- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Leg Cramps
Many people have an occasional leg cramp. However, they occur frequently in some people. They are more common in older people. About 1 in 3 people over the age of 60, and about half of people over the age of 80 have regular leg cramps. About 4 in 10 people who have leg cramps have at least three per week. They occur every day in some cases.
What causes leg cramps?
Unknown cause (idiopathic leg cramps)
In most cases the cause is not known. One theory is that cramps occur when a muscle that is already in a shortened position is stimulated to contract. As the muscle is already shortened, to contract further may cause the muscle to go into spasm. This commonly happens at night in bed as the natural position we lie in is with the knees slightly bent (flexed), and with feet pointing slightly downwards. In this position the calf muscle is relatively shortened and prone to cramps. This theory explains why stretching exercises may cure the problem.
Secondary causes
In some cases, the cramps may be a symptom of another condition or problem. For example:
Note: leg cramps are different to a condition called restless legs syndrome. In this condition the legs can be uncomfortable, you feel creeping sensations in the legs, and it is relieved by walking about. See separate leaflet called 'Restless Legs Syndrome' for details.
What is the treatment for a leg cramp?
Stretching and massaging the affected muscle (usually a calf muscle) can usually relieve an attack of cramp. Most cramps soon ease off. Painkillers are not usually helpful for a sudden attack of cramp. However, a painkiller such as paracetamol may help to ease muscle discomfort and tenderness that sometimes persists for up to 24 hours after a cramp has gone.
What are the options for preventing leg cramps?
If cramps do not occur often, then no particular treatment is usually needed. However, if you have frequent cramps, you may wish to consider ways of preventing them.
Consider your medication (where appropriate) or other conditions
Tell your doctor if you take any of the medicines listed above. It may be causing the leg cramps, or making them recur more often. Alternative medicines may be available. Also, if you have other symptoms apart from cramps, see your doctor who may examine you or do some checks to rule out a secondary cause for the cramps.
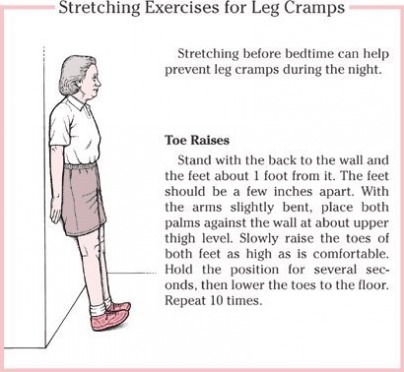
Stretching exercises
Stretching exercises are commonly advised. However, there is a lack of good research evidence to prove that it works. One research study concluded that stretching exercises did reduce the number and severity of cramps, but another study did not confirm this. So, as it may help, it is worth trying if you are able to do the exercises. If it works, you will not need any tablets to prevent the leg cramps.
At first, do stretching exercises of affected muscles for about five minutes, three times a day. Do the last exercise shortly before bedtime. If the cramps ease off, you may then only need to do the exercise once or twice a day to keep the cramps away.
To stretch calf muscles, stand about 60-90 cm from a wall. Then, keeping the soles of your feet flat on the floor, bend forward and lean on the wall. You will feel your calf muscles stretch. Do this several times, each time for as long as you can manage.
Posture of the legs when resting in bed
Positions which prevent the calf muscle from shortening when you are asleep may help. The following are not proven treatments (from research studies), but some experts believe that they help to prevent cramps.
Quinine was a common treatment and it often reduced the number and severity of leg cramps, but the FDA has pulled its use for leg cramps.
Other treatments
Other medicines have been suggested as possible treatments for leg cramps. These include: naftidrofuryl, vitamin E, verapamil, diltiazem, painkillers, aspirin, orphenadrine, magnesium, calcium, and sodium chloride. TENS machines have also been suggested as a possible treatment. So far there is little research evidence to prove that these treatments work well. Your doctor may suggest trying one if all else fails.
What causes leg cramps?
Unknown cause (idiopathic leg cramps)
In most cases the cause is not known. One theory is that cramps occur when a muscle that is already in a shortened position is stimulated to contract. As the muscle is already shortened, to contract further may cause the muscle to go into spasm. This commonly happens at night in bed as the natural position we lie in is with the knees slightly bent (flexed), and with feet pointing slightly downwards. In this position the calf muscle is relatively shortened and prone to cramps. This theory explains why stretching exercises may cure the problem.
Secondary causes
In some cases, the cramps may be a symptom of another condition or problem. For example:
- Some medicines can cause cramps as a side-effect, or make cramps occur more often. These include: diuretics ('water tablets'), nifedipine, cimetidine, salbutamol, terbutaline, lithium, clofibrate, penicillamine, morphine (withdrawal), phenothiazines, and nicotinic acid.
- Over-exertion of muscles.
- Dehydration.
- Conditions that cause alterations in the balance of salts in the bloodstream (such as a high or low sodium or potassium level).
- Some people who have renal (kidney) dialysis get leg cramps.
- Pregnancy - usually in the later stages.
- An untreated under-active thyroid gland (hypothyroidism)
- Peripheral arterial disease (PAD - narrowing of the leg arteries which causes poor circulation).
- Cirrhosis of the liver (is a rare cause)
- Lead poisoning.
- Sarcoidosis.
- Rare disorders of nerves.
- Excess alcohol.
Note: leg cramps are different to a condition called restless legs syndrome. In this condition the legs can be uncomfortable, you feel creeping sensations in the legs, and it is relieved by walking about. See separate leaflet called 'Restless Legs Syndrome' for details.
What is the treatment for a leg cramp?
Stretching and massaging the affected muscle (usually a calf muscle) can usually relieve an attack of cramp. Most cramps soon ease off. Painkillers are not usually helpful for a sudden attack of cramp. However, a painkiller such as paracetamol may help to ease muscle discomfort and tenderness that sometimes persists for up to 24 hours after a cramp has gone.
What are the options for preventing leg cramps?
If cramps do not occur often, then no particular treatment is usually needed. However, if you have frequent cramps, you may wish to consider ways of preventing them.
Consider your medication (where appropriate) or other conditions
Tell your doctor if you take any of the medicines listed above. It may be causing the leg cramps, or making them recur more often. Alternative medicines may be available. Also, if you have other symptoms apart from cramps, see your doctor who may examine you or do some checks to rule out a secondary cause for the cramps.
Stretching exercises
Stretching exercises are commonly advised. However, there is a lack of good research evidence to prove that it works. One research study concluded that stretching exercises did reduce the number and severity of cramps, but another study did not confirm this. So, as it may help, it is worth trying if you are able to do the exercises. If it works, you will not need any tablets to prevent the leg cramps.
At first, do stretching exercises of affected muscles for about five minutes, three times a day. Do the last exercise shortly before bedtime. If the cramps ease off, you may then only need to do the exercise once or twice a day to keep the cramps away.
To stretch calf muscles, stand about 60-90 cm from a wall. Then, keeping the soles of your feet flat on the floor, bend forward and lean on the wall. You will feel your calf muscles stretch. Do this several times, each time for as long as you can manage.
Posture of the legs when resting in bed
Positions which prevent the calf muscle from shortening when you are asleep may help. The following are not proven treatments (from research studies), but some experts believe that they help to prevent cramps.
- using a pillow to prop the feet up in bed while sleeping on your back.
- hanging the feet over the end of the bed while sleeping on your front.
- keeping blankets loose at the foot of the bed to prevent toes and feet from pointing downwards during sleep.
Quinine was a common treatment and it often reduced the number and severity of leg cramps, but the FDA has pulled its use for leg cramps.
Other treatments
Other medicines have been suggested as possible treatments for leg cramps. These include: naftidrofuryl, vitamin E, verapamil, diltiazem, painkillers, aspirin, orphenadrine, magnesium, calcium, and sodium chloride. TENS machines have also been suggested as a possible treatment. So far there is little research evidence to prove that these treatments work well. Your doctor may suggest trying one if all else fails.

Millions With Leg Pain Have Peripheral Artery Disease
Jane E. Brody : NY Times : April 11, 2016
More than eight million older Americans have a condition that can cause leg pain when they walk even short distances. Yet half of those who have the condition don’t know it and consequently don’t get treated for it, putting themselves at risk for a heart attack, stroke or worse.
The condition, called peripheral artery disease, or P.A.D., is marked by diseased or blocked arteries in the legs. More than half of those with such circulatory problems in the extremities also have coronary or cerebral artery disease, noted Dr. Iftikhar J. Kullo, a cardiovascular specialist at the Mayo Clinic, in The New England Journal of Medicine in March. Failure to diagnose and treat blocked arteries elsewhere in the body can result in more serious, or even fatal, problems if they affect the heart or brain.
It may seem odd that people who have serious difficulty walking normal distances would not know something is wrong and get checked out. Yet, as Dr. Kullo noted, P.A.D. is both underdiagnosed and undertreated. And the number of cases of P.A.D. is only likely to rise as the population ages, he said.
“A lot of people limit their activity for other reasons, like a hip problem, back pain or breathing difficulty, and may not push themselves hard enough to provoke symptoms of P.A.D.,” said Dr. Paul W. Wennberg, a cardiologist and specialist in vascular disease at the Mayo Clinic. Or they may think their limited ability to exercise is to be expected, given their advancing years. Still others, Dr. Wennberg said, “may have only minimal disease in their legs, or they adapt their lifestyle to where they don’t notice symptoms anymore.”
In other words, since walking brings on pain, people typically find myriad ways to avoid doing it.
But this very response — remaining sedentary — is counterproductive, Dr. Wennberg said, because the best treatment for P.A.D. is exercise: Walking up to the point of pain, then resting until the pain subsides, then walking again, repeating the sequence until you’ve walked for 20 to 30 minutes (not counting rests) every day.
With this approach, Dr. Wennberg explained, exercise tolerance gradually increases as collateral blood vessels form in the legs that can compensate for blockages in the main arteries.
Just as teachers often have star pupils, Dr. Wennberg talks fondly of a man who was his star patient. When first seen, the patient, a 76-year-old Minnesotan, was afflicted with such severe peripheral artery disease that he couldn’t walk much beyond his backyard. Although a nonsmoker, the man had chronic obstructive pulmonary disease, which also limited how far he could walk. Yet he desperately wanted to be able to hike the nature trail behind his house, which motivated him to follow the doctor’s prescription religiously: Walk until it hurts, rest, then walk some more. Repeat several times a day.
“He got a treadmill to use in his house, and he walked outside whenever he could,” Dr. Wennberg recalled. “In just three months, he had doubled his walking distance as measured on a treadmill in the lab, and before long he was able to walk the mile-long nature trail.” Not only did the exercise prescription reduce his leg pain, it also improved his breathing. Together, these benefits enabled him to walk the desired distance without pain or fatigue.
Another of Dr. Wennberg’s patients, Donovan Merseth, 76, of Zumbrota, Minn., said he walks his two dogs four or five times a day, accumulating daily walks of three to four miles. “The more active I am, the better I feel,” Mr. Merseth said in an interview. “I walk at a moderate pace,” he said, calling his exercise “a senior power walk.”
Variable symptoms present another stumbling block to getting a correct diagnosis of P.A.D. The discomfort P.A.D. causes “is more often atypical than typical,” Dr. Wennberg wrote in the journal Circulation. “Descriptions such as ‘tired,’ ‘giving way,’ ‘sore,’ and ‘hurts’ are offered more often than ‘cramp’,” which can challenge an examining physician’s ability to suspect P.A.D. as the cause of a patient’s discomfort.
He suggested that doctors ask, “What’s the most strenuous thing you do in a typical week? Do you do any routine exercise, like walking? Do you get pain when you walk?”
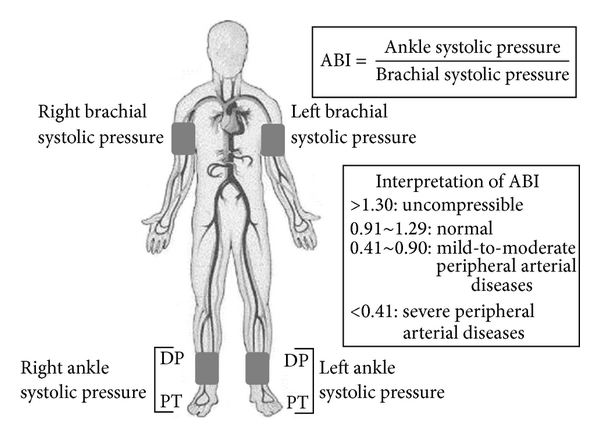
A simple noninvasive test that can be done in any doctor’s office, called the ankle-brachial index, or ABI, test, can reveal the likelihood of P.A.D. The test, which takes only a few minutes, compares blood pressure measured at the ankle with blood pressure measured in the arm. Lower pressure in the leg is an indication of P.A.D.
The index is calculated by dividing the systolic (top number) blood pressure in the arteries near the ankles by the systolic blood pressure in the arms. A low number strongly suggests a narrowing or blockage in the arteries that supply blood to the legs.
Follow-up tests, like an ultrasound exam of the arteries to the brain, may be done as well. “If there’s blockage in one area of the body, it’s likely also to be in another,” Dr. Wennberg noted.
Not surprisingly, the risk factors for P.A.D. closely match those for coronary heart disease: smoking (currently or formerly), diabetes, high blood pressure and high cholesterol. Consider asking your doctor to do the ABI test if you are 50 or older and have any of the above risk factors, even if you haven’t yet noticed a problem with walking (though insurance may not cover the cost if you lack symptoms).
However, Dr. Wennberg wrote, the ABI test done during rest may miss peripheral artery disease in nearly one-third of patients; they may require an ABI test following exercise on a treadmill to reveal the problem. The blood pressure measurements must be taken within a minute of stopping the exercise.
Given the same risk factors, African-Americans are more likely than Caucasians to develop P.A.D.
The average age at which people develop P.A.D. is 70, Dr. Wennberg said, adding that it occurs a decade earlier in people with diabetes and even earlier in people who both smoke and have diabetes.
Smoking increases the risk of developing P.A.D. fourfold, and more than 80 percent of people with the condition are current or former smokers.
Jane E. Brody : NY Times : April 11, 2016
More than eight million older Americans have a condition that can cause leg pain when they walk even short distances. Yet half of those who have the condition don’t know it and consequently don’t get treated for it, putting themselves at risk for a heart attack, stroke or worse.
The condition, called peripheral artery disease, or P.A.D., is marked by diseased or blocked arteries in the legs. More than half of those with such circulatory problems in the extremities also have coronary or cerebral artery disease, noted Dr. Iftikhar J. Kullo, a cardiovascular specialist at the Mayo Clinic, in The New England Journal of Medicine in March. Failure to diagnose and treat blocked arteries elsewhere in the body can result in more serious, or even fatal, problems if they affect the heart or brain.
It may seem odd that people who have serious difficulty walking normal distances would not know something is wrong and get checked out. Yet, as Dr. Kullo noted, P.A.D. is both underdiagnosed and undertreated. And the number of cases of P.A.D. is only likely to rise as the population ages, he said.
“A lot of people limit their activity for other reasons, like a hip problem, back pain or breathing difficulty, and may not push themselves hard enough to provoke symptoms of P.A.D.,” said Dr. Paul W. Wennberg, a cardiologist and specialist in vascular disease at the Mayo Clinic. Or they may think their limited ability to exercise is to be expected, given their advancing years. Still others, Dr. Wennberg said, “may have only minimal disease in their legs, or they adapt their lifestyle to where they don’t notice symptoms anymore.”
In other words, since walking brings on pain, people typically find myriad ways to avoid doing it.
But this very response — remaining sedentary — is counterproductive, Dr. Wennberg said, because the best treatment for P.A.D. is exercise: Walking up to the point of pain, then resting until the pain subsides, then walking again, repeating the sequence until you’ve walked for 20 to 30 minutes (not counting rests) every day.
With this approach, Dr. Wennberg explained, exercise tolerance gradually increases as collateral blood vessels form in the legs that can compensate for blockages in the main arteries.
Just as teachers often have star pupils, Dr. Wennberg talks fondly of a man who was his star patient. When first seen, the patient, a 76-year-old Minnesotan, was afflicted with such severe peripheral artery disease that he couldn’t walk much beyond his backyard. Although a nonsmoker, the man had chronic obstructive pulmonary disease, which also limited how far he could walk. Yet he desperately wanted to be able to hike the nature trail behind his house, which motivated him to follow the doctor’s prescription religiously: Walk until it hurts, rest, then walk some more. Repeat several times a day.
“He got a treadmill to use in his house, and he walked outside whenever he could,” Dr. Wennberg recalled. “In just three months, he had doubled his walking distance as measured on a treadmill in the lab, and before long he was able to walk the mile-long nature trail.” Not only did the exercise prescription reduce his leg pain, it also improved his breathing. Together, these benefits enabled him to walk the desired distance without pain or fatigue.
Another of Dr. Wennberg’s patients, Donovan Merseth, 76, of Zumbrota, Minn., said he walks his two dogs four or five times a day, accumulating daily walks of three to four miles. “The more active I am, the better I feel,” Mr. Merseth said in an interview. “I walk at a moderate pace,” he said, calling his exercise “a senior power walk.”
Variable symptoms present another stumbling block to getting a correct diagnosis of P.A.D. The discomfort P.A.D. causes “is more often atypical than typical,” Dr. Wennberg wrote in the journal Circulation. “Descriptions such as ‘tired,’ ‘giving way,’ ‘sore,’ and ‘hurts’ are offered more often than ‘cramp’,” which can challenge an examining physician’s ability to suspect P.A.D. as the cause of a patient’s discomfort.
He suggested that doctors ask, “What’s the most strenuous thing you do in a typical week? Do you do any routine exercise, like walking? Do you get pain when you walk?”
A simple noninvasive test that can be done in any doctor’s office, called the ankle-brachial index, or ABI, test, can reveal the likelihood of P.A.D. The test, which takes only a few minutes, compares blood pressure measured at the ankle with blood pressure measured in the arm. Lower pressure in the leg is an indication of P.A.D.
The index is calculated by dividing the systolic (top number) blood pressure in the arteries near the ankles by the systolic blood pressure in the arms. A low number strongly suggests a narrowing or blockage in the arteries that supply blood to the legs.
Follow-up tests, like an ultrasound exam of the arteries to the brain, may be done as well. “If there’s blockage in one area of the body, it’s likely also to be in another,” Dr. Wennberg noted.
Not surprisingly, the risk factors for P.A.D. closely match those for coronary heart disease: smoking (currently or formerly), diabetes, high blood pressure and high cholesterol. Consider asking your doctor to do the ABI test if you are 50 or older and have any of the above risk factors, even if you haven’t yet noticed a problem with walking (though insurance may not cover the cost if you lack symptoms).
However, Dr. Wennberg wrote, the ABI test done during rest may miss peripheral artery disease in nearly one-third of patients; they may require an ABI test following exercise on a treadmill to reveal the problem. The blood pressure measurements must be taken within a minute of stopping the exercise.
Given the same risk factors, African-Americans are more likely than Caucasians to develop P.A.D.
The average age at which people develop P.A.D. is 70, Dr. Wennberg said, adding that it occurs a decade earlier in people with diabetes and even earlier in people who both smoke and have diabetes.
Smoking increases the risk of developing P.A.D. fourfold, and more than 80 percent of people with the condition are current or former smokers.