- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
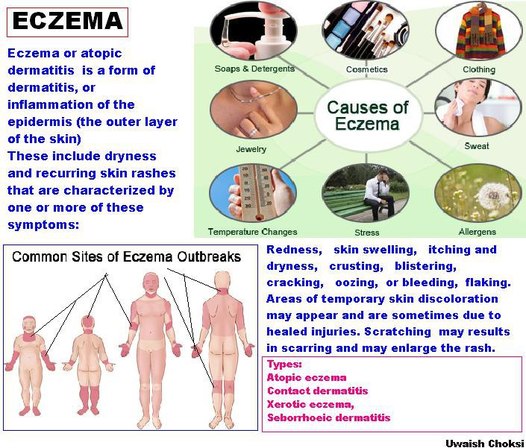
Understanding Eczema to Treat It
By Jane E. Brody : NY Times : July 29, 2013
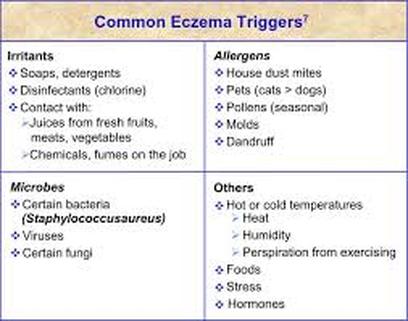
Summer is both a blessing and curse for millions of people afflicted with a common chronic skin condition called eczema. The dry, red and usually intolerably itchy patches often recede when the air is warm and damp and skin is exposed more often to sunlight.
Yet, for many of the 15 million Americans with eczema, shedding the clothes may be embarrassing and, in the case of children, may result in teasing and exclusion. Even for those who are comfortable in a bathing suit, swimming in a pool can be problematic if sensitivity to chlorine worsens the condition.
In industrialized countries, eczema has become two or three times more common in recent decades. Only part of this rise can be attributed to better diagnosis. Now between 15 and 30 percent of children and 2 percent to 10 percent of adults have eczema, which nearly always begins in the first five years of life. Fortunately, in more than two-thirds of children with eczema, the condition resolves on its own before adolescence.
The medical name for eczema is atopic dermatitis, which reflects the immunological nature of the condition. It is more common among children living in cities than those in rural areas. According to the so-called hygiene hypothesis, exposure to infectious agents early in life offers protection against allergic diseases. The more hygienic a child’s environment, the greater the risk.
Eczema is not contagious, but more than one member of a family may be afflicted. The condition seems to have a genetic component. In identical twins, 77 percent will both have eczema, but it occurs in both fraternal twins only 15 percent of the time. My sons, who are identical twins, had eczema as young children, and one still has it in his 40s.
Another indication is the fact that people with celiac disease (a gluten intolerance) are three times more likely to have eczema; relatives of celiac patients are twice as likely to have eczema.
Eczema is often called “the itch you can’t scratch,” though a wiser description would be “the itch you shouldn’t scratch.” Scratching can make the lesions worse and expose the skin to infection.
“Scratching the spot when it’s itchy brings relief only as long as you scratch it,” said my son, Lorin. “After scratching, the itch generally stays the same or worsens. It’s better not to scratch, though sometimes the itch is so intense that scratching feels compulsory.”
Although there is no known cure for eczema, flare-ups can nearly always be minimized and sometimes prevented, and recent research has identified factors involved in its development that may lead to new treatments to control it more effectively.
Normal skin provides a remarkably effective physical and chemical barrier to substances in the environment. It also prevents substances that should remain in the body from escaping.
As Dr. Thomas Bieber, a dermatologist at the University of Bonn in Germany, explained in The New England Journal of Medicine, the hallmark of eczema is an alteration in the skin that allows essential water to escape and environmental allergens (like those from pollen, dust mites and food) to enter. The result is dry, itchy, inflamed patches that are sometimes misdiagnosed as psoriasis.
Eczematous skin also lacks normal amounts of a natural antimicrobial agent called cathelicidin, leaving it susceptible to infections that can be hard to control. More than 90 percent of people with eczema have colonies of the bacterium Staphylococcus aureus growing on their skin and contributing to the skin’s allergic sensitivity and inflammation, Dr. Bieber reported. Scratching the lesions enhances the ability of these bacteria to further disrupt the skin’s barrier function.
While it has long been known that the skin’s outermost layer functions poorly in people with eczema, researchers at the University of Rochester have identified another reason eczematous skin is susceptible to invasion by allergens. Dr. Anna De Benedetto and co-authors showed that a protective protein called claudin-1 is significantly weakened in the skin of eczema patients but not in those with normal skin or other skin conditions.
When claudin-1 is reduced, the “tight junctions” between skin cells become leaky and permeable to environmental allergens and infectious agents. If future studies confirm these findings, developing treatments that strengthen this barrier should improve control of eczema.
Current treatment focuses on reducing inflammation, loss of moisture and colonization by bacteria. Doctors typically recommend a prescription steroid, used topically in tiny amounts, coupled with an over-the-counter moisturizer applied generously right after showering to hold water in the skin. Only mild, nondrying bath soaps should be used.
Overly expensive and exotic skin products are not necessary, according to Dr. Lisa A. Beck, a dermatologist at the University of Rochester. But finding the most helpful products may require trial and error.
For example, my son tried several steroids before finding that mometasone furoate, the generic version of Elocon, is most effective for him. He has also used coal tar-based shampoo, like Neutrogena T/Gel, for occasional eczema on his scalp.
In selecting a moisturizer (often called an emollient), choose a product that contains no scent, which itself can be a skin irritant.
An acquaintance who suffered for years with widespread eczema finally found relief last year when her doctor suggested she try taking a nonsedating antihistamine, like loratadine (Claritin), fexofenadine (Allegra) or cetirizine (Zyrtec).
Sweat can trigger an outbreak, so it is best to shower as soon as possible after a sweat-inducing activity. Stress can provoke flare-ups in some people with eczema, so measures to reduce stress may be helpful.
Food allergies show up as eczema in some patients. Eliminating one potential culprit at a time, like dairy products, eggs or nuts, may reveal an eczema-inducer.
Some people develop a form of eczema that results from skin contact with an irritant, not unlike a reaction to poison ivy. Contact eczema is often an occupational disease stemming from exposure to detergents, for example, or various cleaning agents or wet cement. The condition may show up only after the skin is exposed to sunlight. People with eczema on their hands are usually advised to wear cotton-lined waterproof gloves when washing dishes or working with irritating substances.
By Jane E. Brody : NY Times : July 29, 2013
Summer is both a blessing and curse for millions of people afflicted with a common chronic skin condition called eczema. The dry, red and usually intolerably itchy patches often recede when the air is warm and damp and skin is exposed more often to sunlight.
Yet, for many of the 15 million Americans with eczema, shedding the clothes may be embarrassing and, in the case of children, may result in teasing and exclusion. Even for those who are comfortable in a bathing suit, swimming in a pool can be problematic if sensitivity to chlorine worsens the condition.
In industrialized countries, eczema has become two or three times more common in recent decades. Only part of this rise can be attributed to better diagnosis. Now between 15 and 30 percent of children and 2 percent to 10 percent of adults have eczema, which nearly always begins in the first five years of life. Fortunately, in more than two-thirds of children with eczema, the condition resolves on its own before adolescence.
The medical name for eczema is atopic dermatitis, which reflects the immunological nature of the condition. It is more common among children living in cities than those in rural areas. According to the so-called hygiene hypothesis, exposure to infectious agents early in life offers protection against allergic diseases. The more hygienic a child’s environment, the greater the risk.
Eczema is not contagious, but more than one member of a family may be afflicted. The condition seems to have a genetic component. In identical twins, 77 percent will both have eczema, but it occurs in both fraternal twins only 15 percent of the time. My sons, who are identical twins, had eczema as young children, and one still has it in his 40s.
Another indication is the fact that people with celiac disease (a gluten intolerance) are three times more likely to have eczema; relatives of celiac patients are twice as likely to have eczema.
Eczema is often called “the itch you can’t scratch,” though a wiser description would be “the itch you shouldn’t scratch.” Scratching can make the lesions worse and expose the skin to infection.
“Scratching the spot when it’s itchy brings relief only as long as you scratch it,” said my son, Lorin. “After scratching, the itch generally stays the same or worsens. It’s better not to scratch, though sometimes the itch is so intense that scratching feels compulsory.”
Although there is no known cure for eczema, flare-ups can nearly always be minimized and sometimes prevented, and recent research has identified factors involved in its development that may lead to new treatments to control it more effectively.
Normal skin provides a remarkably effective physical and chemical barrier to substances in the environment. It also prevents substances that should remain in the body from escaping.
As Dr. Thomas Bieber, a dermatologist at the University of Bonn in Germany, explained in The New England Journal of Medicine, the hallmark of eczema is an alteration in the skin that allows essential water to escape and environmental allergens (like those from pollen, dust mites and food) to enter. The result is dry, itchy, inflamed patches that are sometimes misdiagnosed as psoriasis.
Eczematous skin also lacks normal amounts of a natural antimicrobial agent called cathelicidin, leaving it susceptible to infections that can be hard to control. More than 90 percent of people with eczema have colonies of the bacterium Staphylococcus aureus growing on their skin and contributing to the skin’s allergic sensitivity and inflammation, Dr. Bieber reported. Scratching the lesions enhances the ability of these bacteria to further disrupt the skin’s barrier function.
While it has long been known that the skin’s outermost layer functions poorly in people with eczema, researchers at the University of Rochester have identified another reason eczematous skin is susceptible to invasion by allergens. Dr. Anna De Benedetto and co-authors showed that a protective protein called claudin-1 is significantly weakened in the skin of eczema patients but not in those with normal skin or other skin conditions.
When claudin-1 is reduced, the “tight junctions” between skin cells become leaky and permeable to environmental allergens and infectious agents. If future studies confirm these findings, developing treatments that strengthen this barrier should improve control of eczema.
Current treatment focuses on reducing inflammation, loss of moisture and colonization by bacteria. Doctors typically recommend a prescription steroid, used topically in tiny amounts, coupled with an over-the-counter moisturizer applied generously right after showering to hold water in the skin. Only mild, nondrying bath soaps should be used.
Overly expensive and exotic skin products are not necessary, according to Dr. Lisa A. Beck, a dermatologist at the University of Rochester. But finding the most helpful products may require trial and error.
For example, my son tried several steroids before finding that mometasone furoate, the generic version of Elocon, is most effective for him. He has also used coal tar-based shampoo, like Neutrogena T/Gel, for occasional eczema on his scalp.
In selecting a moisturizer (often called an emollient), choose a product that contains no scent, which itself can be a skin irritant.
An acquaintance who suffered for years with widespread eczema finally found relief last year when her doctor suggested she try taking a nonsedating antihistamine, like loratadine (Claritin), fexofenadine (Allegra) or cetirizine (Zyrtec).
Sweat can trigger an outbreak, so it is best to shower as soon as possible after a sweat-inducing activity. Stress can provoke flare-ups in some people with eczema, so measures to reduce stress may be helpful.
Food allergies show up as eczema in some patients. Eliminating one potential culprit at a time, like dairy products, eggs or nuts, may reveal an eczema-inducer.
Some people develop a form of eczema that results from skin contact with an irritant, not unlike a reaction to poison ivy. Contact eczema is often an occupational disease stemming from exposure to detergents, for example, or various cleaning agents or wet cement. The condition may show up only after the skin is exposed to sunlight. People with eczema on their hands are usually advised to wear cotton-lined waterproof gloves when washing dishes or working with irritating substances.