- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
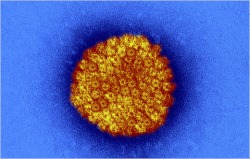
HERPES
Alternative Names
Herpes - genital; Herpes simplex - genital; Herpesvirus 2; HSV-2
Causes
Genital herpes is caused by two viruses:
- Herpes simplex virus type 2 (HSV-2)
- Herpes simplex virus type 1 (HSV-1)
Herpes simplex virus type 1 (HSV-1) most often causes herpes infections of the mouth and lips (commonly called cold sores or fever blisters). HSV-1 can spread from the mouth to the genitals during oral sex.
Herpes simplex virus (HSV) is spread from one person to another during sexual contact. You may be infected with herpes when your skin, vagina, penis, or mouth comes into contact with someone who already has herpes.
Herpes is most likely to be transmitted by contact with the skin of an infected person who has visible sores, blisters, or a rash (an active outbreak), but you can also catch herpes from an infected person's skin when they have NO visible sores present (and the person may not even know that he or she is infected), or from an infected persons mouth (saliva) or vaginal fluids.
Because the virus can be spread even when there are no symptoms or sores present, a sexual partner who has been infected with herpes in the past but has no active herpes sores can still pass the infection on to others.
Genital HSV-2 infections is more common in women (approximately 1 of every 4 women is infected) than it is in men (nearly 1 of every 8 men is infected).
Symptoms »
Many people with HSV-2 infection never have sores, or they have very mild symptoms that they do not even notice or mistake for insect bites or another skin condition.
If signs and symptoms do occur during the first outbreak, they can be quite severe. This first outbreak usually happens within 2 weeks of being infected.
Generalized or whole-body (systemic) symptoms may include:
- Decreased appetite
- Fever
- General sick feeling (Malaise)
- Muscle aches in the lower back, buttocks, thighs, or knees
- In women: on the outer vaginal lips (labia), vagina, cervix, around the anus, and on the thighs or buttocks
- In men: on the penis, scrotum, around the anus, on the thighs or buttocks
- In both sexes: on the tongue, mouth, eyes, gums, lips, fingers, and other parts of the body
- Before the blisters appear, the person may feel the skin tingling, burning, itching, or have pain at the site where the blisters will appear
- When the blisters break, they leave shallow ulcers that are very painful. These ulcers eventually crust over and slowly heal over 7 - 14 days or more
- Enlarged and tender lymph nodes in the groin during an outbreak
- Painful urination
- Women may have vaginal discharge or, occasionally, be unable to empty the bladder and require a urinary catheter
Once a person is infected, however, the virus hides within nerve cells and remains in the body. The virus can remain "asleep" (dormant) for a long period of time (this is called latency).
The infection can flare-up or reactivate at any time. Events that can trigger latent infection to become active and bring on an outbreak include:
- Fatigue
- Genital irritation
- Menstruation
- Physical or emotional stress
- Trauma
Exams and Tests »
Tests can be done on skin sores or blisters to diagnose herpes. These tests are most often done when someone has a first outbreak and when a pregnant women develops genital herpes symptoms.
- Culture of fluid from a blister or open sore may be positive for herpes simplex virus. The herpes simplex virus can in the culture in 2-3 days. It is most useful during the first outbreak.
- A test called PCR performed on fluid from a blister shows small amounts of DNA. It is the most accurate test to tell whether the herpes virus is present in the blister.
- Blood tests check for antibody levels to the herpes virus. These blood tests can identify whether someone has ever been infected with the herpes virus, even between outbreaks. It may be positive even if they've never had an outbreak.
Genital herpes cannot be cured. However, antiviral medication can relieve pain and discomfort during an outbreak by healing the sores more quickly. These drugs appear to help during first attacks more than they do in later outbreaks. Medicines used to treat herpes include acyclovir, famciclovir, and valacyclovir.
For repeat outbreaks, start the medication as soon as the tingling, burning, or itching begins, or as soon as you notice blisters.
People who have many outbreaks may take these medications daily over a period of time. This can help prevent outbreaks or shorten their length. It can also reduce the chance of giving herpes to someone else.
Pregnant women may be treated for herpes during the last month of pregnancy to reduce the chance of having an outbreak at the time of delivery. If there is an outbreak around the time of delivery, a C-section will be recommended to reduce the chance of infecting the baby.
Possible side effects from herpes medications include:
- Fatigue
- Headache
- Nausea and vomiting
- Rash
- Seizures
- Tremor
- Do NOT wear nylon or other synthetic pantyhose, underwear, or pants. Instead, wear loose-fitting cotton garments
- Gentle cleansing with soap and water is recommended.
- Taking warm baths may relieve the pain (afterward, keep the blisters dry)
Outlook (Prognosis)
Once you are infected, the virus stays in your body for the rest of your life. Some people never have another episode, and others have frequent outbreaks.
In most outbreaks, there is no obvious trigger. Many people, however, find that attacks of genital herpes occur with the following conditions:
- Fatigue
- General illness (from mild illnesses to serious conditions, such as operations, heart attacks, and pneumonia)
- Immunosuppression due to AIDS or medication such as chemotherapy or steroids
- Menstruation
- Physical or emotional stress
- Trauma to the affected area, including sexual activity
Possible Complications
Pregnant women who have an active herpes infection on their genitals or in their birth canal when they deliver may pass the infection to their newborn infant.
- The risk of passing the infection to the baby is highest if the mom first becomes infected with herpes during pregnancy. Babies of women who become infected during pregnancy are at risk for premature birth. The baby may develop develop brain infection (meningitis, encephalitis) , chronic skin infeciton, severe developmental delays, or death.
- The risk for severe infection in the baby is lower in recurrent outbreaks, with the highest risk in women experiencing an outbreak at the time of delivery.
- Women with a history of herpes but who only have occasional or no outbreaks rarely transmit the infection to their babies.
Someone with an active herpes infection who has sexual contact with someone who is HIV positive is more likely to contract HIV infection themselves.
When to Contact a Medical Professional
Call for an appointment with your health care provider if you have any symptoms of genital herpes, or if you develop fever, headache, vomiting, or widespread symptoms during or after an outbreak of herpes. Also call if you are unable to urinate.
Prevention
The best way to avoid getting genital herpes is to avoid all sexual contact, including oral sex. Next best is being in a long-term, mutually monogamous relationshipw with someone who has been tested and is not, and never has been, infected with herpes.
Condoms remain the best way to protect against catching genital herpes during sexual activity with someone who is infected. Using a condom correctly and consistently will help prevent the spread of the disease.
- Only latex condomes will work to prevent infection. Animal membrane (sheepskin) condoms won't work because the virus can go right through them.
- The female condom has been tested and shown to reduce the risk of trasmitting herpes, as well.
- A latex condom should be used during ALL sexual contact, even if the infected person does not have any sores or blisters at that time.
Vaccines against herpes have been developed but are still experimental.
Overcoming the Stigma of Herpes
By Eric Sabo : NY Times Article : May 26, 2010
Genital herpes may be the largest epidemic no one wants to talk about. An estimated one out of five Americans over the age of 12 quietly harbor a meek but distressing virus that can cause painful and ugly outbreaks on areas that seldom see the light of day.
The silence has as much to do with the disease as concerns over what it can do to a budding romance. Symptoms, at least for most, are either nonexistent or so mild that it’s often nearly impossible to notice an infection. The main harm in suffering herpes, as many will attest to, comes from the dread of telling your partner the truth.
“Herpes has a stigma attached to it that even H.I.V. doesn’t have anymore,” said Dr. Anna Wald, a virologist at the University of Washington. “It’s very rare to get people to talk about it as openly.”
But a new test — which doctors use to detect herpes in the blood rather than wait for symptoms to appear — is pushing the taboo virus into the spotlight as it becomes easier to know your status and, ideally, take steps to protect others.
There is still no cure for avoiding the delicate topic with your partner. The disease is potentially contagious before or after noticeable outbreaks, and condoms are less protective than against AIDS, since genital herpes also spreads through skin contact.
So it’s often left to public health officials to spread the word: Be honest about having herpes, they say, to keep it from spreading in the bedroom.
A study by Dr. Wald found that such openness clearly helps, at least for a time. Out of 200 people with herpes, those who revealed their diagnosis were able to keep partners free of the disease for about nine months on average, compared to the two months it took when left secret.
Couples who share this information often agree to use condoms, hold off on sex during flare-ups, and avoid skin-to-skin contact around the genital region, which all reduce the risk of transmitting herpes. Some may take prescription drugs that, in addition to relieving symptoms, block some of the viral shedding that causes infections.
“Maybe it’s not even a conscious decision, but people do things differently when they know,” Dr. Wald said.
The push for greater openness has become more urgent as researchers suspect that herpes is adding to the spread of H.I.V. and AIDS. The virus responsible for most outbreaks of genital herpes, herpes simplex type 2, blunts the immune response and leads to higher levels of H.I.V. in the blood, raising the chance of transmitting both infections.
“Herpes is like AIDS in that everyone thinks of it as someone else’s disease,” said Dr. Peter Leone, an associate professor at the University of North Carolina Medical School and director of the state’s sexually transmitted disease program. “But guess what, if you’re sexually active, you’re at risk for herpes.”
Still, getting people to talk openly about the virus remains an uphill battle. Only about half of those knowingly infected with genital herpes divulge their status to regular sex partners. And when it comes to casual hookups, disclosure nosedives to nearly 20 percent.
Medical groups also remain leery of widespread screening for herpes, fearing that a small margin of error on the tests could result in a flood of misdiagnosed patients. The latest blood tests are wrong 2 to 4 percent of the time.
Even with the correct diagnosis, those who find out they have genital herpes through a random screening test often take the news the hardest, according to studies led by Dr. Kenneth Fife of Indiana University.
“It’s pretty tough to deal with when you’re not prepared,” Dr. Fife said.
And after all that trouble, there’s no guarantee that the virus can be stopped. Herpes sheds on areas of skin that condoms fail to protect, regardless of whether symptoms are visible or not, and at any time. The virus appears most contagious during the first few hours of flare-ups, researchers now believe. But there is no way to predict when these outbreaks will occur, and drugs are less effective at blocking viral shedding during such short, potent attacks.
Dr. Wald says she gets calls at least once a month from people asking if scientists created a better herpes test to “use on a Saturday night to see if it’s safe for them to go out.” Unfortunately the answer is no, but the disease does not inevitably jump from one person to the next, nor is there any long-term bodily harm from herpes infections. Genital flare-ups come and go, then largely subside after the first year.
That’s one reason why experts advise it’s better to be upfront about herpes status at first, rather than watching a relationship fall apart after an outbreak occurs.
“People are lucky in a way when they don’t know their symptoms,” Dr. Wald said. “But they may infect a partner, who may be extremely symptomatic.”
Questions and Answers :
Understanding Genital Herpes
By Eric Sabo : NY Times Article : May 27, 2010
Dr. Peter A. Leone is an associate professor at the University of North Carolina School of Medicine and Public Health. He also directs the H.I.V./sexually transmitted disease prevention program for the state of North Carolina and serves on the National Coalition of STD Directors, a group of public health officials who promote awareness of sexually transmitted diseases.
Q: People are more worried about getting H.I.V./AIDS than genital herpes. Should we be paying more attention to herpes?
A: H.I.V./AIDS is viewed as a lethal disease, and herpes isn’t, so many have ignored it. The reason why we should focus on herpes now is that the relationship between herpes and H.I.V. is significant. Although people don’t die from herpes, there is a synergy between these two infections. If a person has genital herpes due to the herpes type 2 virus, their risk of acquiring H.I.V. is much higher than if they didn’t have herpes. And a person who has both H.I.V. and herpes 2 is more likely to transmit both infections.
These two epidemics are linked, and because herpes has been pushed to the side, we haven’t paid enough attention to it. There are 60 million adults in the United States alone who have herpes, and we have a million new cases a year. It’s a big epidemic.
Q:The herpes 2 virus is the main cause of genital outbreaks, but many infections are now being caused by herpes 1. How dangerous is a virus that typically causes harmless cold sores around the mouth?
A: Herpes type 1 is not associated with H.I.V. acquisition. The reason is that these viruses sort of adapt to each site, so herpes 1 is more likely to shed around the mouth and not as likely as to reactivate in the genital tract. Herpes type 2, on the other hand, is much more likely to shed and reactivate in the genital tract. As a result, there’s more of a risk of co-infection with H.I.V. from herpes 2.
But if a woman acquires genital herpes from either herpes 1 or 2 during pregnancy, the risk of having a severe outcome for the baby is high.
Q: How common is it for pregnant woman to have complications because of genital herpes?
A: It’s a pretty rare event, but women who acquire herpes during pregnancy can risk transmitting a fatal infection to the baby. There’s been a lot of debate of whether we screen all pregnant women and there’s been no consensus. It’s one of those things that’s often completely missed, but when it happens, it can be devastating.
Q: Is it possible to tell which type of herpes virus people are infected with?
A: The clinical presentation for herpes 1 and 2 are no different on the genital tract. You can’t distinguish them by how the lesions look or the severity of the initial outbreak. Herpes 2 is more likely to recur, but the symptoms are indistinguishable at first.
A misconception is that people think you can only transmit herpes from the mouth to the genitals when you have a cold sore, or an outbreak. That’s not true. You can have asymptomatic shedding from the mouth. We’re seeing a lot more oral transmission from the mouth to the genital track. About 30 to 50 percent of new genital herpes infections are from herpes 1. All cases should be confirmed by blood tests.
Q: Many doctors are not ready to endorse more widespread screening for genital herpes. What’s the hesitancy?
A: In pregnant women, there is concern that it would lead to unnecessary interventions and Caesarean sections to prevent transmission to the baby. And we’re still hung up about sex and herpes. People and doctors are uncomfortable talking about it and discussing testing with patients.
Some would say there’s not a whole lot to worry about because there’s not much you can do with herpes. It’s sort of this forgotten and neglected infection. But men who have sex with men are at an obviously high risk for H.I.V., and herpes is very prevalent. For certain groups, such as gay men, or men or women who visit a sexually transmitted disease clinic or who have another sexually transmitted disease, screening for herpes should be a routine part of their health care.
But it doesn’t take a lot of partners to acquire herpes: the average is three to four lifetime partners. If you’re an African-American woman, the prevalence rate is 50 percent. So, I think all sexually active adults should consider getting tested.
Q: One of the problems in detecting herpes is that many people don’t notice the symptoms. How can you tell if you have the disease, outside of getting a blood test?
A: The classic way to tell you had herpes was sores or ulcers on the genital area that were painful and lasted a few days, and then went away. But our understanding of herpes has increased as the technology has improved. What we’re finding now is that most cases do not fit this classic description.
The typical, common way herpes presents is mild irritation that may be mistaken for trauma to the genital area. Most people miss these signs, and most clinicians aren’t looking for it. But what we see is that most will have four to six of these outbreaks in the first year of infection, which decreases over time.
Q: How effective are condoms for protecting against genital herpes?
A: Condoms work best in preventing sexually transmitted diseases that are spread through ejaculate and vaginal fluid. But any skin-to-skin contact puts you at risk for herpes. Since most people are not covered in latex when having sex, condoms are not as protective as we see with H.I.V., chlamydia or gonorrhea.
Still, using a condom can reduce herpes transmission by 50 percent, and that’s true for men and women. It’s not a home run, but it does work. There’s been a tendency to say that it’s either all are none. Unless you wear condoms 100 percent of the time, there’s no benefit. That’s not true. Wearing condoms 25 percent of the time can reduce your risk by half.
Q: How contagious is genital herpes from just skin-to-skin contact?
A: Any skin-to-skin contact from the genital area is sufficient. The area that is covered by, say, your boxer shorts is where the virus sheds. Even if you’re infected in one site, you can shed from multiple sites at different times.
About 50 percent of shedding is clustered around an outbreak, so you have a higher risk seven days before, or seven days after. The problem is you don’t know when you’re going to have an outbreak. And more sophisticated studies show that shedding happens all the time.
There is still no way of predicting when herpes will spread, but we do know that recently infected people have a greater risk of shedding and transmitting herpes. So I think we need to redouble our efforts in identifying people who are newly infected.
Q: Three medications can help relieve herpes symptoms, but do we know how good they are at preventing the spread of genital herpes?
A: There has been only one study showing that a drug could reduce transmission. This involved heterosexual couples where one person had herpes and the other didn’t. They had been together, on average, for a couple of years. Daily suppressive therapy with Valtrex reduced the risk of transmission by 48 percent, on top of what our standard has been, which is using condoms, knowing your status and abstaining from sex around the time of an outbreak.
It’s the only study that we know has shown a benefit. But we certainly don’t think any of three drugs would make things worse. They should all reduce transmission because they all reduce shredding.
Q:. Still, is it just a matter of time before an uninfected partner gets herpes from a boyfriend or girlfriend who has the virus, especially the longer they date?
A: It’s not inevitable. The overall transmission rate is perhaps 6 to 10 percent a year. The average time for transmission in a new couple, where one has it and the other doesn’t, is about two months. So, if you’re going to transmit, it’s more likely to be early, not later.
This is important because there’s a tendency for folks to say, ”Well, let’s see how things work out, I don’t need to disclose this to my new partner because they won’t want to have sex with me, or they may tell others, so I’ll avoid it.” But you need to know your status and have open dialogue before you have sex, not after.
Giving Your Partner Herpes
By the NY Times : June 18, 2010
The highest risk of transmitting the herpes virus is during an outbreak. Can someone infected with herpes continue to have sex without giving it to their partner? Do cold sores, which are almost always caused by herpes simplex virus type 1 (HSV-1), protect against genital herpes caused by herpes simplex virus type 2? Can someone be infected with both types of herpes viruses?
Those are among the questions recently posed by readers of the Consults blog. Dr. Peter Leone, an expert on sexually transmitted diseases and associate professor at the University of North Carolina School of Medicine and Public Health, responds.
What’s My Risk of Spreading Herpes?
Q. I found out that I have herpes simplex type 2 (HSV-2) about a month and a half ago. My primary partner, who is male, has been tested twice since then, and both results have been negative. We were fluid-bonded [exposed to each other's bodily fluids] and had plenty of unprotected sex between my most recent negative result and last month’s positive one. What are the rates of transmission in a serologically discordant couple where the female partner has HSV-2?
I’ve read that it’s:
Stella, Chicago
A. Dr. Peter Leone responds:
Transmission of HSV-2 to an uninfected partner depends on many different factors, and it is difficult to give precise figures. Studies involving discordant couples, in which one partner has HSV-2 and the other does not, introduce various biases. Discordant couples, for example, have not transmitted the virus between them and are encouraged to use condoms and take other preventive measures. Given these caveats, here’s what we can say:
Can You Be Infected With Both Types of Herpes?
Q. Can a person have both HSV-1 and HSV-2? And what would it do to your chances of contracting H.I.V.? Or hepatitis C, for that matter?
cardo, Chico, Calif.
A. Dr. Peter Leone responds:
Yes. About 10 percent of adults in the United States have both HSV-1 and HSV-2. Of those with HSV-2, about 40 percent are co-infected with HSV-1.
HSV-2 increases the risk for H.I.V. acquisition. Someone infected with HSV-2 has two to five times greater risk of acquiring H.I.V. through sexual intercourse compared with someone who is not infected with HSV-2. HSV-1 does not increase the risk of H.I.V.
Your question about whether herpes increases the risk of contracting hepatitis C is an interesting one. The biggest risk for hepatitis C is through sharing needles while injecting drugs. But hepatitis C can also be sexually transmitted, and it appears that the risk may be increased in women and in men who have sex with men who are also infected with HSV-2.
Do Cold Sores Protect Against Genital Herpes?
Q. As a kid, I had oral herpes (painful sores on inside of mouth, etc.), and then many years later I dated a girl for two years who had herpes, and I never caught it (though we often, though not always, used condoms). I’m long since married now, but I’ve always wondered, does having had oral herpes make one immune to contracting genital herpes?
Nathan, NYC
A. Dr. Peter Leone responds:
Cold sores are almost always – 98 percent of the time — caused by HSV-1. Having HSV-1 infection may make it more difficult to acquire HSV-2 infection, but, at best, offers only partial immunity.
If someone with HSV-1 acquires HSV-2, he or she is likely to have a mild first outbreak of HSV-2 — or there may not be any symptoms at all. Nearly 40 percent of individuals infected with HSV-2 are also infected with HSV-1. Maybe you don’t have HSV-2 infection, but the only way to know for sure is to get a blood test for HSV-2.
By the NY Times : June 18, 2010
The highest risk of transmitting the herpes virus is during an outbreak. Can someone infected with herpes continue to have sex without giving it to their partner? Do cold sores, which are almost always caused by herpes simplex virus type 1 (HSV-1), protect against genital herpes caused by herpes simplex virus type 2? Can someone be infected with both types of herpes viruses?
Those are among the questions recently posed by readers of the Consults blog. Dr. Peter Leone, an expert on sexually transmitted diseases and associate professor at the University of North Carolina School of Medicine and Public Health, responds.
What’s My Risk of Spreading Herpes?
Q. I found out that I have herpes simplex type 2 (HSV-2) about a month and a half ago. My primary partner, who is male, has been tested twice since then, and both results have been negative. We were fluid-bonded [exposed to each other's bodily fluids] and had plenty of unprotected sex between my most recent negative result and last month’s positive one. What are the rates of transmission in a serologically discordant couple where the female partner has HSV-2?
I’ve read that it’s:
- 4 percent in couples who don’t use barriers but avoid sex during outbreaks, and where the woman is not on antiviral suppressive therapy.
- 2 percent in couples who use condoms and no antivirals.
- 1 percent in couples who use both condoms and daily antivirals.
Stella, Chicago
A. Dr. Peter Leone responds:
Transmission of HSV-2 to an uninfected partner depends on many different factors, and it is difficult to give precise figures. Studies involving discordant couples, in which one partner has HSV-2 and the other does not, introduce various biases. Discordant couples, for example, have not transmitted the virus between them and are encouraged to use condoms and take other preventive measures. Given these caveats, here’s what we can say:
- Women are more likely to acquire HSV-2 from an infected male partner then men are from women. On average, the risk for women acquiring HSV-2 sexually from an infected partner is about 10 percent per year, though there is a large range — from 7 percent to 31 percent — in different studies.
- For uninfected men, the risk of sexually acquiring HSV-2 from an infected woman is about 4 percent per year.
- Having HSV-1 infection may lower the risk of acquiring HSV-2 sexually, but studies on this provide conflicting results.
- Condoms reduce the risk of transmission by about 30 percent, and daily suppressive therapy reduces the risk of transmission by about 48 percent, studies show. Using condoms and taking daily suppressive therapy reduces the risk even further than either measure alone, though studies were not large enough to provide reliable numbers.
- Unfortunately, there is no available data on the rate of transmission for same-sex couples.
Can You Be Infected With Both Types of Herpes?
Q. Can a person have both HSV-1 and HSV-2? And what would it do to your chances of contracting H.I.V.? Or hepatitis C, for that matter?
cardo, Chico, Calif.
A. Dr. Peter Leone responds:
Yes. About 10 percent of adults in the United States have both HSV-1 and HSV-2. Of those with HSV-2, about 40 percent are co-infected with HSV-1.
HSV-2 increases the risk for H.I.V. acquisition. Someone infected with HSV-2 has two to five times greater risk of acquiring H.I.V. through sexual intercourse compared with someone who is not infected with HSV-2. HSV-1 does not increase the risk of H.I.V.
Your question about whether herpes increases the risk of contracting hepatitis C is an interesting one. The biggest risk for hepatitis C is through sharing needles while injecting drugs. But hepatitis C can also be sexually transmitted, and it appears that the risk may be increased in women and in men who have sex with men who are also infected with HSV-2.
Do Cold Sores Protect Against Genital Herpes?
Q. As a kid, I had oral herpes (painful sores on inside of mouth, etc.), and then many years later I dated a girl for two years who had herpes, and I never caught it (though we often, though not always, used condoms). I’m long since married now, but I’ve always wondered, does having had oral herpes make one immune to contracting genital herpes?
Nathan, NYC
A. Dr. Peter Leone responds:
Cold sores are almost always – 98 percent of the time — caused by HSV-1. Having HSV-1 infection may make it more difficult to acquire HSV-2 infection, but, at best, offers only partial immunity.
If someone with HSV-1 acquires HSV-2, he or she is likely to have a mild first outbreak of HSV-2 — or there may not be any symptoms at all. Nearly 40 percent of individuals infected with HSV-2 are also infected with HSV-1. Maybe you don’t have HSV-2 infection, but the only way to know for sure is to get a blood test for HSV-2.