lin.
In addition, few people realize that delayed treatment may make hearing loss worse. “If you don’t use it, you’ll lose it,” said Dr. Remensnyder. “I have a retired nurse, age 90, who has lived alone with no auditory stimulation for years. She doesn’t understand 50 percent of the words, and I can’t reverse that now.”
Even among the enlightened, hearing aids still carry a stigma. “Men think, ‘It’s a sign of weakness,’ and women think, ‘It’s showing my age,’ ” said Dr. Hagberg. Anyone over 60 remembers when the words “deaf and dumb” were always uttered together – and “dumb” was not used to mean “mute.”
Vanity, too, is still a deterrent. But that may be receding now that new hearing aids are smaller and less visible than ever. Besides, it’s increasingly commonplace to see young and old alike walking around with devices plugged into their ears. (A good thing, too, because the bigger, more noticeable devices tend to produce better sound.)
Money can also be a serious obstacle. Hearing aids can run from $1,800 to $6,800 or more per pair, according to Consumer Reports. They are not covered by Medicare or most insurance. (Caregivers should ask if the audiologist will set up a payment plan – many do.)
Bottom line: Caregivers have a lot of obstacles to overcome, but they also have a lot of ammunition to explain that the health pros in getting hearing help outweigh the cons.
Start with something simple. “Stop being a living hearing aid,” Dr. Hagberg advised. “Everybody has one — a seemingly helpful caregiver, husband or wife who feeds back the information so the other person doesn’t need to seek help.”
Second, “I tell patients who deny they have a problem, even after testing, to go home and pay attention to every time they say, ‘What?’ or they miss the punchline on TV or ask people to repeat something,” said Dr. Hagberg. “They usually come back in a week” – ready for a hearing aid.
Primary care doctors often fail to test for hearing loss. It helps to line up a certified audiologist who is patient and passionate about working with the elderly. Interview certified audiologists (listed here and here) until you find one you like.
Don’t be fooled by the misconception that hearing aids are plug-and-play. “There’s still an art to programming hearing aids,” said Dr. Remensnyder. “I spend 80 percent of my time making adjustments and showing patients how to use them properly.”
Caregivers and patients alike should be realistic about their expectations. Hearing aids won’t solve everything. “I am absolutely pro-hearing aids, but there is vast room for improvement in them,” said Richard Einhorn, whose use of hearing aids and other high-tech devices has enabled him to continue his successful career in New York as a classical composer. Mr. Einhorn pointed out that the sound quality can be especially disappointing in noisy restaurants, where the devices cannot filter out much of the background clatter.
Still, a majority of those who finally get hearing aids — and do the necessary follow-up visits with an audiologist — experience positive results.
“It’s thrilling,” said Barb Merry, age 68, from Appleton, Wis., describing life after she got hearing aids — especially the improvement in watching TV. She uses an additional device in the TV area that operates much the way metal induction loops installed in many theaters, concert halls and public institutions do – transmitting sound directly into a telecoil in her hearing aids.
“When I used to watch ‘Downton Abbey,’ that English series, my understanding was maybe 40 percent at best — I thought the problem was their English accents,” Mrs. Merry said. “But now I understand 95 percent. Only 5 percent is the English thing.”
She continued, “I want to talk to everyone I know and say, ‘Get over the shyness about hearing aids – life can be better.’ “
Lifelines for People With Hearing LossBy Jane E. Brody : NY Times : January 16, 2012
Hearing loss, a disability currently untreated in about 85 percent of those affected, may be the nation’s most damaging and costly sensory handicap. It is a hidden disability, often not obvious to others or even to those who have it.
Its onset is usually insidious, gradually worsening over years and thus easily ignored.
Most of those affected can still hear sounds and think the real problem is that people aren’t speaking clearly. They often ask others to speak up, repeat what was said or speak more slowly. Or they pretend they can hear, but their conversations may be filled with non sequiturs.
As hearing worsens, they are likely to become increasingly frustrated and socially isolated. Unable to hear well in social settings, they gradually stop going to the theater, movies, places of worship, senior centers or parties or out to restaurants with friends or family.
Social isolation, in turn, has been linked to depression and an increased risk of death from conditions like heart disease. And now there is another major risk associated with hearing problems: dementia and Alzheimer’s disease. This finding alone should prompt more people to get their hearing tested and, if found impaired, get properly fitted with aids that can help to keep them cognitively engaged.
Perhaps it will also grab the attention of politicians who determine what is and what is not covered by Medicare and, in turn, by other health insurers. Currently, Medicare does not pay for hearing aids, and many older people cannot afford the many thousands of dollars that quality aids and auditory training can cost.
Furthermore, for the fewer than 15 percent of hearing-impaired people who have hearing aids, the devices themselves are not an adequate solution. Hearing aids work best when the distance between the sound and the listener is less than six feet and when background noise is minimal, which can preclude clear communication in theaters, airports, restaurants and many other social settings.
Hearing and the Brain
Although hearing impairment was first linked in major medical journals to dementia and cognitive dysfunction more than two decades ago, not until last year did researchers demonstrate an independent association with dementia over time.
By following 639 people ages 36 to 90 for nearly 12 years, Dr. Frank R. Lin, an otolaryngologist at Johns Hopkins Medicine, and his colleagues there and at the National Institute on Aging showed a direct relationship between the participants’ degree of hearing loss and their risk of later developing dementia or Alzheimer’s disease.
For each 10-decibel loss in hearing, the risk of dementia rose about 20 percent among the participants. Compared with those who could hear normally when first examined, the risk of dementia doubled among those with mild hearing loss, tripled among those with moderate hearing loss and increased fivefold among those with severe hearing loss.
The relationship between hearing loss and dementia persisted even when other factors linked to cognitive disease, like hypertension, diabetes and smoking, were taken into account.
“People are most likely to notice communication problems when their hearing loss exceeds 25 decibels,” Dr. Lin said in an interview. “It’s not that they can’t hear, but they can’t understand. Hearing loss at this level affects the clarity of words.”
How, then, might this lead to cognitive deficits?
“The brain dedicates a lot of resources to hearing,” Dr. Lin said. “When the clarity of words is garbled, the brain gets a garbled message. It has to reallocate resources to hear at the expense of other brain functions.”
Thus, the overworked brain may lose “cognitive reserve,” the ability of healthy parts of the brain to take over functions lost by other parts.
Another mechanism may be the effects of social isolation. “A decline in social engagement and resulting loneliness is one of the most important determinants of health outcomes in older adults,” Dr. Lin said. Isolation has been linked to an increase in inflammation throughout the body, which in turn can result in age-related disorders like heart disease and dementia, Dr. Lin said.
How Proper Aids Help
Rose Marie Jewett, 83, of Janesville, Wis., who had experienced progressively worsening hearing loss for 40 years, had all but given up hope of hearing others speak or ever again enjoying music.
She said she could understand how hearing loss could lead to dementia, because she was “forgetful” when she did not hear what she should have heard.
It’s not that she forgot things; rather, she had never heard them to begin with, and the strain of constantly trying to piece things together was taking its toll.
“When you can’t hear anybody, you don’t pay attention,” Ms. Jewett said. “You shut yourself off from the world, you don’t think very well, your memory gets bad and you get kind of dull.”
But now it’s a whole new world for Ms. Jewett. Linda S. Remensnyder, an audiologist and founder of Hearing Associates in Illinois, taught her how to maximize her ability to hear clearly in social settings. She fitted Ms. Jewett with the right kind of hearing aids and with devices that allow her to hear clearly on the telephone, when watching television and in public settings that have been equipped with hearing loops.
A hearing loop, installed around the periphery of a room, is a thin copper wire that radiates electromagnetic signals. The signals can be picked up by a tiny receiver called a telecoil that is built into most hearing aids and cochlear implants. With the press of a tiny button on the aid, sound comes through to people with impaired hearing with even greater clarity than can be heard by someone with normal hearing.
Since 2009, Dr. Remensnyder said, hearing loops have been installed in about 1,000 public places, including museums, stores, banks, theaters, airports, sports arenas and other spaces that are challenging for the hearing-impaired.
“The public is misled into thinking that by getting two hearing aids, they’ll be able to hear everywhere,” she said. “Aids are just a small segment of the solution.”
Neither Dr. Lin nor Dr. Remensnyder can yet say whether improving auditory signals for the hearing-impaired will diminish or delay the development of dementia. That remains for a clinical trial to demonstrate. Meanwhile, Dr. Remensnyder said, it can “revolutionize” the lives of people with hearing difficulties, a virtue in itself.
Hearing loss, a disability currently untreated in about 85 percent of those affected, may be the nation’s most damaging and costly sensory handicap. It is a hidden disability, often not obvious to others or even to those who have it.
Its onset is usually insidious, gradually worsening over years and thus easily ignored.
Most of those affected can still hear sounds and think the real problem is that people aren’t speaking clearly. They often ask others to speak up, repeat what was said or speak more slowly. Or they pretend they can hear, but their conversations may be filled with non sequiturs.
As hearing worsens, they are likely to become increasingly frustrated and socially isolated. Unable to hear well in social settings, they gradually stop going to the theater, movies, places of worship, senior centers or parties or out to restaurants with friends or family.
Social isolation, in turn, has been linked to depression and an increased risk of death from conditions like heart disease. And now there is another major risk associated with hearing problems: dementia and Alzheimer’s disease. This finding alone should prompt more people to get their hearing tested and, if found impaired, get properly fitted with aids that can help to keep them cognitively engaged.
Perhaps it will also grab the attention of politicians who determine what is and what is not covered by Medicare and, in turn, by other health insurers. Currently, Medicare does not pay for hearing aids, and many older people cannot afford the many thousands of dollars that quality aids and auditory training can cost.
Furthermore, for the fewer than 15 percent of hearing-impaired people who have hearing aids, the devices themselves are not an adequate solution. Hearing aids work best when the distance between the sound and the listener is less than six feet and when background noise is minimal, which can preclude clear communication in theaters, airports, restaurants and many other social settings.
Hearing and the Brain
Although hearing impairment was first linked in major medical journals to dementia and cognitive dysfunction more than two decades ago, not until last year did researchers demonstrate an independent association with dementia over time.
By following 639 people ages 36 to 90 for nearly 12 years, Dr. Frank R. Lin, an otolaryngologist at Johns Hopkins Medicine, and his colleagues there and at the National Institute on Aging showed a direct relationship between the participants’ degree of hearing loss and their risk of later developing dementia or Alzheimer’s disease.
For each 10-decibel loss in hearing, the risk of dementia rose about 20 percent among the participants. Compared with those who could hear normally when first examined, the risk of dementia doubled among those with mild hearing loss, tripled among those with moderate hearing loss and increased fivefold among those with severe hearing loss.
The relationship between hearing loss and dementia persisted even when other factors linked to cognitive disease, like hypertension, diabetes and smoking, were taken into account.
“People are most likely to notice communication problems when their hearing loss exceeds 25 decibels,” Dr. Lin said in an interview. “It’s not that they can’t hear, but they can’t understand. Hearing loss at this level affects the clarity of words.”
How, then, might this lead to cognitive deficits?
“The brain dedicates a lot of resources to hearing,” Dr. Lin said. “When the clarity of words is garbled, the brain gets a garbled message. It has to reallocate resources to hear at the expense of other brain functions.”
Thus, the overworked brain may lose “cognitive reserve,” the ability of healthy parts of the brain to take over functions lost by other parts.
Another mechanism may be the effects of social isolation. “A decline in social engagement and resulting loneliness is one of the most important determinants of health outcomes in older adults,” Dr. Lin said. Isolation has been linked to an increase in inflammation throughout the body, which in turn can result in age-related disorders like heart disease and dementia, Dr. Lin said.
How Proper Aids Help
Rose Marie Jewett, 83, of Janesville, Wis., who had experienced progressively worsening hearing loss for 40 years, had all but given up hope of hearing others speak or ever again enjoying music.
She said she could understand how hearing loss could lead to dementia, because she was “forgetful” when she did not hear what she should have heard.
It’s not that she forgot things; rather, she had never heard them to begin with, and the strain of constantly trying to piece things together was taking its toll.
“When you can’t hear anybody, you don’t pay attention,” Ms. Jewett said. “You shut yourself off from the world, you don’t think very well, your memory gets bad and you get kind of dull.”
But now it’s a whole new world for Ms. Jewett. Linda S. Remensnyder, an audiologist and founder of Hearing Associates in Illinois, taught her how to maximize her ability to hear clearly in social settings. She fitted Ms. Jewett with the right kind of hearing aids and with devices that allow her to hear clearly on the telephone, when watching television and in public settings that have been equipped with hearing loops.
A hearing loop, installed around the periphery of a room, is a thin copper wire that radiates electromagnetic signals. The signals can be picked up by a tiny receiver called a telecoil that is built into most hearing aids and cochlear implants. With the press of a tiny button on the aid, sound comes through to people with impaired hearing with even greater clarity than can be heard by someone with normal hearing.
Since 2009, Dr. Remensnyder said, hearing loops have been installed in about 1,000 public places, including museums, stores, banks, theaters, airports, sports arenas and other spaces that are challenging for the hearing-impaired.
“The public is misled into thinking that by getting two hearing aids, they’ll be able to hear everywhere,” she said. “Aids are just a small segment of the solution.”
Neither Dr. Lin nor Dr. Remensnyder can yet say whether improving auditory signals for the hearing-impaired will diminish or delay the development of dementia. That remains for a clinical trial to demonstrate. Meanwhile, Dr. Remensnyder said, it can “revolutionize” the lives of people with hearing difficulties, a virtue in itself.
Testing, Testing...Can You Hear Better Now?
Melinda Beck : WSJ : September 10, 2012
To many people, hearing loss represents another step in the dreaded march to old age. In fact, only about 20% of the 36 million Americans who could benefit from a hearing aid actually use one, according to the National Institute on Deafness and Other Communication Diseases
Many audio-speaker manufacturers are jumping into the hearing-aid market due to a recent FDA ruling that hearing-assist devices could be sold over-the-counter.
Now, a wave of new devices that are smaller, hipper and sold over-the-counter are trying to win over more consumers—and appeal to the growing number of younger people with hearing damage from loud music.
One upcoming model is a smartphone app. Others look like MP3 players or Bluetooth headsets. Some can barely be seen at all.
They're also less expensive: Traditional hearing aids can cost more than $4,000 per ear and aren't covered by Medicare or most insurers.
Often likened to "reading glasses" for the ears, many of the new models come preset to boost sounds in the high frequencies that most people lose first. That lets consumers bypass audiologists, who have traditionally controlled the market by giving hearing tests and selling custom-programmed hearing aids.
Technically, many of the new devices are "personal sound amplification products," or PSAPs, intended to help people with normal hearing better hear in situations like noisy restaurants and large gatherings, according to Food and Drug Administration guidelines issued in 2009. Hearing aids, by contrast, are medical devices for the hearing-impaired and subject to FDA approval, the agency says.
But the distinctions are blurring, with some PSAPs boasting the same technology that digital hearing aids offer for hundreds, not thousands, of dollars. Meanwhile, online retailers such as America Hears Inc. and Audicus are selling custom-programmed hearing aids at steep discounts direct to consumers when they send in their hearing-test results.
Amps for the Ears
Audiologists warn that consumers who skip the professional exam could damage their hearing further with PSAPs. They also may miss finding a treatable cause for their hearing problems, from excess earwax to an auditory tumor. But industry observers say the new versions could get more consumers to at least consider getting help.
"If friends and family are bugging you because you ask them to repeat themselves too often, and if you can't hear the TV without turning it up, a PSAP is a great way to address the problem initially," says David Copithorne, a marketing executive who writes the influential blog, HearingMojo.com. "You can buy a PSAP over the Internet, stick it in your ear, and see if it helps. For a lot of people it will."
Like millions of others, I have mild hearing loss but am not ready for a hearing aid. So I've been trying some of these alternatives. Here's what I found:
The most impressive new PSAP is the Able Planet Personal Sound AMP 2500, which debuts this week at AblePlanet.com. It is the size of a Cheerio and sits in the ear where it is virtually invisible. The company, known for its noise-canceling headphones, put the same Linx Audio technology into each tiny earpiece to reduce background noise while it amplifies frequencies that carry speech.
Say What?
If you answer yes to more than two of the following questions, experts recommend having your hearing evaluated by a certified audiologist:
"It's like having the smallest noise-canceling headphone in the world," says Able Planet Chairman and CEO Kevin Semcken. There is no volume control, but as the sound environment changes—say, the restaurant gets noisier—you can discreetly switch among four built-in programs by cupping your hand over your ear and tapping.
While trying the Able Planet in both ears for the past few weeks I said "What?" and "Huh?" much less often—to my family's delight. I didn't need to crank up the TV and even at a deafening pro football game, I could hear conversations easily. No one noticed I was wearing them.
The sound quality is as good as high-end hearing aids I've tried with less background noise and at a fraction of the price—$499 for one and $899 for the pair.
The Symphonix, made by RCA, looks like a small behind-the-ear hearing aid. A clear plastic tube links it to a tiny plastic dome that fits inside the ear canal. The earpiece has an on-off switch, a three-stage volume control and uses a rechargeable battery. It costs $299 at Radio Shack and other retailers, and you can adjust it to fit in the right or left ear. I tried it at the football game, at a party and while watching TV and it definitely amplified speech. But it also amplified many distracting background sounds as well. I sometimes heard feedback when I moved my head, but wiggling the dome deeper into my ear canal helped.
The MDHearingAid also sits behind the ear with a plastic dome in the ear canal. It is an FDA-approved hearing aid, but it is sold online and preprogrammed for typical mild to moderate hearing loss. "Hearing loss is a medical condition, but we don't want people going without help," says Sreekant Cherukuri, the Chicago otolaryngologist who designed it for patients who couldn't afford high-end hearing aids. The "Pro" model I tried felt more substantial than the Symphonix, was easier to adjust and had less feedback. It cost $180 for one; $329 for a pair.
Walker's Game Ear makes a variety of PSAPs for hunters who want to amplify the sound of prey in the woods, but need protection from loud noises like shotgun fire. The bass and treble can be adjusted for other tough hearing environments, like factories or lectures. I tried the behind-the-ear $209 Elite HD Pro at the office and on Manhattan sidewalks. Voices came in great, but so did passing sirens. (Mercifully, there was no gunfire.)
Later this year, Soundfest, a Needham, Mass., start-up, plans to offer a downloadable app called Real Clarity that will turn an iPhone or Android smartphone into a hearing-assistance device. The phone's built-in microphone will pick up sounds, the app will process the signals and send the enhanced sound through the user's earphones. The app, which will be priced at $10 to $20, will store a user's individual hearing profile, but it can be modified for different situations. "Our theory is that people know what they can and can't hear, and they can adjust it themselves," says Soundfest CEO David Duehren. A version planned for next year will work with a Bluetooth wireless receiver for $179.
The Panasonic JZ looks like an MP3 player with headphones, but it is designed for elderly people and others who would have trouble manipulating tiny hearing-aid batteries and buttons. Dials on the 2-by-2 inch device let users control volume and switch among four programs—from "standard" to "party"—displayed on an LCD screen. A true FDA-approved hearing aid, the JZ is individually programmed and sold through audiologists, for about $1,000.
A wide range of older, analog devices are available online for well under $100. Most simply boost all nearby sounds indiscriminately without enhancing speech or blocking noise, so they aren't for the hearing-impaired. I tried the Bell + Howell Silver Sonic XL, which looks like a Bluetooth headset and promises to amplify sounds up to 90 feet away for $19.99 each. It's good for eavesdropping on office mates but makes their keyboard clattering and snacking sounds so loud, it's impossible to get any work done.
Melinda Beck : WSJ : September 10, 2012
To many people, hearing loss represents another step in the dreaded march to old age. In fact, only about 20% of the 36 million Americans who could benefit from a hearing aid actually use one, according to the National Institute on Deafness and Other Communication Diseases
Many audio-speaker manufacturers are jumping into the hearing-aid market due to a recent FDA ruling that hearing-assist devices could be sold over-the-counter.
Now, a wave of new devices that are smaller, hipper and sold over-the-counter are trying to win over more consumers—and appeal to the growing number of younger people with hearing damage from loud music.
One upcoming model is a smartphone app. Others look like MP3 players or Bluetooth headsets. Some can barely be seen at all.
They're also less expensive: Traditional hearing aids can cost more than $4,000 per ear and aren't covered by Medicare or most insurers.
Often likened to "reading glasses" for the ears, many of the new models come preset to boost sounds in the high frequencies that most people lose first. That lets consumers bypass audiologists, who have traditionally controlled the market by giving hearing tests and selling custom-programmed hearing aids.
Technically, many of the new devices are "personal sound amplification products," or PSAPs, intended to help people with normal hearing better hear in situations like noisy restaurants and large gatherings, according to Food and Drug Administration guidelines issued in 2009. Hearing aids, by contrast, are medical devices for the hearing-impaired and subject to FDA approval, the agency says.
But the distinctions are blurring, with some PSAPs boasting the same technology that digital hearing aids offer for hundreds, not thousands, of dollars. Meanwhile, online retailers such as America Hears Inc. and Audicus are selling custom-programmed hearing aids at steep discounts direct to consumers when they send in their hearing-test results.
Amps for the Ears
Audiologists warn that consumers who skip the professional exam could damage their hearing further with PSAPs. They also may miss finding a treatable cause for their hearing problems, from excess earwax to an auditory tumor. But industry observers say the new versions could get more consumers to at least consider getting help.
"If friends and family are bugging you because you ask them to repeat themselves too often, and if you can't hear the TV without turning it up, a PSAP is a great way to address the problem initially," says David Copithorne, a marketing executive who writes the influential blog, HearingMojo.com. "You can buy a PSAP over the Internet, stick it in your ear, and see if it helps. For a lot of people it will."
Like millions of others, I have mild hearing loss but am not ready for a hearing aid. So I've been trying some of these alternatives. Here's what I found:
The most impressive new PSAP is the Able Planet Personal Sound AMP 2500, which debuts this week at AblePlanet.com. It is the size of a Cheerio and sits in the ear where it is virtually invisible. The company, known for its noise-canceling headphones, put the same Linx Audio technology into each tiny earpiece to reduce background noise while it amplifies frequencies that carry speech.
Say What?
If you answer yes to more than two of the following questions, experts recommend having your hearing evaluated by a certified audiologist:
- Do you have a problem hearing over the telephone?
- Do people complain that you turn the TV volume up too high?
- Do you have to strain to understand conversation?
- Do you have trouble hearing in a noisy background?
- Do you have dizziness, pain or ringing in your ears?
- Do you find yourself asking people to repeat themselves?
- Do many people you talk to seem to mumble (or not speak clearly)?
- Do you have trouble understanding the speech of women and children?
"It's like having the smallest noise-canceling headphone in the world," says Able Planet Chairman and CEO Kevin Semcken. There is no volume control, but as the sound environment changes—say, the restaurant gets noisier—you can discreetly switch among four built-in programs by cupping your hand over your ear and tapping.
While trying the Able Planet in both ears for the past few weeks I said "What?" and "Huh?" much less often—to my family's delight. I didn't need to crank up the TV and even at a deafening pro football game, I could hear conversations easily. No one noticed I was wearing them.
The sound quality is as good as high-end hearing aids I've tried with less background noise and at a fraction of the price—$499 for one and $899 for the pair.
The Symphonix, made by RCA, looks like a small behind-the-ear hearing aid. A clear plastic tube links it to a tiny plastic dome that fits inside the ear canal. The earpiece has an on-off switch, a three-stage volume control and uses a rechargeable battery. It costs $299 at Radio Shack and other retailers, and you can adjust it to fit in the right or left ear. I tried it at the football game, at a party and while watching TV and it definitely amplified speech. But it also amplified many distracting background sounds as well. I sometimes heard feedback when I moved my head, but wiggling the dome deeper into my ear canal helped.
The MDHearingAid also sits behind the ear with a plastic dome in the ear canal. It is an FDA-approved hearing aid, but it is sold online and preprogrammed for typical mild to moderate hearing loss. "Hearing loss is a medical condition, but we don't want people going without help," says Sreekant Cherukuri, the Chicago otolaryngologist who designed it for patients who couldn't afford high-end hearing aids. The "Pro" model I tried felt more substantial than the Symphonix, was easier to adjust and had less feedback. It cost $180 for one; $329 for a pair.
Walker's Game Ear makes a variety of PSAPs for hunters who want to amplify the sound of prey in the woods, but need protection from loud noises like shotgun fire. The bass and treble can be adjusted for other tough hearing environments, like factories or lectures. I tried the behind-the-ear $209 Elite HD Pro at the office and on Manhattan sidewalks. Voices came in great, but so did passing sirens. (Mercifully, there was no gunfire.)
Later this year, Soundfest, a Needham, Mass., start-up, plans to offer a downloadable app called Real Clarity that will turn an iPhone or Android smartphone into a hearing-assistance device. The phone's built-in microphone will pick up sounds, the app will process the signals and send the enhanced sound through the user's earphones. The app, which will be priced at $10 to $20, will store a user's individual hearing profile, but it can be modified for different situations. "Our theory is that people know what they can and can't hear, and they can adjust it themselves," says Soundfest CEO David Duehren. A version planned for next year will work with a Bluetooth wireless receiver for $179.
The Panasonic JZ looks like an MP3 player with headphones, but it is designed for elderly people and others who would have trouble manipulating tiny hearing-aid batteries and buttons. Dials on the 2-by-2 inch device let users control volume and switch among four programs—from "standard" to "party"—displayed on an LCD screen. A true FDA-approved hearing aid, the JZ is individually programmed and sold through audiologists, for about $1,000.
A wide range of older, analog devices are available online for well under $100. Most simply boost all nearby sounds indiscriminately without enhancing speech or blocking noise, so they aren't for the hearing-impaired. I tried the Bell + Howell Silver Sonic XL, which looks like a Bluetooth headset and promises to amplify sounds up to 90 feet away for $19.99 each. It's good for eavesdropping on office mates but makes their keyboard clattering and snacking sounds so loud, it's impossible to get any work done.
Can’t Hear in Noisy Places? It’s a Real Medical Condition
New studies of causes and treatments for deterioration in your brain’s ability to decode words in loud situations, also known as hidden hearing loss.
By Melinda Beck : WSJ : Sept. 26, 2016
Many people have trouble understanding conversations in noisy situations. Scientists are beginning to understand why.
The problem is sometimes called “hidden hearing loss”: Standard hearing tests don’t measure it, and sufferers are often told their hearing is normal. But the distress they feel struggling to discern what others are saying in crowded restaurants and business meetings is real.
Now there’s growing evidence that the causes of problems processing speech amid noise are different than the causes of problems hearing sound. Scientists believe exposure to loud noises can erode the brain’s ability to listen selectively and decode words, without causing traditional hearing damage. Difficulty understanding speech amid noise can set in long before traditional hearing loss.
“This is something we’ve recognized for a long time—and this research tells us why it’s happening,” says Anne Oyler, associate director for audiology at the American Speech-Language-Hearing Association. “Audiologists will have to start actively looking for this disorder.”
In a normal inner ear, sounds reach the brain when hair cells connect to nerve fibers via synapses, New research has found that exposure to loud noises can damage those synapses and disrupt the connection, long before the hair cells deteriorate. Hearing loss in adults is usually associated with damage to the tiny hair cells that line the inner ear and transfer sound signals to nerve fibers that lead to the brain. Aging, trauma and noise exposure can all cause those hair cells to deteriorate.
New research suggests that the synapses connecting the hair cells to nerve fibers are even more vulnerable and suffer permanent damage long before the hair cells deteriorate, bringing about the difficulties in selective listening.
While there aren’t immediate remedies, there is a glimmer of hope that the damage might be reversible. In a study published in Nature in April 2016, University of Michigan researchers were able to regenerate cochlear synapses in mice that had been exposed to loud noises by injecting them with neurotrophin-3, a protein that stimulates nerve growth.
In a landmark study in 2009, scientists at Massachusetts Eye and Ear Infirmary, led by otolaryngologist Charles Liberman, showed that mice exposed to loud noises lost up to 50% of those synapses even though their hair cells soon returned to normal.
Earlier in September, the same researchers showed that such damage occurs in humans as well. In a study published in the journal PLOS One, they compared a group of college-age music students regularly exposed to loud sounds for four to six hours with another group studying quieter subjects. Both groups tested normal on standard hearing tests and were equally able to understand words in quiet environments. But the high-risk students fared significantly worse on tests of understanding speech-in-noise. Tests with electrodes showed that their auditory nerves had a diminished response to sound stimulation compared with the low-risk group.
A new device called Soundhawk offers help to people who sometimes find it hard to hear—but aren't ready for a $3,000 hearing aid. Personal Tech columnist Geoffrey A. Fowler tests it out.“We believe this is the first evidence of hidden hearing loss in humans—but it is just a first step,” said Stéphane Maison, the study’s lead investigator. He and his colleagues are hoping to develop more precise tests to measure damage to cochlear synapses and diagnose it definitively.
Exactly how such damage, called cochlear synaptopathy, compromises the ability to understand speech amid noise isn’t fully understood. Dr. Liberman likens sound signals arriving at the brain to a high-resolution photo, with nerve connections like thousands of pixels creating a clear picture. If some of those nerve connections die, the brain gets a lower-resolution image and may lose the ability to distinguish where sounds are coming from and who is speaking.
The researchers think cochlear synaptopathy may help explain tinnitus, the persistent buzzing or ringing some people hear, as well as hyperacusis, which is an increased sensitivity to unpleasant sounds such as a baby crying or a siren. With fewer signals from the auditory nerve fibers reaching it, the brain may generate the buzzing to fill in the vacuum, or turn up its internal volume, making sounds that already loud become intolerable.
Audiologists are well aware that many patients have trouble understanding speech in noisy situations. “It’s the primary reason people walk in the door,” says Joanna Roufos, an audiologist with Manhattan Audiology in New York.
Besides giving standard hearing tests, many audiologists now use speech-in-noise tests that ask patients to pick out and repeat words or entire sentences amid a variety of background sounds and voices. There is little consensus, though, about what to do when such tests confirm a problem with understanding speech in noise. Many factors, including aging, cognitive ability, memory and conventional hearing loss, all play a role. Some patients are sent for an evaluation of an auditory-processing disorder, although such specialists may be more accustomed to dealing with children.
“The jury is still out as to how hidden hearing loss manifests in humans and how we might diagnose it,” says James W. Hall III, an expert in auditory processing disorders at Salus University in Elkins Park, Pa. “We don’t have enough information yet for it to be part of routine diagnosis of hearing problems.”
Many patients who have speech-in-noise difficulties also have traditional hearing loss. Audiologists say both can be improved with hearing aids, especially newer models with directional microphones and technology that damps background noise.
But hearing aids can’t return hearing to normal, experts caution. “The number one complaint of people who wear hearing aids is that they have trouble hearing in noise, and that’s not going to change,” says Dr. Oyler.
A variety of assistive listening devices can also help patients hear what they want to hear in specific situations. With a personal frequency-modulation (FM) system, for example, the person speaking uses a microphone and the listener wears a wireless Bluetooth receiver. Other devices transmit the audio feeds in theaters, concerts, meetings, churches or even home TV directly to listeners without amplifying background sounds.
Many people who struggle with speech in noise are reluctant to take such remedial steps, however. Hearing-aid companies often say it takes people seven years, on average, to seek treatment after they first suspect a hearing issue.
Audiologists urge sufferers to get evaluated, even if the solutions aren’t perfect. “Some people feel they can fake their way through conversations,” says Sarah Sydlowski, an audiologist at Cleveland Clinic and board member of the American Academy of Audiology. “But it can be extremely taxing to go through a busy workday and be constantly struggling to understand.”
The Epley Maneuver
VESTIBULAR REHABILITATION
Garineh Goshdigian, PT, MSPT
Mount Auburn Hospital Rehabilitation Services
625 Mt Auburn Street, First Floor,
Cambridge, MA 02138
617-499-5011
Treatment of vestibular disorders
include
maneuvers and exercises that aim to promote vestibular compensation, habituation, or adaptation of the vestibule-ocular and vestibule-spinal reflexes
Mount Auburn Hospital Rehabilitation Services
625 Mt Auburn Street, First Floor,
Cambridge, MA 02138
617-499-5011
Treatment of vestibular disorders
include
maneuvers and exercises that aim to promote vestibular compensation, habituation, or adaptation of the vestibule-ocular and vestibule-spinal reflexes
Confident Strides Program
Comprehensive approach to treating gait and balance problems run by Mount Auburn Hospital Rehabilitation Services at two locations
- 725 Concord Avenue, Suite 5100, Cambridge, MA 02138
- Tel # 617-499-6760
- 625 Mt Auburn Street, Suite 101, Cambridge, MA 02138 Tel # 617-499-5011
HEARING TESTING
Audiology Services Inc.
90 Concord Avenue, 2nd Floor,
Belmont, MA 02478
617-484-8700
www.audiologyservicesinc.com
[email protected]
90 Concord Avenue, 2nd Floor,
Belmont, MA 02478
617-484-8700
www.audiologyservicesinc.com
[email protected]