- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
Skin Cancer
- Fighting Melanoma in the Mirror
By Eric Sabo : NY Times Article : October 16, 2008
Brief Overview: - Skin self-exams are the most direct method for detecting potentially deadly melanoma, though the benefits remain unproved.
- Moles that are smaller than a pencil eraser are rarely cancerous.
- 90 percent of melanoma growths are curable if caught early and removed; untreated, survival rates are worse than for lung cancer.
“Melanoma is the biggest no-brainer for screening,” said Myles Cockburn, a preventive medicine expert at the University of Southern California. “You’re looking right at the tumor.”
Moles at least the size of a pencil eraser are of greatest concern, since smaller spots are rarely cancerous, said Dr. David Polsky, a dermatologist at New York University School of Medicine. “To get hung up on the real small stuff is missing the bigger picture,” he said.
But changes to the color, size or shape of any mole may be an early indication of trouble, especially for someone who has a family history of melanoma or lots of unusual moles.
And while sun-drenched areas on the head or legs are likely sites for other forms of skin cancer, melanoma can develop anywhere on the body.
About 90 percent of melanoma growths are curable if caught early and surgically removed, putting the impetus on people at home to look for cancerous spots. When growths are left unchecked, the chances of surviving the disease for long are worse than for lung or colon cancer.
But in the push to make everyone better skin cancer detectives, tough obstacles — and questions — remain.
To locate the first signs of danger requires studious attention, and few people seem willing to bother. Nine to 18 percent of Americans regularly examine their own skin for melanoma, surveys show. Dermatologists, typically the first responders for skin cancer, may be quicker to schedule a Botox appointment than to verify a patient’s concern about changing moles, research shows.
Furthermore, there is no proof so far that such screening will ultimately help save any of the estimated 8,400 lives lost to melanoma each year in the United States.
“It’s still an open question,” said Dr. Marianne Berwick, a melanoma specialist at the University of New Mexico who led the largest and most rigorous investigation so far on skin self-exams. That study found that fastidious skin watchers had no better chance of surviving cancer after five years than those who did not check for moles. Two decades of follow-up have failed to show any improvement, she said.
The stakes are high. The chance of surviving melanoma turns sharply for the worse once the tumors have spread beyond their original site on the skin, making it critical to find changes early.
“There’s no really good proven therapy for advanced disease,” said Dr. Martin Weinstock, a professor of dermatology at Brown University Medical School.
Researchers have tested various treatments, including chemotherapy, radiation and the drug interferon, which show only modest effects against the later stages of melanoma. Newer drugs and vaccines are undergoing testing now. But the main reasons that melanoma survival rates have improved at all over the past 30 years are earlier detection and better screening.
Yet in the rush to get the cancer out fast, experts say they are noticing a relaxing of standards in diagnosing melanoma. Doctors these days are more likely to take out any suspicious mole out of fear of missing a cancerous one, and possibly getting sued for a missed diagnosis, these experts say.
A separate study conducted by Dr. Berwick found that 40 percent of the melanomas detected in 1988 would not have been considered cancerous 10 years earlier.
This could mean that surgeons are removing a fair share of lesions that aren’t melanoma, though even pathologists examining the same skin biopsy samples often disagree on whether the diagnosis is melanoma. At the same time, doctors who aren’t trained in spotting may be leaving harder-to-detect, slow-growing tumors behind.
“Unless you’re specifically trained as a clinician to do a skin exam, you can’t necessarily do a good one,” said Dr. Cockburn of U.S.C.
Nonetheless, like many doctors, Dr. Cockburn still believes that the odds can improve by teaching “your average Joe” to look for melanoma spots, a view shared by the American Cancer Society and other medical groups.
Enlisting the help of a spouse or partner may make it easier to track evolving moles on the body. A camera may also help. One study found that people who took photos of their skin improved their chances of detecting possible melanomas by 12 percent.
The only downside to home screening is in creating a nation of skin cancer hypochondriacs who further tilt the balance to unnecessary operations, experts warn.
But in this age of plastic surgery, the chance to overcome a deadly, but treatable, cancer is worth the risk, Dr. Cockburn said. “With the amount of stuff that gets chopped off these days,” he said, “I don’t really think there’s a problem.”
Expert Q & A :
Gauging Your Risk for Melanoma
By Eric Sabo : NY Times Article : October 16, 2008
Dr. Martin Weinstock is a dermatology professor at Brown University Medical School and the chief of dermatology at the Veteran’s Affairs Medical Center in Providence, R.I. He is also the chairman of the skin cancer advisory group for the American Cancer Society.
Q: The incidence of melanoma appears to be increasing, especially among young women. What accounts for this rise?
A: There are several trends, including greater sun exposure, going to sun-tanning booths and an emphasis in early detection that’s picking up more of the disease. Probably all three are playing a role.
Q: Some doctors question whether sun exposure causes melanoma. Do we know how big of a risk it is for this type of skin cancer?
A: There’s no real debate. Back in 1992 the World Health Organization convened an expert panel, and it concluded that ultraviolet light is a cause of melanoma. Now having said that, that doesn’t mean all melanomas are caused by ultraviolet rays. And indeed, we know some varieties of melanoma do not seem to be caused by it.
There is controversy over what proportion of melanomas are caused by sun exposure. But there’s no question that ultraviolet light is a cause. It’s beyond dispute as far as I’m concerned. Sun exposure is the most important avoidable risk factor for melanoma.
Q: Is sunscreen effective at preventing melanoma?
A: There’s good evidence that sunscreens may help prevent melanoma, but how effective they are is really poorly defined. In general, at least in the majority of melanomas, there seems to be a long lag period between ultraviolet exposure and the onset of the melanoma.
So it’s hard to measure the effect of sunscreens, and there’s a lot we don’t know. I wouldn’t say that should you use sunscreen you will prevent melanoma, but you can reduce your risk.
Q: What about other risk factors, like family history or having light skin? How important are these in causing melanoma?
A: Family and personal history are both very important. Certain genes affect the susceptibility of developing melanoma and can be inherited. It’s not a strictly genetic disorder, meaning that if your father had it, you will have it. But people who have a family history of melanoma are at a markedly higher risk. In addition, if you had a melanoma before, you are at much higher risk of getting it again.
The other major risk is irregular or larger moles. Having these, especially lots of large and irregular moles, can all increase your risk for melanoma.
Q: If one of your family members has another type of skin cancer, like squamous cell or basal cell carcinoma, are you at higher risk for melanoma?
A: They tend to go along separate lines to a large degree. But if you had a basal cell skin cancer before, for example, you have a higher risk for melanoma.
Q: Many medical professionals recommend early detection of cancerous moles as the best way to catch melanoma in time. How good is your average person at spotting suspicious moles and then seeing a doctor?
A: There are two things that are important for detecting melanoma. One is looking, and the other is seeing. Most people don’t even look. And in terms of looking, most don’t look at their skin in a thorough and systematic manner once a month, which is what’s recommended.
We don’t expect people to look at a spot and say, “Oh, that’s a melanoma.” But if there’s a warning sign, then it makes sense to have a doctor check it out.
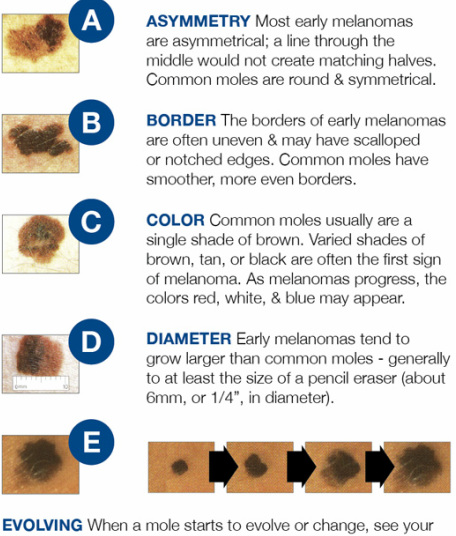
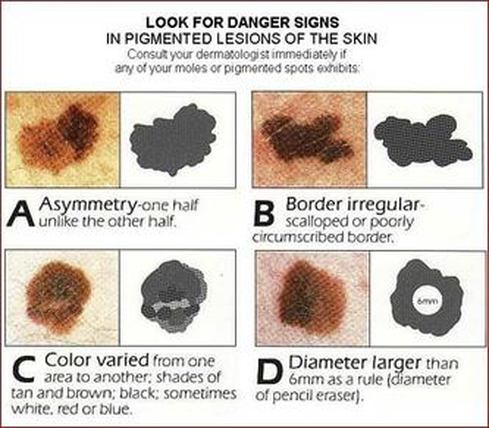
Q: What are the main warnings signs?
A: Spots that are new or changing in size, shape or color. Of if a mole looks different than the rest on your body.
There are the classic warning signs, or ABCD: A for asymmetry; B for irregular borders; C for multiple colors; D for diameter being more than six millimeters, the size of a pencil eraser. Those signs aren’t used as much as before because they’re not really sensitive enough. They tend to pick up more advanced melanomas, and we’re trying to pick up earlier melanomas.
The most important warning signs are newer, changing moles.
Q: Where do cancerous moles mostly show up?
A: They can be anywhere on your body. The back is a common place, but it can be anywhere. On the bottom of foot is not as common a spot, but it is the most common spot for brown skin colors.
Q: Are there any downsides to screening, or is it better to be safe than sorry?
A: Better to be safe than sorry. We recommend people self-screen and generally be aware of their own skin. It may result in a bunch of unnecessary trips to the doctor, and that’s a consequence.
The actual definitive test to determine if a mole is a melanoma is to do a biopsy. That’s really good for accuracy, but obviously you don’t want to biopsy everything on your skin, because you would be one big scar.
Q: Are there any high-tech devices that could help a person better track skin changes?
A: There’s a lot on the market, but many of these devices are expensive and mainly for clinicians.
Photography is helpful, and a camera is something you can obviously go and buy. Digital photos can be useful because if you’re looking for new lesions, having a picture of what your back used to look like, and then looking again later, can help you detect changes. You can put the photos on the Web, on Facebook or wherever.
Q:. How long can you have melanoma before it’s no longer curable by surgery?
A: Melanomas can grow in a month or two, or grow slowly over the years. We’re concerned if this is a melanoma lesion now, in which case it needs to be removed so you don’t suffer long-term consequences of an untreated cancer.
Whenever a melanoma is diagnosed or suspected, it’s surgically removed, and that can be curative. Melanoma is dangerous once it spreads beyond that local area. Looking at the lesion we took out by surgery, we can try to determine the characteristics of the tumor.
Q: If the cancer is caught late and cannot be cured by surgery, how effective are the current therapies at prolonging life?
A: Whether or not the melanoma has spread to other parts of the body is very important. If it has spread to other distant sites, such as to the lung or the brain, then the prognosis is very poor. It’s very likely that the person will succumb to melanoma. It’s not 100 percent, but there’s less of a chance for survival at that point.
Q: Is there any progress with new treatments, like vaccines or other therapies?
A: There’s lots of active research. We hear from time to time of some promising possibilities. But at the moment, there’s no really good proven therapy for advanced disease.
Q: So early detection is most important for finding melanomas in time and getting effective treatment?
A: That’s the best way for sure.
5 Things to Know :
Getting to Know Melanoma
By Eric Sabo : NY Times Article : October 16, 2008
Dr. Julie Lange is an assistant professor of surgery and oncology at the Johns Hopkins Medical School in Baltimore. She also helped write melanoma treatment guidelines for patients as part of the National Comprehensive Cancer Network. Here are five things she says patients should know about melanoma — the third most common, and most lethal, form of skin cancer.
Examine your skin regularly.
Check your entire body for suspicious moles that are new, growing or changing color. These may be the first warning sign of melanoma, or that your melanoma has returned. If caught in time, melanoma can be surgically removed and cured. People who have been treated for melanoma should see their doctor for a checkup at least once a year.
Confirm suspicious moles with a biopsy.
Having a specially trained expert analyze the results is as important as seeing a qualified dermatologist to check your skin. Biopsies that shave off small chunks of suspected tumors may leave the cancer behind and make it harder to determine if your melanoma has already spread. Surgical and so-called punch biopsies, which cut out a portion of skin, are the preferred method for confirming invasive melanoma. The lymph nodes are a common site for this type of cancer to spread, so a doctor may also biopsy these glands for more advanced melanomas.
Know what you’re fighting.
Tumors that pierce the skin by one millimeter or less are easier to treat. “The thinner the better,” Dr. Lange says. Surgery is 90 to 95 percent successful with such early-stage melanomas. In some cases, simply removing the cancerous mole during a biopsy can eliminate the disease, though thin tumors can also spread before they are detected. Tumors that grow to 4 to 10 millimeters thick are harder to treat, with cure rates dropping in more advanced stages of the disease.
Explore your options.
Treating your melanoma will depend on the size of the tumor and whether it has spread. Surgery is the preferred option during early stages of disease, while more advanced melanomas may require one of several different drugs. These include chemotherapy and radiation, along with special immune therapies, like interferon. Dr. Lange says there is considerable debate’ about whether interferon works for advanced melanomas, and all drugs come with unpleasant side effects. Patients may want to join a clinical trial, or turn to support care, which can minimize painful symptoms.
Limit your sun exposure.
Ultraviolet rays cause skin cancer and have been linked to some forms of melanoma. Stay out of the sun during the hottest parts of the day, and put on sunscreen or protective clothing when you have no choice but to be outside during these times. But sunlight also has positive benefits, including helping your body produce vitamin D, and at least four studies suggest that melanoma patients may live longer in sunny environments. “You don’t need to hide in a dark space,” Dr. Lange says.
PROTECT YOURSELF FROM THE SUN
(1) Use sunscreen. Apply often and liberally
(2) Wear sunglasses
(3) Wear a hat
(4) Limit your time in the sun. Try to avoid the sun between 10am and 2pm.
Explaining Sunscreen and the New Rules
By Jane E. Martin : June 20, 2011
Attention, sun lovers (and yes, that includes all who think they are adequately protected against the sun’s damaging rays): Nearly four years after announcing its intention to improve the labeling of sunscreens, the Food and Drug Administration has finally issued new rules that should help reduce the confusion that currently prevails when consumers confront the aisle-long array of products in most pharmacies.
But these rules will not take effect for another year (and for small manufacturers, two years). Meanwhile, everyone needs to know what to do now about preventing painful sunburns, disfiguring and deadly skin cancers and premature skin aging.
How high an SPF should one choose? Is SPF 60 really that much better than SPF 30? What does “broad spectrum” mean? Are all sunscreen ingredients equally effective? And equally safe?
And perhaps the most frightening question: Why has the incidence of melanoma, the deadliest of skin cancers, doubled since sunscreens (as opposed to tanning lotions) became popular?
No better time to get the answers to these questions than now, the week of the summer solstice. Even if it is not sunny where you are, the ultraviolet rays hitting your skin will be their most intense.
Rating Sunscreens
First, some facts about sun and current sunscreen labels. There are two kinds of solar rays: short ones called UVB that cause burning and skin cancer and long ones called UVA that cause skin cancer and wrinkling. SPF ratings — the letters stand for sun protection factor — reflect only the extent of protection against UVB. The higher the rating, the longer one can stay in the sun before burning.
But there are two important caveats. First, SPF ratings are based on a rather thick application of sunscreen, not the amount consumers normally use, which is most often a quarter to a half the amount applied in manufacturers’ tests. An adult in a bathing suit should apply about three tablespoons of lotion every two hours, experts say.
Second, above an SPF of 30, which can block 97 percent of UVB (if used in testing amounts), effectiveness increases by only 1 or 2 percent. In the way that sunscreens are used in the real world, then, a product with an SPF of 30 actually provides the protection of SPF 2.3 to 5.5, and one rated SPF 50 provides the protection of SPF 2.7 to 7.1, according to a report published this month in Drug and Therapeutics Bulletin.
UVA, which represents more than 95 percent of solar radiation reaching the earth, does not figure in SPF ratings. The phrase “broad spectrum” is meant to indicate protection against UVA, but there is no numerical rating for product effectiveness. Under the new rules, products labeled “broad spectrum” will have to provide equal protection against UVB and UVA, and only products with an SPF of 15 or higher will be allowed to claim protection against skin cancer and premature skin aging.
Meanwhile, dermatologists suggest choosing only products that are labeled “broad spectrum” and have an SPF rating of 30 to 50. There is no evidence that anything higher than 50 is any better. Apply the sunscreen just before exposure, and reapply it two hours later — it loses effectiveness over time. And even if the label claims the sunscreen is water resistant, be sure to reapply it after swimming or sweating heavily.
The rise in melanoma has led to fears that sunscreens may actually cause this deadly cancer. But other explanations are more likely. By allowing people to stay in the sun longer, sunscreens have greatly increased exposure to UVA radiation. And many, if not most, victims of melanoma were damaged long before sunscreens became popular. A history of sunburn is a major risk factor for this cancer; five sunburns per decade raise the risk by about threefold.
Another reason for the increase in diagnoses: skin cancer screening and detection have improved greatly in recent decades.
With regard to ingredients, many dermatologists recommend products with micronized titanium or zinc oxide as the most effective sun blockers that leave no white residue on the skin. There is some concern, based on animal studies, that the most popular ingredient in sunscreens, oxybenzone, may disrupt natural hormones, but the scientific evidence is scant.
Another chemical, retinyl palmitate, sometimes listed among the inactive ingredients, has been linked to skin cancers in animal studies. Because it is converted into a compound that can cause birth defects, it should be avoided by women who are pregnant or likely to become pregnant.
However, although more studies of these possible risks should be done, Consumer Reports concluded that “the proven benefits of sunscreen outweigh any potential risks.”
Finally, don’t be fooled by price. In tests of 22 sunscreens, Consumer Reports found nine to be effective against UVB and UVA and ranked three as “Best Buys”: Up & Up Sport SPF spray (88 cents an ounce) at Target; No-Ad With Aloe and Vitamin E SPF 45 lotion (59 cents); and Equate Baby SPF 50 lotion (63 cents). The organization said La Roche-Posay Anthelios SPF 40 cream, at $18.82 an ounce, scored well below these three in effectiveness.
Although it may be tempting to try to kill two birds at once with a combination sunscreen and insect repellent, the Centers for Disease Control and Prevention does not recommend this. Multiple applications could result in an overdose of the repellent.
Seek Other Protection
The best advice to prevent UV damage is to stay out of the midday sun altogether and to cover up with clothing, a hat and umbrella during the rest of the day even if it is cloudy. Clouds do not block damaging rays.
Keep in mind that ultraviolet radiation is reflected off sand and water, intensifying exposure even if you are protected by an umbrella from above.
Ordinary clothing provides a good sun shield when dry (the tighter the weave, the better) but little or no protection when wet. Special sun-protective clothing is costly but works well wet or dry; it is a wise investment for children who tend to stay in or around water for hours. Caps with a neck flap are especially helpful for sports enthusiasts. And no matter how well covered up you are, don’t forget to apply sunscreen to your face, ears, neck and hands.
Also, keep in mind that some sun exposure is necessary to maintain a healthful level of vitamin D. Dermatologists suggest, for light-skinned people, that exposing one’s hands, arms, face or back to nonburning doses of sunlight for 15 minutes two or three times a week from April to September should result in adequate vitamin D synthesis. Dark-skinned people need longer exposure.
Saving Young Skin From the Sun’s Perils
By Jane E. Brody : NY Times Article : June 19, 2007
Dr. Michael L. Ramsey, a dermatologist at the Geisinger Medical Center in Danville, Pa., coaches his son’s Little League team these summery days when he’s not removing patients’ skin cancers.
“The last thing I want is to someday see one of my baseball players as a patient,” he remarked recently in The Skin Cancer Foundation Journal.
And so, while encouraging the players to do their best on the field, he also pays close attention to their need to protect themselves from the sun’s skin-damaging ultraviolet rays. For he knows all too well that more than 90 percent of all skin cancers are caused by sun exposure; that the risk for a future skin cancer doubles with five or more sunburns; and that while the jury is still out, the risk of future melanoma, the deadliest form of skin cancer, may well be increased by even one blistering sunburn in childhood.
Moreover, while children may find it hard to imagine ever being old (over 50), repeated sun exposure also ages the skin, causing premature wrinkling and a mottled, leathery hide that resembles an elephant’s. It may also be hard to impress children with the possibility of cumulative sun damage to their eyes, like cataracts.
Children — as well as their parents and school authorities — have a lot to learn about protection against sun damage. Arrangements should be made in school, for example, for children to apply sunscreen and wear hats at recess. A child’s skin is especially vulnerable to the damaging effects of ultraviolet radiation. Most children will have had nearly a quarter of their lifetime exposure to this radiation by age 18, and the resulting damage is compounded repeatedly by subsequent exposure.
I’d be the last person to suggest that children spend the glorious months of summer indoors. I want them out playing actively year-round, and the warm months are ideal for such activities as running through sprinklers, swimming, boating, playing ball, riding bicycles and scooters, playing in sandboxes and on playground equipment, and otherwise having a grand old time being children.
But just as children must be protected against the hazards of traffic and predators, so must they also be protected against the downside of that life-giving force, the sun. Yet a study in Florida in 2001 found that only 33 percent of parents used any form of sun protection for their children, and those who did relied solely on sunscreen, which other studies have found is used incorrectly most of the time.
Some parents worry about a possible deficiency of vitamin D in babies kept out of the sun, since this essential nutrient is produced in skin in the presence of sunlight. But it takes only a few minutes of exposure to ultraviolet light two or three times a week during the summer months to make enough vitamin D to last all year. And child health experts, including the American Academy of Pediatrics, suggest that a safer alternative is to take 200 International Units of vitamin D a day, starting at the age of 2 months, through infant formula, fortified cows’ milk or soy milk, or a vitamin.
Short of remaining indoors, there are three main approaches to sun protection, regardless of age:
- Wearing clothes that block much of the sun’s radiation.
- Applying a complete sunscreen throughout the day every day.
- Staying out of the midday sun and in the shade as much as possible.
However, for as long as parents can get away with it, clothing is the ideal sunblock. In fact, for infants under 6 months old it is the only sunblock, far more effective than keeping babies in the shade. The skin of very young children is highly susceptible to sunburn and other harmful effects of ultraviolet radiation.
Wise parents will start putting hats on their children as soon as they are born and never stop. That greatly reduces battles about wearing a hat when they’re older. A baseball-style cap is not enough. The hat should have a full wide brim or desert-type flap that shields the face, ears and back of the neck.
Dark-colored clothing (again, not ideal for a hot summer day) is a better sunscreen than something light-colored. A white T-shirt, which some children wear in the water, has an sun protection factor, or S.P.F., of only about two when wet.
Instead of buying your child a costly toy this summer, consider investing in clothing specially designed with a built-in S.P.F. of 30 that offers 97 percent ultraviolet protection. One popular brand, Solumbra, includes neck-to-ankle swim suits for toddlers and swim shirts and leggings for older children, as well as everyday sun-protective clothing for children through size 12. The Web site is www.sunprecautions.com and the phone number is (800) 882-7860.
The fabric in this and other brands is designed to retain sun-protective properties through scores of washings, and the clothes can be handed down to younger children. Alternatively, try washing your children’s clothes with SunGuard, which treats fabric with Tinosorb, offering 96 percent ultraviolet protection that is retained through about 20 washings.
And don’t forget sunglasses with full ultraviolet protection (check the label), which should be worn by babies and children as well as adults. An elastic band can keep them on and not easily lost.
The Sunscreen Necessity This is a must for everyone starting at age 6 months, and there are now many effective products to choose from, including some that incorporate a light artificial tanning agent. Make sure the product provides full ultraviolet protection, against both UVA and UVB rays. The S.P.F. rating, which should be 15 or higher, refers only to UVB, the burning rays. Products with higher S.P.F. ratings offer minimal added protection.
Whether it is sunny or overcast and whether the child’s skin is light or dark, sunscreen should be applied daily, 20 minutes before the child goes outdoors so the chemicals can interact with skin. And it should be reapplied every two hours, because sun gradually degrades the chemicals. Each application should fully cover the child’s exposed skin, including ears and feet. Add a lip balm with an S.P.F. of 15 or higher.
Look for water-resistant products, though even these should be reapplied after swimming or heavy sweating. And check the expiration date because old sunscreen may lose some effectiveness
.
SPF rating : Is higher really better?
By Anahad O'Connor : NY Times Article : August 7, 2007
THE FACTS
Everyone knows that an SPF rating of 60 provides double the protection of SPF 30 — or does it?
Studies over the years have shown that sunscreen with an SPF, or sun protection factor, of 30 blocks about 97 percent of ultraviolet rays. A rating of 15 means 93 percent of UV rays are blocked, and anything higher than 30 remains in the 97 or 98 percent range.
In 1999 the Food and Drug Administration recommended that sunscreens with an SPF higher than 30 be labeled “30+,” mostly to prevent people from developing a false sense of security that might lead them to spend more time in the sun.
What many people do not realize is that the amount of sunscreen applied plays an enormous role. A study in The British Journal of Dermatology this year found that applying less than two ounces over the entire body at one time can leave people with an SPF rating far lower than what is on the bottle. Some studies have shown that people typically apply just 10 percent of the amount recommended.
It is also important to look for sunscreens that protect against UVA and UVB radiation. SPF ratings apply only to UVB rays, and some sunscreens provide no protection at all against UVA rays, which penetrate the skin more deeply. For broad protection, look for sunscreens with avobenzene, zinc oxide or titanium dioxide, all of which block UVA.
THE BOTTOM LINE
Above SPF 30, the increased protection is minimal.
Made in the Shade While staying in the shade is better than nothing, a lot of ultraviolet radiation is reflected off the ground or nearby objects when you are under an awning or beach umbrella. Infants should be protected by shade as well as clothing.
Even with sunscreen on, it is best to keep children out of the sun from 10 a.m. to 4 p.m. Parents may have to lobby their schools to provide shaded areas for children during recess.
Finally, set a good example by following the above advice yourself. For additional information, see “Sun Protection for Life,” by Mary Mills Barrow and John F. Barrow (New Harbinger Publications, 2005).
Skin Deep: Beware the Afterglow
By Natasha Singer : NY Times article : May 3, 2007
Years before Ursula Andress, the Swiss actress who was the first Bond girl, emerged from the waves in “Dr. No” with her caramel skin offset by a blindingly white bikini, the tan had taken hold as the abiding fashion image.
A honey-glowing face and a body that is buff and bronzed had come to conjure up associations of beauty, leisure and upper-class privilege: of exotic private beaches, robust games of tennis, long afternoons aboard a yacht and, of course, the healthy-looking afterglow of exercise or sex.
Even in the 25 years since medical groups began warning that ultraviolet irradiation can lead to skin cancer as well as to dire consequences for the appearance-conscious — wrinkles! — tan-looking skin has remained an iconic beauty image, promoted by fashion magazines, advertisements and celebrities.
But the chic method of acquiring a tan has shifted. With sunbathing and tanning beds deemed risky, some doctors, magazines and beauty companies are promoting the idea of a “sunless” tan begat by cosmetics as the safe alternative to UV irradiation.
And so simulated tanning is booming. This month, cosmetics brands are introducing new artificial bronzing agents including sprays, lotions, mousses, powders and towelettes into a market that is already brimming with products. Meanwhile, fashion magazines are enthusing over the fake tan with buzzwords like sun-kissed, radiant, natural-looking, tawny, healthy and glowing.
“We are being inundated with the look of a woman of leisure who has a beautiful glow, whether from a sunless tanner or a bronzer,” said Karen Grant, the senior beauty industry analyst for the NPD Group, a market research firm. “The marketing theme is that the products can give you the same glow that the sun can provide without the risks of going out into the sun.”
Indeed, the notion of a safe, healthy sunless tan is making Malibu Barbie the retro icon of the season.
But some researchers who study the skin are worried that promulgating the simulated tan as a beauty ideal is simply perpetuating an image that is fundamentally linked to risky behavior. The concern is that the fashion for a bronzed look, even a cosmetically induced one, may encourage young women to seek a tanned appearance at any cost.
According to a study published last year in the Journal of the American Academy of Dermatology, for example, young women who used sunless tanners were more likely to have been sunburned and to have visited tanning parlors compared with those who were not interested in and did not use such bronzing lotions. The study, conducted at Boston University School of Medicine, also reported that, although many self-tanning products do not contain sunscreen, a number of young women believe they offer sun protection.
“We know that physicians are urging patients to use sunless tanning products instead of tanning booths,” said Alan C. Geller, a research associate professor in dermatology at Boston University and one of the authors of the study. “But sunless tanners are not serving the purpose of a safe alternative because we found young women using them as an adjunct to sunbathing and tanning beds.”
Many women say self-tanners have become as regular a part of their beauty routine as moisturizer or mascara. Most commonly, they apply powdered bronzer to their faces and tanning moisturizers to their arms and legs.
The sales figures bear this out. In the last five years, department-store bronzer sales have increased to about $62 million from about $30 million, according to NPD. At the mass market level, self-tanners, bronzers and tanning moisturizers, called “natural glow” lotions, have annual sales of about $229 million, according to Information Resources Inc., a market research firm that covers the personal care industry.
Nina Jablonski, the chairwoman of the anthropology department at Penn State University, said that trying to change one’s skin color is a peculiar and disturbing phenomenon — whether it be Africans and Asians who use bleaching products to lighten skin or lighter-pigmented Americans seeking to emulate deck stain. Along that continuum, the sun-tanned look is a relatively new beauty ideal, she said.
“For most of the last 500 years, a tan was considered the mark of a hard-working person who toiled outside,” said Dr. Jablonski, the author of “Skin: A Natural History.” “A tan was eschewed by people who considered themselves upper class.”
During the Industrial Revolution, as work increasingly moved to indoor factories, sun-baked skin became the province of the upper classes who had more leisure time and money to travel. Coco Chanel, who returned to Paris with a dramatic suntan acquired during a holiday on the Riviera in the 1920s, is credited with initiating the vogue for sunbathing. She reincarnated what had been a lower-class stigma as an aspiration, a symbol of upper-class wealth, leisure, good looks and healthy athleticism.
In the 1960s, George Hamilton personified the perpetual tan. In 1971, Mattel introduced Malibu Barbie, the ultimate beach bunny. And baby oil, used to hasten a deeper tan, was the rage in the 1970s.
“The tan went from being a thing that working people got by the sweat of their brows to being associated with a glamorous, luxurious lifestyle,” Dr. Jablonski said. “It is one of the most deeply ingrained images in American advertising.”
But in the early 1980s, the tan began to lose some of its allure after health authorities in Australia noticed an increased incidence of skin cancer among residents who had emigrated from Europe. They began to link skin cancer and sunbathing. In 1985, the American Academy of Dermatology conducted its first national campaign to warn Americans about the risks of sun exposure.
As a result, the product-induced tan has replaced the outdoorsy tan as a beauty ideal. And celebrities like Jennifer Lopez, Jessica Alba and Eva Longoria, with their own naturally glowing skin, are inspiring legions of imitators. Now starlets like Lindsay Lohan and Paris Hilton often appear preternaturally bronzed. Even the model Natalia Vodianova, known for her porcelain face, appears this month in a Calvin Klein perfume ad looking as if she has been powdered with baked earth.
“Bronzer makes you look healthy, healthy, healthy,” said Olivier Échaudemaison, the makeup artistic designer for Guerlain. “Pale skin makes you look tired, but if you are wearing bronzer nobody knows you are tired underneath.”
To provide that simulacrum of health, cosmetics that create ersatz tans now come in three categories: self-tanners, bronzers and “glow” lotions.
Self-tanners trigger a chemical reaction, causing a brownish stain to form on the outer layer of the skin. Until recently, self-tanners were often messy to use, noxious-smelling, time-consuming and capable of turning the skin a bright shade of Oompa-Loompa orange. In the last few years, however, cosmetics companies have introduced improved formulas.
Bronzers are powders that are applied like blush. Guerlain is credited with creating the category in 1984 when it introduced Terracotta Powder, which could be brushed on for an instant coppery sheen.
“Suddenly, they have the look of just coming back from St. Barth’s, but really they spent the weekend at home and put on the powder,” Mr. Échaudemaison said.
Meanwhile, other brands, including Lancôme, are bringing out increasingly elaborate bronzing compacts that are embossed with patterns and come in multiple luminescent hues that can be used all over the body.
“Women today are on the go and they have no time or desire to sit down and sunbathe or wait overnight for a tanner to show its real color,” said Gracemarie Papaleo, assistant vice president for new product development at Lancôme USA. “With a bronzer, you get immediate results.”
“Glow” lotions, which are moisturizers that gradually darken the skin with each use, are also a growing trend. Jergens Natural Glow, introduced in 2005, was the first successful tanning moisturizer. Now other beauty brands are coming out with similar products based on the idea of a healthy, natural-looking glow. Ads for the new Nivea Visage Sunkissed Facial Moisturizer, for example, promise “a healthy-looking tan in just five days.”
“People want to look healthy without getting sun damage, to have that same California, sun-kissed type of look like every celebrity on the red carpet,” said Leigh Anne Rowinski, director of client solutions at Information Resources Inc.
But some critics worry that promoting sunless tans and glows as healthy, stylish and natural perpetuates the tan — whether cosmetic induced or sun-induced— as a beauty ideal, even as it posits pale skin as unhealthy, dull, unnatural and even passé.
“Even though a tan is now associated with pathology, it has had such a profound impact on the American psyche that to be untan is to look as terribly uncool as an unplucked chicken,” said Dr. Jablonski of Penn State. “People tend to think they look healthier if they have some sort of glow on their cheeks.”
But researchers at Boston University School of Medicine did not find that those who use self-tanners necessarily avoid UV rays. In a survey of 448 people age 18 to 30, the researchers found that young women who used sunless tanners were more likely to get sunburns and use sun beds than their peers who were not interested in self-tanning products; the results were similar to those found in studies in Australia. The researchers urged companies to include a minimum of S.P.F. 15 sunscreen in every sunless tanning product.
In a related research project, Zeina Dajani, a medical student at Boston University, found that a number of sunless tanners that did not contain sunscreen failed to carry a warning label, mandated by the Food and Drug Administration, to indicate that the products do not protect against sunburn and other damage.
“The question is whether dermatologists should stop recommending sunless tanning products as an alternative to tanning beds and discourage the idea of a tan altogether,” Ms. Dajani said.
At least one celebrity is glow-averse. In the May issue of Allure magazine, the actress Michelle Trachtenberg said the pressure to bronze is her pet peeve with beauty advisers at makeup counters.
“They’re like, ‘Maybe you’d like to warm up your skin tone,’ ” Ms. Trachtenberg is quoted as saying. “And I’m like, ‘No, I’m going to embrace the pale.’ ”
Wrinkles : Three Treatments Shown To Work
By Nicholas Bakalar : NY Times Article : August 19, 2008
Nostrums that promise to smooth wrinkled skin are a staple of snake-oil salesmen everywhere, but now there is strong evidence that certain kinds of treatment are effective. Over the past decade, researchers have been learning which treatments work, and why.
The key is a growing understanding of the skin's connective tissue, called the dermal collagen, and a recognition that damage to the mechanical properties of the collagen outside the skin cells, and not necessarily genetic damage to the cells themselves, causes wrinkled skin.
A recent review in The Archives of Dermatology concludes that three anti-aging treatments are proven clinically effective:
- the topical application of retinol;
- carbon dioxide laser resurfacing; and
- injection of hyaluronic acid, a moisture-retaining acid that occurs naturally in the skin.
"This is an area where there's a lot of hype and not much substance," said David J. Leffell, a professor of dermatology and surgery at Yale who was not involved in the review. But, he said, this study is "good science."
Theory and experiment back these treatments, the authors write. Fibroblasts — connective tissue cells — secrete a complex group of polysaccharides and proteins that creates collagen, which gives the skin shape and elasticity and supports the blood vessels that permeate it. The network of collagen tissue is maintained by its mechanical tension with these skin cells.
Skin deteriorates as it ages, but its exposure to sunlight inhibits the ability of fibroblasts to produce collagen. The hands, face, neck and upper chest all suffer more than unexposed skin, and light-pigmented people wrinkle more readily than others. This damage, the authors write, is essentially an accelerated version of chronological aging. Ultraviolet radiation induces production of the same enzymes that degrade collagen with age.
Collagen fibers last as long as 30 years. But with age and ultraviolet exposure, they deteriorate and fragment, and fragmented collagen impairs the collagen-producing function of the fibroblasts that created it. As the fragmented collagen accumulates, new collagen production declines, the connections between the fibroblasts and the collagen weaken, and the skin, now lacking support, begins to wrinkle.
But there are treatments that counter this process. Topical application of retinol, a form of vitamin A, was the first to be proved useful. Although the molecular pathways are not well understood, retinol causes new collagen to form in chronologically aged skin and in skin damaged by ultraviolet light.
Skin creams with retinol are available over the counter, but many do not indicate the concentration of the active ingredient. "Many products just refer to retinol or vitamin A as a buzzword," said Gary J. Fisher, the lead author of the review and a professor of dermatology at the University of Michigan.
Concentrations of 0.2 to 0.6 percent are enough, Dr. Fisher said, but preparations strong enough to have an effect can also have a side effect, a rash called retinoid dermatitis. Dr. Fisher's advice is to stop using it if a rash occurs. The rash can sometimes be avoided if the concentration is increased gradually.
Retinol also makes the skin more sensitive to damage from ultraviolet light, so protection from the sun while using it is essential. "O.T.C. products tend to try to walk the line between effects and side effects," Dr. Fisher said. "But many intentionally keep the concentration too low to have any benefit."
Dr. Robyn S. Gmyrek, an assistant professor of dermatology at Columbia University, is also skeptical of over-the-counter wrinkle creams. "If something shows true biological activity, it's regulated as a drug," she said. "A cream bought over the counter is certainly not going to do what prescription-strength retinol will do." Dr. Gmyrek was not involved in the study.
Carbon dioxide laser resurfacing is another well-tested treatment for wrinkles. The laser removes thin layers of skin without damaging surrounding tissue. As the wound heals, new collagen is produced. The treatment works first by inducing high levels of matrix metalloproteinase, or MMP, an enzyme that destroys fragmented collagen. Then it reduces MMP and the production of new and undamaged replacement material. The procedure is also used for removing scars, warts and birthmarks.
Healing takes two to three weeks, and the wound has to be cleaned with saline or diluted vinegar and treated with ointments to prevent scarring. In most cases, the procedure is done only once, Dr. Fisher said, and lasts many years.
There are now some less invasive laser procedures, the authors write, but their effectiveness is doubtful.
The third effective treatment is injecting a form of hyaluronic acid, similar to a substance the skin normally produces, into the dermis that underlies the wrinkles. This was originally designed as a space filler, with no intended physiological effect. But as the injection stretches the dermis, the fibroblasts respond by producing more collagen and less MMP. The authors cite studies that have demonstrated that increased collagen production is visible within a month after the injection. The benefit lasts about six months, Dr. Fisher said.
This type of hyaluronic acid, he said, should not be confused with hyaluronic acid in some topical cosmetic products. Rubbing such products on the skin will not stimulate collagen production.
Do the benefits of these treatments outweigh the risks?
"It's a matter of the kind of problem a person perceives and how he wants to deal with it," Dr. Fisher said. "For these treatments, which have sound research behind them, and for people who want to improve their appearance, the benefits far outweigh any problems."
The authors have no ties to companies that make skin care products, but the University of Michigan, where they teach, has patents on the use of matrix metalloproteinase inhibitors in the treatment and prevention of aging skin.
Skin-Cancer Groups Push for More Checkups
Melanoma is on the rise, particularly in people younger than age 30.
Laura Landro : WSJ : September 2, 2013
With current estimates that 1 in 5 Americans will develop skin cancer in their lifetime, dermatologists and cancer groups are stepping up efforts to screen patients at least once a year and teach them to perform their own self-exams as often as monthly.
Doctors are creating photographic "mole maps" to track changes over time, and some dermatologists are turning to a new, noninvasive device that helps determine which moles should be biopsied for melanoma, the deadliest form of skin cancer.
What to Look For Skin Cancer Warning Signs
Unexpected Spots
Skin cancer can occur even in spots usually not exposed to sunlight. Some areas of the body people may fail to check:
Skin cancer accounts for nearly half of all cancers in the U.S., with an estimated 3.5 million non-melanoma types diagnosed each year, according to federal data analyzed for a 2010 study in the journal in the journal JAMA Dermatology. Melanoma is rarer, with an estimated 137,900 new cases predicted for this year, nearly 78,000 of them invasive. But its incidence is rapidly increasing, especially in people younger than 30.
While skin cancers such as basal and squamous cell cancers can be disfiguring, they are highly curable. Melanoma is curable if caught early and surgically removed, but can quickly thicken, spread elsewhere in the body and turn lethal. Recurrence of melanoma 10 or more years after treatment is more common than previously thought, occurring in more than 1 in 20 patients, according to a study in July in the Journal of the American College of Surgeons.
While melanoma can occur in any skin color and in areas such as the soles of the feet where there is little or no sun exposure, all skin cancers are strongly linked to ultraviolet radiation from the sun and increasingly, from tanning beds.
One blistering sunburn at a young age can more than double the chances of melanoma later in life. Pediatric melanomas, though still unusual, are steadily rising. A study in April in the journal Pediatrics found that childhood and adolescent melanoma increased 2% a year from 1973 to 2009, driven by 15- to-19 year-olds, with 18 cases per million.
Dirk Elston, president of the American Academy of Dermatology, says there is increasing evidence that self-exams and physician examinations may lead to a reduction in melanoma thickness at time of diagnosis and improved survival rates.
The issue of how widely to screen patients is a subject of debate. The U.S. Preventive Services Task Force, an advisory body, concluded in 2009 that evidence isn't sufficient to assess the balance of benefits and harms of whole-body skin exams or self exams for the general population. It cites risks from misdiagnosis, over-diagnosis and harms from unnecessary biopsies and overtreatment.
The task force says doctors should remain alert for unusual skin lesions in physical exams performed for other purposes and consider risk factors such as fair skin, number of moles and family history. (Generally, a family history appears to increase risk of melanoma by about twofold, according to the National Cancer Institute. In recent years, researchers have found gene mutations that seem to play a part in some cases.)
The task force is expected to review new evidence next year, which includes a 2012 study from Germany, where more than 360,000 patients in one state were offered skin-cancer checks. The screening detected earlier-stage tumors and significantly reduced mortality rates compared with other parts of the country without the screening programs.
While widespread screening for melanoma in children isn't necessary, says Lynn Cornelius, chief of dermatology at Washington University in St. Louis, kids should be checked individually. She tells parents, "know your kids' moles, and when something is persistent, changing or bleeding, or it is unusual looking and new, bring it to your pediatrician's attention."
At the beginning of the summer, Jennifer Phillips became concerned about changes in a mole on her 13-year-old daughter Maggie Foley-Phillips's back since birth. Ms. Phillips says she is vigilant about sunscreen, but the family lives in Rancho Palos Verdes, Calif., and is active outdoors. She asked Manhattan Beach dermatologist, Glynis Ablon, to take a look.
Dermatologists typically view moles with a magnifying lens known as a dermatascope that examines the skin's surface. Dr. Ablon used a device called MelaFind, approved by the Food and Drug Administration in 2011, which relies on computer light technology to examine moles as deep as 2.5 millimeters below the skin's surface. Dr. Ablon, also a consultant to the device's developerMela Sciences Inc., MELA -0.46% says the results indicated the mole was benign, and helped her determine a biopsy wasn't necessary.
Dermatologists pay about $10,000 for the machine and a fee per usage, then charge patients $25 to $40 per lesion or $150 to $175 per session for multiple lesions, which isn't covered by insurance. Ms. Phillips says her 16-year-old daughter, Mackenzie, had a skin biopsy several years ago that hurt and left a scar, so Maggie was apprehensive. Ms. Phillips was relieved not to put her through the same thing unnecessarily. "It was the best $150 I ever spent," she says.
Jennie Brach, owner of a Brooklyn, N.Y., furnishings and design company, saw Darrell Rigel, a professor of dermatology at New York University who consults for Mela Sciences, last year about an unusual patch of skin on her leg. "It had some changes and had spread out a little bit," she says. After MelaFind indicated it had irregular growth patterns under the surface, Dr. Rigel did a biopsy. The mole turned out to be an early stage melanoma, and was surgically removed. "It hit me like a bomb, and was very traumatic, but thank God it was only on the surface," Ms. Brach says.
MelaFind is in use in about 100 doctors offices and clinics in 29 states.
One concern, says Dr. Cornelius of Washington University, is that the device may lead doctors to become "complacent" and not do a thorough visual exam. "The jury is still out as to whether this is better than a trained eye with a dermatascope," she says. She creates mole maps using digital photos to track changes over time, but advises patients to be vigilant in monthly self exams, "because things can change so quickly."
Melanoma is on the rise, particularly in people younger than age 30.
Laura Landro : WSJ : September 2, 2013
With current estimates that 1 in 5 Americans will develop skin cancer in their lifetime, dermatologists and cancer groups are stepping up efforts to screen patients at least once a year and teach them to perform their own self-exams as often as monthly.
Doctors are creating photographic "mole maps" to track changes over time, and some dermatologists are turning to a new, noninvasive device that helps determine which moles should be biopsied for melanoma, the deadliest form of skin cancer.
What to Look For Skin Cancer Warning Signs
- A skin growth that increases in size and appears pearly, translucent, tan, brown, black, or multicolored
- A spot or sore that continues to itch, hurt, crust, scab, erode, or bleed
- An open sore that does not heal within three weeks
- A mole, birthmark, beauty mark, or any brown spot that: changes color; increases in size or thickness; changes in texture; is irregular in outline; is bigger than 6 mm or ¾ inch, the size of a pencil eraser; appears after age 21.
Unexpected Spots
Skin cancer can occur even in spots usually not exposed to sunlight. Some areas of the body people may fail to check:
- Scalp
- Soles of the feet
- Palms of the hands
- Fingernails, toenails
- Back of the legs
- Genital area
Skin cancer accounts for nearly half of all cancers in the U.S., with an estimated 3.5 million non-melanoma types diagnosed each year, according to federal data analyzed for a 2010 study in the journal in the journal JAMA Dermatology. Melanoma is rarer, with an estimated 137,900 new cases predicted for this year, nearly 78,000 of them invasive. But its incidence is rapidly increasing, especially in people younger than 30.
While skin cancers such as basal and squamous cell cancers can be disfiguring, they are highly curable. Melanoma is curable if caught early and surgically removed, but can quickly thicken, spread elsewhere in the body and turn lethal. Recurrence of melanoma 10 or more years after treatment is more common than previously thought, occurring in more than 1 in 20 patients, according to a study in July in the Journal of the American College of Surgeons.
While melanoma can occur in any skin color and in areas such as the soles of the feet where there is little or no sun exposure, all skin cancers are strongly linked to ultraviolet radiation from the sun and increasingly, from tanning beds.
One blistering sunburn at a young age can more than double the chances of melanoma later in life. Pediatric melanomas, though still unusual, are steadily rising. A study in April in the journal Pediatrics found that childhood and adolescent melanoma increased 2% a year from 1973 to 2009, driven by 15- to-19 year-olds, with 18 cases per million.
Dirk Elston, president of the American Academy of Dermatology, says there is increasing evidence that self-exams and physician examinations may lead to a reduction in melanoma thickness at time of diagnosis and improved survival rates.
The issue of how widely to screen patients is a subject of debate. The U.S. Preventive Services Task Force, an advisory body, concluded in 2009 that evidence isn't sufficient to assess the balance of benefits and harms of whole-body skin exams or self exams for the general population. It cites risks from misdiagnosis, over-diagnosis and harms from unnecessary biopsies and overtreatment.
The task force says doctors should remain alert for unusual skin lesions in physical exams performed for other purposes and consider risk factors such as fair skin, number of moles and family history. (Generally, a family history appears to increase risk of melanoma by about twofold, according to the National Cancer Institute. In recent years, researchers have found gene mutations that seem to play a part in some cases.)
The task force is expected to review new evidence next year, which includes a 2012 study from Germany, where more than 360,000 patients in one state were offered skin-cancer checks. The screening detected earlier-stage tumors and significantly reduced mortality rates compared with other parts of the country without the screening programs.
While widespread screening for melanoma in children isn't necessary, says Lynn Cornelius, chief of dermatology at Washington University in St. Louis, kids should be checked individually. She tells parents, "know your kids' moles, and when something is persistent, changing or bleeding, or it is unusual looking and new, bring it to your pediatrician's attention."
At the beginning of the summer, Jennifer Phillips became concerned about changes in a mole on her 13-year-old daughter Maggie Foley-Phillips's back since birth. Ms. Phillips says she is vigilant about sunscreen, but the family lives in Rancho Palos Verdes, Calif., and is active outdoors. She asked Manhattan Beach dermatologist, Glynis Ablon, to take a look.
Dermatologists typically view moles with a magnifying lens known as a dermatascope that examines the skin's surface. Dr. Ablon used a device called MelaFind, approved by the Food and Drug Administration in 2011, which relies on computer light technology to examine moles as deep as 2.5 millimeters below the skin's surface. Dr. Ablon, also a consultant to the device's developerMela Sciences Inc., MELA -0.46% says the results indicated the mole was benign, and helped her determine a biopsy wasn't necessary.
Dermatologists pay about $10,000 for the machine and a fee per usage, then charge patients $25 to $40 per lesion or $150 to $175 per session for multiple lesions, which isn't covered by insurance. Ms. Phillips says her 16-year-old daughter, Mackenzie, had a skin biopsy several years ago that hurt and left a scar, so Maggie was apprehensive. Ms. Phillips was relieved not to put her through the same thing unnecessarily. "It was the best $150 I ever spent," she says.
Jennie Brach, owner of a Brooklyn, N.Y., furnishings and design company, saw Darrell Rigel, a professor of dermatology at New York University who consults for Mela Sciences, last year about an unusual patch of skin on her leg. "It had some changes and had spread out a little bit," she says. After MelaFind indicated it had irregular growth patterns under the surface, Dr. Rigel did a biopsy. The mole turned out to be an early stage melanoma, and was surgically removed. "It hit me like a bomb, and was very traumatic, but thank God it was only on the surface," Ms. Brach says.
MelaFind is in use in about 100 doctors offices and clinics in 29 states.
One concern, says Dr. Cornelius of Washington University, is that the device may lead doctors to become "complacent" and not do a thorough visual exam. "The jury is still out as to whether this is better than a trained eye with a dermatascope," she says. She creates mole maps using digital photos to track changes over time, but advises patients to be vigilant in monthly self exams, "because things can change so quickly."