- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
When Gluten Sensitivity Isn’t Celiac Disease
By Jane E. Brody : NT Times : October 6, 2014
Supermarket shelves are now packed with foods labeled gluten-free (including some, like peanut and almond butter, that naturally lack gluten). Chefs, too, have joined the cause: Many high-end restaurants and even pizza parlors now offer gluten-free dishes.
Those who say they react to gluten, a protein in wheat and other grains, report symptoms like abdominal pain; bloating; gas;diarrhea; headache; fatigue; joint pain; foggy mind; numbness in the legs, arms or fingers; and balance problems after eating a gluten-rich food.
I suspected at first that the gluten-free craze was an attempt by some to find a physical explanation for emotional problems, similar to the “epidemic” of hypoglycemia in decades past. But a growing body of research indicates that many may be suffering a real condition called non-celiac gluten sensitivity, or NCGS.
It is not celiac disease, a far less common autoimmune condition that can destroy the small intestine. Indeed, no one has conclusively identified a physical explanation for gluten sensitivity and its array of symptoms.
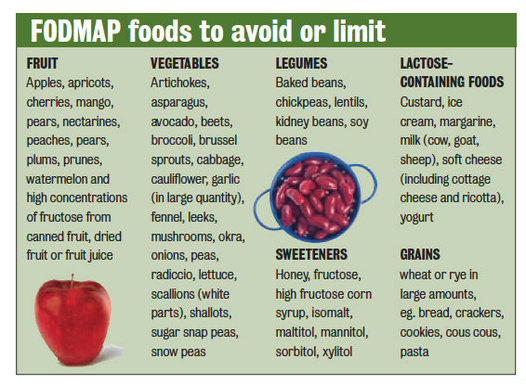
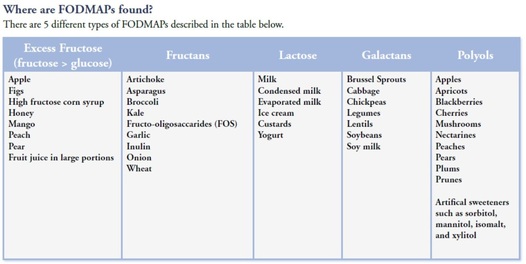
Recent studies have strongly suggested that many, and possibly most, people who react badly to gluten may have a more challenging problem: sensitivity to a long list of foods containing certain carbohydrates.
In 2011, Dr. Peter Gibson, a gastroenterologist at Monash University in Victoria, Australia, and his colleagues studied 34 people with irritable bowel syndrome who did not have celiac disease but reacted badly to wheat, a gluten-rich grain. The researchers concluded that non-celiac gluten sensitivity “may exist.”
Many of their subjects still had symptoms on a gluten-free diet, however, which prompted a second study of 37 patients with irritable bowel syndrome and non-celiac gluten sensitivity who were randomly assigned to a two-week diet low in certain carbohydrates, collectively called Fodmaps.
All patients on the special diet improved, but got significantly worse when fed gluten or whey protein. Only 8 percent of the participants reacted specifically to gluten, prompting the researchers to conclude that Fodmaps, not gluten, accounted for most of the distress.
Fodmaps is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols, sugars that draw water into the intestinal tract. They may be poorly digested or absorbed, and become fodder for colonic bacteria that produce gas and can cause abdominal distress. They are:
■ Fructose: A sugar prominent in apples, pears, watermelon, mangoes, grapes, blueberries, tomatoes and tomato concentrate, and all dried fruits; vegetables like sugar-snap peas, sweet peppers and pickles; honey; agave; and jams, dressings and drinks made with high-fructose corn syrup.
■ Lactose: The sugar in milk from cows, goats and sheep, present in ice cream, soft cheeses, sour cream and custard.
■ Fructans: Soluble fiber found in bananas, garlic, onions, leeks, artichokes, asparagus, beets, wheat and rye.
■ Galactans: Complex sugars prominent in dried peas and beans, soybeans, soy milk, broccoli, cabbage and brussels sprouts.
■ Polyols: The sugar alcohols (sweeteners) isomalt, mannitol, sorbitol and xylitol, present in stone fruits like avocado, cherries, peaches, plums and apricots.
People with irritable bowel syndrome often find that their symptoms lessen or disappear when avoiding foods rich in Fodmaps; however, it can take six to eight weeks on a low-Fodmap diet to see a significant improvement.
Experts advise those patients to eliminate all foods rich in Fodmaps at the start. (You can find a list of foods low in these carbohydrates at stanfordhealthcare.org.) Once symptoms resolve, individual foods are returned to the diet one by one to identify those to which patients react.
So what about patients who think they are sensitive only to gluten?
Dr. Joseph A. Murray, gastroenterologist at the Mayo Clinic and an expert on celiac disease, urges that they first be tested for celiac disease, a condition that has become dramatically more prevalent in recent decades. The signs of gluten sensitivity often mimic those of celiac disease, as well as irritable bowel syndrome.
Tests for celiac disease are less accurate if the diet does not currently include gluten. “Test first, test right,” Dr. Murray said in an interview. “We’re seeing people with symptoms who go on a gluten-free diet, and then we can’t make a correct diagnosis.”
With non-celiac gluten sensitivity, there is no damage to the small intestine, meaning many people may consume small amounts of gluten without incident. A forthcoming book edited by Dr. Murray, “Mayo Clinic Going Gluten Free,” lists the essential requirements for diagnosis of non-celiac gluten sensitivity:
■ Negative blood tests for celiac disease and no sign of damage on an intestinal biopsy.
■ Symptom improvement when gluten is removed from the diet.
■ Recurrence of symptoms when gluten is reintroduced.
■ No other explanation for the symptoms.
It is not yet known if the condition results from an immunological reaction similar to that seen in celiac disease, or whether gluten exerts a chemical or other negative effect on digestion.
Gluten sensitivity is not the same as a wheat allergy, a far less common problem with symptoms like swelling, itching, skin rash, tingling or burning of the mouth, and nasal congestion.
The best way to test for non-celiac gluten sensitivity (after ruling out celiac disease) is to remove all sources of gluten from one’s diet for several weeks. If the symptoms disappear, reintroduce gluten to see if they recur. Another option is to keep a food diary for a few weeks, recording everything you eat and drink and any symptoms that follow.
In addition to the inconvenience and added expense, a gluten-free diet can result in a poor intake of fiber and certain essential nutrients. It may be wise to consult a registered dietitian if you plan to go gluten-free.
By Jane E. Brody : NT Times : October 6, 2014
Supermarket shelves are now packed with foods labeled gluten-free (including some, like peanut and almond butter, that naturally lack gluten). Chefs, too, have joined the cause: Many high-end restaurants and even pizza parlors now offer gluten-free dishes.
Those who say they react to gluten, a protein in wheat and other grains, report symptoms like abdominal pain; bloating; gas;diarrhea; headache; fatigue; joint pain; foggy mind; numbness in the legs, arms or fingers; and balance problems after eating a gluten-rich food.
I suspected at first that the gluten-free craze was an attempt by some to find a physical explanation for emotional problems, similar to the “epidemic” of hypoglycemia in decades past. But a growing body of research indicates that many may be suffering a real condition called non-celiac gluten sensitivity, or NCGS.
It is not celiac disease, a far less common autoimmune condition that can destroy the small intestine. Indeed, no one has conclusively identified a physical explanation for gluten sensitivity and its array of symptoms.
Recent studies have strongly suggested that many, and possibly most, people who react badly to gluten may have a more challenging problem: sensitivity to a long list of foods containing certain carbohydrates.
In 2011, Dr. Peter Gibson, a gastroenterologist at Monash University in Victoria, Australia, and his colleagues studied 34 people with irritable bowel syndrome who did not have celiac disease but reacted badly to wheat, a gluten-rich grain. The researchers concluded that non-celiac gluten sensitivity “may exist.”
Many of their subjects still had symptoms on a gluten-free diet, however, which prompted a second study of 37 patients with irritable bowel syndrome and non-celiac gluten sensitivity who were randomly assigned to a two-week diet low in certain carbohydrates, collectively called Fodmaps.
All patients on the special diet improved, but got significantly worse when fed gluten or whey protein. Only 8 percent of the participants reacted specifically to gluten, prompting the researchers to conclude that Fodmaps, not gluten, accounted for most of the distress.
Fodmaps is an acronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols, sugars that draw water into the intestinal tract. They may be poorly digested or absorbed, and become fodder for colonic bacteria that produce gas and can cause abdominal distress. They are:
■ Fructose: A sugar prominent in apples, pears, watermelon, mangoes, grapes, blueberries, tomatoes and tomato concentrate, and all dried fruits; vegetables like sugar-snap peas, sweet peppers and pickles; honey; agave; and jams, dressings and drinks made with high-fructose corn syrup.
■ Lactose: The sugar in milk from cows, goats and sheep, present in ice cream, soft cheeses, sour cream and custard.
■ Fructans: Soluble fiber found in bananas, garlic, onions, leeks, artichokes, asparagus, beets, wheat and rye.
■ Galactans: Complex sugars prominent in dried peas and beans, soybeans, soy milk, broccoli, cabbage and brussels sprouts.
■ Polyols: The sugar alcohols (sweeteners) isomalt, mannitol, sorbitol and xylitol, present in stone fruits like avocado, cherries, peaches, plums and apricots.
People with irritable bowel syndrome often find that their symptoms lessen or disappear when avoiding foods rich in Fodmaps; however, it can take six to eight weeks on a low-Fodmap diet to see a significant improvement.
Experts advise those patients to eliminate all foods rich in Fodmaps at the start. (You can find a list of foods low in these carbohydrates at stanfordhealthcare.org.) Once symptoms resolve, individual foods are returned to the diet one by one to identify those to which patients react.
So what about patients who think they are sensitive only to gluten?
Dr. Joseph A. Murray, gastroenterologist at the Mayo Clinic and an expert on celiac disease, urges that they first be tested for celiac disease, a condition that has become dramatically more prevalent in recent decades. The signs of gluten sensitivity often mimic those of celiac disease, as well as irritable bowel syndrome.
Tests for celiac disease are less accurate if the diet does not currently include gluten. “Test first, test right,” Dr. Murray said in an interview. “We’re seeing people with symptoms who go on a gluten-free diet, and then we can’t make a correct diagnosis.”
With non-celiac gluten sensitivity, there is no damage to the small intestine, meaning many people may consume small amounts of gluten without incident. A forthcoming book edited by Dr. Murray, “Mayo Clinic Going Gluten Free,” lists the essential requirements for diagnosis of non-celiac gluten sensitivity:
■ Negative blood tests for celiac disease and no sign of damage on an intestinal biopsy.
■ Symptom improvement when gluten is removed from the diet.
■ Recurrence of symptoms when gluten is reintroduced.
■ No other explanation for the symptoms.
It is not yet known if the condition results from an immunological reaction similar to that seen in celiac disease, or whether gluten exerts a chemical or other negative effect on digestion.
Gluten sensitivity is not the same as a wheat allergy, a far less common problem with symptoms like swelling, itching, skin rash, tingling or burning of the mouth, and nasal congestion.
The best way to test for non-celiac gluten sensitivity (after ruling out celiac disease) is to remove all sources of gluten from one’s diet for several weeks. If the symptoms disappear, reintroduce gluten to see if they recur. Another option is to keep a food diary for a few weeks, recording everything you eat and drink and any symptoms that follow.
In addition to the inconvenience and added expense, a gluten-free diet can result in a poor intake of fiber and certain essential nutrients. It may be wise to consult a registered dietitian if you plan to go gluten-free.