- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
A New Look at Living Wills
These critical documents about your preferences for end-of-life care don't always work as planned. More flexibility might be the answer.
Laura Johannes : WSJ : June 8, 2012
My father was in a coma, hooked up to a ventilator, and I had to make a tough call.
His living will expressed his desires for a few black-and-white situations: He didn't want to be kept alive if he was terminally ill, or in an irreversible vegetative state. But the situation I faced wasn't so simple. The neurologist said he would wake up from the coma, but there was a good chance he would have severe brain damage. How much of a chance? The doctors couldn't say.
Doctors and nurses say my heart-wrenching experience is typical of the complexity of real-life bedside decisions. An estimated 25% to 30% of Americans have filled out living wills, documents that spell out wishes for medical treatment. But ethicists say the typically simplistic documents aren't the solution many hoped they would be. Life-prolonging medical technology has far outstripped doctors' ability to predict outcomes. The hardest choices center on when quality of life will be so diminished that death is preferable.
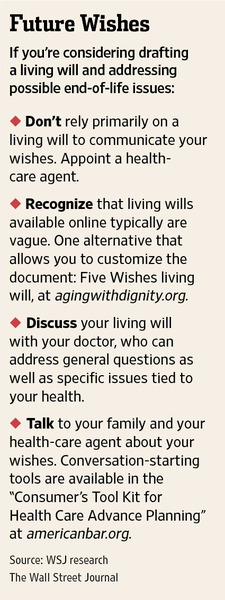
As such, some health organizations are trying to improve living wills, allowing for more flexibility and nuance. Some ethicists, meanwhile, are de-emphasizing living wills altogether and focusing on appointing a trusted family member or friend as your health-care agent.
"Most of us have come to the conclusion that the way to get over the vagueness is to get someone to speak for you," says Robert M. Veatch, a professor of medical ethics at Georgetown University's Kennedy Institute of Ethics in Washington, D.C.
Living wills were created in the 1960s and gained national attention in the 1970s when a young woman, Karen Ann Quinlan, following alcohol and drug use at a party, was left in a vegetative state, raising alarms about medical technology keeping people alive in hopeless circumstances.
"We had a naive view that if you had a document, that would solve the problem," says Daniel Callahan, co-founder and president emeritus of the Hastings Center, a Garrison, N.Y., nonprofit that was an early champion of living wills. "In practice," he says, "all sorts of problems arise" that aren't spelled out in the documents.
When Paul Shalline, an active 86-year-old who regularly bested his grandchildren at ping pong, was unable to communicate after a severe stroke in March, treatment decisions fell to his daughter, Robin. Ms. Shalline, a 57-year-old teacher from Monkton, Vt., says her father had a living will but had never talked to her about his wishes. "There is so much gray area," she says. "You'd hope the living will would spell it all out, but it doesn't."
His living will called for withdrawing life support if there was no reasonable expectation of regaining a "meaningful quality of life" but didn't describe what that meant, she says. Ms. Shalline, when told by doctors that her father could be blind in one eye, unable to feed himself and might never walk again, made the decision to withdraw the ventilator based on "what I knew about his life." Mr. Shalline, who loved Wiffle ball and had recently helped build a staircase, was "proud of his 'physicalness,' " she says. He died March 18. It is hard enough, under the best of circumstances, to know what your family member would want in a particular situation. But add to that the fact that even top doctors can't predict outcomes very well.
Lee H. Schwamm, vice chairman of the neurology department at Massachusetts General Hospital in Boston, where Mr. Shalline was treated, says that even when he thinks he can predict a patient's outcome after a stroke, he is wrong 15% to 20% of the time on major outcome measures, such as whether a patient will be able to walk again. "I've never seen a living will—and I've seen a lot—that speaks to this question of diagnostic uncertainty," says Dr. Schwamm.
Living Documents
You can get a living will from a lawyer or download it from the Internet. Many focus on permanent comas and clearly hopeless conditions. Florida's statute-suggested living will, for example, directs life-prolonging treatments to be stopped if there is "no reasonable medical probability" of recovery from a terminal condition or persistent vegetative state. Florida, like most states, allows you to write your own living will; a few states, such as New Hampshire, specify that living wills must use a state-approved form. (A bill now being considered in New Hampshire would make the state form optional.)
A number of efforts have been made to improve on the standard-style living will. A document available online from Lifecare Directives LLC, Las Vegas, for example, spells out several levels of cognitive decline from coma to mental "confusion" that require 24-hour supervision, and asks if you would want life support if your brain failed that much. The document also gives you an option to say whether you want doctors to be "positively certain," "certain to a high degree" or "reasonably certain" that you will never recover before pulling the plug.
A simpler but also innovative approach is the popular Five Wishes living will. Five Wishes is written at a sixth- to seventh-grade level, says Paul Malley, president of Aging with Dignity, a nonprofit that distributes the document. Despite its simplicity, the Five Wishes living will addresses issues many others don't—for example, asking if you want pain medication to relieve suffering even if it makes you sleepy. It also has a blank space where people can specify a state in which they wouldn't want to be kept alive.
"Some people have a phrase that pops out in their mind: 'If I'm in the same condition as Aunt Mary,' " Mr. Malley says. Originally written in 1997, the Five Wishes will has been available online in an interactive format since last year.
Open to Interpretation
The problem with living wills is that most people can't articulate what they want, says ethicist Angela Fagerlin, co-director of the University of Michigan-affiliated Center for Bioethics and Social Sciences in Medicine in Ann Arbor. And even if they can, family members often don't properly interpret those wishes.
In a 400-patient study published in 2001, Dr. Fagerlin and colleagues found that family members who were presented with nine hypothetical scenarios correctly predicted patient wishes about 70% of the time, whether or not the patient had filled out a living will.
Can you forgo such documents completely? Mr. Callahan, who championed living wills in their early days, says he doesn't have one, preferring instead to give decision-making power to his wife, to whom he has said simply, "When in doubt, don't treat."
A health-care agent—a trusted family member, for instance—could supplant the need for a living will. Under the legal doctrine of "substituted judgment," health-care agents must try to make the decision you would if you could, says Alan Meisel, the director of the Center for Bioethics and Health Law at the University of Pittsburgh. Anything—a phone conversation, a list of instructions or a formal living will—can be used as evidence of your wishes, he adds.
As for my father, we postponed the decision, and he woke up, sharp as a tack, able to make his own decisions.
These critical documents about your preferences for end-of-life care don't always work as planned. More flexibility might be the answer.
Laura Johannes : WSJ : June 8, 2012
My father was in a coma, hooked up to a ventilator, and I had to make a tough call.
His living will expressed his desires for a few black-and-white situations: He didn't want to be kept alive if he was terminally ill, or in an irreversible vegetative state. But the situation I faced wasn't so simple. The neurologist said he would wake up from the coma, but there was a good chance he would have severe brain damage. How much of a chance? The doctors couldn't say.
Doctors and nurses say my heart-wrenching experience is typical of the complexity of real-life bedside decisions. An estimated 25% to 30% of Americans have filled out living wills, documents that spell out wishes for medical treatment. But ethicists say the typically simplistic documents aren't the solution many hoped they would be. Life-prolonging medical technology has far outstripped doctors' ability to predict outcomes. The hardest choices center on when quality of life will be so diminished that death is preferable.
As such, some health organizations are trying to improve living wills, allowing for more flexibility and nuance. Some ethicists, meanwhile, are de-emphasizing living wills altogether and focusing on appointing a trusted family member or friend as your health-care agent.
"Most of us have come to the conclusion that the way to get over the vagueness is to get someone to speak for you," says Robert M. Veatch, a professor of medical ethics at Georgetown University's Kennedy Institute of Ethics in Washington, D.C.
Living wills were created in the 1960s and gained national attention in the 1970s when a young woman, Karen Ann Quinlan, following alcohol and drug use at a party, was left in a vegetative state, raising alarms about medical technology keeping people alive in hopeless circumstances.
"We had a naive view that if you had a document, that would solve the problem," says Daniel Callahan, co-founder and president emeritus of the Hastings Center, a Garrison, N.Y., nonprofit that was an early champion of living wills. "In practice," he says, "all sorts of problems arise" that aren't spelled out in the documents.
When Paul Shalline, an active 86-year-old who regularly bested his grandchildren at ping pong, was unable to communicate after a severe stroke in March, treatment decisions fell to his daughter, Robin. Ms. Shalline, a 57-year-old teacher from Monkton, Vt., says her father had a living will but had never talked to her about his wishes. "There is so much gray area," she says. "You'd hope the living will would spell it all out, but it doesn't."
His living will called for withdrawing life support if there was no reasonable expectation of regaining a "meaningful quality of life" but didn't describe what that meant, she says. Ms. Shalline, when told by doctors that her father could be blind in one eye, unable to feed himself and might never walk again, made the decision to withdraw the ventilator based on "what I knew about his life." Mr. Shalline, who loved Wiffle ball and had recently helped build a staircase, was "proud of his 'physicalness,' " she says. He died March 18. It is hard enough, under the best of circumstances, to know what your family member would want in a particular situation. But add to that the fact that even top doctors can't predict outcomes very well.
Lee H. Schwamm, vice chairman of the neurology department at Massachusetts General Hospital in Boston, where Mr. Shalline was treated, says that even when he thinks he can predict a patient's outcome after a stroke, he is wrong 15% to 20% of the time on major outcome measures, such as whether a patient will be able to walk again. "I've never seen a living will—and I've seen a lot—that speaks to this question of diagnostic uncertainty," says Dr. Schwamm.
Living Documents
You can get a living will from a lawyer or download it from the Internet. Many focus on permanent comas and clearly hopeless conditions. Florida's statute-suggested living will, for example, directs life-prolonging treatments to be stopped if there is "no reasonable medical probability" of recovery from a terminal condition or persistent vegetative state. Florida, like most states, allows you to write your own living will; a few states, such as New Hampshire, specify that living wills must use a state-approved form. (A bill now being considered in New Hampshire would make the state form optional.)
A number of efforts have been made to improve on the standard-style living will. A document available online from Lifecare Directives LLC, Las Vegas, for example, spells out several levels of cognitive decline from coma to mental "confusion" that require 24-hour supervision, and asks if you would want life support if your brain failed that much. The document also gives you an option to say whether you want doctors to be "positively certain," "certain to a high degree" or "reasonably certain" that you will never recover before pulling the plug.
A simpler but also innovative approach is the popular Five Wishes living will. Five Wishes is written at a sixth- to seventh-grade level, says Paul Malley, president of Aging with Dignity, a nonprofit that distributes the document. Despite its simplicity, the Five Wishes living will addresses issues many others don't—for example, asking if you want pain medication to relieve suffering even if it makes you sleepy. It also has a blank space where people can specify a state in which they wouldn't want to be kept alive.
"Some people have a phrase that pops out in their mind: 'If I'm in the same condition as Aunt Mary,' " Mr. Malley says. Originally written in 1997, the Five Wishes will has been available online in an interactive format since last year.
Open to Interpretation
The problem with living wills is that most people can't articulate what they want, says ethicist Angela Fagerlin, co-director of the University of Michigan-affiliated Center for Bioethics and Social Sciences in Medicine in Ann Arbor. And even if they can, family members often don't properly interpret those wishes.
In a 400-patient study published in 2001, Dr. Fagerlin and colleagues found that family members who were presented with nine hypothetical scenarios correctly predicted patient wishes about 70% of the time, whether or not the patient had filled out a living will.
Can you forgo such documents completely? Mr. Callahan, who championed living wills in their early days, says he doesn't have one, preferring instead to give decision-making power to his wife, to whom he has said simply, "When in doubt, don't treat."
A health-care agent—a trusted family member, for instance—could supplant the need for a living will. Under the legal doctrine of "substituted judgment," health-care agents must try to make the decision you would if you could, says Alan Meisel, the director of the Center for Bioethics and Health Law at the University of Pittsburgh. Anything—a phone conversation, a list of instructions or a formal living will—can be used as evidence of your wishes, he adds.
As for my father, we postponed the decision, and he woke up, sharp as a tack, able to make his own decisions.
Living wills, other end of life decisions
and why a Health Care Proxy is a better idea in Massachusetts
End of Life Decisions
By Melinda Beck : WSJ Article : August 18, 2009
Forget about the health-reform debate for the moment. Should you have a living will specifying the kind of care you'd want at the end of life if you couldn't speak for yourself?
Doctors, lawmakers and ethicists have been urging Americans to fill out advance directives, as they are called, for decades. Yet less than a third of American adults, and less than half of nursing-home patients, have done so. Many people don't understand the options or the consequences, or they are baffled by the legalities, according to a report prepared for Congress last year by Rand Corp., and doctors and patients alike are reluctant to broach the subject of death.
"Everybody knows they're going to die, but it's really scary to think about how," says Audrey Seeley, a registered nurse in the stroke unit at Inova Hospital in Falls Church, Va., who sees many patients who are suddenly seriously incapacitated. "A lot of people say, 'If I get to that point, I don't care what happens to me.' But your family does."
Connie Paeglow works with elderly people and their families to discuss end-of-life preferences, including deciding on life-support care using the Five Wishes advanced-directives form.
Indeed, advance directives are as much for the living as for the dying. Without specific instructions, family members may have to decide whether you would want to be kept alive artificially, what level of disability you'd be willing to live with and how to let you die if you had no hope of recovery.
If family members aren't available, doctors are generally empowered to discontinue medical care they deem futile. But that rarely happens, largely for legal reasons, says Neil Wenger, director, UCLA Health System Ethics Center, and one of the authors of the Rand report. More often, he says, some family members are present and they want to keep terminal patients connected to life support and hope for a miracle.
Studies have found that most people would not want life-sustaining care if they were in an irreversible coma, Dr. Wenger notes. On the other hand, some patients want to be kept alive at all costs, and some religions require it. "Oftentimes, people think [advance directives] are just about ending life. But you can use them to request every intervention possible," says Jon Radulovic, a spokesman for the National Hospice and Palliative Care Organization.
Advance directives come in two varieties. A living will that sets out what kind of life-support care you would want in various situations, such as "if I become terminally ill or injured" or "if I become permanently unconscious." They can't anticipate every situation, so a second kind called a durable power of attorney for health care or a health-care proxy allows you to appoint someone to make health-care decisions for you.
Every state has its own versions and they are widely available online. The Caring Connections Web site of the National Hopsice and Palliative Care Organization has all 50 state forms available free at www.caringinfo.org/stateaddownload.
The Patient Self-Determination Act of 1991 requires all health-care facilities that receive Medicare or Medicaid funds to ask patients if they have advance directives and make them available. But that often occurs during the admitting process when a serious discussion is difficult.
"Five Wishes" is a less legalistic version that meets the legal requirements in 40 states. It's available from www.agingwithdignity.org for $5 a copy.
What you can specify:
Most state forms are brief, setting out hypothetical situations and giving options such as being put on a ventilator, receiving cardiopulmonary resuscitation, or receiving food or water artificially.
Five Wishes adds a third option in which you can specify that such life-support measures may be started, but then stopped if a doctor says they're not doing any good. It also asks whether you want to die at home or in a hospice and whether you would want pain medication, even if it put you to sleep. "Some people want to be awake and communicating with their family as long as possible," says Paul Malley, president of Aging with Dignity, which distributes Five Wishes. "Other people don't want to be in pain—it's their greatest fear."
Sometimes alleviating pain can also hasten death—and that's something patients should understand. "Most people want to live and they don't want to suffer and sometimes those can't both occur," says Christine Blasky, associate director of ICU at Salem Hospital in Salem, Mass.
"I put huge boxes and exclamation points around 'I do not want to be in pain,'" says Ms. Seeley, the stroke-unit nurse, who has filled out a Five Wishes form even though she is only 27. "I don't want somebody to have the burden of making a decision for me. I've seen it. It's gut-wrenching."
Connie Paeglow was given the Five Wishes form at a hospital in Denver when her husband, Wes, was diagnosed with cirrhosis of the liver and hepatitis C in 1998. He designated her as his health-care agent, said he didn't want to go on a ventilator if he couldn't breathe for himself and chose hospice care if his condition became terminal. Wes, who died in 2003, also specified that he wanted his favorite music—"Superman" by Five for Fighting—playing when hHaving all that in writing helped settle disputes with other family members, who wanted everything possible done for him, says Mrs. Paeglow, who now helps other families and patients with Five Wishes.
What do to with the forms:
Advance directives do not need to be filed officially. They go into effect automatically as soon as they are signed and witnessed; some states also require notarization. It's important to give your family members and doctors copies, or at least instructions on how to access them. Some states have electronic registries that store advance directives online. Google Health has started a similar free online service. See www.google.com/intl/en/health/advance-directive.html.
How to have the discussion:
The best time to begin considering advance directives is long before a health-care crisis looms. Having a doctor involved can be useful for answering medical questions. Medicare reimburses doctors for such discussions in some circumstances.
"We call these part of the important discussions in later life, along with 'When is it time to stop driving?' and 'When do you need help at home?'" says AARP President Jennie Chin Hansen. She adds that older people are often less reticent about discussing death than younger people suspect. "When you're 90 years old, it's not like you haven't thought about it, but it may be that nobody has ever asked you," she says.
Aging With Dignity's Next Steps booklet lists many possible ways to begin the conversation with loved ones, such as mentioning your own end-of-life preferences, or discussing the forms as a family group. "Everybody 18 and older should think of what they would want in case of an emergency. Let your family know, 'Here's what I value. Here's what's important to me,'" says Mr. Malley.
Are Living Wills the Answer?
By Drake Bennett
Whether they thinkher life was unduly prolonged or cruelly curtailed, one thing most people can agree on in the wake of Terri Schiavo's death is the importance of a living will: a document, also known as an ''advance directive,'' making clear the sort of care a person does and does not want should they find themselves unable to communicate their wishes. The nonprofit organization Aging with Dignity, distributor of one of the most popular living will forms, estimates a tenfold increase in requests due to the Schiavo case.
But how useful are living wills? According to many of the people actually responsible for drawing up and trying to follow such directives, not terribly. ''Enough. The living will has failed, and it is time to say so,'' Angela Fagerlin and Carl Schneider, a medical research scientist and a law professor, respectively, at the University of Michigan, declared last year in an article in the journal of the The Hastings Center, a bioethics research institute. And among counselors, doctors, and lawyers, that position isn't in fact so extreme.
For one thing, people change their minds, and a living will may be obsolete by the time its signer is in a condition to need it. As Steve O'Neill, a social worker and lawyer and the assistant director of the Ethics Support Service at Beth Israel Deaconess Medical Center, puts it, ''For any of us, what would be important to me now, at this point in my life, might be different from when I was 25 years old, before I had kids. Say you fill one out when you're 25 and you're now 75. Is it still accurate?''
Research suggests that such shifts are often large - Fagerlin and Schneider's meta-analysis of 11 such studies found that ''over periods as short as two years, almost one-third of preferences for life-sustaining medical treatments changed'' - and imperceptible enough that a person might not think there's any need to change their living will.
A person's attitude about living with a debilitating illness is especially likely to change when they find themselves ill. According to Diane Coleman, founder of the disability-rights organization Not Dead Yet, ''Disabled people are very familiar with this process. They think they'd rather die than live a certain way, then they discover, Oh gee, I don't feel that way after all.''' The difficulty, of course, is that the sorts of conditions in which a living will come into play are by definition those in which it's impossible to know whether a patient has changed his mind.
Even without such a reconsideration, circumstances can complicate what were originally simple medical instructions - especially when, as is often the case, the signer of the living will isn't terribly knowledgeable about medical matters in the first place. Nancy Coleman, director of the American Bar Association's Commission on Law and Aging (and no relation to Diane Coleman), offers the hypothetical example of a person who had signed a living will demanding not to be given health care if ill with a terminal disease or severe dementia. If that person were to develop Alzheimer's disease and then fall and break her hip, a literal interpretation of the living will would demand that nothing be done for the hip.
Hospital staff, therefore, tend to treat living wills not as strict instructions but as guides to a patient's general attitudes. Or they just ignore them, as several studies have shown. According to Jay D. Rosenbaum, a partner at the Boston law firm Palmer & Dodge currently teaching a wills and trusts class at Harvard Law School, ''Often, doctors do what doctors do notwithstanding any legal document.''
A better solution, according to many involved in end-of-life care situations, is to designate a health care proxy, someone entrusted to make medical decisions in one's stead. According to the ABA's Coleman, the result ''gives the patient an advocate and makes for a much stronger document.'' But this depends on the assumption that a proxy is acting in the patient's best interest. As both the Schiavo case and, closer to home, the recent protracted legal battle over the fate of Barbara Howe (a 79-year-old Dorchester woman with late-stage Lou Gehrig's disease) have made clear, such interests can be bitterly contested.
Designating a health care proxy also happens to be the only option for patients in Massachusetts, where living wills are not legally binding. Nevertheless, John J. Paris, a Jesuit priest and bioethics professor at Boston College, remains a staunch living will proponent: ''Massachusetts law certainly doesn't prohibit your drawing up a living will. Your proxy needs to know what you want. What's the best way of conveying that? Put it into writing.''
Living wills, for all their limits, are often the most complete source of information as to someone's wishes. ''We can never know what it is under every conceivable circumstance that someone would have wanted,'' says Paris. ''We can never have that level of certitude. At a certain point we have to take the existing best option. The perfect is sometimes the enemy of the good.”
Medical Due Diligence: A Living Will Should Spell Out the Specifics
By Jane E. Brody : Personal Health NY Times : November 28, 2006
When I ask people whether and how they have made preparations for the ends of their lives, the most frequent response is, “Well, I have a living will.” But chances are they are unaware of the serious limitations inherent in such a document and how it is likely to be interpreted by medical personnel should a life-threatening crisis arise.
A living will is an advance directive, a document that states your wishes about how you should be cared for at the end of your life. It is meant to be activated when you are unable to say what you do or do not want to be done medically — if, for example, you are in a terminal condition, your heart and breathing cease, you are in a persistent vegetative state because of severe brain damage or you are too demented to understand the situation.
A living will lists your general preferences for or against life-prolonging treatment like cardiopulmonary resuscitation if your heart suddenly stops, or mechanical respiration if you cannot breathe well enough on your own. But the simple statements contained in most living wills, more often than not, are hard to apply to the great variety of medical situations that can arise.
For example, let’s say you’re a 70-year-old active retiree with congestive heart failure who develops pneumonia and has trouble breathing. You go to the emergency room, living will in hand, stating that if you become terminally ill, you do not want to be treated with antibiotics or placed on a ventilator.
Open to Misinterpretation
The admitting physician reading your living will may interpret it as a “do not resuscitate,” or D.N.R., statement, meaning you want no treatment for your life-threatening infection, in which case you would probably die. Yet a course of antibiotics and a week or so with assisted breathing could restore you to your previously active state.
Dr. Ferdinando L. Mirarchi, chairman of emergency medicine at Hamot Medical Center in Erie, Pa., tells of a very active 64-year-old woman who nearly died because a nurse read her living will as a D.N.R. statement. The woman had slipped on ice and broken a leg, which was reset surgically. On the second postoperative day she began bleeding in her abdomen, and excreted and vomited blood. But the nurse saw her living will and told the physician on call that she was D.N.R. and thus did not warrant admission to the intensive care unit. Fortunately, another physician overrode the nurse’s interpretation and resuscitated the woman, who successfully underwent emergency surgery to stop the bleeding.
Living wills became popular — and were established as legally binding documents in all states except New York, Massachusetts and Michigan — after personal experiences and highly publicized cases like that of Terri Schiavo demonstrated the futility of prolonging lives that met few people’s definition of living.
Countless billions of dollars have been spent to support the hearts and lungs of people who will never leave the hospital alive. Many people, appalled by these torturously medicalized deaths, completed a notarized document to prevent this when they neared the end of their lives. About 20 percent of the population has a living will. But will it really help, or might it harm?
An Improved Document
Dr. Mirarchi has studied how health professionals interpret living wills and found that the overwhelming majority think they mean that the patient wants to be treated as D.N.R., when in fact aggressive life-saving interventions could restore some patients to their previous state of health.
Accordingly, he has devised a more comprehensive living will — an advance directive he calls a medical living will with “code status” — that people can fill out in consultation with their physicians and perhaps an attorney to help assure they get the kind of care they would want if they could ask for it. The “code status” tells medical personnel exactly how someone wants to be treated in a life-threatening medical emergency, removing the guesswork.
If, for example, you choose “full code,” the directive would say: “I would like to receive all lifesaving and supportive measures should an emergency arise. Should my condition fail to improve and I am no longer able to make my own decisions, then I would like my advance directive to be active and followed.”
Only at that point, then, would individually stated requests be honored, such as not being resuscitated, defibrillated, ventilated, fed by tube, transfused, given antibiotics or placed on a dialysis machine.
You could also choose “full code except cardiac arrest,” meaning that all measures short of restarting your stopped heart should be tried. Or let’s say you are a terminally ill cancer patient and recognize the futility of continued treatment. You could choose “comfort care, hospice care” and have only your symptoms treated to ease your departure from this life. Dr. Mirarchi’s reasons for the revised living will are spelled out in his forthcoming book, “Understanding Your Living Will: What You Need to Know Before a Medical Emergency” (Addicus Books).
Dr. Mirarchi strongly recommends that people periodically review and update their living wills as needs and medical conditions change. He points out that if you choose to be an organ donor, your living will should state that and give permission to temporarily suspend the document to preserve the viability of your organs.
Medical consultants writing in Patient Care (Nov. 15, 2000) noted that “the less inclusive a living will is, the more trouble it can cause.” Doctors may be uncomfortable following vague directives. The consultants suggested that living wills could be more useful if the directives were disease specific. For example, if you have emphysema, you may want to accept antibiotics and mechanical ventilation if you develop pneumonia, but you may not want such treatment if you are near death from cancer.
Your living will should also state that you (or your heirs) will not sue health care workers or facilities for following your stated wishes. The document can also call for a two-physician conference before life-prolonging treatments are withdrawn. The final document should be notarized.
Make several copies of your completed living will. File them with your personal physician or local medical center, your next of kin and attorney, and include a copy with your medical records and your last will and testament. You might also carry a wallet-size card stating your chosen “status code,” emergency information and name and phone number of your health care proxy.
Have a Health Care Proxy, Too
As may already be apparent, it is not enough to have a living will. You should also assign someone you trust to voice your medical wishes when you cannot speak for yourself. That person should first have a detailed conversation with you about how you want to be treated under various circumstances and also have a copy of your living will.
It may be best if that person has no vested interest in your estate and is younger than you. In most states, the health care proxy is recognized as acting for the patient, compelling medical personnel to follow the proxy’s instructions.
Finally, it should also be obvious that both a living will and a health care proxy should be in place as soon as a person turns 18 and becomes an adult in the eyes of the law. You never know how old or healthy you may be when its instructions are needed. Ms. Schiavo was only 26 when she suffered a brain-damaging cardiac arrest.
Making our wishes known
By Dr. Terry L. Schraeder : Boston Globe Article : December 5, 2006
Many people in my generation are watching and worrying as our parents get further and further into their senior years. My own 75-year-old mother's health is slowly but certainly ebbing. Each week there seems to be a new health issue that needs attention: something on her body to be scoped, or biopsied, X-rayed or MRI'd.
She and I talk about such things. But she has not yet fully shared her desires about her death -- about what she does and does not want to do when the end draws near. I am reluctant to ask too much. Even for me, her daughter and a doctor, it is a difficult conversation to have. Especially with the holidays at hand, who wants to talk about that? But having witnessed excruciating hospital bedside discussions occurring far too late or "do not resuscitate" orders being considered far too early, I can attest to the importance of discussing what doctors delicately call "end-of-life issues." We all need to ask our loved ones how they feel about organ donation, life support, and living wills. Anything in particular they want at the end? And we need to tell them of our own wishes. I don't want to be on a ventilator. Or I want everything possible to stay alive. I do not want to donate my organs. Or I do.
It seems particularly crazy to talk about these difficult issues at a holiday time . Yet this is the time of year when families are physically close together, and people who live far from their loved ones can have crucial conversations face to face.
This is also when we ask those closest to us, "What do you really want this year?" Instead of assuming we know what our spouse, parent, sibling, or friend desires for a gift (and to ensure we give them exactly what they want), we simply ask -- sometimes reluctantly, sometimes not so reluctantly. There are far more important issues that we should discuss in just as straightforward a manner.
"How can I make sure you have what you want when you can no longer speak for yourself?" we need to say.
And we need to ask, "Can I tell you now about what I want when I die?"
Unfortunately, baby boomers like me are truly unprepared for these issues. When we hit the senior years, we will make up a tidal wave of elderly. We will no doubt overwhelm our current system at a time when our society, nursing homes, healthcare, and government will least be able to help us. It is imperative that we talk about a plan with our loved ones now and try to put those plans in place, both personally by drafting a living will or advanced directive and financially by securing our insurance, savings plans, and wills.
As our own health fails and we can no longer maneuver through our multi-level homes or in our high-level sport utility vehicles -- and we may haveno children to take care of us -- we need to take responsibility for ourselves and our ultimate exits. Death itself won't be a suffering, isolating, and painful moment but a time when our loved ones and friends are near to us and we are leaving this life the way we want to.
Our generation has certainly taken on big issues and dilemmas before and managed them well. But unfortunately, when our time comes for nursing homes and advanced directives or hospice care, we may no longer have the intellectual capacity, influence, or energy to figure things out so well.
Putting our wishes on paper right now is easy. Living will forms are available from hospitals, attorneys, libraries, and the Internet. Organ donations cards are available from motor vehicle registries and at organdonor.gov.
If we all make our wishes clear, if we have discussions with those we love, perhaps we can help ensure the end is what we planned it to be.
This is what I want this year. What do you want?
Putting Muscle Behind End-of-Life Wishes
By Jane E. Brody : NY Times Article : February 24, 2009
My friend’s 94-year-old father was near death from congestive heart failure. He had requested in writing that no extraordinary measures be used to prolong his life; he wanted to die peacefully at home. But one day when he began struggling to breathe, my friend, his daughter, panicked and called 911.
Although the paramedics were told of his wishes, they followed established procedures and went right to work, helping him breathe and taking him to the hospital. But they told his distressed daughter that if he stopped breathing again, she should wait 20 minutes before calling 911, at which point resuscitation would not be possible. A few days later, her father died peacefully at home.
Millions of Americans have living wills that they think provide clear instructions to medical personnel about what should and should not be done if their lives hang in the balance and they cannot speak for themselves. Yet in case after case, study after study, it seems that these documents fail to result in the desired end among patients in hospitals and nursing homes.
Misconceptions
Now a new study confirms that confusion about interpreting living wills prevails in prehospital settings, as well. The study, conducted among 150 emergency medical technicians and paramedics by a team at Hamot Medical Center in Erie, Pa., and published this month in The Journal of Emergency Medicine, found that concern for patient safety can collide with confusion about the intent of living wills and do-not-resuscitate orders.
Even when a living will did not specifically say “do not resuscitate,” 90 percent of the emergency medical technicians and paramedics interpreted the mere existence of a living will to mean they should provide only comfort and end-of-life care and not attempt to save the person’s life.
“A living will does not necessarily say, ‘Do not treat me if I have a critical illness.’ This is a major misconception,” said Dr. Ferdinando Mirarchi, the director of emergency medicine at Hamot and the director of the study.
The study did find that when the living will incorporated a code status, like “full code,” meaning that every effort should be made to resuscitate the patient, it was much more likely that emergency responders would provide life-saving care.
But more often than not, the reverse situation occurs. Patients who have clearly specified that no attempt should be made to prolong life if they become unresponsive are nonetheless resuscitated or hooked up to respirators and feeding tubes.
Uncooperative Doctors
In “To Die Well,” Dr. Sidney Wanzer, a co-author, relates the experience of his 92-year-old mother, who was living in a nursing home with advanced Alzheimer’s disease. Long before the disease had overtaken her mind, he wrote, she had completed a living will stating that “she did not want her death prolonged by medical treatment if the quality of her life ever became so poor that there was no significant intellectual activity or reward.” Yet when her heart developed an irregular rhythm that would have soon been fatal, the doctor in charge implanted a pacemaker, which kept her alive another five years in a helpless state “lacking all dignity, totally contrary to her written request,” Dr. Wanzer wrote.
“I thought everything was all set,” he continued. “But we made a big mistake. We did not ask her doctor explicitly, ‘Do you agree with this approach and will you promise to adhere to our mother’s wishes?’ ”
As more and more Americans live beyond the eighth decade, when the risk of dementia rises significantly, cases in which a doctor chooses medical intervention — in the presence or absence of a patient’s wishes — are likely to become more common. Yet in a 1999 study by Dr. Dwenda K. Gjerdingen and colleagues at the University of Minnesota among 84 cognitively normal men and women 65 and older, three-fourths said they would not want to be resuscitated, put on a respirator or nourished by a feeding tube at the end of life if they had mild dementia, and 95 percent would reject such measures if they had severe dementia.
A costly, four-year, multicenter study begun in 1989 sought to improve doctors’ ability to interpret and carry out patients’ wishes for end-of-life care. Yet informing doctors of what hospitalized patients wanted and placing that information in the medical records did nothing to influence the care they provided. Having a living will had no effect on whether doctors used resuscitative efforts at the end of life. The doctors, it seemed, simply could not let patients go even if that was a patient’s explicit wish.
Help for First Responders
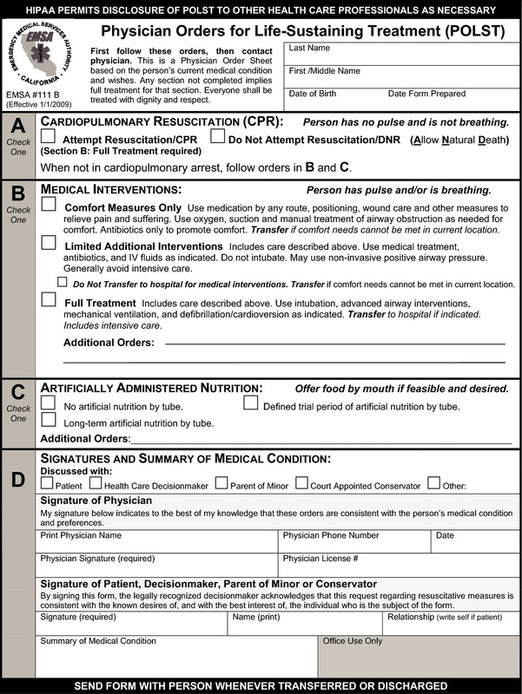
Last year, a law went into effect in New York State to help solve the problem of emergency responders’ being forced to give invasive care to people at the end of life, even if that is contrary to the wishes of the dying person and relatives.
The law allows the use of a bright pink form, the Medical Orders for Life-Sustaining Treatment form, which lets people to indicate whether they would want intravenous fluids, medications like antibiotics, a feeding tube, a breathing tube or other interventions, and whether they want to go to a hospital. On the form, which is signed by a physician and is considered a medical order, patients can also specify that they want only comfort care or would want a trial of certain treatments.
Before the law was passed, the only directive emergency technicians could obey was an out-of-hospital “do not resuscitate” form specifying that no cardiopulmonary resuscitation be tried if a patient stopped breathing or had no pulse. Not covered were the myriad cases like that of my friend’s father, in which patients were near the end of life but not in cardiac arrest.
California, North Carolina, Oregon, Washington, West Virginia and parts of Wisconsin also have programs that use these physicians’ order forms to clarify treatment and end-of-life decisions for medical personnel. Programs are being developed in still other states.
Can similar improvements in adherence to advance directives be made for all of us, including hospitalized patients? One approach is to assign a trusted person to be your health care proxy, to hold dual power of attorney for health care when you are unable to make your wishes known to medical personnel. Discuss your wishes under various conditions with that person, give the person your detailed living will and complete a health care proxy form. Update the information if your feelings change.
My husband and I carry our proxy forms in our wallets, to help medical personnel figure out whom to contact in an emergency and how to proceed in accordance with our wishes.
You can find more information about advance directives and other end-of-life issues in the newly published “Jane Brody’s Guide to the Great Beyond” (Random House).
By Melinda Beck : WSJ Article : August 18, 2009
Forget about the health-reform debate for the moment. Should you have a living will specifying the kind of care you'd want at the end of life if you couldn't speak for yourself?
Doctors, lawmakers and ethicists have been urging Americans to fill out advance directives, as they are called, for decades. Yet less than a third of American adults, and less than half of nursing-home patients, have done so. Many people don't understand the options or the consequences, or they are baffled by the legalities, according to a report prepared for Congress last year by Rand Corp., and doctors and patients alike are reluctant to broach the subject of death.
"Everybody knows they're going to die, but it's really scary to think about how," says Audrey Seeley, a registered nurse in the stroke unit at Inova Hospital in Falls Church, Va., who sees many patients who are suddenly seriously incapacitated. "A lot of people say, 'If I get to that point, I don't care what happens to me.' But your family does."
Connie Paeglow works with elderly people and their families to discuss end-of-life preferences, including deciding on life-support care using the Five Wishes advanced-directives form.
Indeed, advance directives are as much for the living as for the dying. Without specific instructions, family members may have to decide whether you would want to be kept alive artificially, what level of disability you'd be willing to live with and how to let you die if you had no hope of recovery.
If family members aren't available, doctors are generally empowered to discontinue medical care they deem futile. But that rarely happens, largely for legal reasons, says Neil Wenger, director, UCLA Health System Ethics Center, and one of the authors of the Rand report. More often, he says, some family members are present and they want to keep terminal patients connected to life support and hope for a miracle.
Studies have found that most people would not want life-sustaining care if they were in an irreversible coma, Dr. Wenger notes. On the other hand, some patients want to be kept alive at all costs, and some religions require it. "Oftentimes, people think [advance directives] are just about ending life. But you can use them to request every intervention possible," says Jon Radulovic, a spokesman for the National Hospice and Palliative Care Organization.
Advance directives come in two varieties. A living will that sets out what kind of life-support care you would want in various situations, such as "if I become terminally ill or injured" or "if I become permanently unconscious." They can't anticipate every situation, so a second kind called a durable power of attorney for health care or a health-care proxy allows you to appoint someone to make health-care decisions for you.
Every state has its own versions and they are widely available online. The Caring Connections Web site of the National Hopsice and Palliative Care Organization has all 50 state forms available free at www.caringinfo.org/stateaddownload.
The Patient Self-Determination Act of 1991 requires all health-care facilities that receive Medicare or Medicaid funds to ask patients if they have advance directives and make them available. But that often occurs during the admitting process when a serious discussion is difficult.
"Five Wishes" is a less legalistic version that meets the legal requirements in 40 states. It's available from www.agingwithdignity.org for $5 a copy.
What you can specify:
Most state forms are brief, setting out hypothetical situations and giving options such as being put on a ventilator, receiving cardiopulmonary resuscitation, or receiving food or water artificially.
Five Wishes adds a third option in which you can specify that such life-support measures may be started, but then stopped if a doctor says they're not doing any good. It also asks whether you want to die at home or in a hospice and whether you would want pain medication, even if it put you to sleep. "Some people want to be awake and communicating with their family as long as possible," says Paul Malley, president of Aging with Dignity, which distributes Five Wishes. "Other people don't want to be in pain—it's their greatest fear."
Sometimes alleviating pain can also hasten death—and that's something patients should understand. "Most people want to live and they don't want to suffer and sometimes those can't both occur," says Christine Blasky, associate director of ICU at Salem Hospital in Salem, Mass.
"I put huge boxes and exclamation points around 'I do not want to be in pain,'" says Ms. Seeley, the stroke-unit nurse, who has filled out a Five Wishes form even though she is only 27. "I don't want somebody to have the burden of making a decision for me. I've seen it. It's gut-wrenching."
Connie Paeglow was given the Five Wishes form at a hospital in Denver when her husband, Wes, was diagnosed with cirrhosis of the liver and hepatitis C in 1998. He designated her as his health-care agent, said he didn't want to go on a ventilator if he couldn't breathe for himself and chose hospice care if his condition became terminal. Wes, who died in 2003, also specified that he wanted his favorite music—"Superman" by Five for Fighting—playing when hHaving all that in writing helped settle disputes with other family members, who wanted everything possible done for him, says Mrs. Paeglow, who now helps other families and patients with Five Wishes.
What do to with the forms:
Advance directives do not need to be filed officially. They go into effect automatically as soon as they are signed and witnessed; some states also require notarization. It's important to give your family members and doctors copies, or at least instructions on how to access them. Some states have electronic registries that store advance directives online. Google Health has started a similar free online service. See www.google.com/intl/en/health/advance-directive.html.
How to have the discussion:
The best time to begin considering advance directives is long before a health-care crisis looms. Having a doctor involved can be useful for answering medical questions. Medicare reimburses doctors for such discussions in some circumstances.
"We call these part of the important discussions in later life, along with 'When is it time to stop driving?' and 'When do you need help at home?'" says AARP President Jennie Chin Hansen. She adds that older people are often less reticent about discussing death than younger people suspect. "When you're 90 years old, it's not like you haven't thought about it, but it may be that nobody has ever asked you," she says.
Aging With Dignity's Next Steps booklet lists many possible ways to begin the conversation with loved ones, such as mentioning your own end-of-life preferences, or discussing the forms as a family group. "Everybody 18 and older should think of what they would want in case of an emergency. Let your family know, 'Here's what I value. Here's what's important to me,'" says Mr. Malley.
Are Living Wills the Answer?
By Drake Bennett
Whether they thinkher life was unduly prolonged or cruelly curtailed, one thing most people can agree on in the wake of Terri Schiavo's death is the importance of a living will: a document, also known as an ''advance directive,'' making clear the sort of care a person does and does not want should they find themselves unable to communicate their wishes. The nonprofit organization Aging with Dignity, distributor of one of the most popular living will forms, estimates a tenfold increase in requests due to the Schiavo case.
But how useful are living wills? According to many of the people actually responsible for drawing up and trying to follow such directives, not terribly. ''Enough. The living will has failed, and it is time to say so,'' Angela Fagerlin and Carl Schneider, a medical research scientist and a law professor, respectively, at the University of Michigan, declared last year in an article in the journal of the The Hastings Center, a bioethics research institute. And among counselors, doctors, and lawyers, that position isn't in fact so extreme.
For one thing, people change their minds, and a living will may be obsolete by the time its signer is in a condition to need it. As Steve O'Neill, a social worker and lawyer and the assistant director of the Ethics Support Service at Beth Israel Deaconess Medical Center, puts it, ''For any of us, what would be important to me now, at this point in my life, might be different from when I was 25 years old, before I had kids. Say you fill one out when you're 25 and you're now 75. Is it still accurate?''
Research suggests that such shifts are often large - Fagerlin and Schneider's meta-analysis of 11 such studies found that ''over periods as short as two years, almost one-third of preferences for life-sustaining medical treatments changed'' - and imperceptible enough that a person might not think there's any need to change their living will.
A person's attitude about living with a debilitating illness is especially likely to change when they find themselves ill. According to Diane Coleman, founder of the disability-rights organization Not Dead Yet, ''Disabled people are very familiar with this process. They think they'd rather die than live a certain way, then they discover, Oh gee, I don't feel that way after all.''' The difficulty, of course, is that the sorts of conditions in which a living will come into play are by definition those in which it's impossible to know whether a patient has changed his mind.
Even without such a reconsideration, circumstances can complicate what were originally simple medical instructions - especially when, as is often the case, the signer of the living will isn't terribly knowledgeable about medical matters in the first place. Nancy Coleman, director of the American Bar Association's Commission on Law and Aging (and no relation to Diane Coleman), offers the hypothetical example of a person who had signed a living will demanding not to be given health care if ill with a terminal disease or severe dementia. If that person were to develop Alzheimer's disease and then fall and break her hip, a literal interpretation of the living will would demand that nothing be done for the hip.
Hospital staff, therefore, tend to treat living wills not as strict instructions but as guides to a patient's general attitudes. Or they just ignore them, as several studies have shown. According to Jay D. Rosenbaum, a partner at the Boston law firm Palmer & Dodge currently teaching a wills and trusts class at Harvard Law School, ''Often, doctors do what doctors do notwithstanding any legal document.''
A better solution, according to many involved in end-of-life care situations, is to designate a health care proxy, someone entrusted to make medical decisions in one's stead. According to the ABA's Coleman, the result ''gives the patient an advocate and makes for a much stronger document.'' But this depends on the assumption that a proxy is acting in the patient's best interest. As both the Schiavo case and, closer to home, the recent protracted legal battle over the fate of Barbara Howe (a 79-year-old Dorchester woman with late-stage Lou Gehrig's disease) have made clear, such interests can be bitterly contested.
Designating a health care proxy also happens to be the only option for patients in Massachusetts, where living wills are not legally binding. Nevertheless, John J. Paris, a Jesuit priest and bioethics professor at Boston College, remains a staunch living will proponent: ''Massachusetts law certainly doesn't prohibit your drawing up a living will. Your proxy needs to know what you want. What's the best way of conveying that? Put it into writing.''
Living wills, for all their limits, are often the most complete source of information as to someone's wishes. ''We can never know what it is under every conceivable circumstance that someone would have wanted,'' says Paris. ''We can never have that level of certitude. At a certain point we have to take the existing best option. The perfect is sometimes the enemy of the good.”
Medical Due Diligence: A Living Will Should Spell Out the Specifics
By Jane E. Brody : Personal Health NY Times : November 28, 2006
When I ask people whether and how they have made preparations for the ends of their lives, the most frequent response is, “Well, I have a living will.” But chances are they are unaware of the serious limitations inherent in such a document and how it is likely to be interpreted by medical personnel should a life-threatening crisis arise.
A living will is an advance directive, a document that states your wishes about how you should be cared for at the end of your life. It is meant to be activated when you are unable to say what you do or do not want to be done medically — if, for example, you are in a terminal condition, your heart and breathing cease, you are in a persistent vegetative state because of severe brain damage or you are too demented to understand the situation.
A living will lists your general preferences for or against life-prolonging treatment like cardiopulmonary resuscitation if your heart suddenly stops, or mechanical respiration if you cannot breathe well enough on your own. But the simple statements contained in most living wills, more often than not, are hard to apply to the great variety of medical situations that can arise.
For example, let’s say you’re a 70-year-old active retiree with congestive heart failure who develops pneumonia and has trouble breathing. You go to the emergency room, living will in hand, stating that if you become terminally ill, you do not want to be treated with antibiotics or placed on a ventilator.
Open to Misinterpretation
The admitting physician reading your living will may interpret it as a “do not resuscitate,” or D.N.R., statement, meaning you want no treatment for your life-threatening infection, in which case you would probably die. Yet a course of antibiotics and a week or so with assisted breathing could restore you to your previously active state.
Dr. Ferdinando L. Mirarchi, chairman of emergency medicine at Hamot Medical Center in Erie, Pa., tells of a very active 64-year-old woman who nearly died because a nurse read her living will as a D.N.R. statement. The woman had slipped on ice and broken a leg, which was reset surgically. On the second postoperative day she began bleeding in her abdomen, and excreted and vomited blood. But the nurse saw her living will and told the physician on call that she was D.N.R. and thus did not warrant admission to the intensive care unit. Fortunately, another physician overrode the nurse’s interpretation and resuscitated the woman, who successfully underwent emergency surgery to stop the bleeding.
Living wills became popular — and were established as legally binding documents in all states except New York, Massachusetts and Michigan — after personal experiences and highly publicized cases like that of Terri Schiavo demonstrated the futility of prolonging lives that met few people’s definition of living.
Countless billions of dollars have been spent to support the hearts and lungs of people who will never leave the hospital alive. Many people, appalled by these torturously medicalized deaths, completed a notarized document to prevent this when they neared the end of their lives. About 20 percent of the population has a living will. But will it really help, or might it harm?
An Improved Document
Dr. Mirarchi has studied how health professionals interpret living wills and found that the overwhelming majority think they mean that the patient wants to be treated as D.N.R., when in fact aggressive life-saving interventions could restore some patients to their previous state of health.
Accordingly, he has devised a more comprehensive living will — an advance directive he calls a medical living will with “code status” — that people can fill out in consultation with their physicians and perhaps an attorney to help assure they get the kind of care they would want if they could ask for it. The “code status” tells medical personnel exactly how someone wants to be treated in a life-threatening medical emergency, removing the guesswork.
If, for example, you choose “full code,” the directive would say: “I would like to receive all lifesaving and supportive measures should an emergency arise. Should my condition fail to improve and I am no longer able to make my own decisions, then I would like my advance directive to be active and followed.”
Only at that point, then, would individually stated requests be honored, such as not being resuscitated, defibrillated, ventilated, fed by tube, transfused, given antibiotics or placed on a dialysis machine.
You could also choose “full code except cardiac arrest,” meaning that all measures short of restarting your stopped heart should be tried. Or let’s say you are a terminally ill cancer patient and recognize the futility of continued treatment. You could choose “comfort care, hospice care” and have only your symptoms treated to ease your departure from this life. Dr. Mirarchi’s reasons for the revised living will are spelled out in his forthcoming book, “Understanding Your Living Will: What You Need to Know Before a Medical Emergency” (Addicus Books).
Dr. Mirarchi strongly recommends that people periodically review and update their living wills as needs and medical conditions change. He points out that if you choose to be an organ donor, your living will should state that and give permission to temporarily suspend the document to preserve the viability of your organs.
Medical consultants writing in Patient Care (Nov. 15, 2000) noted that “the less inclusive a living will is, the more trouble it can cause.” Doctors may be uncomfortable following vague directives. The consultants suggested that living wills could be more useful if the directives were disease specific. For example, if you have emphysema, you may want to accept antibiotics and mechanical ventilation if you develop pneumonia, but you may not want such treatment if you are near death from cancer.
Your living will should also state that you (or your heirs) will not sue health care workers or facilities for following your stated wishes. The document can also call for a two-physician conference before life-prolonging treatments are withdrawn. The final document should be notarized.
Make several copies of your completed living will. File them with your personal physician or local medical center, your next of kin and attorney, and include a copy with your medical records and your last will and testament. You might also carry a wallet-size card stating your chosen “status code,” emergency information and name and phone number of your health care proxy.
Have a Health Care Proxy, Too
As may already be apparent, it is not enough to have a living will. You should also assign someone you trust to voice your medical wishes when you cannot speak for yourself. That person should first have a detailed conversation with you about how you want to be treated under various circumstances and also have a copy of your living will.
It may be best if that person has no vested interest in your estate and is younger than you. In most states, the health care proxy is recognized as acting for the patient, compelling medical personnel to follow the proxy’s instructions.
Finally, it should also be obvious that both a living will and a health care proxy should be in place as soon as a person turns 18 and becomes an adult in the eyes of the law. You never know how old or healthy you may be when its instructions are needed. Ms. Schiavo was only 26 when she suffered a brain-damaging cardiac arrest.
Making our wishes known
By Dr. Terry L. Schraeder : Boston Globe Article : December 5, 2006
Many people in my generation are watching and worrying as our parents get further and further into their senior years. My own 75-year-old mother's health is slowly but certainly ebbing. Each week there seems to be a new health issue that needs attention: something on her body to be scoped, or biopsied, X-rayed or MRI'd.
She and I talk about such things. But she has not yet fully shared her desires about her death -- about what she does and does not want to do when the end draws near. I am reluctant to ask too much. Even for me, her daughter and a doctor, it is a difficult conversation to have. Especially with the holidays at hand, who wants to talk about that? But having witnessed excruciating hospital bedside discussions occurring far too late or "do not resuscitate" orders being considered far too early, I can attest to the importance of discussing what doctors delicately call "end-of-life issues." We all need to ask our loved ones how they feel about organ donation, life support, and living wills. Anything in particular they want at the end? And we need to tell them of our own wishes. I don't want to be on a ventilator. Or I want everything possible to stay alive. I do not want to donate my organs. Or I do.
It seems particularly crazy to talk about these difficult issues at a holiday time . Yet this is the time of year when families are physically close together, and people who live far from their loved ones can have crucial conversations face to face.
This is also when we ask those closest to us, "What do you really want this year?" Instead of assuming we know what our spouse, parent, sibling, or friend desires for a gift (and to ensure we give them exactly what they want), we simply ask -- sometimes reluctantly, sometimes not so reluctantly. There are far more important issues that we should discuss in just as straightforward a manner.
"How can I make sure you have what you want when you can no longer speak for yourself?" we need to say.
And we need to ask, "Can I tell you now about what I want when I die?"
Unfortunately, baby boomers like me are truly unprepared for these issues. When we hit the senior years, we will make up a tidal wave of elderly. We will no doubt overwhelm our current system at a time when our society, nursing homes, healthcare, and government will least be able to help us. It is imperative that we talk about a plan with our loved ones now and try to put those plans in place, both personally by drafting a living will or advanced directive and financially by securing our insurance, savings plans, and wills.
As our own health fails and we can no longer maneuver through our multi-level homes or in our high-level sport utility vehicles -- and we may haveno children to take care of us -- we need to take responsibility for ourselves and our ultimate exits. Death itself won't be a suffering, isolating, and painful moment but a time when our loved ones and friends are near to us and we are leaving this life the way we want to.
Our generation has certainly taken on big issues and dilemmas before and managed them well. But unfortunately, when our time comes for nursing homes and advanced directives or hospice care, we may no longer have the intellectual capacity, influence, or energy to figure things out so well.
Putting our wishes on paper right now is easy. Living will forms are available from hospitals, attorneys, libraries, and the Internet. Organ donations cards are available from motor vehicle registries and at organdonor.gov.
If we all make our wishes clear, if we have discussions with those we love, perhaps we can help ensure the end is what we planned it to be.
This is what I want this year. What do you want?
Putting Muscle Behind End-of-Life Wishes
By Jane E. Brody : NY Times Article : February 24, 2009
My friend’s 94-year-old father was near death from congestive heart failure. He had requested in writing that no extraordinary measures be used to prolong his life; he wanted to die peacefully at home. But one day when he began struggling to breathe, my friend, his daughter, panicked and called 911.
Although the paramedics were told of his wishes, they followed established procedures and went right to work, helping him breathe and taking him to the hospital. But they told his distressed daughter that if he stopped breathing again, she should wait 20 minutes before calling 911, at which point resuscitation would not be possible. A few days later, her father died peacefully at home.
Millions of Americans have living wills that they think provide clear instructions to medical personnel about what should and should not be done if their lives hang in the balance and they cannot speak for themselves. Yet in case after case, study after study, it seems that these documents fail to result in the desired end among patients in hospitals and nursing homes.
Misconceptions
Now a new study confirms that confusion about interpreting living wills prevails in prehospital settings, as well. The study, conducted among 150 emergency medical technicians and paramedics by a team at Hamot Medical Center in Erie, Pa., and published this month in The Journal of Emergency Medicine, found that concern for patient safety can collide with confusion about the intent of living wills and do-not-resuscitate orders.
Even when a living will did not specifically say “do not resuscitate,” 90 percent of the emergency medical technicians and paramedics interpreted the mere existence of a living will to mean they should provide only comfort and end-of-life care and not attempt to save the person’s life.
“A living will does not necessarily say, ‘Do not treat me if I have a critical illness.’ This is a major misconception,” said Dr. Ferdinando Mirarchi, the director of emergency medicine at Hamot and the director of the study.
The study did find that when the living will incorporated a code status, like “full code,” meaning that every effort should be made to resuscitate the patient, it was much more likely that emergency responders would provide life-saving care.
But more often than not, the reverse situation occurs. Patients who have clearly specified that no attempt should be made to prolong life if they become unresponsive are nonetheless resuscitated or hooked up to respirators and feeding tubes.
Uncooperative Doctors
In “To Die Well,” Dr. Sidney Wanzer, a co-author, relates the experience of his 92-year-old mother, who was living in a nursing home with advanced Alzheimer’s disease. Long before the disease had overtaken her mind, he wrote, she had completed a living will stating that “she did not want her death prolonged by medical treatment if the quality of her life ever became so poor that there was no significant intellectual activity or reward.” Yet when her heart developed an irregular rhythm that would have soon been fatal, the doctor in charge implanted a pacemaker, which kept her alive another five years in a helpless state “lacking all dignity, totally contrary to her written request,” Dr. Wanzer wrote.
“I thought everything was all set,” he continued. “But we made a big mistake. We did not ask her doctor explicitly, ‘Do you agree with this approach and will you promise to adhere to our mother’s wishes?’ ”
As more and more Americans live beyond the eighth decade, when the risk of dementia rises significantly, cases in which a doctor chooses medical intervention — in the presence or absence of a patient’s wishes — are likely to become more common. Yet in a 1999 study by Dr. Dwenda K. Gjerdingen and colleagues at the University of Minnesota among 84 cognitively normal men and women 65 and older, three-fourths said they would not want to be resuscitated, put on a respirator or nourished by a feeding tube at the end of life if they had mild dementia, and 95 percent would reject such measures if they had severe dementia.
A costly, four-year, multicenter study begun in 1989 sought to improve doctors’ ability to interpret and carry out patients’ wishes for end-of-life care. Yet informing doctors of what hospitalized patients wanted and placing that information in the medical records did nothing to influence the care they provided. Having a living will had no effect on whether doctors used resuscitative efforts at the end of life. The doctors, it seemed, simply could not let patients go even if that was a patient’s explicit wish.
Help for First Responders
Last year, a law went into effect in New York State to help solve the problem of emergency responders’ being forced to give invasive care to people at the end of life, even if that is contrary to the wishes of the dying person and relatives.
The law allows the use of a bright pink form, the Medical Orders for Life-Sustaining Treatment form, which lets people to indicate whether they would want intravenous fluids, medications like antibiotics, a feeding tube, a breathing tube or other interventions, and whether they want to go to a hospital. On the form, which is signed by a physician and is considered a medical order, patients can also specify that they want only comfort care or would want a trial of certain treatments.
Before the law was passed, the only directive emergency technicians could obey was an out-of-hospital “do not resuscitate” form specifying that no cardiopulmonary resuscitation be tried if a patient stopped breathing or had no pulse. Not covered were the myriad cases like that of my friend’s father, in which patients were near the end of life but not in cardiac arrest.
California, North Carolina, Oregon, Washington, West Virginia and parts of Wisconsin also have programs that use these physicians’ order forms to clarify treatment and end-of-life decisions for medical personnel. Programs are being developed in still other states.
Can similar improvements in adherence to advance directives be made for all of us, including hospitalized patients? One approach is to assign a trusted person to be your health care proxy, to hold dual power of attorney for health care when you are unable to make your wishes known to medical personnel. Discuss your wishes under various conditions with that person, give the person your detailed living will and complete a health care proxy form. Update the information if your feelings change.
My husband and I carry our proxy forms in our wallets, to help medical personnel figure out whom to contact in an emergency and how to proceed in accordance with our wishes.
You can find more information about advance directives and other end-of-life issues in the newly published “Jane Brody’s Guide to the Great Beyond” (Random House).
New Efforts to Simplify End-of-Life Care Wishes
By Laura Landro : WSJ : March 14, 2011
Advance directives, which allow people to plan ahead for end-of-life care, can be too vague to cover many medical situations. Now, a growing number of states are promoting another program to help guide physicians with a patient's specific instructions.
The programs are known as Physician Orders for Life-Sustaining Treatment, or Polst. They are meant to complement advance directives, sometimes known as living wills, in which people state in broad terms how much medical intervention they will want when their condition no longer allows them to communicate. A Polst, which is signed by both the patient and the doctor, spells out such choices as whether a patient wants to be on a mechanical breathing machine or feeding tube and receive antibiotics.
Polst programs are currently in use in 14 states and regions, including California, Oregon and New York. Three states, Colorado, Idaho and Pennsylvania, adopted Polst programs recently, and another 16 states and six regions are developing programs. Besides providing documents that meet local regulations, the programs train health-care providers to discuss end-of-life treatment choices with patients with terminal illness or anyone wishing to define their care preferences.
"More than 75% of people will be unable to make some or all of their own medical decisions at the end of life, but we don't prepare patients and their families to deal with this situation, and it's frightening and difficult for them to know what to do," says Rebecca Sudore, a physician at the University of California, San Francisco and the city's VA Medical Center.
Planning ahead for end-of-life care is meant to allow patients to reduce the amount of medical intervention, if that's what they prefer. But patients also can make clear their wishes if they prefer maximum intervention.
Planning Ahead
Advance directives allow patients to make their end-of-life wishes known in the event they are unable to communicate.
Here are some typical advance directives:
A living will: This instructs family and medical providers on the treatments that a patient wants to receive. The most common decisions involve these life-sustaining treatments:
a) Cardiopulmonary resuscitation (CPR): Used when a patient's heart or breathing stops.
b) A Do Not Resuscitate (DNR) order: A written physician's order that prevents the health-care team from initiating CPR.
c) A Do Not Intubate (DNI) order: Intubation is the placement of a tube into the nose or mouth in order to have it enter the windpipe (trachea) to help the patient breathe.
d) Artificial nutrition and hydration: Used when patients are no longer able to take food and fluid by mouth.
Medical power of attorney lets patients select someone else, usually a family member or close friend, to make care decisions when patients are temporarily or permanently unable to communicate or make decisions on their own.
Physician Orders for Life-Sustaining Treatment, or Polst, is a medical order form signed by the patient and the doctor. It becomes part of the patient's medical record and provides specific instructions to the medical team on such issues as the use of mechanical breathing machines and feeding tubes.
A Polst form is an official medical order, says Susan Tolle, director of the Center for Ethics in Health Care at Oregon Health & Science University, a developer of the Polst program. Unlike an advance directive, which can be misplaced or vaguely worded, a Polst spells out specific treatment instructions and remains part of a patient's medical record. In Oregon, for example, the documents also are stored in a state registry so emergency medical technicians as well as hospitals have access to them. States that have adopted the Polst program also have put in place general protections for medical personnel who follow the directives.
Advance directives, which also allow people to designate a surrogate to make decisions about care, vary state by state. While some states' forms may be highly specific, they may be printed out and stored somewhere where they can't be found when needed. Many states also accept other documents such as a form called Five Wishes that allows people to spell out what kind of quality of life they want, and make requests such as having their bodies massaged with oils for comfort.
A study supported by the National Institutes of Health last year found that patients with Polst forms were more likely to have treatment preferences documented than patients who used traditional documents such as living wills and do-not-resuscitate orders.
Making end-of-life decisions when a loved one's wishes are not known can be difficult for families. After years of struggling with Parkinson's disease and congestive heart failure, Nancy Williamson's mother became seriously ill last August and slipped into a coma from which doctors said she would never recover. Although Ms. Williamson and her sisters wanted doctors to do more, they learned that their mother had signed a Polst form asking for only limited medical treatment.
Ms. Williamson, a California lawyer, says that after arguing with doctors because she wanted to hold on to her mother, "I realized having the Polst made it easier for us because my mom had made her own health-care decisions." The experience led her to help clients prepare end-of-life documents, Ms. Williamson says.
End-of-life directives are controversial. Anti-abortion group LifeTree Inc., for example, opposes the signing of living wills and says life sustaining treatment should always be administered. Elizabeth D. Wickham, the group's executive director, says Polst programs provide legal protection to medical personnel for hastening death, thus encouraging imposed death on patients.
Studies show that many elderly patients prefer to limit medical interventions. In one study of hospice patients, 79% wanted comfort measures only, and 20% wanted only limited additional interventions such as intravenous fluids and antibiotics. In another study only 12% of residents of a long-term skilled nursing facility wanted intensive-care unit treatment that would put them on a breathing machine.
Physicians often don't have the time or training to coach patients through end-of-life-care conversations, says Bernard Hammes, chairman of a national task force that helps develop Polst programs. In a program he designed at the Gunderson Lutheran Health System in LaCrosse, Wis., nurses, social workers, chaplains and others are trained as advance care planning facilitators to help patients and families discuss and document end of life wishes.
The program, Respecting Choices, has been used as a model by dozens of health systems in the U.S. and overseas. Dr. Hammes says studies at Gunderson Lutheran have shown patients with advanced illness who have documented their wishes are more likely to prefer that their care be focused on comfort and function. They are also less likely to want to have their final medical care in a hospital, or to have interventions like CPR attempted. Those patients also use about $2,000 less in physician and hospital services in the last six months of life, a time when the highest medical expenses often occur, he says.
Insurer Aetna began using nurse-care managers to help manage both Medicare and commercially insured patients with terminal illness in 2004, using telephone consultations with patients, doctors and families to, among other things, ensure advance directives are in place and complied with. As a result of the program, a higher proportion of members elected hospice care compared to prior years, which was associated with a decrease in the use of acute care, intensive care and emergency services, particularly for Medicare Advantage beneficiaries. Precise cost reductions couldn't be determined for patients in Medicare because it paid the costs directly, Aetna said. But in the commercially insured population, the program led to a net medical cost decrease of 22% compared to a control group not using the care-management services.
Aetna has extended its terminal-illness-care management to all eligible members. "No one is suggesting that anyone be pushed in any specific direction about the choices they make for end-of-life care," says Randall Krakauer, Aetna's head of Medicare medical management. But because such choices often aren't known at a time when patients can no longer express their wishes, "by default we end up using very aggressive curative therapy which in most cases is not only inappropriate, but would not be the patient's choice."
Regardless of whether people fill out Polst forms or advance directives, or both, a coalition of health-care groups says it is important for people to make some decisions about end of life wishes and to choose a surrogate who understands their wishes to step in if necessary. The group is promoting April 16 as National HealthCare Decisions Day via its website, NHDD.org. "There is so much fear about having these discussions, when for most people the problems are going to happen when they haven't had these discussions," says Amy Berman, a senior program officer for the John A. Hartford Foundation, which focuses on improving health care for older Americans.
By Laura Landro : WSJ : March 14, 2011
Advance directives, which allow people to plan ahead for end-of-life care, can be too vague to cover many medical situations. Now, a growing number of states are promoting another program to help guide physicians with a patient's specific instructions.
The programs are known as Physician Orders for Life-Sustaining Treatment, or Polst. They are meant to complement advance directives, sometimes known as living wills, in which people state in broad terms how much medical intervention they will want when their condition no longer allows them to communicate. A Polst, which is signed by both the patient and the doctor, spells out such choices as whether a patient wants to be on a mechanical breathing machine or feeding tube and receive antibiotics.
Polst programs are currently in use in 14 states and regions, including California, Oregon and New York. Three states, Colorado, Idaho and Pennsylvania, adopted Polst programs recently, and another 16 states and six regions are developing programs. Besides providing documents that meet local regulations, the programs train health-care providers to discuss end-of-life treatment choices with patients with terminal illness or anyone wishing to define their care preferences.
"More than 75% of people will be unable to make some or all of their own medical decisions at the end of life, but we don't prepare patients and their families to deal with this situation, and it's frightening and difficult for them to know what to do," says Rebecca Sudore, a physician at the University of California, San Francisco and the city's VA Medical Center.
Planning ahead for end-of-life care is meant to allow patients to reduce the amount of medical intervention, if that's what they prefer. But patients also can make clear their wishes if they prefer maximum intervention.
Planning Ahead
Advance directives allow patients to make their end-of-life wishes known in the event they are unable to communicate.
Here are some typical advance directives:
A living will: This instructs family and medical providers on the treatments that a patient wants to receive. The most common decisions involve these life-sustaining treatments:
a) Cardiopulmonary resuscitation (CPR): Used when a patient's heart or breathing stops.
b) A Do Not Resuscitate (DNR) order: A written physician's order that prevents the health-care team from initiating CPR.
c) A Do Not Intubate (DNI) order: Intubation is the placement of a tube into the nose or mouth in order to have it enter the windpipe (trachea) to help the patient breathe.
d) Artificial nutrition and hydration: Used when patients are no longer able to take food and fluid by mouth.
Medical power of attorney lets patients select someone else, usually a family member or close friend, to make care decisions when patients are temporarily or permanently unable to communicate or make decisions on their own.
Physician Orders for Life-Sustaining Treatment, or Polst, is a medical order form signed by the patient and the doctor. It becomes part of the patient's medical record and provides specific instructions to the medical team on such issues as the use of mechanical breathing machines and feeding tubes.
A Polst form is an official medical order, says Susan Tolle, director of the Center for Ethics in Health Care at Oregon Health & Science University, a developer of the Polst program. Unlike an advance directive, which can be misplaced or vaguely worded, a Polst spells out specific treatment instructions and remains part of a patient's medical record. In Oregon, for example, the documents also are stored in a state registry so emergency medical technicians as well as hospitals have access to them. States that have adopted the Polst program also have put in place general protections for medical personnel who follow the directives.
Advance directives, which also allow people to designate a surrogate to make decisions about care, vary state by state. While some states' forms may be highly specific, they may be printed out and stored somewhere where they can't be found when needed. Many states also accept other documents such as a form called Five Wishes that allows people to spell out what kind of quality of life they want, and make requests such as having their bodies massaged with oils for comfort.
A study supported by the National Institutes of Health last year found that patients with Polst forms were more likely to have treatment preferences documented than patients who used traditional documents such as living wills and do-not-resuscitate orders.
Making end-of-life decisions when a loved one's wishes are not known can be difficult for families. After years of struggling with Parkinson's disease and congestive heart failure, Nancy Williamson's mother became seriously ill last August and slipped into a coma from which doctors said she would never recover. Although Ms. Williamson and her sisters wanted doctors to do more, they learned that their mother had signed a Polst form asking for only limited medical treatment.
Ms. Williamson, a California lawyer, says that after arguing with doctors because she wanted to hold on to her mother, "I realized having the Polst made it easier for us because my mom had made her own health-care decisions." The experience led her to help clients prepare end-of-life documents, Ms. Williamson says.
End-of-life directives are controversial. Anti-abortion group LifeTree Inc., for example, opposes the signing of living wills and says life sustaining treatment should always be administered. Elizabeth D. Wickham, the group's executive director, says Polst programs provide legal protection to medical personnel for hastening death, thus encouraging imposed death on patients.
Studies show that many elderly patients prefer to limit medical interventions. In one study of hospice patients, 79% wanted comfort measures only, and 20% wanted only limited additional interventions such as intravenous fluids and antibiotics. In another study only 12% of residents of a long-term skilled nursing facility wanted intensive-care unit treatment that would put them on a breathing machine.
Physicians often don't have the time or training to coach patients through end-of-life-care conversations, says Bernard Hammes, chairman of a national task force that helps develop Polst programs. In a program he designed at the Gunderson Lutheran Health System in LaCrosse, Wis., nurses, social workers, chaplains and others are trained as advance care planning facilitators to help patients and families discuss and document end of life wishes.
The program, Respecting Choices, has been used as a model by dozens of health systems in the U.S. and overseas. Dr. Hammes says studies at Gunderson Lutheran have shown patients with advanced illness who have documented their wishes are more likely to prefer that their care be focused on comfort and function. They are also less likely to want to have their final medical care in a hospital, or to have interventions like CPR attempted. Those patients also use about $2,000 less in physician and hospital services in the last six months of life, a time when the highest medical expenses often occur, he says.
Insurer Aetna began using nurse-care managers to help manage both Medicare and commercially insured patients with terminal illness in 2004, using telephone consultations with patients, doctors and families to, among other things, ensure advance directives are in place and complied with. As a result of the program, a higher proportion of members elected hospice care compared to prior years, which was associated with a decrease in the use of acute care, intensive care and emergency services, particularly for Medicare Advantage beneficiaries. Precise cost reductions couldn't be determined for patients in Medicare because it paid the costs directly, Aetna said. But in the commercially insured population, the program led to a net medical cost decrease of 22% compared to a control group not using the care-management services.
Aetna has extended its terminal-illness-care management to all eligible members. "No one is suggesting that anyone be pushed in any specific direction about the choices they make for end-of-life care," says Randall Krakauer, Aetna's head of Medicare medical management. But because such choices often aren't known at a time when patients can no longer express their wishes, "by default we end up using very aggressive curative therapy which in most cases is not only inappropriate, but would not be the patient's choice."
Regardless of whether people fill out Polst forms or advance directives, or both, a coalition of health-care groups says it is important for people to make some decisions about end of life wishes and to choose a surrogate who understands their wishes to step in if necessary. The group is promoting April 16 as National HealthCare Decisions Day via its website, NHDD.org. "There is so much fear about having these discussions, when for most people the problems are going to happen when they haven't had these discussions," says Amy Berman, a senior program officer for the John A. Hartford Foundation, which focuses on improving health care for older Americans.
Making our Wishes Known at the End of Life
By Pauline W. Chen, MD : NY Times Article : April 15, 2010
Tomorrow is Health Care Decisions Day, part of a national campaign to encourage Americans to complete their advance directives or living wills and document their desires regarding medical treatment at the end of life.
I will spend the day thinking about my father-in-law and how the wishes outlined in his advance directives continue to affect our family a month after his death.
My father-in-law was a lifelong educator, a gentle Latin scholar and former school head. That he also possessed cinematic-grade good looks seemed irrelevant to him. Instead, his greatest delights were, in descending order, his family and friends, word games and reeling off a good story, the quality of which could be judged by the wryness of the final one-liner. Even as he suffered from dementia, my father-in-law retained his ability to deliver the unexpected zinger.
Earlier this year at his skilled nursing facility, after joining one of two teams involved in a spelling bee, a staff member asked him what he wanted to name his team. He looked up at his elderly, slightly glassy-eyed comrades, then surveyed his opponents.
“The Winners,” he answered, with a slight smile. “Our name is ‘The Winners.’ ”
But there were no witty quips that morning four weeks ago when he woke up with a cold left arm. Later, in the hospital, surgeons would tell us that he had a clot in the arm’s main artery, as well as multiple clots in other arteries. With these pathways for oxygenated blood obstructed, my father-in-law’s arm, part of his spleen and a small segment of intestine were dying. Without multiple surgical interventions, the dying organs would soon release a torrent of toxins into his bloodstream. The tingling, numbness and slight discomfort he was complaining about would eventually give way to excruciating pain.
Even with my experience of having cared for patients in similar situations, I wanted at first to believe, against all odds, that my father-in-law’s course might be different. It seemed easier that morning to take the responsibility of deciding to do something, to proceed with an operation, than it was deciding not to intervene.
But was it right to count on the small chance that he might survive such an operation, when in fact it was more likely that our interventions would leave him languishing in an intensive care unit and returning over and over again to the operating room?
As it turned out, none of his family had to brood over the decision for long. In his gentle, understated way, my father-in-law had lifted the burden of that choice from his family’s shoulders years earlier. In the folder of papers that he carried with him to the hospital were the advance directives that spelled out how he wanted to live and that recapitulated conversations he had had with his children years ago about the inevitable end of his life.
My father-in-law completed those documents with the hope but not the assurance that they would actually influence the end of his life. In fact, not even experts in end-of-life care could have assured him or predicted whether his living will would have made any difference. While advance directives have been around for almost 40 years and have been federally mandated in all Medicare-certified institutions for two decades, there has been no research to show that patients with living wills actually end up dying in a way that is consistent with their wishes.
Now we have the evidence that advance directives do make a difference.
Researchers at the University of Michigan in Ann Arbor combed through the records of over 4,000 individuals over age 60 and found that almost a third of these patients would eventually become too incapacitated to make the necessary decisions regarding medical treatment at the end of life. But among them, nearly all of those with a living will requesting limited or comfort care only ultimately did receive such care at the end of their lives. And those patients who specified all care possible were far more likely to receive aggressive care than those who did not request it.
“We need to take the initiative to document decisions seriously,” said Dr. Maria J. Silveira, lead author of the study and an assistant professor of internal medicine at the University of Michigan. “Every person who comes through the door at age 60 or above has a significant chance of losing decisional capacity.”
The number of individuals with living wills has increased steadily over the years; still, fewer than half of the patients in the study had one. Without such documents, patients remain vulnerable even if they have already had end-of-life care conversations with a physician. “We live in a time where care is very fragmented,” Dr. Silveira said. “You can’t be sure that the doctor who has the conversation with the patient is the same doctor who will care for the patient in the hospital or in the nursing home.”
These conversations will likely become less frequent as time pressures mount for physicians. “The most important thing when you are discussing these preferences is a relationship of trust,” Dr. Silveira noted. “You cannot develop that in five minutes or in one visit.” While reimbursing physicians would help encourage such end-of-life care discussions, efforts last fall to legislate such reimbursements failed. Now, with 40 million new patients in the health care system and shrinking numbers of primary care physicians, such patient-doctor conversations may become nearly impossible.
One solution, suggests Dr. Silveira, is to use Web sites that help patients create living wills. Two she recommends are Caring Connections and Aging With Dignity, for patients; and for doctors, Endlink, from Northwestern University, and EPERC, from the Medical College of Wisconsin.
“You don’t need an attorney to get these documents done,” Dr. Silveira said. Physicians themselves can also work around the time issue by asking their patients to designate a health care proxy, a trusted friend or relative who can make decisions when that patient can’t. “Proxies can have as much of an effect on hospitalization and care as living wills, and naming one takes less than two minutes,” Dr. Silveira observed. “It is a far less difficult and emotional discussion to ask for a name than it is to talk about advanced directives.”
Added Dr. Silveira: “The goal is to assure patients that their autonomy is respected, as much as it is to alleviate family and loved ones of the burden of making a decision they’ll regret or wonder about forever.”
I was with my father-in-law on the last day of his life. He sat in bed, face so luminous that the sunlight seemed to reflect off of his cheeks. It was hard for me to take my eyes off of him that morning because he looked not like the man I had always known but the man I had only seen in pictures. He looked as he had in the full bloom of his youth — gentle, beautiful and eyes shining with hope.
Later that day I understood why. My father-in-law was at home, he was surrounded by family and he was dying as he had wished.
He, one of “The Winners,” had won.
By Pauline W. Chen, MD : NY Times Article : April 15, 2010
Tomorrow is Health Care Decisions Day, part of a national campaign to encourage Americans to complete their advance directives or living wills and document their desires regarding medical treatment at the end of life.
I will spend the day thinking about my father-in-law and how the wishes outlined in his advance directives continue to affect our family a month after his death.
My father-in-law was a lifelong educator, a gentle Latin scholar and former school head. That he also possessed cinematic-grade good looks seemed irrelevant to him. Instead, his greatest delights were, in descending order, his family and friends, word games and reeling off a good story, the quality of which could be judged by the wryness of the final one-liner. Even as he suffered from dementia, my father-in-law retained his ability to deliver the unexpected zinger.
Earlier this year at his skilled nursing facility, after joining one of two teams involved in a spelling bee, a staff member asked him what he wanted to name his team. He looked up at his elderly, slightly glassy-eyed comrades, then surveyed his opponents.
“The Winners,” he answered, with a slight smile. “Our name is ‘The Winners.’ ”
But there were no witty quips that morning four weeks ago when he woke up with a cold left arm. Later, in the hospital, surgeons would tell us that he had a clot in the arm’s main artery, as well as multiple clots in other arteries. With these pathways for oxygenated blood obstructed, my father-in-law’s arm, part of his spleen and a small segment of intestine were dying. Without multiple surgical interventions, the dying organs would soon release a torrent of toxins into his bloodstream. The tingling, numbness and slight discomfort he was complaining about would eventually give way to excruciating pain.
Even with my experience of having cared for patients in similar situations, I wanted at first to believe, against all odds, that my father-in-law’s course might be different. It seemed easier that morning to take the responsibility of deciding to do something, to proceed with an operation, than it was deciding not to intervene.
But was it right to count on the small chance that he might survive such an operation, when in fact it was more likely that our interventions would leave him languishing in an intensive care unit and returning over and over again to the operating room?
As it turned out, none of his family had to brood over the decision for long. In his gentle, understated way, my father-in-law had lifted the burden of that choice from his family’s shoulders years earlier. In the folder of papers that he carried with him to the hospital were the advance directives that spelled out how he wanted to live and that recapitulated conversations he had had with his children years ago about the inevitable end of his life.
My father-in-law completed those documents with the hope but not the assurance that they would actually influence the end of his life. In fact, not even experts in end-of-life care could have assured him or predicted whether his living will would have made any difference. While advance directives have been around for almost 40 years and have been federally mandated in all Medicare-certified institutions for two decades, there has been no research to show that patients with living wills actually end up dying in a way that is consistent with their wishes.
Now we have the evidence that advance directives do make a difference.
Researchers at the University of Michigan in Ann Arbor combed through the records of over 4,000 individuals over age 60 and found that almost a third of these patients would eventually become too incapacitated to make the necessary decisions regarding medical treatment at the end of life. But among them, nearly all of those with a living will requesting limited or comfort care only ultimately did receive such care at the end of their lives. And those patients who specified all care possible were far more likely to receive aggressive care than those who did not request it.
“We need to take the initiative to document decisions seriously,” said Dr. Maria J. Silveira, lead author of the study and an assistant professor of internal medicine at the University of Michigan. “Every person who comes through the door at age 60 or above has a significant chance of losing decisional capacity.”
The number of individuals with living wills has increased steadily over the years; still, fewer than half of the patients in the study had one. Without such documents, patients remain vulnerable even if they have already had end-of-life care conversations with a physician. “We live in a time where care is very fragmented,” Dr. Silveira said. “You can’t be sure that the doctor who has the conversation with the patient is the same doctor who will care for the patient in the hospital or in the nursing home.”
These conversations will likely become less frequent as time pressures mount for physicians. “The most important thing when you are discussing these preferences is a relationship of trust,” Dr. Silveira noted. “You cannot develop that in five minutes or in one visit.” While reimbursing physicians would help encourage such end-of-life care discussions, efforts last fall to legislate such reimbursements failed. Now, with 40 million new patients in the health care system and shrinking numbers of primary care physicians, such patient-doctor conversations may become nearly impossible.
One solution, suggests Dr. Silveira, is to use Web sites that help patients create living wills. Two she recommends are Caring Connections and Aging With Dignity, for patients; and for doctors, Endlink, from Northwestern University, and EPERC, from the Medical College of Wisconsin.
“You don’t need an attorney to get these documents done,” Dr. Silveira said. Physicians themselves can also work around the time issue by asking their patients to designate a health care proxy, a trusted friend or relative who can make decisions when that patient can’t. “Proxies can have as much of an effect on hospitalization and care as living wills, and naming one takes less than two minutes,” Dr. Silveira observed. “It is a far less difficult and emotional discussion to ask for a name than it is to talk about advanced directives.”
Added Dr. Silveira: “The goal is to assure patients that their autonomy is respected, as much as it is to alleviate family and loved ones of the burden of making a decision they’ll regret or wonder about forever.”
I was with my father-in-law on the last day of his life. He sat in bed, face so luminous that the sunlight seemed to reflect off of his cheeks. It was hard for me to take my eyes off of him that morning because he looked not like the man I had always known but the man I had only seen in pictures. He looked as he had in the full bloom of his youth — gentle, beautiful and eyes shining with hope.
Later that day I understood why. My father-in-law was at home, he was surrounded by family and he was dying as he had wished.
He, one of “The Winners,” had won.
MASSACHUSETTS HEALTH CARE PROXY
Information, Instructions, and Form
What does the Health Care Proxy Law allow?
The Health Care Proxy is a simple legal document that allows you to name someone you know and trust to
make health care decisions for you if, for any reason and at any time, you become unable to make or communicate
those decisions. It is an important document, however, because it concerns not only the choices you
make about your health care, but also the relationships you have with your physician, family, and others who
may be involved with your care. Read this and follow the instructions to ensure that your wishes are honored.
Under the Health Care Proxy Law (Massachusetts General Laws, Chapter 201D), any competent adult 18
years of age or over may use this form to appoint a Health Care Agent. You (known as the "Principal") can
appoint any adult EXCEPT the administrator, operator, or employee of a health care facility such as a hospital
or nursing home where you are a patient or resident UNLESS that person is also related to you by blood, marriage,
or adoption.
What can my Agent do?
Your Agent will make decisions about your health care only when you are, for some reason, unable to do that
yourself. This means that your Agent can act for you if you are temporarily unconscious, in a coma, or have
some other condition in which you cannot make or communicate health care decisions. Your Agent cannot act
for you until your doctor determines, in writing, that you lack the ability to make health care decisions. Your
doctor will tell you of this if there is any sign that you would understand it.
Acting with your authority, your Agent can make any health care decision that you could, if you were able. If
you give your Agent full authority to act for you, he or she can consent to or refuse any medical treatment,
including treatment that could keep you alive.
Your Agent will make decisions for you only after talking with your doctor or health care provider, and after
fully considering all the options regarding diagnosis, prognosis, and treatment of your illness or condition.
Your Agent has the legal right to get any information, including confidential medical information, necessary to
make informed decisions for you.
Your Agent will make health care decisions for you according to your wishes or according to his/her assessment
of your wishes, including your religious or moral beliefs. You may wish to talk first with your doctor,
religious advisor, or other people before giving instructions to your Agent. It is very important that you talk
with your Agent so that he or she knows what is important to you. If your Agent does not know what your
wishes would be in a particular situation, your Agent will decide based on what he or she thinks would be in
your best interests. After your doctor has determined that you lack the ability to make health care decisions, if
you still object to any decision made by your Agent, your own decisions will be honored unless a Court determines
that you lack capacity to make health care decisions.
Your Agent's decisions will have the same authority as yours would, if you were able, and will be honored
over those of any other person, except for any limitation you yourself made, or except for a Court Order
specifically overriding the Proxy.
How do I fill out the form?
At the top of the form, print your full name and address. Print the name, address, and phone number of the person you choose as your Health Care Agent. (Optional: If you think your Agent might not be available at any future time, you may name a second person as an Alternate Agent. Your Alternate Agent will be called if your Agent is unwilling or unable to serve.)
Setting limits on your Agent's authority might make it difficult for your Agent to act for you in an unexpectedsituation. If you want your Agent to have full authority to act for you, leave the limitations space blank. However, if you want to limit the kinds of decisions you would want your Agent or Alternate Agent to make for you, include them in the blank.
BEFORE you sign, be sure you have two adults present who can witness you signing the document.
The only people who cannot serve as witnesses are your Agent and Alternate Agent. Then sign the document
yourself. (Or, if you are physically unable, have someone other than either witness sign your name at your
direction. The person who signs your name for you should put his/her own name and address in the spaces
provided.)
Have your witnesses fill in the date, sign their names and print their names and addresses.
OPTIONAL: On the back of the form are statements to be signed by your Agent and any Alternate
Agent. This is not required by law, but is recommended to ensure that you have talked with the person or persons
who may have to make important decisions about your care and that each of them realizes the importance
of the task they may have to do.
Who should have the original and copies?
After you have filled in the form, remove this information page and make at least four photocopies of the
form. Keep the original yourself where it can be found easily (not in your safe deposit box). Give copies to
your doctor and/or health plan to put into your medical record. Give copies to your Agent and any Alternate
Agent. You can give additional copies to family members, your clergy and/or lawyer, and other people who
may be involved in your health care decisionmaking.
How can I revoke or cancel the document?
Your Health Care Proxy is revoked when any of the following four things happens:
1. You sign another Health Care Proxy later on.
2. You legally separate from or divorce your spouse who is named in the Proxy as your Agent.
3. You notify your Agent, your doctor, or other health care provider, orally or in writing, that you
want to revoke your Health Care Proxy.
4. You do anything else that clearly shows you want to revoke the Proxy, for example, tearing
up or destroying the Proxy, crossing it out, telling other people, etc.
MASSACHUSETTS HEALTH CARE PROXY
1. I, , residing at
(Principal -- PRINT your name)
(Street) (City or Town) (State)
appoint as my Health Care Agent:
(Name of person you choose as Agent)
of
(Street) (City/town) (State) (Phone)
( OPTIONAL: If my Agent is unwilling or unable to serve, then I appoint as my Alternate Agent:
, of
(Name of person you choose as Alternate Agent)
.)
(Street) (City/town) (State) (Phone)
2. My Agent shall have the authority to make all health care decisions for me, including decisions about lifesustaining
treatment, subject to any limitations I state below, if I am unable to make health care decisions
myself. My Agent's authority becomes effective if my attending physician determines in writing that I lack the
capacity to make or to communicate health care decisions. My Agent is then to have the same authority to
make health care decisions as I would if I had the capacity to make them EXCEPT (here list the limitations, if
any, you wish to place on your Agent's authority):
I direct my Agent to make health care decisions based on my Agent's assessment of my personal wishes. If
my personal wishes are unknown, my Agent is to make health care decisions based on my Agent's assessment
of my best interests. Photocopies of this Health Care Proxy shall have the same force and effect as the original
and may be given to other health care providers.
3. Signed:
Complete only if Principal is physically unable to sign: I have signed the Principal's name above at his/her
direction in the presence of the Principal and two witnesses.
(Name) (Street)
(City/town) (State)
4. WITNESS STATEMENT: We, the undersigned, each witnessed the signing of this Health Care Proxy by
the Principal or at the direction of the Principal and state that the Principal appears to be at least 18 years of
age, of sound mind and under no constraint or undue influence. Neither of us is named as the Health Care
Agent or Alternate Agent in this document.
In our presence, on this day of .. FILL IN DATE
Witness #1
(Signature)
Name (print)
Address:
Witness #1
(Signature)
Name (print)
Address:
YOUR B IRTH DAT E
____/____/____
5. Statements of Health Care Agent and Alternate Agent (OPTIONAL)
Health Care Agent: I have been named by the Principal as the Principal's Health Care Agent by this Health
Care Proxy. I have read this document carefully, and have personally discussed with the Principal his/her
health care wishes at a time of possible incapacity. I know the Principal and accept this appointment freely. I
am not an operator, administrator or employee of a hospital, clinic, nursing home, rest home, Soldiers Home or
other health facility where the Principal is presently a patient or resident or has applied for admission. Or if I
am a person so described, I am also related to the Principal by blood, marriage, or adoption. If called upon
and to the best of my ability, I will try to carry out the Principal's wishes.
(Signature of Health Care Agent)
Alternate Agent: I have been named by the Principal as the Principal's Alternate Agent by this Health Care
Proxy. I have read this document carefully, and have personally discussed with the Principal his/her health
care wishes at a time of possible incapacity. I know the Principal and accept this appointment freely. I am not
an operator, administrator or employee of a hospital, clinic, nursing home, rest home, Soldiers Home or other
health facility where the Principal is presently a patient or resident or has applied for admission. Or if I am a
person so described, I am also related to the Principal by blood, marriage, or adoption. If called upon and to
the best of my ability, I will try to carry out the Principal's wishes.
(Signature of Alternate Agent)
* * * * *
Model Health Care Proxy form developed by a Task Force of the following organizations:
Boston University Schools of Medicine and Public
Health:
Law, Medicine, and Ethics Program
Deaconess ElderCare Program
Hospice Federation of Massachusetts
Massachusetts Bar Association
Massachusetts Department of Public Health
Massachusetts Executive Office of Elder Affairs
Massachusetts Federation of Nursing Homes
Massachusetts Health Decisions
Massachusetts Hospital Association
Massachusetts Medical Society
Massachusetts Nurses Association
Medical Center of Central Massachusetts
Suffolk University Law School:
Elder Law Clinic
University of Massachusetts at Boston:
The Gerontology Institute
Visiting Nurse Associations of Massachusetts
End of life care
In practice A (good) death panel
By Suzanne Koven, M.D. : Boston Globe : May 23, 2011
When Ivan, a successful 45-year-old attorney, realized he would never recover from his illness, he thought things couldn’t get any worse. Things got worse. His pain became uncontrollable. His wife and children, frightened by Ivan’s groans and gaunt appearance, withdrew from him. Friends and colleagues stopped visiting. His doctors gave up hope. Finally, feeling entirely alone, Ivan died.
Ivan was not a patient of mine — or anyone else’s. He’s the title character of Leo Tolstoy’s novella “The Death of Ivan Ilyich.’’ Though it first appeared in 1886, “Ivan Ilyich’’ couldn’t be more relevant to our current national conversation about dying. Everyone would agree that Ilyich, isolated and suffering, died a bad death. What’s become more controversial is the role medical professionals and the government should play in helping people avoid Ivan’s fate.
This controversy took a heated turn last year when Congress debated health care reform. One provision, scrapped from the new law but later proposed as a Medicare regulation, was payment for what’s called “advanced care planning.’’ Clinicians would be reimbursed for advising patients older than 65 of their potential treatment options in the event of a life-threatening illness.
Opponents of this provision felt it represented too much intrusion by the government into personal decisions about health care. Talk of “death panels,’’ in which bureaucrats could “pull the plug on Grandma,’’ inflamed the debate.
The truth is, though, that opponents of this aspect of health care reform are not the only challenge doctors face in improving how we take care of people at the end of their lives. Our greatest obstacle may be ourselves. As surgeon and author of the book “Final Exam,’’ Pauline Chen has noted, doctors simply are not taught how to counsel and treat the dying.
I know I wasn’t. In medical school I learned more about malaria and bubonic plague — two diseases I’ve yet to encounter in 20 years of practice in downtown Boston — than about advising patients as they approach death. Though some medical schools now do offer training in end-of-life care, and consultants specializing in palliative and hospice care have become more widely available, many physicians remain uncomfortable even discussing death with their patients.
I asked Dr. Vicki Jackson, director of the Palliative Care Service at Massachusetts General Hospital, why she thinks this is so. “We’re swimming in a culture of death denial,’’ Jackson told me. Expectations of medical science have become so inflated, she explained, that many patients and even doctors have trouble accepting the fact that people actually die.
A doctor is likely to see a patient’s death as a failure — a failure that he or she may not wish to contemplate. Yet a comfortable and dignified death can be, as Jackson puts it, “a beautiful thing,’’ and doctors should embrace more readily the part they might play in it.
I witnessed such a death not long ago. A patient of mine, a vibrant woman in her 70s, developed pancreatic cancer. She underwent exploratory surgery but the tumor proved too far advanced to be removed.
In the hospital, as she recuperated from her operation, the woman and her husband had several visitors. An oncologist helped them weigh the pros and cons of chemotherapy, which the patient, with her husband’s support, elected not to pursue. Palliative care consultants helped them understand their options regarding life support and made recommendations about pain control.
They also arranged for a psychologist to advise them about how best to share the news of her condition with their young grandchildren. A priest from the hospital’s chaplaincy prayed with them, and a case manager organized the woman’s transfer to a hospice in the town where the couple had once lived for several years and in which they still had many friends.
After my patient died, I asked her husband if all this activity was helpful, and he agreed readily that it had been. His wife’s illness, he told me, was “such a painful moment but also such an intense experience.’’ The palliative care team, the priest, and others, he felt, allowed them “the possibility of fully recognizing what was happening.’’
His statement was both moving and fascinating, and when I shared it with Dr. Jackson she knew exactly what the woman’s husband had meant. One of the most important things professionals who focus on end-of-life care offer, she said, is a “safe space’’ in which the many emotions patients and their families feel in the face of death — anger, sadness, confusion, regret, and yes, even joy — are validated.
But counseling patients for whom death is imminent may be easier for many clinicians than the no-less important task of reviewing end-of-life options for patients whose prognosis is more uncertain. Studies have shown that physicians are especially reluctant to initiate such discussions with patients they’ve known for a long time. We are particularly attached to these people and may find it hard to acknowledge that they will die, or we may fear that such discussions will signal to patients that we’re giving up on them.
Dr. Atul Gawande of the Harvard Medical School and Harvard School of Public Health, as well as a staff writer for The New Yorker, has recently received a grant to study how end-of-life counseling can become an automatic part of a patient’s care; part of a checklist, like screening colonoscopies and mammograms.
At the hospice, my patient with pancreatic cancer was surrounded by family and old friends and died peacefully. Afterward, her husband told me that he felt angry when he heard talk of “death panels.’’ Like many family members of patients who’ve received end-of-life care, he’d seen its benefits firsthand.
Perhaps he would agree that his wife had, in fact, had a “death panel,’’ of sorts — a team of nurses, doctors, clergy, neighbors, friends, and family who all supported her in the last days of her life. “I’m comforted,’’ he said, “happy, even, that she died the way she wanted to, that so many people were there for her. If there’s such a thing as a ‘good death,’ it was hers.’’
Three weeks after my patient’s death, the White House withdrew the proposal that advanced care planning be covered under Medicare.
In practice A (good) death panel
By Suzanne Koven, M.D. : Boston Globe : May 23, 2011
When Ivan, a successful 45-year-old attorney, realized he would never recover from his illness, he thought things couldn’t get any worse. Things got worse. His pain became uncontrollable. His wife and children, frightened by Ivan’s groans and gaunt appearance, withdrew from him. Friends and colleagues stopped visiting. His doctors gave up hope. Finally, feeling entirely alone, Ivan died.
Ivan was not a patient of mine — or anyone else’s. He’s the title character of Leo Tolstoy’s novella “The Death of Ivan Ilyich.’’ Though it first appeared in 1886, “Ivan Ilyich’’ couldn’t be more relevant to our current national conversation about dying. Everyone would agree that Ilyich, isolated and suffering, died a bad death. What’s become more controversial is the role medical professionals and the government should play in helping people avoid Ivan’s fate.
This controversy took a heated turn last year when Congress debated health care reform. One provision, scrapped from the new law but later proposed as a Medicare regulation, was payment for what’s called “advanced care planning.’’ Clinicians would be reimbursed for advising patients older than 65 of their potential treatment options in the event of a life-threatening illness.
Opponents of this provision felt it represented too much intrusion by the government into personal decisions about health care. Talk of “death panels,’’ in which bureaucrats could “pull the plug on Grandma,’’ inflamed the debate.
The truth is, though, that opponents of this aspect of health care reform are not the only challenge doctors face in improving how we take care of people at the end of their lives. Our greatest obstacle may be ourselves. As surgeon and author of the book “Final Exam,’’ Pauline Chen has noted, doctors simply are not taught how to counsel and treat the dying.
I know I wasn’t. In medical school I learned more about malaria and bubonic plague — two diseases I’ve yet to encounter in 20 years of practice in downtown Boston — than about advising patients as they approach death. Though some medical schools now do offer training in end-of-life care, and consultants specializing in palliative and hospice care have become more widely available, many physicians remain uncomfortable even discussing death with their patients.
I asked Dr. Vicki Jackson, director of the Palliative Care Service at Massachusetts General Hospital, why she thinks this is so. “We’re swimming in a culture of death denial,’’ Jackson told me. Expectations of medical science have become so inflated, she explained, that many patients and even doctors have trouble accepting the fact that people actually die.
A doctor is likely to see a patient’s death as a failure — a failure that he or she may not wish to contemplate. Yet a comfortable and dignified death can be, as Jackson puts it, “a beautiful thing,’’ and doctors should embrace more readily the part they might play in it.
I witnessed such a death not long ago. A patient of mine, a vibrant woman in her 70s, developed pancreatic cancer. She underwent exploratory surgery but the tumor proved too far advanced to be removed.
In the hospital, as she recuperated from her operation, the woman and her husband had several visitors. An oncologist helped them weigh the pros and cons of chemotherapy, which the patient, with her husband’s support, elected not to pursue. Palliative care consultants helped them understand their options regarding life support and made recommendations about pain control.
They also arranged for a psychologist to advise them about how best to share the news of her condition with their young grandchildren. A priest from the hospital’s chaplaincy prayed with them, and a case manager organized the woman’s transfer to a hospice in the town where the couple had once lived for several years and in which they still had many friends.
After my patient died, I asked her husband if all this activity was helpful, and he agreed readily that it had been. His wife’s illness, he told me, was “such a painful moment but also such an intense experience.’’ The palliative care team, the priest, and others, he felt, allowed them “the possibility of fully recognizing what was happening.’’
His statement was both moving and fascinating, and when I shared it with Dr. Jackson she knew exactly what the woman’s husband had meant. One of the most important things professionals who focus on end-of-life care offer, she said, is a “safe space’’ in which the many emotions patients and their families feel in the face of death — anger, sadness, confusion, regret, and yes, even joy — are validated.
But counseling patients for whom death is imminent may be easier for many clinicians than the no-less important task of reviewing end-of-life options for patients whose prognosis is more uncertain. Studies have shown that physicians are especially reluctant to initiate such discussions with patients they’ve known for a long time. We are particularly attached to these people and may find it hard to acknowledge that they will die, or we may fear that such discussions will signal to patients that we’re giving up on them.
Dr. Atul Gawande of the Harvard Medical School and Harvard School of Public Health, as well as a staff writer for The New Yorker, has recently received a grant to study how end-of-life counseling can become an automatic part of a patient’s care; part of a checklist, like screening colonoscopies and mammograms.
At the hospice, my patient with pancreatic cancer was surrounded by family and old friends and died peacefully. Afterward, her husband told me that he felt angry when he heard talk of “death panels.’’ Like many family members of patients who’ve received end-of-life care, he’d seen its benefits firsthand.
Perhaps he would agree that his wife had, in fact, had a “death panel,’’ of sorts — a team of nurses, doctors, clergy, neighbors, friends, and family who all supported her in the last days of her life. “I’m comforted,’’ he said, “happy, even, that she died the way she wanted to, that so many people were there for her. If there’s such a thing as a ‘good death,’ it was hers.’’
Three weeks after my patient’s death, the White House withdrew the proposal that advanced care planning be covered under Medicare.
Letting Doctors Make the Tough Decisions
By Pauline Chen MD : NY Times : August 11, 2011
Soon after I finished my surgical training, I worked with a young doctor who was impressive not only for his clinical skills but also for his devotion to patients. He was large and powerfully built but never seemed to loom over his patients, miraculously shrinking down to their eye level whenever he spoke with them. He listened intently to every detail of their travails and always ended the visits by asking if they still had any unanswered questions.
One afternoon I was surprised to see him at a nursing station, his massive arms gesticulating as he complained to a nurse about one patient’s family. The patient was dying, and the young doctor had organized a meeting with the family to talk about withdrawing life-support machines and medications and starting comfort measures. The family had spent the entire meeting asking questions but then refused to make any decisions or withdraw any treatments.
“I spent all this time telling them we could continue to inflict pain on their loved one or we could make him comfortable,” he said, his hands still moving. “I told them suffering or comfort — it was their decision. But in the end, they made no decision and just walked right out of the room.”
The way doctors and patients approach medical decisions has changed sharply over the last 50 years. For generations, these decisions were the exclusive purview of doctors; and patients, if they participated, often had little say in the final choice. But that paternalistic decision-making process began to change in the late 1960s and ’70s, as movements calling for patient empowerment grew and medical ethicists began articulating principles regarding the ethical care of patients.
One tenet that gained particular traction among clinicians was respect for the person. Applied to the work done in wards, clinics and operating rooms, this ethical principle led to a new clinical ideal: patient-centered care.
But a second ethical principle, one closely linked to the first, also played an increasingly important role in the patient-doctor relationship: the notion of respect for a person’s autonomy. With time, autonomy would mean letting patients make their own decisions; and that interpretation would work its way into the teaching programs of medical schools and into state laws that mandated discussion of treatment options with patients.
For the next 40 years, young doctors, myself included, would be trained to restrain ourselves from making anything but emergency or mundane decisions for patients.
But a new study reveals that too much physician restraint may not be all that good for the patient — and perhaps may even be unethical. While doctors might equate letting patients make their own decisions with respect, a large number of patients don’t see it that way. In fact, it appears that a majority of patients are being left to make decisions that they never wanted to in the first place.
Researchers interviewed more than 8,000 hospitalized patients at the University of Chicago. When it came to medical decisions, almost all the respondents wanted their doctors to offer choices and consider their opinions. But a majority of patients — two out of three — also preferred that their doctors make the final decisions regarding their medical care.
“The data says decisively that most patients don’t want to make these decisions on their own” said Dr. Farr A. Curlin, an associate professor of medicine at the University of Chicago and one of the authors of the study.
The challenges appear to arise not when the medical choices are obvious, but when the best option for a patient is uncertain. In these situations, when doctors pass the burden of decision-making to a patient or family, it can exacerbate an already stressful situation. “If a physician with all of his or her clinical experience is feeling that much uncertainty,” Dr. Curlin said, “imagine what kind of serious anxiety and confusion the patient and family may be feeling.”
Patients and their families also often don’t realize that their doctors may be grappling with their own set of worries. “Doctors may think, ‘Who am I to presume to know what my patients need?’” Dr. Curlin noted, and may be hesitant to assert their own opinions for fear that they might commit some kind of ethical transgression. Some will resort to veiling their own opinions in a halfhearted attempt to direct the decision. While the doctors might be convinced that they are being objective and dispassionate, more often than not they are sending mixed messages.
A doctor may, for example, tell relatives that it is their choice to withdraw life support from a dying patient. But that doctor may also use value-laden language to describe the options. One alternative may be described to the family as “reasonable” or “comforting,” while the other is depicted as “invasive,” “aggressive” or “painful.”
“This creates a kind of bizarre dishonesty in how we communicate,” Dr. Curlin said. “Patients end up feeling manipulated and will resist making any decision at all.”
For doctors, then, the key to preserving patient autonomy — and patient-centered care — lies not in letting patients make the final decisions alone but in respecting their opinions and shouldering the responsibility together. And while patients will need to be more explicit and ask for that help, doctors, like my young colleague and, I admit, myself, will need to be more mindful of whether patients want them to share information, be directive or hand over the responsibility of the decision.
“We have to stop drawing a circle around patients and their families,” Dr. Curlin said. “We have to stop subjecting them to the loneliness and burden of autonomy and instead begin standing in that circle with them.”
How Doctors Die
It’s Not Like the Rest of Us, But It Should Be
by Ken Murray
Years ago, Charlie, a highly respected orthopedist and a mentor of mine, found a lump in his stomach. He had a surgeon explore the area, and the diagnosis was pancreatic cancer. This surgeon was one of the best in the country. He had even invented a new procedure for this exact cancer that could triple a patient’s five-year-survival odds—from 5 percent to 15 percent—albeit with a poor quality of life. Charlie was uninterested. He went home the next day, closed his practice, and never set foot in a hospital again. He focused on spending time with family and feeling as good as possible. Several months later, he died at home. He got no chemotherapy, radiation, or surgical treatment. Medicare didn’t spend much on him.
It’s not a frequent topic of discussion, but doctors die, too. And they don’t die like the rest of us. What’s unusual about them is not how much treatment they get compared to most Americans, but how little. For all the time they spend fending off the deaths of others, they tend to be fairly serene when faced with death themselves. They know exactly what is going to happen, they know the choices, and they generally have access to any sort of medical care they could want. But they go gently.
Of course, doctors don’t want to die; they want to live. But they know enough about modern medicine to know its limits. And they know enough about death to know what all people fear most: dying in pain, and dying alone. They’ve talked about this with their families. They want to be sure, when the time comes, that no heroic measures will happen—that they will never experience, during their last moments on earth, someone breaking their ribs in an attempt to resuscitate them with CPR (that’s what happens if CPR is done right).
Almost all medical professionals have seen what we call “futile care” being performed on people. That’s when doctors bring the cutting edge of technology to bear on a grievously ill person near the end of life. The patient will get cut open, perforated with tubes, hooked up to machines, and assaulted with drugs. All of this occurs in the Intensive Care Unit at a cost of tens of thousands of dollars a day. What it buys is misery we would not inflict on a terrorist. I cannot count the number of times fellow physicians have told me, in words that vary only slightly, “Promise me if you find me like this that you’ll kill me.” They mean it. Some medical personnel wear medallions stamped “NO CODE” to tell physicians not to perform CPR on them. I have even seen it as a tattoo.
To administer medical care that makes people suffer is anguishing. Physicians are trained to gather information without revealing any of their own feelings, but in private, among fellow doctors, they’ll vent. “How can anyone do that to their family members?” they’ll ask. I suspect it’s one reason physicians have higher rates of alcohol abuse and depression than professionals in most other fields. I know it’s one reason I stopped participating in hospital care for the last 10 years of my practice.
How has it come to this—that doctors administer so much care that they wouldn’t want for themselves? The simple, or not-so-simple, answer is this: patients, doctors, and the system.
To see how patients play a role, imagine a scenario in which someone has lost consciousness and been admitted to an emergency room. As is so often the case, no one has made a plan for this situation, and shocked and scared family members find themselves caught up in a maze of choices. They’re overwhelmed. When doctors ask if they want “everything” done, they answer yes. Then the nightmare begins. Sometimes, a family really means “do everything,” but often they just mean “do everything that’s reasonable.” The problem is that they may not know what’s reasonable, nor, in their confusion and sorrow, will they ask about it or hear what a physician may be telling them. For their part, doctors told to do “everything” will do it, whether it is reasonable or not.
The above scenario is a common one. Feeding into the problem are unrealistic expectations of what doctors can accomplish. Many people think of CPR as a reliable lifesaver when, in fact, the results are usually poor. I’ve had hundreds of people brought to me in the emergency room after getting CPR. Exactly one, a healthy man who’d had no heart troubles (for those who want specifics, he had a “tension pneumothorax”), walked out of the hospital. If a patient suffers from severe illness, old age, or a terminal disease, the odds of a good outcome from CPR are infinitesimal, while the odds of suffering are overwhelming. Poor knowledge and misguided expectations lead to a lot of bad decisions.
But of course it’s not just patients making these things happen. Doctors play an enabling role, too. The trouble is that even doctors who hate to administer futile care must find a way to address the wishes of patients and families. Imagine, once again, the emergency room with those grieving, possibly hysterical, family members. They do not know the doctor. Establishing trust and confidence under such circumstances is a very delicate thing. People are prepared to think the doctor is acting out of base motives, trying to save time, or money, or effort, especially if the doctor is advising against further treatment.
Some doctors are stronger communicators than others, and some doctors are more adamant, but the pressures they all face are similar. When I faced circumstances involving end-of-life choices, I adopted the approach of laying out only the options that I thought were reasonable (as I would in any situation) as early in the process as possible. When patients or families brought up unreasonable choices, I would discuss the issue in layman’s terms that portrayed the downsides clearly. If patients or families still insisted on treatments I considered pointless or harmful, I would offer to transfer their care to another doctor or hospital.
Should I have been more forceful at times? I know that some of those transfers still haunt me. One of the patients of whom I was most fond was an attorney from a famous political family. She had severe diabetes and terrible circulation, and, at one point, she developed a painful sore on her foot. Knowing the hazards of hospitals, I did everything I could to keep her from resorting to surgery. Still, she sought out outside experts with whom I had no relationship. Not knowing as much about her as I did, they decided to perform bypass surgery on her chronically clogged blood vessels in both legs. This didn’t restore her circulation, and the surgical wounds wouldn’t heal. Her feet became gangrenous, and she endured bilateral leg amputations. Two weeks later, in the famous medical center in which all this had occurred, she died.
It’s easy to find fault with both doctors and patients in such stories, but in many ways all the parties are simply victims of a larger system that encourages excessive treatment. In some unfortunate cases, doctors use the fee-for-service model to do everything they can, no matter how pointless, to make money. More commonly, though, doctors are fearful of litigation and do whatever they’re asked, with little feedback, to avoid getting in trouble.
Even when the right preparations have been made, the system can still swallow people up. One of my patients was a man named Jack, a 78-year-old who had been ill for years and undergone about 15 major surgical procedures. He explained to me that he never, under any circumstances, wanted to be placed on life support machines again. One Saturday, however, Jack suffered a massive stroke and got admitted to the emergency room unconscious, without his wife. Doctors did everything possible to resuscitate him and put him on life support in the ICU. This was Jack’s worst nightmare. When I arrived at the hospital and took over Jack’s care, I spoke to his wife and to hospital staff, bringing in my office notes with his care preferences. Then I turned off the life support machines and sat with him. He died two hours later.
Even with all his wishes documented, Jack hadn’t died as he’d hoped. The system had intervened. One of the nurses, I later found out, even reported my unplugging of Jack to the authorities as a possible homicide. Nothing came of it, of course; Jack’s wishes had been spelled out explicitly, and he’d left the paperwork to prove it. But the prospect of a police investigation is terrifying for any physician. I could far more easily have left Jack on life support against his stated wishes, prolonging his life, and his suffering, a few more weeks. I would even have made a little more money, and Medicare would have ended up with an additional $500,000 bill. It’s no wonder many doctors err on the side of overtreatment.
But doctors still don’t over-treat themselves. They see the consequences of this constantly. Almost anyone can find a way to die in peace at home, and pain can be managed better than ever. Hospice care, which focuses on providing terminally ill patients with comfort and dignity rather than on futile cures, provides most people with much better final days. Amazingly, studies have found that people placed in hospice care often live longer than people with the same disease who are seeking active cures. I was struck to hear on the radio recently that the famous reporter Tom Wicker had “died peacefully at home, surrounded by his family.” Such stories are, thankfully, increasingly common.
Several years ago, my older cousin Torch (born at home by the light of a flashlight—or torch) had a seizure that turned out to be the result of lung cancer that had gone to his brain. I arranged for him to see various specialists, and we learned that with aggressive treatment of his condition, including three to five hospital visits a week for chemotherapy, he would live perhaps four months. Ultimately, Torch decided against any treatment and simply took pills for brain swelling. He moved in with me.
We spent the next eight months doing a bunch of things that he enjoyed, having fun together like we hadn’t had in decades. We went to Disneyland, his first time. We’d hang out at home. Torch was a sports nut, and he was very happy to watch sports and eat my cooking. He even gained a bit of weight, eating his favorite foods rather than hospital foods. He had no serious pain, and he remained high-spirited. One day, he didn’t wake up. He spent the next three days in a coma-like sleep and then died. The cost of his medical care for those eight months, for the one drug he was taking, was about $20.
Torch was no doctor, but he knew he wanted a life of quality, not just quantity. Don’t most of us? If there is a state of the art of end-of-life care, it is this: death with dignity. As for me, my physician has my choices. They were easy to make, as they are for most physicians. There will be no heroics, and I will go gentle into that good night. Like my mentor Charlie. Like my cousin Torch. Like my fellow doctors.
Ken Murray, MD, is Clinical Assistant Professor of Family Medicine at USC.
It’s Not Like the Rest of Us, But It Should Be
by Ken Murray
Years ago, Charlie, a highly respected orthopedist and a mentor of mine, found a lump in his stomach. He had a surgeon explore the area, and the diagnosis was pancreatic cancer. This surgeon was one of the best in the country. He had even invented a new procedure for this exact cancer that could triple a patient’s five-year-survival odds—from 5 percent to 15 percent—albeit with a poor quality of life. Charlie was uninterested. He went home the next day, closed his practice, and never set foot in a hospital again. He focused on spending time with family and feeling as good as possible. Several months later, he died at home. He got no chemotherapy, radiation, or surgical treatment. Medicare didn’t spend much on him.
It’s not a frequent topic of discussion, but doctors die, too. And they don’t die like the rest of us. What’s unusual about them is not how much treatment they get compared to most Americans, but how little. For all the time they spend fending off the deaths of others, they tend to be fairly serene when faced with death themselves. They know exactly what is going to happen, they know the choices, and they generally have access to any sort of medical care they could want. But they go gently.
Of course, doctors don’t want to die; they want to live. But they know enough about modern medicine to know its limits. And they know enough about death to know what all people fear most: dying in pain, and dying alone. They’ve talked about this with their families. They want to be sure, when the time comes, that no heroic measures will happen—that they will never experience, during their last moments on earth, someone breaking their ribs in an attempt to resuscitate them with CPR (that’s what happens if CPR is done right).
Almost all medical professionals have seen what we call “futile care” being performed on people. That’s when doctors bring the cutting edge of technology to bear on a grievously ill person near the end of life. The patient will get cut open, perforated with tubes, hooked up to machines, and assaulted with drugs. All of this occurs in the Intensive Care Unit at a cost of tens of thousands of dollars a day. What it buys is misery we would not inflict on a terrorist. I cannot count the number of times fellow physicians have told me, in words that vary only slightly, “Promise me if you find me like this that you’ll kill me.” They mean it. Some medical personnel wear medallions stamped “NO CODE” to tell physicians not to perform CPR on them. I have even seen it as a tattoo.
To administer medical care that makes people suffer is anguishing. Physicians are trained to gather information without revealing any of their own feelings, but in private, among fellow doctors, they’ll vent. “How can anyone do that to their family members?” they’ll ask. I suspect it’s one reason physicians have higher rates of alcohol abuse and depression than professionals in most other fields. I know it’s one reason I stopped participating in hospital care for the last 10 years of my practice.
How has it come to this—that doctors administer so much care that they wouldn’t want for themselves? The simple, or not-so-simple, answer is this: patients, doctors, and the system.
To see how patients play a role, imagine a scenario in which someone has lost consciousness and been admitted to an emergency room. As is so often the case, no one has made a plan for this situation, and shocked and scared family members find themselves caught up in a maze of choices. They’re overwhelmed. When doctors ask if they want “everything” done, they answer yes. Then the nightmare begins. Sometimes, a family really means “do everything,” but often they just mean “do everything that’s reasonable.” The problem is that they may not know what’s reasonable, nor, in their confusion and sorrow, will they ask about it or hear what a physician may be telling them. For their part, doctors told to do “everything” will do it, whether it is reasonable or not.
The above scenario is a common one. Feeding into the problem are unrealistic expectations of what doctors can accomplish. Many people think of CPR as a reliable lifesaver when, in fact, the results are usually poor. I’ve had hundreds of people brought to me in the emergency room after getting CPR. Exactly one, a healthy man who’d had no heart troubles (for those who want specifics, he had a “tension pneumothorax”), walked out of the hospital. If a patient suffers from severe illness, old age, or a terminal disease, the odds of a good outcome from CPR are infinitesimal, while the odds of suffering are overwhelming. Poor knowledge and misguided expectations lead to a lot of bad decisions.
But of course it’s not just patients making these things happen. Doctors play an enabling role, too. The trouble is that even doctors who hate to administer futile care must find a way to address the wishes of patients and families. Imagine, once again, the emergency room with those grieving, possibly hysterical, family members. They do not know the doctor. Establishing trust and confidence under such circumstances is a very delicate thing. People are prepared to think the doctor is acting out of base motives, trying to save time, or money, or effort, especially if the doctor is advising against further treatment.
Some doctors are stronger communicators than others, and some doctors are more adamant, but the pressures they all face are similar. When I faced circumstances involving end-of-life choices, I adopted the approach of laying out only the options that I thought were reasonable (as I would in any situation) as early in the process as possible. When patients or families brought up unreasonable choices, I would discuss the issue in layman’s terms that portrayed the downsides clearly. If patients or families still insisted on treatments I considered pointless or harmful, I would offer to transfer their care to another doctor or hospital.
Should I have been more forceful at times? I know that some of those transfers still haunt me. One of the patients of whom I was most fond was an attorney from a famous political family. She had severe diabetes and terrible circulation, and, at one point, she developed a painful sore on her foot. Knowing the hazards of hospitals, I did everything I could to keep her from resorting to surgery. Still, she sought out outside experts with whom I had no relationship. Not knowing as much about her as I did, they decided to perform bypass surgery on her chronically clogged blood vessels in both legs. This didn’t restore her circulation, and the surgical wounds wouldn’t heal. Her feet became gangrenous, and she endured bilateral leg amputations. Two weeks later, in the famous medical center in which all this had occurred, she died.
It’s easy to find fault with both doctors and patients in such stories, but in many ways all the parties are simply victims of a larger system that encourages excessive treatment. In some unfortunate cases, doctors use the fee-for-service model to do everything they can, no matter how pointless, to make money. More commonly, though, doctors are fearful of litigation and do whatever they’re asked, with little feedback, to avoid getting in trouble.
Even when the right preparations have been made, the system can still swallow people up. One of my patients was a man named Jack, a 78-year-old who had been ill for years and undergone about 15 major surgical procedures. He explained to me that he never, under any circumstances, wanted to be placed on life support machines again. One Saturday, however, Jack suffered a massive stroke and got admitted to the emergency room unconscious, without his wife. Doctors did everything possible to resuscitate him and put him on life support in the ICU. This was Jack’s worst nightmare. When I arrived at the hospital and took over Jack’s care, I spoke to his wife and to hospital staff, bringing in my office notes with his care preferences. Then I turned off the life support machines and sat with him. He died two hours later.
Even with all his wishes documented, Jack hadn’t died as he’d hoped. The system had intervened. One of the nurses, I later found out, even reported my unplugging of Jack to the authorities as a possible homicide. Nothing came of it, of course; Jack’s wishes had been spelled out explicitly, and he’d left the paperwork to prove it. But the prospect of a police investigation is terrifying for any physician. I could far more easily have left Jack on life support against his stated wishes, prolonging his life, and his suffering, a few more weeks. I would even have made a little more money, and Medicare would have ended up with an additional $500,000 bill. It’s no wonder many doctors err on the side of overtreatment.
But doctors still don’t over-treat themselves. They see the consequences of this constantly. Almost anyone can find a way to die in peace at home, and pain can be managed better than ever. Hospice care, which focuses on providing terminally ill patients with comfort and dignity rather than on futile cures, provides most people with much better final days. Amazingly, studies have found that people placed in hospice care often live longer than people with the same disease who are seeking active cures. I was struck to hear on the radio recently that the famous reporter Tom Wicker had “died peacefully at home, surrounded by his family.” Such stories are, thankfully, increasingly common.
Several years ago, my older cousin Torch (born at home by the light of a flashlight—or torch) had a seizure that turned out to be the result of lung cancer that had gone to his brain. I arranged for him to see various specialists, and we learned that with aggressive treatment of his condition, including three to five hospital visits a week for chemotherapy, he would live perhaps four months. Ultimately, Torch decided against any treatment and simply took pills for brain swelling. He moved in with me.
We spent the next eight months doing a bunch of things that he enjoyed, having fun together like we hadn’t had in decades. We went to Disneyland, his first time. We’d hang out at home. Torch was a sports nut, and he was very happy to watch sports and eat my cooking. He even gained a bit of weight, eating his favorite foods rather than hospital foods. He had no serious pain, and he remained high-spirited. One day, he didn’t wake up. He spent the next three days in a coma-like sleep and then died. The cost of his medical care for those eight months, for the one drug he was taking, was about $20.
Torch was no doctor, but he knew he wanted a life of quality, not just quantity. Don’t most of us? If there is a state of the art of end-of-life care, it is this: death with dignity. As for me, my physician has my choices. They were easy to make, as they are for most physicians. There will be no heroics, and I will go gentle into that good night. Like my mentor Charlie. Like my cousin Torch. Like my fellow doctors.
Ken Murray, MD, is Clinical Assistant Professor of Family Medicine at USC.
Death’s Companion: PaperworkPaula Span : NY Times : March 15, 2012Heidi Foreman’s father died in November. Ronald Foreman, a retired sporting goods manufacturer, had been struggling with poor health for several years, and he had been in a suburban Philadelphia hospital for treatment of chronic lung disease. But Mr. Foreman was determined to check himself out so that he could celebrate Thanksgiving with his family, and he did. He died at home at 85, his wife and children with him, a few days later.
Phyllis and Ronald Foreman. After his death, the family discovered an immense number of administrative tasks were necessary.After the funeral, family members allowed themselves a couple of weeks to mourn and to not do much of anything. Then, they roused themselves to confront the long list of tasks that follow a death.
This turned out to be a separate level of hell. “There was a tidal wave of things to do,” Ms. Foreman said. “We were surprised by how much and how hard it was. When you think something’s done, it’s not. Everything takes multiple tries.”
Ms. Foreman, a marketing consultant in Chicago, invented the perfect phrase for this scut work that seems to keep expanding even as you cross chores off the list: administrivia.
Administrivia would be enough to try the patience of cheerful people at a stable time in their lives. It was worse for Ms. Foreman’s mother, Phyllis, an 82-year-old who’d just lost her mate of 60 years and had never lived alone, and for her children, scattered from New Jersey to San Francisco.
“In the midst of grief, trying to go through all this is incredibly frustrating,” Ms. Foreman told me. “You have to summon all this energy.”
So as a public service to those who are coping with the same tedious chores or may soon be, the Foreman family assembled a list of stuff to do, stuff almost everyone will have to do, after a loved one dies.
We’re leaving aside the financial matters: wills, estates, lawyers and so forth. We’re also leaving aside the sometimes wrenching, sometimes comforting process of sorting and donating clothing and personal items. We’re dealing only with administrivia, some of which can be handled online but much of which requires phone calls and letters and a whole lot of persistence.
So, first: contacting Social Security and Medicare. One interview suffices to cancel coverage or transfer it to a surviving spouse, and, the family learned, that interview can take place via phone. “Of everybody we’ve dealt with, they were the most on top of things,” Ms. Foreman said. “The ‘massive government bureaucracy’ did better than any private corporation.”
Also important: changing advance directives. Like most couples, Phyllis and Ronald Foreman had designated each other in their health care proxies and power-of-attorney documents. Now, “if something happened to my mom, we couldn’t do anything,” Ms. Foreman worried. The family’s lawyer swiftly drew up new documents to be signed and notarized.
Changing bank accounts. Fortunately, the Foremans had a joint checking account, so Mrs. Foreman had access to it after her husband’s death. Had it been in his name only, the bank would have frozen the account, and she wouldn’t have been able to access that money until a court approved the will and appointed executors — a process that can take weeks or months. Words to the wise: joint checking.
Selling the car. This task is one of many requiring a death certificate, so Ms. Foreman advises ordering multiple copies from the funeral home. It also required digging up the title to the car. The Foremans had kept important papers in a locked fireproof box in their home, so at least Mrs. Foreman knew where to look.
Changing or canceling bills and subscriptions. Utilities. Credit cards. Phones. Many of these accounts were in Mr. Foreman’s name, and switching them to his widow’s took many calls. The phone company wouldn’t do so without checking her credit rating — and who wanted to deal with that right then? — but it agreed to add Mrs. Foreman to the account.
Adjusting bill-paying. Mr. Foreman loved computers and had set up online banking for some monthly bills; others were paid automatically through his American Express account. Uncertain about which were which, Mrs. Foreman wound up double-paying several charges and receiving overdue notices for others. “Trying to get a refund from a credit card company took multiple phone calls and letters,” her daughter discovered.
Canceling monthly prescriptions. Like many other older adults, Mr. Foreman took nearly a dozen expensive medications, sent by a mail-order pharmacy in 90-day batches. After he died, “they just kept coming, and because of all the privacy laws, it was way too hard to stop them,” Ms. Foreman said. Her brother eventually stayed on the line with the pharmacy for 90 minutes and halted the flow.
Updating emergency contacts. “Here’s one most people don’t think about: My father was the emergency contact on any form my mother ever filled in,” Ms. Foreman said. Now, she and her siblings appear on doctors’ records, on Mrs. Foreman’s gym membership, on the card in her wallet.
Filing taxes. They outlast death — the Foremans’ 2011 taxes still have to be paid by April 15. A family friend who’s an accountant volunteered to handle this, and Mr. Foreman’s well-organized records made the process less onerous than it might have been. But his survivors still had to gather every 1099 and relevant receipt.
Family members also dealt with a raft of other jobs: transferring the deed to the house, tracking down insurance payments, canceling doctors’ appointments. Some families will need to look into veterans’ benefits and employer benefits as well.
Phyllis Foreman, let’s note, is healthy and lucid and computer-literate, with four children standing by when the administrivia gets too overwhelming. “What does everyone else do?” Ms. Foreman wondered. “Can’t we make it easier?”
One way to do that, of course, is to try to set up a system before it’s needed. A list of account numbers, insurance policies, phone contacts and online passwords can help family members handle these duties more easily. Another way is to share information about what lies ahead.
So if you have your own experiences with administrivia, please tell us about them in the comments section below.
I asked Ms. Foreman if she and her family were seeing light at the end of the tunnel, nearly four months after her father’s death.
“We’ve made a lot of progress,” she said cautiously. “But because things keep coming up, I don’t know where the end of the tunnel is.”
Phyllis and Ronald Foreman. After his death, the family discovered an immense number of administrative tasks were necessary.After the funeral, family members allowed themselves a couple of weeks to mourn and to not do much of anything. Then, they roused themselves to confront the long list of tasks that follow a death.
This turned out to be a separate level of hell. “There was a tidal wave of things to do,” Ms. Foreman said. “We were surprised by how much and how hard it was. When you think something’s done, it’s not. Everything takes multiple tries.”
Ms. Foreman, a marketing consultant in Chicago, invented the perfect phrase for this scut work that seems to keep expanding even as you cross chores off the list: administrivia.
Administrivia would be enough to try the patience of cheerful people at a stable time in their lives. It was worse for Ms. Foreman’s mother, Phyllis, an 82-year-old who’d just lost her mate of 60 years and had never lived alone, and for her children, scattered from New Jersey to San Francisco.
“In the midst of grief, trying to go through all this is incredibly frustrating,” Ms. Foreman told me. “You have to summon all this energy.”
So as a public service to those who are coping with the same tedious chores or may soon be, the Foreman family assembled a list of stuff to do, stuff almost everyone will have to do, after a loved one dies.
We’re leaving aside the financial matters: wills, estates, lawyers and so forth. We’re also leaving aside the sometimes wrenching, sometimes comforting process of sorting and donating clothing and personal items. We’re dealing only with administrivia, some of which can be handled online but much of which requires phone calls and letters and a whole lot of persistence.
So, first: contacting Social Security and Medicare. One interview suffices to cancel coverage or transfer it to a surviving spouse, and, the family learned, that interview can take place via phone. “Of everybody we’ve dealt with, they were the most on top of things,” Ms. Foreman said. “The ‘massive government bureaucracy’ did better than any private corporation.”
Also important: changing advance directives. Like most couples, Phyllis and Ronald Foreman had designated each other in their health care proxies and power-of-attorney documents. Now, “if something happened to my mom, we couldn’t do anything,” Ms. Foreman worried. The family’s lawyer swiftly drew up new documents to be signed and notarized.
Changing bank accounts. Fortunately, the Foremans had a joint checking account, so Mrs. Foreman had access to it after her husband’s death. Had it been in his name only, the bank would have frozen the account, and she wouldn’t have been able to access that money until a court approved the will and appointed executors — a process that can take weeks or months. Words to the wise: joint checking.
Selling the car. This task is one of many requiring a death certificate, so Ms. Foreman advises ordering multiple copies from the funeral home. It also required digging up the title to the car. The Foremans had kept important papers in a locked fireproof box in their home, so at least Mrs. Foreman knew where to look.
Changing or canceling bills and subscriptions. Utilities. Credit cards. Phones. Many of these accounts were in Mr. Foreman’s name, and switching them to his widow’s took many calls. The phone company wouldn’t do so without checking her credit rating — and who wanted to deal with that right then? — but it agreed to add Mrs. Foreman to the account.
Adjusting bill-paying. Mr. Foreman loved computers and had set up online banking for some monthly bills; others were paid automatically through his American Express account. Uncertain about which were which, Mrs. Foreman wound up double-paying several charges and receiving overdue notices for others. “Trying to get a refund from a credit card company took multiple phone calls and letters,” her daughter discovered.
Canceling monthly prescriptions. Like many other older adults, Mr. Foreman took nearly a dozen expensive medications, sent by a mail-order pharmacy in 90-day batches. After he died, “they just kept coming, and because of all the privacy laws, it was way too hard to stop them,” Ms. Foreman said. Her brother eventually stayed on the line with the pharmacy for 90 minutes and halted the flow.
Updating emergency contacts. “Here’s one most people don’t think about: My father was the emergency contact on any form my mother ever filled in,” Ms. Foreman said. Now, she and her siblings appear on doctors’ records, on Mrs. Foreman’s gym membership, on the card in her wallet.
Filing taxes. They outlast death — the Foremans’ 2011 taxes still have to be paid by April 15. A family friend who’s an accountant volunteered to handle this, and Mr. Foreman’s well-organized records made the process less onerous than it might have been. But his survivors still had to gather every 1099 and relevant receipt.
Family members also dealt with a raft of other jobs: transferring the deed to the house, tracking down insurance payments, canceling doctors’ appointments. Some families will need to look into veterans’ benefits and employer benefits as well.
Phyllis Foreman, let’s note, is healthy and lucid and computer-literate, with four children standing by when the administrivia gets too overwhelming. “What does everyone else do?” Ms. Foreman wondered. “Can’t we make it easier?”
One way to do that, of course, is to try to set up a system before it’s needed. A list of account numbers, insurance policies, phone contacts and online passwords can help family members handle these duties more easily. Another way is to share information about what lies ahead.
So if you have your own experiences with administrivia, please tell us about them in the comments section below.
I asked Ms. Foreman if she and her family were seeing light at the end of the tunnel, nearly four months after her father’s death.
“We’ve made a lot of progress,” she said cautiously. “But because things keep coming up, I don’t know where the end of the tunnel is.”