- RETIREMENT ANNOUNCEMENT
- HOME PAGE
- "MYCHART" the new patient portal
- BELMONT MEDICAL ASSOCIATES
- MOUNT AUBURN HOSPITAL
- EMERGENCIES
- PRACTICE PHILOSOPHY
- MY RESUME
- TELEMEDICINE CONSULTATION
- CONTACT ME
- LAB RESULTS
- ePRESCRIPTIONS
- eREFERRALS
- RECORD RELEASE
- MEDICAL SCRIBE
- PHYSICIAN ASSISTANT (PA)
- Medicare Annual Wellness Visit
- Case management/Social work
- Quality Care Measures
- Emergency closing notice
- FEEDBACK
- Talking to your doctor
- Choosing..... and losing a doctor
- INDEX A - Z
- ALLERGIC REACTIONS
- Alternative Medicine
- Alzheimer's Disease
- Bladder Problems
- Blood disorders
- Cancer Concerns
- GENETIC TESTING FOR HEREDITARY CANCER
- Chronic Obstructive Pulmonary Disease
- Controversial Concerns
- CPR : Learn and save a life
- CRP : Inflammatory marker
- Diabetes Management
- Dizziness, Vertigo,Tinnitus and Hearing Loss
- EXERCISE
- FEMALE HEALTH
-
GASTROINTESTINAL topics
- Appendicitis
- BRAT diet
- Celiac Disease or Sprue
- Crohn's Disease
- Gastroenterologists for Colon Cancer Screening
- Colonoscopy PREP
- Constipation
- Gluten sensitivity, but not celiac disease
- Heartburn and GERD
- Hemorrhoids and Anal fissure
- Irritable Bowel Syndrome (IBS)
- Inflammatory Bowel Disease
- NASH : Non Alcoholic Steato Hepatitis
- FEET PROBLEMS
- HEART RELATED topics
-
INFECTIOUS DISEASES
- Antibiotic Resistance
- Cat bites >
- Clostridia difficile infection - the "antibiotic associated germ"
- CORONA VIRUS
- Dengue Fever and Chikungunya Fever
- Food borne illnesses
- Shingles Vaccine
- Hepatitis B
- Hepatitis C
- Herpes
- Influenza
- Helicobacter pylori - the "ulcer germ"
- HIV Screening
- Lyme and other tick borne diseases
- Measles
- Meningitis
- MRSA (Staph infection)
- Norovirus
- Sexually Transmitted Diseases
- Shingles (Herpes Zoster)
- Sinusitis
- West Nile Virus
- Whooping Cough (Pertussis)
- Zika virus and pregnancy
- INSURANCE related topics
- KIDNEY STONES
- LEG CRAMPS
- LIBRARY for patients
- LIFE DECISIONS
- MALE HEALTH
- Medication/Drug side effects
- MEDICAL MARIJUANA
- MENTAL HEALTH
- Miscellaneous Articles
-
NUTRITION - EXERCISE - WEIGHT
- Cholesterol : New guidelines for treatment
- Advice to lower your cholesterol
- Cholesterol : Control
- Cholesterol : Raising your HDL Level
- Exercise
- Food : Making Smart Choices
- Food : Making Poor Choices
- Food : Grape Fruit and Drug Interaction
- Food : Vitamins, Minerals and Supplements
- Omega 3 fatty acids
- Vitamin B12 deficiency
- Vitamin D
- Weight Loss
- ORTHOPEDICS
- PAIN
- PATIENTS' RIGHTS
- SKIN
- SLEEP
- SMOKING
- STROKE
- THYROID
- SUBSTANCE ABUSE
- Travel and Vaccination
- TREMOR
- Warfarin Anticoagulation
- OTHER STUFF FOLLOWS
- Fact or Opinion?
- Hippocratic Oath
- FREE ADVICE.......for what its worth!
- LAUGHTER.....is the best medicine
- Physicians Pet Peeves
- PHOTO ALBUM - its not all work!
- Cape Town, South Africa
- Tribute page
- The 100 Club
- Free Wi-Fi
FOOD BORNE ILLNESSES
http://www.cdc.gov/foodsafety/diseases/
Food Illness and the Kitchen
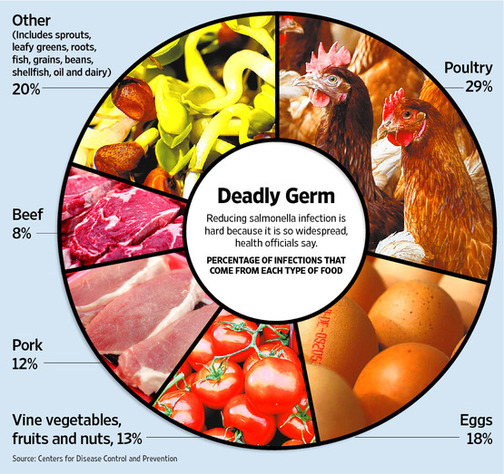
Salmonella Infections Rose Last Year; Home Cooks Fail to Act Safely, Studies Say
By Laura Landro : WSJ June 14, 2011
A rise in infections from salmonella, the deadliest food-borne germ, is spurring a new push by health officials to prevent food contamination at the last line of defense: the home kitchen.
Despite scary reports from Europe, most food-borne illnesses are on the decline in the U.S. Dangerous E. coli infections, for instance, have been cut in half over the past 15 years, thanks to better surveillance and preventive measures.
But over the same period, salmonella infections have remained roughly constant. More than a million people a year get sick from salmonella poisoning, according to recent data from the Centers for Disease Control and Prevention. The number of confirmed cases of salmonella infection last year rose 10%, erasing a small improvement in 2009, the CDC said.
The U.S. Department of Agriculture last month revised its recommendations for safely cooking pork, steaks, roasts and chops to avoid salmonella and other infections. The USDA also is planning to launch its first national multimedia campaign this summer on safe-food preparation. And some employee-benefit health plans are running seminars on how to keep food safe during the hot summer months.
"We know it is our job to make food as safe as possible before it reaches consumers' tables, but knowing the risk is not zero and it may never be zero, we have to get the word out about what consumers can do," says Elisabeth Hagen, undersecretary for food safety at the USDA.
Salmonella can contaminate many foods, including raw meat, eggs and vegetables. It is often described as the sneakiest germ: It can enter a cantaloupe through a knife that cuts through an unwashed rind, for instance. And it can contaminate eggs before the shell is formed inside a hen. While salmonella may cause only mild illness that lasts a few days, it also leads to more hospitalizations and deaths than any other kind of germ found in food.
Outbreaks of salmonella also have been linked to processed foods including pot pies and peanut butter. Although salmonella can be destroyed by proper cooking, when it comes to foods like peanut butter, consumers can do little to prevent exposure.
A growing number of studies show that many consumers fail to follow recommended practices for food preparation, such as safely defrosting meat, using a meat thermometer at the end of cooking to test for internal "doneness" and properly chilling leftovers.
One online survey, which polled 1,000 Americans this spring, found 79% of respondents said they wash their hands with soap and water when handling food, down from 89% last year and 92% in 2008. The survey, conducted by the nonprofit International Food Information Council Foundation, a research group overseen by university, government and food-company trustees, also found that 71% of respondents said they washed cutting boards with soap and water, down from 78% in 2010 and 84% in 2008.
Even when home cooks know about safe food-handling practices they don't always follow them, says Michael Shapiro, an associate professor of media psychology at Cornell University. In focus groups used to help design more effective messages for the nonprofit Partnership for Food Safety Education, some cooks said employing food thermometers might indicate to others that they didn't know what they were doing or were an unsafe cook, Mr. Shapiro says.
"We've been rather stupid as a society about our attitudes towards food, and people never want to consider the possibility that it was something that happened in their own home," says Elizabeth Scott, co-director of the Center for Hygiene and Health in Home and Community at Simmons College in Boston.
Amy Emberle's son Ryan, then 2 years old, contracted a salmonella infection in 2007 that was later traced to microwave pot pies made by ConAgra Foods. It took about three weeks to confirm salmonella was the culprit, during which time the toddler lost nearly 10 pounds from constant vomiting, bloody diarrhea and severe dehydration, says Ms. Emberle, an assistant quality manager for an aerospace manufacturer in Nebraska.
"Once you go through something like this you are so much more conscious of the potential for food-borne illness," says Ms. Emberle, whose son recovered. She says she now takes extra precautions when reading cooking instructions and preparing fresh foods.
A lawsuit Ms. Emberle brought against the company was settled for an undisclosed sum. ConAgra in October 2007 recalled all pot pies produced in its Marshall, Mo., plant. The company says it has invested more than $100 million in improving food safety since 2007. It made cooking instructions clearer on its packaging with visual cues such as a thermometer with the proper temperature and phrases such as "cook until steaming" to help consumers understand when the food is cooked properly.
Federal health officials are applying lessons learned from reducing E. coli infections to tackle salmonella's spread, and legislation passed last year gives the Food and Drug Administration broad authority to regulate food facilities.
The USDA's new recommendations suggest cooking whole cuts of meat to 145 degrees Fahrenheit as measured with a food thermometer placed in the thickest part of the meat. Then, the meat should be allowed to rest for three minutes before being carved or consumed to destroy any remaining pathogens. The USDA said pork could be cooked to 145 degrees safely, instead of 160 degrees previously recommended with no rest time; as long as the rest time is added to the lower temperature, the meat is safe even if it still looks pink, the USDA said. Ground meats should be cooked to 160 degrees, with no rest time required, and the safe cooking temperature for all poultry products is 165 degrees.
The Partnership for Food Safety Education, whose members include food-industry associations and food-science professionals, offers cleaning tips for consumers on its fightbac.org website. These include washing hands with warm water and soap for at least 20 seconds after handling food and using the bathroom, and washing surfaces with a mixture of ¾ teaspoon of bleach per quart of water for added protection against bacteria. It also suggests using paper towels, since cloth towels and sponges can be contaminated after use.
"Your don't have to go crazy, but just make sure you clean the kitchen counter when meat juice falls on it and cook food to proper temperatures," says Martin Bucknavage, a food-safety expert at Penn Sate University. "When we have a lapse in good practices, salmonella is an organism that can really take advantage of that." Also important, says Mr. Bucknavage, is cooling hot food after it is prepared but not consumed to avoid new bacteria growth. And for those who like runny eggs, he says, "there's always a potential that salmonella could be there" if the egg isn't fully cooked.
Nancy Donley, president of Stop Foodborne Illness, a consumer group for food-safety awareness, lost her 6-year-old son to an E. coli infection from eating undercooked hamburger in 1993. Back then, she says, she wrongly assumed food at a supermarket was safe. The CDC's reports that overall food-borne infections are down may be misinterpreted by consumers as signaling the danger is past, she warns.
"The problem is that food-safety messages dance around trying not to scare people too much, and then we get conflicting messages that say we have the safest food supply in the world," Ms. Donley says. "Consumers may then think, if it's so safe, why do I have to do anything?" Her advice: "We are never going to have a 100% safe food supply, so consider it contaminated when you bring it in the house, and practice safe food handling."
Corrections & Amplifications
Cleaning surfaces with a mixture of ¾ teaspoon of bleach per quart of water can provide added protection against bacteria. A previous version of this column used an incorrect formula of ¾ of a teaspoon per gallon.
Salmonella Infections Rose Last Year; Home Cooks Fail to Act Safely, Studies Say
By Laura Landro : WSJ June 14, 2011
A rise in infections from salmonella, the deadliest food-borne germ, is spurring a new push by health officials to prevent food contamination at the last line of defense: the home kitchen.
Despite scary reports from Europe, most food-borne illnesses are on the decline in the U.S. Dangerous E. coli infections, for instance, have been cut in half over the past 15 years, thanks to better surveillance and preventive measures.
But over the same period, salmonella infections have remained roughly constant. More than a million people a year get sick from salmonella poisoning, according to recent data from the Centers for Disease Control and Prevention. The number of confirmed cases of salmonella infection last year rose 10%, erasing a small improvement in 2009, the CDC said.
The U.S. Department of Agriculture last month revised its recommendations for safely cooking pork, steaks, roasts and chops to avoid salmonella and other infections. The USDA also is planning to launch its first national multimedia campaign this summer on safe-food preparation. And some employee-benefit health plans are running seminars on how to keep food safe during the hot summer months.
"We know it is our job to make food as safe as possible before it reaches consumers' tables, but knowing the risk is not zero and it may never be zero, we have to get the word out about what consumers can do," says Elisabeth Hagen, undersecretary for food safety at the USDA.
Salmonella can contaminate many foods, including raw meat, eggs and vegetables. It is often described as the sneakiest germ: It can enter a cantaloupe through a knife that cuts through an unwashed rind, for instance. And it can contaminate eggs before the shell is formed inside a hen. While salmonella may cause only mild illness that lasts a few days, it also leads to more hospitalizations and deaths than any other kind of germ found in food.
Outbreaks of salmonella also have been linked to processed foods including pot pies and peanut butter. Although salmonella can be destroyed by proper cooking, when it comes to foods like peanut butter, consumers can do little to prevent exposure.
A growing number of studies show that many consumers fail to follow recommended practices for food preparation, such as safely defrosting meat, using a meat thermometer at the end of cooking to test for internal "doneness" and properly chilling leftovers.
One online survey, which polled 1,000 Americans this spring, found 79% of respondents said they wash their hands with soap and water when handling food, down from 89% last year and 92% in 2008. The survey, conducted by the nonprofit International Food Information Council Foundation, a research group overseen by university, government and food-company trustees, also found that 71% of respondents said they washed cutting boards with soap and water, down from 78% in 2010 and 84% in 2008.
Even when home cooks know about safe food-handling practices they don't always follow them, says Michael Shapiro, an associate professor of media psychology at Cornell University. In focus groups used to help design more effective messages for the nonprofit Partnership for Food Safety Education, some cooks said employing food thermometers might indicate to others that they didn't know what they were doing or were an unsafe cook, Mr. Shapiro says.
"We've been rather stupid as a society about our attitudes towards food, and people never want to consider the possibility that it was something that happened in their own home," says Elizabeth Scott, co-director of the Center for Hygiene and Health in Home and Community at Simmons College in Boston.
Amy Emberle's son Ryan, then 2 years old, contracted a salmonella infection in 2007 that was later traced to microwave pot pies made by ConAgra Foods. It took about three weeks to confirm salmonella was the culprit, during which time the toddler lost nearly 10 pounds from constant vomiting, bloody diarrhea and severe dehydration, says Ms. Emberle, an assistant quality manager for an aerospace manufacturer in Nebraska.
"Once you go through something like this you are so much more conscious of the potential for food-borne illness," says Ms. Emberle, whose son recovered. She says she now takes extra precautions when reading cooking instructions and preparing fresh foods.
A lawsuit Ms. Emberle brought against the company was settled for an undisclosed sum. ConAgra in October 2007 recalled all pot pies produced in its Marshall, Mo., plant. The company says it has invested more than $100 million in improving food safety since 2007. It made cooking instructions clearer on its packaging with visual cues such as a thermometer with the proper temperature and phrases such as "cook until steaming" to help consumers understand when the food is cooked properly.
Federal health officials are applying lessons learned from reducing E. coli infections to tackle salmonella's spread, and legislation passed last year gives the Food and Drug Administration broad authority to regulate food facilities.
The USDA's new recommendations suggest cooking whole cuts of meat to 145 degrees Fahrenheit as measured with a food thermometer placed in the thickest part of the meat. Then, the meat should be allowed to rest for three minutes before being carved or consumed to destroy any remaining pathogens. The USDA said pork could be cooked to 145 degrees safely, instead of 160 degrees previously recommended with no rest time; as long as the rest time is added to the lower temperature, the meat is safe even if it still looks pink, the USDA said. Ground meats should be cooked to 160 degrees, with no rest time required, and the safe cooking temperature for all poultry products is 165 degrees.
The Partnership for Food Safety Education, whose members include food-industry associations and food-science professionals, offers cleaning tips for consumers on its fightbac.org website. These include washing hands with warm water and soap for at least 20 seconds after handling food and using the bathroom, and washing surfaces with a mixture of ¾ teaspoon of bleach per quart of water for added protection against bacteria. It also suggests using paper towels, since cloth towels and sponges can be contaminated after use.
"Your don't have to go crazy, but just make sure you clean the kitchen counter when meat juice falls on it and cook food to proper temperatures," says Martin Bucknavage, a food-safety expert at Penn Sate University. "When we have a lapse in good practices, salmonella is an organism that can really take advantage of that." Also important, says Mr. Bucknavage, is cooling hot food after it is prepared but not consumed to avoid new bacteria growth. And for those who like runny eggs, he says, "there's always a potential that salmonella could be there" if the egg isn't fully cooked.
Nancy Donley, president of Stop Foodborne Illness, a consumer group for food-safety awareness, lost her 6-year-old son to an E. coli infection from eating undercooked hamburger in 1993. Back then, she says, she wrongly assumed food at a supermarket was safe. The CDC's reports that overall food-borne infections are down may be misinterpreted by consumers as signaling the danger is past, she warns.
"The problem is that food-safety messages dance around trying not to scare people too much, and then we get conflicting messages that say we have the safest food supply in the world," Ms. Donley says. "Consumers may then think, if it's so safe, why do I have to do anything?" Her advice: "We are never going to have a 100% safe food supply, so consider it contaminated when you bring it in the house, and practice safe food handling."
Corrections & Amplifications
Cleaning surfaces with a mixture of ¾ teaspoon of bleach per quart of water can provide added protection against bacteria. A previous version of this column used an incorrect formula of ¾ of a teaspoon per gallon.
What is foodborne disease?
Foodborne disease is caused by consuming contaminated foods or beverages. Many different disease-causing microbes, or pathogens, can contaminate foods, so there are many different foodborne infections. In addition, poisonous chemicals, or other harmful substances can cause foodborne diseases if they are present in food.
More than 250 different foodborne diseases have been described. Most of these diseases are infections, caused by a variety of bacteria, viruses, and parasites that can be foodborne. Other diseases are poisonings, caused by harmful toxins or chemicals that have contaminated the food, for example, poisonous mushrooms. These different diseases have many different symptoms, so there is no one "syndrome" that is foodborne illness. However, the microbe or toxin enters the body through the gastrointestinal tract, and often causes the first symptoms there, so nausea, vomiting, abdominal cramps and diarrhea are common symptoms in many foodborne diseases.
Many microbes can spread in more than one way, so we cannot always know that a disease is foodborne. The distinction matters, because public health authorities need to know how a particular disease is spreading to take the appropriate steps to stop it. For example, Escherichia coli O157:H7 infections can spread through contaminated food, contaminated drinking water, contaminated swimming water, and from toddler to toddler at a day care center. Depending on which means of spread caused a case, the measures to stop other cases from occurring could range from removing contaminated food from stores, chlorinating a swimming pool, or closing a child day care center.
What are the most common foodborne diseases?
The most commonly recognized foodborne infections are those caused by the bacteria Campylobacter, Salmonella, and E. coli O157:H7, and by a group of viruses called calicivirus, also known as the Norwalk and Norwalk-like viruses.
Campylobacter is a bacterial pathogen that causes fever, diarrhea, and abdominal cramps. It is the most commonly identified bacterial cause of diarrheal illness in the world. These bacteria live in the intestines of healthy birds, and most raw poultry meat has Campylobacter on it. Eating undercooked chicken, or other food that has been contaminated with juices dripping from raw chicken is the most frequent source of this infection.
Salmonella is also a bacterium that is widespread in the intestines of birds, reptiles and mammals. It can spread to humans via a variety of different foods of animal origin. The illness it causes, salmonellosis, typically includes fever, diarrhea and abdominal cramps. In persons with poor underlying health or weakened immune systems, it can invade the bloodstream and cause life-threatening infections.
E. coli O157:H7 is a bacterial pathogen that has a reservoir in cattle and other similar animals. Human illness typically follows consumption of food or water that has been contaminated with microscopic amounts of cow feces. The illness it causes is often a severe and bloody diarrhea and painful abdominal cramps, without much fever. In 3% to 5% of cases, a complication called hemolytic uremic syndrome (HUS) can occur several weeks after the initial symptoms. This severe complication includes temporary anemia, profuse bleeding, and kidney failure.
Calicivirus, or Norwalk-like virus is an extremely common cause of foodborne illness, though it is rarely diagnosed, because the laboratory test is not widely available. It causes an acute gastrointestinal illness, usually with more vomiting than diarrhea, that resolves within two days. Unlike many foodborne pathogens that have animal reservoirs, it is believed that Norwalk-like viruses spread primarily from one infected person to another. Infected kitchen workers can contaminate a salad or sandwich as they prepare it, if they have the virus on their hands. Infected fishermen have contaminated oysters as they harvested them.
Some common diseases are occasionally foodborne, even though they are usually transmitted by other routes. These include infections caused by Shigella, hepatitis A, and the parasites Giardia lamblia and Cryptosporidia. Even strep throats have been transmitted occasionally through food.
In addition to disease caused by direct infection, some foodborne diseases are caused by the presence of a toxin in the food that was produced by a microbe in the food. For example, the bacterium Staphylococcus aureus can grow in some foods and produce a toxin that causes intense vomiting. The rare but deadly disease botulism occurs when the bacterium Clostridium botulinum grows and produces a powerful paralytic toxin in foods. These toxins can produce illness even if the microbes that produced them are no longer there.
Other toxins and poisonous chemicals can cause foodborne illness. People can become ill if a pesticide is inadvertently added to a food, or if naturally poisonous substances are used to prepare a meal. Every year, people become ill after mistaking poisonous mushrooms for safe species, or after eating poisonous reef fishes.
Are the types of foodborne diseases changing?
The spectrum of foodborne diseases is constantly changing. A century ago, typhoid fever, tuberculosis and cholera were common foodborne diseases. Improvements in food safety, such as pasteurization of milk, safe canning, and disinfection of water supplies have conquered those diseases. Today other foodborne infections have taken their place, including some that have only recently been discovered. For example, in 1996, the parasite Cyclospora suddenly appeared as a cause of diarrheal illness related to Guatemalan raspberries. These berries had just started to be grown commercially in Guatemala, and somehow became contaminated in the field there with this unusual parasite. In 1998, a new strain of the bacterium Vibrio parahemolyticus contaminated oyster beds in Galveston Bay and caused an epidemic of diarrheal illness in persons eating the oysters raw. The affected oyster beds were near the shipping lanes, which suggested that the bacterium arrived in the ballast water of freighters and tankers coming into the harbor from distant ports. Newly recognized microbes emerge as public health problems for several reasons: microbes can easily spread around the world, new microbes can evolve, the environment and ecology are changing, food production practices and consumption habits change, and because better laboratory tests can now identify microbes that were previously unrecognized.
In the last 15 years, several important diseases of unknown cause have turned out to be complications of foodborne infections. For example, we now know that the Guillain-Barre syndrome can be caused by Campylobacter infection, and that the most common cause of acute kidney failure in children, hemolytic uremic syndrome, is caused by infection with E. coli O157:H7 and related bacteria. In the future, other diseases whose origins are currently unknown may turn out be related to foodborne infections.
What happens in the body after the microbes that produce illness are swallowed?
After they are swallowed, there is a delay, called the incubation period, before the symptoms of illness begin. This delay may range from hours to days, depending on the organism, and on how many of them were swallowed. During the incubation period, the microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade the deeper body tissues. The symptoms produced depend greatly on the type of microbe. Numerous organisms cause similar symptoms, especially diarrhea, abdominal cramps, and nausea. There is so much overlap that it is rarely possible to say which microbe is likely to be causing a given illness unless laboratory tests are done to identify the microbe, or unless the illness is part of a recognized outbreak.
How are foodborne diseases diagnosed?
The infection is usually diagnosed by specific laboratory tests that identify the causative organism. Bacteria such as Campylobacter, Salmonella, E. coli O157 are found by culturing stool samples in the laboratory and identifying the bacteria that grow on the agar or other culture medium. Parasites can be identified by examining stools under the microscope. Viruses are more difficult to identify, as they are too small to see under a light microscope and are difficult to culture. Viruses are usually identified by testing stool samples for genetic markers that indicate a specific virus is present.
Many foodborne infections are not identified by routine laboratory procedures and require specialized, experimental, and/or expensive tests that are not generally available. If the diagnosis is to be made, the patient has to seek medical attention, the physician must decide to order diagnostic tests, and the laboratory must use the appropriate procedures. Because many ill persons to not seek attention, and of those that do, many are not tested, many cases of foodborne illness go undiagnosed. For example, CDC estimates that 38 cases of salmonellosis actually occur for every case that is actually diagnosed and reported to public health authorities.
How are foodborne diseases treated?
There are many different kinds of foodborne diseases and they may require different treatments, depending on the symptoms they cause. Illnesses that are primarily diarrhea or vomiting can lead to dehydration if the person loses more body fluids and salts (electrolytes) than they take in. Replacing the lost fluids and electrolytes and keeping up with fluid intake are important. If diarrhea is severe, oral rehydration solution such as Ceralyte*, Pedialyte* or Oralyte*, should be drunk to replace the fluid losses and prevent dehydration. Sports drinks such as Gatorade* do not replace the losses correctly and should not be used for the treatment of diarrheal illness. Preparations of bismuth subsalicylate (e.g., Pepto-Bismol)* can reduce the duration and severity of simple diarrhea. If diarrhea and cramps occur, without bloody stools or fever, taking an antidiarrheal medication may provide symptomatic relief, but these medications should be avoided if there is high fever or blood in the stools because they may make the illness worse.
*CDC does not endorse commercial products or services.
When should I consult my doctor about a diarrheal illness?
A health care provider should be consulted for a diarrheal illness is accompanied by
high fever (temperature over 101.5 F, measured orally) blood in the stools prolonged vomiting that prevents keeping liquids down (which can lead to dehydration) signs of dehydration, including a decrease in urination, a dry mouth and throat, and feeling dizzy when standing up. diarrheal illness that lasts more than 3 days Do not be surprised if your doctor does not prescribe an antibiotic. Many diarrheal illnesses are caused by viruses and will improve in 2 or 3 days without antibiotic therapy. In fact, antibiotics have no effect on viruses, and using an antibiotic to treat a viral infection could cause more harm than good It is often not necessary to take an antibiotic even in the case of a mild bacterial infection. Other treatments can help the symptoms, and careful handwashing can prevent the spread of infection to other people. Overuse of antibiotics is the principal reason many bacteria are becoming resistant. Resistant bacteria are no longer killed by the antibiotic. This means that it is important to use antibiotics only when they are really needed. Partial treatment can also cause bacteria to become resistant. If an antibiotic is prescribed, it is important to take all of the medication as prescribed, and not stop early just because the symptoms seem to be improving.
How many cases of foodborne disease are there in the United States?
CDC estimates that that each year roughly 1 out of 6 Americans (or 48 million people) gets sick, 128,000 are hospitalized, and 3,000 die from foodborne diseases. The great majority of these cases are mild and cause symptoms for only a day or two. The most severe cases tend to occur in the very old, the very young, those who have an illness already that reduces their immune system function, and in healthy people exposed to a very high dose of an organism.
How do public health departments track foodborne diseases?
Routine monitoring of important diseases by public health departments is called disease surveillance. Each state decides which diseases are to be under surveillance in that state. In most states, diagnosed cases of salmonellosis, E. coli O157:H7 and other serious infections are routinely reported to the health department. The county reports them to the state health department, which reports them to CDC. Tens of thousands of cases of these "notifiable conditions" are reported every year. For example, nearly 35,000 cases of Salmonella infection were reported to CDC in 1998. However, most foodborne infections go undiagnosed and unreported, either because the ill person does not see a doctor, or the doctor does not make a specific diagnosis. Also, infections with some microbes are not reportable in the first place.
To get more information about infections that might be diagnosed but not reported, CDC developed a special surveillance system called FoodNet. FoodNet provides the best available information about specific foodborne infections in the United States, and summarizes them in an annual report.
In addition to tracking the number of reported cases of individual infections, states also collect information about foodborne outbreaks, and report a summary of that information to CDC. About 400-500 foodborne outbreaks investigated by local and state health departments are reported each year. This includes information about many diseases that are not notifiable and thus are not under individual surveillance, so it provides some useful general information about foodborne diseases.
What are foodborne disease outbreaks and why do they occur?
An outbreak of foodborne illness occurs when a group of people consume the same contaminated food and two or more of them come down with the same illness. It may be a group that ate a meal together somewhere, or it may be a group of people who do not know each other at all, but who all happened to buy and eat the same contaminated item from a grocery store or restaurant. For an outbreak to occur, something must have happened to contaminate a batch of food that was eaten by a the group of people. Often, a combination of events contributes to the outbreak. A contaminated food may be left out a room temperature for many hours, allowing the bacteria to multiply to high numbers, and then be insufficiently cooked to kill the bacteria.
Many outbreaks are local in nature. They are recognized when a group of people realize that they all became ill after a common meal, and someone calls the local health department. This classic local outbreak might follow a catered meal at a reception, a pot-luck supper, or eating a meal at an understaffed restaurant on a particularly busy day. However, outbreaks are increasingly being recognized that are more widespread, that affect persons in many different places, and that are spread out over several weeks. For example, a recent outbreak of salmonellosis was traced to persons eating a breakfast cereal produced at a factory in Minnesota, and marketed under several different brand names in many different states. No one county or state had very many cases and the cases did not know each other. The outbreaks was recognized because it was caused by an unusual strain of Salmonella, and because state public health laboratories that type Salmonella strains noticed a sudden increase in this one rare strain. In another recent outbreak, a particular peanut snack food caused the same illness in Israel, Europe and North America. Again, this was recognized as an increase in infections caused by a rare strain of Salmonella.
The vast majority of reported cases of foodborne illness are not part of recognized outbreaks, but occurs as individual or "sporadic" cases. It may be that many of these cases are actually part of unrecognized widespread or diffuse outbreaks. Detecting and investigating such widespread outbreaks is a major challenge to our public health system. This is the reason that new and more sophisticated laboratory methods are being used at CDC and in state public health department laboratories.
Why do public health officials investigate outbreaks?
A foodborne outbreak is an indication that something needs to be improved in our food safety system. Public health scientists investigate outbreaks to control them, and also to learn how similar outbreaks can be prevented in the future. Just as when a fire breaks out in a large building or when an airliner crashes, two activities are critical when an outbreak occurs. First, emergency action is needed to keep the immediate danger from spreading, and second, a detailed objective scientific investigation is needed to learn what went wrong, so that future similar events can be prevented. Much of what we know about foodborne disease and its prevention comes from detailed investigation of outbreaks. This is often how a new pathogen is identified, and this is how the critical information linking a pathogen to a specific food and animal reservoir is first gathered. The full investigation can require a team with multiple talents, including the epidemiologist, microbiologist, food sanitarian, food scientist, veterinarian, and factory process engineer.
How are outbreaks of foodborne disease detected?
The initial clue that an outbreak is occurring can come in various ways. It may be when a person realizes that several other people who were all together at an event have become ill and he or she calls the local health department. It may be when a physician realizes she has seen more than the usual number of patients with the same illness. It may be when a county health department gets an unusually large number of reports of illness. The hardest outbreaks to detect are those that are spread over a large geographic area, with only a few cases in each state. These outbreaks can be detected by combining surveillance reports at the regional or national level and looking for increases in infections of a specific type. This is why state public health laboratories determine the serotype of Salmonella bacteria isolated from people. New "DNA fingerprinting" technologies can make detecting outbreaks easier too. For example, the new molecular subtyping network, PulseNet, allows state laboratories and CDC to compare strains of E. coli O157:H7 and an increasing number of other pathogens from all across the United States to detect widespread outbreaks.
After an apparent cluster of cases is detected, it is important to determine whether these cases represent a real increase above the expected number of cases and whether they really might be related. Sometimes a cluster of reported cases is caused by something other than an actual outbreak of illness. For example, if the person responsible for reporting has just returned from a vacation and is clearing up a backlog of cases by reporting them all at once, the sudden surge of reports is just a false cluster.
How is a foodborne disease outbreak investigated?
Once an outbreak is strongly suspected, an investigation begins. A search is made for more cases among persons who may have been exposed. The symptoms and time of onset, and location of possible cases is determined, and a "case definition" is developed that describes these typical cases. The outbreak is systematically described by time, place, and person. A graph is drawn of the number of people who fell ill on each successive day to show pictorially when it occurred. A map of where the ill people live, work, or eat may be helpful to show where it occurred. Calculating the distribution of cases by age and sex shows who is affected. If the causative microbe is not known, samples of stool or blood are collected from ill people and sent to the public health laboratory to make the diagnosis.
To identify the food or other source of the outbreak, the investigators first interview a few persons with the most typical cases about exposures they may have had in the few days before they got sick. In this way, certain potential exposures may be excluded while others that are mentioned repeatedly emerge as possibilities. Combined with other information, such as the likely sources for the specific microbe involved, these hypotheses are then tested in a formal epidemiologic investigation. The investigators conduct systematic interviews about a list of possible exposures with the ill persons, and with a comparable group people who are not ill. By comparing how often an exposure is reported by ill people and by well people, investigators can measure the association of the exposure with illness. Using probability statistics, similar to those used to describe coin flips, the probability of no association is directly calculated.
For example, imagine that an outbreak has occurred after a catered event. Initial investigation suggested that Hollandaise sauce was eaten by at least some of the attendees, so it is on the list of possible hypotheses. Now, we interview 20 persons who attended the affair, 10 of whom became ill and 10 who remained well. Each ill or well person is interviewed about whether or not they ate the Hollandaise sauce, as well as various other food items. If half the people ate the sauce, but the sauce was not associated with the illness, then we would expect each person to have a 50/50 chance of reporting that they ate it, regardless of whether they were ill or not. Suppose, however, that we find that all 10 ill people but none of the well persons reported eating Hollandaise sauce at the event? This would be very unlikely to occur by chance alone if eating the Hollandaise sauce were not somehow related to the risk of illness. In fact, it would be about as unlikely as getting heads ten times in a row by flipping a coin (That is 50% multiplied by itself 10 times over, or a chance of just under 1 in 1000). So the epidemiologist concludes that eating the Hollandaise sauce was very likely to be associated with the risk of illness. Note that the investigator can draw this conclusion even though there is no Hollandaise sauce left to test in a laboratory. The association is even stronger if she can show that those who ate second helpings of Hollandaise were even more likely to become ill, or that persons who ate leftover Hollandaise sauce that went home in doggie bags also became ill.
Once a food item is statistically implicated in this manner, further investigation into its ingredients and preparation, and microbiologic culture of leftover ingredients or the food itself (if available) may provide additional information about the nature of contamination. Perhaps the Hollandaise sauce was made using raw eggs. The source of the raw eggs can be determined, and it may even be possible to trace them back to the farm and show that chickens on the farm are carrying the same strain of Salmonella in their ovaries. If so, the eggs from that farm can be pasteurized to prevent them from causing other outbreaks.
Some might think that the best investigation method would be just to culture all the leftover foods in the kitchen, and conclude that the one that is positive is the one that caused the outbreak. The trouble is that this can be misleading, because it happens after the fact. What if the Hollandaise sauce is all gone, but the spoon that was in the sauce got placed in potato salad that was not served at the function? Now, cultures of the potato salad yield a pathogen, and the unwary tester might call that the source of the outbreak, even though the potato salad had nothing to do with it. This means that laboratory testing without epidemiologic investigation can lead to the wrong conclusion.
Even without isolating microbes from food, a well-conducted epidemiologic investigation can guide immediate efforts to control the outbreak. A strong and consistent statistical association between illness and a particular food item that explains the distribution of the outbreak in time, place and person should be acted upon immediately to stop further illness from occurring.
An outbreak ends when the critical exposure stops. This may happen because all the contaminated food is eaten or recalled, because a restaurant is closed or a food processor shuts down or changes its procedures, or an infected food handler is no longer infectious or is no longer working with food. An investigation that clarifies the nature and mechanism of contamination can provide critical information even if the outbreak is over. Understanding the contamination event well enough to prevent it can guide the decision to resume usual operations, and lead to more general prevention measures that reduce the risk of similar outbreaks happening elsewhere.
How does food become contaminated?
We live in a microbial world, and there are many opportunities for food to become contaminated as it is produced and prepared. Many foodborne microbes are present in healthy animals (usually in their intestines) raised for food. Meat and poultry carcasses can become contaminated during slaughter by contact with small amounts of intestinal contents. Similarly, fresh fruits and vegetables can be contaminated if they are washed or irrigated with water that is contaminated with animal manure or human sewage. Some types of Salmonella can infect a hen's ovary so that the internal contents of a normal looking egg can be contaminated with Salmonella even before the shell in formed. Oysters and other filter feeding shellfish can concentrate Vibrio bacteria that are naturally present in sea water, or other microbes that are present in human sewage dumped into the sea.
Later in food processing, other foodborne microbes can be introduced from infected humans who handle the food, or by cross contamination from some other raw agricultural product. For example, Shigella bacteria, hepatitis A virus and Norwalk virus can be introduced by the unwashed hands of food handlers who are themselves infected. In the kitchen, microbes can be transferred from one food to another food by using the same knife, cutting board or other utensil to prepare both without washing the surface or utensil in between. A food that is fully cooked can become recontaminated if it touches other raw foods or drippings from raw foods that contain pathogens.
The way that food is handled after it is contaminated can also make a difference in whether or not an outbreak occurs. Many bacterial microbes need to multiply to a larger number before enough are present in food to cause disease. Given warm moist conditions and an ample supply of nutrients, one bacterium that reproduces by dividing itself every half hour can produce 17 million progeny in 12 hours. As a result, lightly contaminated food left out overnight can be highly infectious by the next day. If the food were refrigerated promptly, the bacteria would not multiply at all. In general, refrigeration or freezing prevents virtually all bacteria from growing but generally preserves them in a state of suspended animation. This general rule has a few surprising exceptions. Two foodborne bacteria, Listeria monocytogenes and Yersinia enterocolitica can actually grow at refrigerator temperatures. High salt, high sugar or high acid levels keep bacteria from growing, which is why salted meats, jam, and pickled vegetables are traditional preserved foods.
Microbes are killed by heat. If food is heated to an internal temperature above 160oF, or 78oC, for even a few seconds this sufficient to kill parasites, viruses or bacteria, except for the Clostridium bacteria, which produce a heat-resistant form called a spore. Clostridium spores are killed only at temperatures above boiling. This is why canned foods must be cooked to a high temperature under pressure as part of the canning process.
The toxins produced by bacteria vary in their sensitivity to heat. The staphylococcal toxin which causes vomiting is not inactivated even if it is boiled. Fortunately, the potent toxin that causes botulism is completely inactivated by boiling.
What foods are most associated with foodborne illness?
Raw foods of animal origin are the most likely to be contaminated; that is, raw meat and poultry, raw eggs, unpasteurized milk, and raw shellfish. Because filter-feeding shellfish strain microbes from the sea over many months, they are particularly likely to be contaminated if there are any pathogens in the seawater. Foods that mingle the products of many individual animals, such as bulk raw milk, pooled raw eggs, or ground beef, are particularly hazardous because a pathogen present in any one of the animals may contaminate the whole batch. A single hamburger may contain meat from hundreds of animals. A single restaurant omelet may contain eggs from hundreds of chickens. A glass of raw milk may contain milk from hundreds of cows. A broiler chicken carcass can be exposed to the drippings and juices of many thousands of other birds that went through the same cold water tank after slaughter.
Fruits and vegetables consumed raw are a particular concern. Washing can decrease but not eliminate contamination, so the consumers can do little to protect themselves. Recently, a number of outbreak have been traced to fresh fruits and vegetables that were processed under less than sanitary conditions. These outbreaks show that the quality of the water used for washing and chilling the produce after it is harvested is critical. Using water that is not clean can contaminate many boxes of produce. Fresh manure used to fertilize vegetables can also contaminate them. Alfalfa sprouts and other raw sprouts pose a particular challenge, as the conditions under which they are sprouted are ideal for growing microbes as well as sprouts, and because they are eaten without further cooking. That means that a few bacteria present on the seeds can grow to high numbers of pathogens on the sprouts. Unpasteurized fruit juice can also be contaminated if there are pathogens in or on the fruit that is used to make it.
What can consumers do to protect themselves from foodborne illness?
A few simple precautions can reduce the risk of foodborne diseases:
COOK meat, poultry and eggs thoroughly. Using a thermometer to measure the internal temperature of meat is a good way to be sure that it is cooked sufficiently to kill bacteria. For example, ground beef should be cooked to an internal temperature of 160o F. Eggs should be cooked until the yolk is firm.
SEPARATE: Don't cross-contaminate one food with another. Avoid cross-contaminating foods by washing hands, utensils, and cutting boards after they have been in contact with raw meat or poultry and before they touch another food. Put cooked meat on a clean platter, rather back on one that held the raw meat.
CHILL: Refrigerate leftovers promptly. Bacteria can grow quickly at room temperature, so refrigerate leftover foods if they are not going to be eaten within 4 hours. Large volumes of food will cool more quickly if they are divided into several shallow containers for refrigeration.
CLEAN: Wash produce. Rinse fresh fruits and vegetables in running tap water to remove visible dirt and grime. Remove and discard the outermost leaves of a head of lettuce or cabbage. Because bacteria can grow well on the cut surface of fruit or vegetable, be careful not to contaminate these foods while slicing them up on the cutting board, and avoid leaving cut produce at room temperature for many hours. Don't be a source of foodborne illness yourself. Wash your hands with soap and water before preparing food. Avoid preparing food for others if you yourself have a diarrheal illness. Changing a baby's diaper while preparing food is a bad idea that can easily spread illness.
REPORT: Report suspected foodborne illnesses to your local health department. The local public health department is an important part of the food safety system. Often calls from concerned citizens are how outbreaks are first detected. If a public health official contacts you to find our more about an illness you had, your cooperation is important. In public health investigations, it can be as important to talk to healthy people as to ill people. Your cooperation may be needed even if you are not ill.
Are some people more likely to contract a foodborne illness? If so, are there special precautions they should take?
Some persons at particularly high risk should take more precautions.
What can consumers do when they eat in restaurants?
You can protect yourself first by choosing which restaurant to patronize. Restaurants are inspected by the local health department to make sure they are clean and have adequate kitchen facilities. Find out how restaurants did on their most recent inspections, and use that score to help guide your choice. In many jurisdictions, the latest inspection score is posted in the restaurant. Some restaurants have specifically trained their staff in principles of food safety. This is also good to know in deciding which restaurant to patronize.
You can also protect yourself from foodborne disease when ordering specific foods, just as you would at home. When ordering a hamburger, ask for it to be cooked to a temperature of 160oF and send it back if it is still pink in the middle. Before you order something that is made with many eggs pooled together, such as scrambled eggs, omelets or French toast, ask the waiter whether it was made with pasteurized egg, and choose something else if it was not.
There is only so much the consumer can do. How can food be made safer in the first place?
Making food safe in the first place is a major effort, involving the farm and fishery, the production plant or factory, and many other points from the farm to the table. Many different groups in public health, industry, regulatory agencies, and academia have roles to play in making the food supply less contaminated. Consumers can promote general food safety with their dollars, by purchasing foods that have been processed for safety. For example, milk pasteurization was a major advance in food safety that was developed 100 years ago. Buying pasteurized milk rather than raw unpasteurized milk still prevents an enormous number of foodborne diseases every day. Now juice pasteurization is a recent important step forward that prevents E. coli O157:H7 infections and many other diseases. Consumers can look for and buy pasteurized fruit juices and ciders. In the future, meat and other foods will be available that has been treated for safety with irradiation. These new technologies are likely to be as important a step forward as the pasteurization of milk.
Foodborne diseases are largely preventable, though there is no simple one-step prevention measure like a vaccine. Instead, measures are needed to prevent or limit contamination all the way from farm to table. A variety of good agricultural and manufacturing practices can reduce the spread of microbes among animals and prevent the contamination of foods. Careful review of the whole food production process can identify the principal hazards, and the control points where contamination can be prevented, limited, or eliminated. A formal method for evaluating the control of risk in foods exists is called the Hazard Analysis Critical Control Point, or HACCP system. This was first developed by NASA to make sure that the food eaten by astronauts was safe. HACCP safety principles are now being applied to an increasing spectrum of foods, including meat, poultry, and seafood.
For some particularly risky foods, even the most careful hygiene and sanitation are insufficient to prevent contamination, and a definitive microbe-killing step must be included in the process. For example, early in the century, large botulism outbreaks occurred when canned foods were cooked insufficiently to kill the botulism spores. After research was done to find out exactly how much heat was needed to kill the spores, the canning industry and the government regulators went to great lengths to be sure every can was sufficiently cooked. As a result, botulism related to commercial canned foods has disappeared in this country. Similarly the introduction of careful pasteurization of milk eliminated a large number of milk-borne diseases. This occurred after sanitation in dairies had already reached a high level. In the future, other foods can be made much safer by new pasteurizing technologies, such as in-shell pasteurization of eggs, and irradiation of ground beef. Just as with milk, these new technologies should be implemented in addition to good sanitation, not as a replacement for it.
In the end, it is up to the consumer to demand a safe food supply; up to industry to produce it; up to researchers to develop better ways of doing so; and up to government to see that it happens, to make sure it works and to identify problems still in need of solutions.
What is CDC doing to control and prevent foodborne disease?
CDC is part of the U. S. Public Health Service, with a mission to use the best scientific information to monitor, investigate, control and prevent public health problems. Using the tools of epidemiology and laboratory science, CDC provides scientific assessment of public health threats. CDC works closely with state health departments to monitor the frequency of specific diseases and conducts national surveillance for them. CDC provides expert epidemiologic and microbiologic consultation to health departments and other federal agencies on a variety of public health issues, including foodborne disease, and it stations epidemiologists in state health departments to help with the surveillance and investigation of many problems. CDC can also send a team into the field to conduct emergency field investigations of large or unusual outbreaks, in collaboration with state public health officials. CDC researchers develop new methods for identifying, characterizing and fingerprinting the microbes that cause disease. We translate laboratory research into practical field methods that can be used by public health authorities in States and counties.
CDC is not a regulatory agency. Government regulation of food safety is carried out by the Food and Drug Administration (FDA) , the U.S. Department of Agriculture (USDA), the National Marine Fisheries Service, and other regulatory agencies. CDC maintains regular contact with the regulatory agencies.
When new public health threats appear, CDC learns what they are and how they can be controlled through rapid scientific field and laboratory investigation. CDC shares the results of these investigations with the states, with the regulatory federal agencies and with the industries themselves. Although we do not regulate the safety of food, CDC assesses the effectiveness of current prevention efforts. We provide independent scientific assessment of what the problems are, how they can be controlled, and of where there are gaps in our knowledge.
What are some unsolved problems in foodborne disease?
As new foodborne problems emerge, several questions need to be answered before the problem can be successfully controlled. It takes careful scientific observation and research to answer these questions. Some pressing unanswered questions include:
How do the foodborne pathogens spread among the animals themselves, and how can this be prevented? This includes E. coli O157:H7 among cattle, Salmonella Enteritis among egg-laying hens, and Campylobacter in broiler chickens. If we could prevent the animals from becoming infected in the first place, we would not have as much illness in the humans who eat them. What is the microbial cause of outbreaks in which no pathogen can be identified by current methods? This is true for over half of the reported foodborne outbreaks. Will wider application of existing experimental diagnostic methods help, or are these outbreaks caused by pathogens we simply do not yet know how to identify? What would be the impact of basic food safety education of restaurant workers on the risk of foodborne disease among restaurant patrons? How can the food and water that animals consume be made safer? How can we dispose of animal manure usefully, without threatening the food supply and the environment? How can basic food safety principles be most effectively taught to school children? How can we be sure food safety standards in other countries are as good as those in the United States? As we import more of our fresh foods from other countries, we need to be confident that they are produced with the same level of safety as food in the United States. What control strategies in the slaughter plant will reduce the contamination of poultry meat with Campylobacter? How can irradiation pasteurization of certain high risk foods, such as ground beef, be used most effectively? How do raspberries in Central America get contaminated with Cyclospora in the first place? Does this parasite have an animal reservoir? How can alfalfa sprouts and other raw sprouts be produced safely? Sprouts are unique among foods in that the conditions for sprouting are also perfect for bacterial growth, and they are not cooked after that.
Foodborne disease is caused by consuming contaminated foods or beverages. Many different disease-causing microbes, or pathogens, can contaminate foods, so there are many different foodborne infections. In addition, poisonous chemicals, or other harmful substances can cause foodborne diseases if they are present in food.
More than 250 different foodborne diseases have been described. Most of these diseases are infections, caused by a variety of bacteria, viruses, and parasites that can be foodborne. Other diseases are poisonings, caused by harmful toxins or chemicals that have contaminated the food, for example, poisonous mushrooms. These different diseases have many different symptoms, so there is no one "syndrome" that is foodborne illness. However, the microbe or toxin enters the body through the gastrointestinal tract, and often causes the first symptoms there, so nausea, vomiting, abdominal cramps and diarrhea are common symptoms in many foodborne diseases.
Many microbes can spread in more than one way, so we cannot always know that a disease is foodborne. The distinction matters, because public health authorities need to know how a particular disease is spreading to take the appropriate steps to stop it. For example, Escherichia coli O157:H7 infections can spread through contaminated food, contaminated drinking water, contaminated swimming water, and from toddler to toddler at a day care center. Depending on which means of spread caused a case, the measures to stop other cases from occurring could range from removing contaminated food from stores, chlorinating a swimming pool, or closing a child day care center.
What are the most common foodborne diseases?
The most commonly recognized foodborne infections are those caused by the bacteria Campylobacter, Salmonella, and E. coli O157:H7, and by a group of viruses called calicivirus, also known as the Norwalk and Norwalk-like viruses.
Campylobacter is a bacterial pathogen that causes fever, diarrhea, and abdominal cramps. It is the most commonly identified bacterial cause of diarrheal illness in the world. These bacteria live in the intestines of healthy birds, and most raw poultry meat has Campylobacter on it. Eating undercooked chicken, or other food that has been contaminated with juices dripping from raw chicken is the most frequent source of this infection.
Salmonella is also a bacterium that is widespread in the intestines of birds, reptiles and mammals. It can spread to humans via a variety of different foods of animal origin. The illness it causes, salmonellosis, typically includes fever, diarrhea and abdominal cramps. In persons with poor underlying health or weakened immune systems, it can invade the bloodstream and cause life-threatening infections.
E. coli O157:H7 is a bacterial pathogen that has a reservoir in cattle and other similar animals. Human illness typically follows consumption of food or water that has been contaminated with microscopic amounts of cow feces. The illness it causes is often a severe and bloody diarrhea and painful abdominal cramps, without much fever. In 3% to 5% of cases, a complication called hemolytic uremic syndrome (HUS) can occur several weeks after the initial symptoms. This severe complication includes temporary anemia, profuse bleeding, and kidney failure.
Calicivirus, or Norwalk-like virus is an extremely common cause of foodborne illness, though it is rarely diagnosed, because the laboratory test is not widely available. It causes an acute gastrointestinal illness, usually with more vomiting than diarrhea, that resolves within two days. Unlike many foodborne pathogens that have animal reservoirs, it is believed that Norwalk-like viruses spread primarily from one infected person to another. Infected kitchen workers can contaminate a salad or sandwich as they prepare it, if they have the virus on their hands. Infected fishermen have contaminated oysters as they harvested them.
Some common diseases are occasionally foodborne, even though they are usually transmitted by other routes. These include infections caused by Shigella, hepatitis A, and the parasites Giardia lamblia and Cryptosporidia. Even strep throats have been transmitted occasionally through food.
In addition to disease caused by direct infection, some foodborne diseases are caused by the presence of a toxin in the food that was produced by a microbe in the food. For example, the bacterium Staphylococcus aureus can grow in some foods and produce a toxin that causes intense vomiting. The rare but deadly disease botulism occurs when the bacterium Clostridium botulinum grows and produces a powerful paralytic toxin in foods. These toxins can produce illness even if the microbes that produced them are no longer there.
Other toxins and poisonous chemicals can cause foodborne illness. People can become ill if a pesticide is inadvertently added to a food, or if naturally poisonous substances are used to prepare a meal. Every year, people become ill after mistaking poisonous mushrooms for safe species, or after eating poisonous reef fishes.
Are the types of foodborne diseases changing?
The spectrum of foodborne diseases is constantly changing. A century ago, typhoid fever, tuberculosis and cholera were common foodborne diseases. Improvements in food safety, such as pasteurization of milk, safe canning, and disinfection of water supplies have conquered those diseases. Today other foodborne infections have taken their place, including some that have only recently been discovered. For example, in 1996, the parasite Cyclospora suddenly appeared as a cause of diarrheal illness related to Guatemalan raspberries. These berries had just started to be grown commercially in Guatemala, and somehow became contaminated in the field there with this unusual parasite. In 1998, a new strain of the bacterium Vibrio parahemolyticus contaminated oyster beds in Galveston Bay and caused an epidemic of diarrheal illness in persons eating the oysters raw. The affected oyster beds were near the shipping lanes, which suggested that the bacterium arrived in the ballast water of freighters and tankers coming into the harbor from distant ports. Newly recognized microbes emerge as public health problems for several reasons: microbes can easily spread around the world, new microbes can evolve, the environment and ecology are changing, food production practices and consumption habits change, and because better laboratory tests can now identify microbes that were previously unrecognized.
In the last 15 years, several important diseases of unknown cause have turned out to be complications of foodborne infections. For example, we now know that the Guillain-Barre syndrome can be caused by Campylobacter infection, and that the most common cause of acute kidney failure in children, hemolytic uremic syndrome, is caused by infection with E. coli O157:H7 and related bacteria. In the future, other diseases whose origins are currently unknown may turn out be related to foodborne infections.
What happens in the body after the microbes that produce illness are swallowed?
After they are swallowed, there is a delay, called the incubation period, before the symptoms of illness begin. This delay may range from hours to days, depending on the organism, and on how many of them were swallowed. During the incubation period, the microbes pass through the stomach into the intestine, attach to the cells lining the intestinal walls, and begin to multiply there. Some types of microbes stay in the intestine, some produce a toxin that is absorbed into the bloodstream, and some can directly invade the deeper body tissues. The symptoms produced depend greatly on the type of microbe. Numerous organisms cause similar symptoms, especially diarrhea, abdominal cramps, and nausea. There is so much overlap that it is rarely possible to say which microbe is likely to be causing a given illness unless laboratory tests are done to identify the microbe, or unless the illness is part of a recognized outbreak.
How are foodborne diseases diagnosed?
The infection is usually diagnosed by specific laboratory tests that identify the causative organism. Bacteria such as Campylobacter, Salmonella, E. coli O157 are found by culturing stool samples in the laboratory and identifying the bacteria that grow on the agar or other culture medium. Parasites can be identified by examining stools under the microscope. Viruses are more difficult to identify, as they are too small to see under a light microscope and are difficult to culture. Viruses are usually identified by testing stool samples for genetic markers that indicate a specific virus is present.
Many foodborne infections are not identified by routine laboratory procedures and require specialized, experimental, and/or expensive tests that are not generally available. If the diagnosis is to be made, the patient has to seek medical attention, the physician must decide to order diagnostic tests, and the laboratory must use the appropriate procedures. Because many ill persons to not seek attention, and of those that do, many are not tested, many cases of foodborne illness go undiagnosed. For example, CDC estimates that 38 cases of salmonellosis actually occur for every case that is actually diagnosed and reported to public health authorities.
How are foodborne diseases treated?
There are many different kinds of foodborne diseases and they may require different treatments, depending on the symptoms they cause. Illnesses that are primarily diarrhea or vomiting can lead to dehydration if the person loses more body fluids and salts (electrolytes) than they take in. Replacing the lost fluids and electrolytes and keeping up with fluid intake are important. If diarrhea is severe, oral rehydration solution such as Ceralyte*, Pedialyte* or Oralyte*, should be drunk to replace the fluid losses and prevent dehydration. Sports drinks such as Gatorade* do not replace the losses correctly and should not be used for the treatment of diarrheal illness. Preparations of bismuth subsalicylate (e.g., Pepto-Bismol)* can reduce the duration and severity of simple diarrhea. If diarrhea and cramps occur, without bloody stools or fever, taking an antidiarrheal medication may provide symptomatic relief, but these medications should be avoided if there is high fever or blood in the stools because they may make the illness worse.
*CDC does not endorse commercial products or services.
When should I consult my doctor about a diarrheal illness?
A health care provider should be consulted for a diarrheal illness is accompanied by
high fever (temperature over 101.5 F, measured orally) blood in the stools prolonged vomiting that prevents keeping liquids down (which can lead to dehydration) signs of dehydration, including a decrease in urination, a dry mouth and throat, and feeling dizzy when standing up. diarrheal illness that lasts more than 3 days Do not be surprised if your doctor does not prescribe an antibiotic. Many diarrheal illnesses are caused by viruses and will improve in 2 or 3 days without antibiotic therapy. In fact, antibiotics have no effect on viruses, and using an antibiotic to treat a viral infection could cause more harm than good It is often not necessary to take an antibiotic even in the case of a mild bacterial infection. Other treatments can help the symptoms, and careful handwashing can prevent the spread of infection to other people. Overuse of antibiotics is the principal reason many bacteria are becoming resistant. Resistant bacteria are no longer killed by the antibiotic. This means that it is important to use antibiotics only when they are really needed. Partial treatment can also cause bacteria to become resistant. If an antibiotic is prescribed, it is important to take all of the medication as prescribed, and not stop early just because the symptoms seem to be improving.
How many cases of foodborne disease are there in the United States?
CDC estimates that that each year roughly 1 out of 6 Americans (or 48 million people) gets sick, 128,000 are hospitalized, and 3,000 die from foodborne diseases. The great majority of these cases are mild and cause symptoms for only a day or two. The most severe cases tend to occur in the very old, the very young, those who have an illness already that reduces their immune system function, and in healthy people exposed to a very high dose of an organism.
How do public health departments track foodborne diseases?
Routine monitoring of important diseases by public health departments is called disease surveillance. Each state decides which diseases are to be under surveillance in that state. In most states, diagnosed cases of salmonellosis, E. coli O157:H7 and other serious infections are routinely reported to the health department. The county reports them to the state health department, which reports them to CDC. Tens of thousands of cases of these "notifiable conditions" are reported every year. For example, nearly 35,000 cases of Salmonella infection were reported to CDC in 1998. However, most foodborne infections go undiagnosed and unreported, either because the ill person does not see a doctor, or the doctor does not make a specific diagnosis. Also, infections with some microbes are not reportable in the first place.
To get more information about infections that might be diagnosed but not reported, CDC developed a special surveillance system called FoodNet. FoodNet provides the best available information about specific foodborne infections in the United States, and summarizes them in an annual report.
In addition to tracking the number of reported cases of individual infections, states also collect information about foodborne outbreaks, and report a summary of that information to CDC. About 400-500 foodborne outbreaks investigated by local and state health departments are reported each year. This includes information about many diseases that are not notifiable and thus are not under individual surveillance, so it provides some useful general information about foodborne diseases.
What are foodborne disease outbreaks and why do they occur?
An outbreak of foodborne illness occurs when a group of people consume the same contaminated food and two or more of them come down with the same illness. It may be a group that ate a meal together somewhere, or it may be a group of people who do not know each other at all, but who all happened to buy and eat the same contaminated item from a grocery store or restaurant. For an outbreak to occur, something must have happened to contaminate a batch of food that was eaten by a the group of people. Often, a combination of events contributes to the outbreak. A contaminated food may be left out a room temperature for many hours, allowing the bacteria to multiply to high numbers, and then be insufficiently cooked to kill the bacteria.
Many outbreaks are local in nature. They are recognized when a group of people realize that they all became ill after a common meal, and someone calls the local health department. This classic local outbreak might follow a catered meal at a reception, a pot-luck supper, or eating a meal at an understaffed restaurant on a particularly busy day. However, outbreaks are increasingly being recognized that are more widespread, that affect persons in many different places, and that are spread out over several weeks. For example, a recent outbreak of salmonellosis was traced to persons eating a breakfast cereal produced at a factory in Minnesota, and marketed under several different brand names in many different states. No one county or state had very many cases and the cases did not know each other. The outbreaks was recognized because it was caused by an unusual strain of Salmonella, and because state public health laboratories that type Salmonella strains noticed a sudden increase in this one rare strain. In another recent outbreak, a particular peanut snack food caused the same illness in Israel, Europe and North America. Again, this was recognized as an increase in infections caused by a rare strain of Salmonella.
The vast majority of reported cases of foodborne illness are not part of recognized outbreaks, but occurs as individual or "sporadic" cases. It may be that many of these cases are actually part of unrecognized widespread or diffuse outbreaks. Detecting and investigating such widespread outbreaks is a major challenge to our public health system. This is the reason that new and more sophisticated laboratory methods are being used at CDC and in state public health department laboratories.
Why do public health officials investigate outbreaks?
A foodborne outbreak is an indication that something needs to be improved in our food safety system. Public health scientists investigate outbreaks to control them, and also to learn how similar outbreaks can be prevented in the future. Just as when a fire breaks out in a large building or when an airliner crashes, two activities are critical when an outbreak occurs. First, emergency action is needed to keep the immediate danger from spreading, and second, a detailed objective scientific investigation is needed to learn what went wrong, so that future similar events can be prevented. Much of what we know about foodborne disease and its prevention comes from detailed investigation of outbreaks. This is often how a new pathogen is identified, and this is how the critical information linking a pathogen to a specific food and animal reservoir is first gathered. The full investigation can require a team with multiple talents, including the epidemiologist, microbiologist, food sanitarian, food scientist, veterinarian, and factory process engineer.
How are outbreaks of foodborne disease detected?
The initial clue that an outbreak is occurring can come in various ways. It may be when a person realizes that several other people who were all together at an event have become ill and he or she calls the local health department. It may be when a physician realizes she has seen more than the usual number of patients with the same illness. It may be when a county health department gets an unusually large number of reports of illness. The hardest outbreaks to detect are those that are spread over a large geographic area, with only a few cases in each state. These outbreaks can be detected by combining surveillance reports at the regional or national level and looking for increases in infections of a specific type. This is why state public health laboratories determine the serotype of Salmonella bacteria isolated from people. New "DNA fingerprinting" technologies can make detecting outbreaks easier too. For example, the new molecular subtyping network, PulseNet, allows state laboratories and CDC to compare strains of E. coli O157:H7 and an increasing number of other pathogens from all across the United States to detect widespread outbreaks.
After an apparent cluster of cases is detected, it is important to determine whether these cases represent a real increase above the expected number of cases and whether they really might be related. Sometimes a cluster of reported cases is caused by something other than an actual outbreak of illness. For example, if the person responsible for reporting has just returned from a vacation and is clearing up a backlog of cases by reporting them all at once, the sudden surge of reports is just a false cluster.
How is a foodborne disease outbreak investigated?
Once an outbreak is strongly suspected, an investigation begins. A search is made for more cases among persons who may have been exposed. The symptoms and time of onset, and location of possible cases is determined, and a "case definition" is developed that describes these typical cases. The outbreak is systematically described by time, place, and person. A graph is drawn of the number of people who fell ill on each successive day to show pictorially when it occurred. A map of where the ill people live, work, or eat may be helpful to show where it occurred. Calculating the distribution of cases by age and sex shows who is affected. If the causative microbe is not known, samples of stool or blood are collected from ill people and sent to the public health laboratory to make the diagnosis.
To identify the food or other source of the outbreak, the investigators first interview a few persons with the most typical cases about exposures they may have had in the few days before they got sick. In this way, certain potential exposures may be excluded while others that are mentioned repeatedly emerge as possibilities. Combined with other information, such as the likely sources for the specific microbe involved, these hypotheses are then tested in a formal epidemiologic investigation. The investigators conduct systematic interviews about a list of possible exposures with the ill persons, and with a comparable group people who are not ill. By comparing how often an exposure is reported by ill people and by well people, investigators can measure the association of the exposure with illness. Using probability statistics, similar to those used to describe coin flips, the probability of no association is directly calculated.
For example, imagine that an outbreak has occurred after a catered event. Initial investigation suggested that Hollandaise sauce was eaten by at least some of the attendees, so it is on the list of possible hypotheses. Now, we interview 20 persons who attended the affair, 10 of whom became ill and 10 who remained well. Each ill or well person is interviewed about whether or not they ate the Hollandaise sauce, as well as various other food items. If half the people ate the sauce, but the sauce was not associated with the illness, then we would expect each person to have a 50/50 chance of reporting that they ate it, regardless of whether they were ill or not. Suppose, however, that we find that all 10 ill people but none of the well persons reported eating Hollandaise sauce at the event? This would be very unlikely to occur by chance alone if eating the Hollandaise sauce were not somehow related to the risk of illness. In fact, it would be about as unlikely as getting heads ten times in a row by flipping a coin (That is 50% multiplied by itself 10 times over, or a chance of just under 1 in 1000). So the epidemiologist concludes that eating the Hollandaise sauce was very likely to be associated with the risk of illness. Note that the investigator can draw this conclusion even though there is no Hollandaise sauce left to test in a laboratory. The association is even stronger if she can show that those who ate second helpings of Hollandaise were even more likely to become ill, or that persons who ate leftover Hollandaise sauce that went home in doggie bags also became ill.
Once a food item is statistically implicated in this manner, further investigation into its ingredients and preparation, and microbiologic culture of leftover ingredients or the food itself (if available) may provide additional information about the nature of contamination. Perhaps the Hollandaise sauce was made using raw eggs. The source of the raw eggs can be determined, and it may even be possible to trace them back to the farm and show that chickens on the farm are carrying the same strain of Salmonella in their ovaries. If so, the eggs from that farm can be pasteurized to prevent them from causing other outbreaks.
Some might think that the best investigation method would be just to culture all the leftover foods in the kitchen, and conclude that the one that is positive is the one that caused the outbreak. The trouble is that this can be misleading, because it happens after the fact. What if the Hollandaise sauce is all gone, but the spoon that was in the sauce got placed in potato salad that was not served at the function? Now, cultures of the potato salad yield a pathogen, and the unwary tester might call that the source of the outbreak, even though the potato salad had nothing to do with it. This means that laboratory testing without epidemiologic investigation can lead to the wrong conclusion.
Even without isolating microbes from food, a well-conducted epidemiologic investigation can guide immediate efforts to control the outbreak. A strong and consistent statistical association between illness and a particular food item that explains the distribution of the outbreak in time, place and person should be acted upon immediately to stop further illness from occurring.
An outbreak ends when the critical exposure stops. This may happen because all the contaminated food is eaten or recalled, because a restaurant is closed or a food processor shuts down or changes its procedures, or an infected food handler is no longer infectious or is no longer working with food. An investigation that clarifies the nature and mechanism of contamination can provide critical information even if the outbreak is over. Understanding the contamination event well enough to prevent it can guide the decision to resume usual operations, and lead to more general prevention measures that reduce the risk of similar outbreaks happening elsewhere.
How does food become contaminated?
We live in a microbial world, and there are many opportunities for food to become contaminated as it is produced and prepared. Many foodborne microbes are present in healthy animals (usually in their intestines) raised for food. Meat and poultry carcasses can become contaminated during slaughter by contact with small amounts of intestinal contents. Similarly, fresh fruits and vegetables can be contaminated if they are washed or irrigated with water that is contaminated with animal manure or human sewage. Some types of Salmonella can infect a hen's ovary so that the internal contents of a normal looking egg can be contaminated with Salmonella even before the shell in formed. Oysters and other filter feeding shellfish can concentrate Vibrio bacteria that are naturally present in sea water, or other microbes that are present in human sewage dumped into the sea.
Later in food processing, other foodborne microbes can be introduced from infected humans who handle the food, or by cross contamination from some other raw agricultural product. For example, Shigella bacteria, hepatitis A virus and Norwalk virus can be introduced by the unwashed hands of food handlers who are themselves infected. In the kitchen, microbes can be transferred from one food to another food by using the same knife, cutting board or other utensil to prepare both without washing the surface or utensil in between. A food that is fully cooked can become recontaminated if it touches other raw foods or drippings from raw foods that contain pathogens.
The way that food is handled after it is contaminated can also make a difference in whether or not an outbreak occurs. Many bacterial microbes need to multiply to a larger number before enough are present in food to cause disease. Given warm moist conditions and an ample supply of nutrients, one bacterium that reproduces by dividing itself every half hour can produce 17 million progeny in 12 hours. As a result, lightly contaminated food left out overnight can be highly infectious by the next day. If the food were refrigerated promptly, the bacteria would not multiply at all. In general, refrigeration or freezing prevents virtually all bacteria from growing but generally preserves them in a state of suspended animation. This general rule has a few surprising exceptions. Two foodborne bacteria, Listeria monocytogenes and Yersinia enterocolitica can actually grow at refrigerator temperatures. High salt, high sugar or high acid levels keep bacteria from growing, which is why salted meats, jam, and pickled vegetables are traditional preserved foods.
Microbes are killed by heat. If food is heated to an internal temperature above 160oF, or 78oC, for even a few seconds this sufficient to kill parasites, viruses or bacteria, except for the Clostridium bacteria, which produce a heat-resistant form called a spore. Clostridium spores are killed only at temperatures above boiling. This is why canned foods must be cooked to a high temperature under pressure as part of the canning process.
The toxins produced by bacteria vary in their sensitivity to heat. The staphylococcal toxin which causes vomiting is not inactivated even if it is boiled. Fortunately, the potent toxin that causes botulism is completely inactivated by boiling.
What foods are most associated with foodborne illness?
Raw foods of animal origin are the most likely to be contaminated; that is, raw meat and poultry, raw eggs, unpasteurized milk, and raw shellfish. Because filter-feeding shellfish strain microbes from the sea over many months, they are particularly likely to be contaminated if there are any pathogens in the seawater. Foods that mingle the products of many individual animals, such as bulk raw milk, pooled raw eggs, or ground beef, are particularly hazardous because a pathogen present in any one of the animals may contaminate the whole batch. A single hamburger may contain meat from hundreds of animals. A single restaurant omelet may contain eggs from hundreds of chickens. A glass of raw milk may contain milk from hundreds of cows. A broiler chicken carcass can be exposed to the drippings and juices of many thousands of other birds that went through the same cold water tank after slaughter.
Fruits and vegetables consumed raw are a particular concern. Washing can decrease but not eliminate contamination, so the consumers can do little to protect themselves. Recently, a number of outbreak have been traced to fresh fruits and vegetables that were processed under less than sanitary conditions. These outbreaks show that the quality of the water used for washing and chilling the produce after it is harvested is critical. Using water that is not clean can contaminate many boxes of produce. Fresh manure used to fertilize vegetables can also contaminate them. Alfalfa sprouts and other raw sprouts pose a particular challenge, as the conditions under which they are sprouted are ideal for growing microbes as well as sprouts, and because they are eaten without further cooking. That means that a few bacteria present on the seeds can grow to high numbers of pathogens on the sprouts. Unpasteurized fruit juice can also be contaminated if there are pathogens in or on the fruit that is used to make it.
What can consumers do to protect themselves from foodborne illness?
A few simple precautions can reduce the risk of foodborne diseases:
COOK meat, poultry and eggs thoroughly. Using a thermometer to measure the internal temperature of meat is a good way to be sure that it is cooked sufficiently to kill bacteria. For example, ground beef should be cooked to an internal temperature of 160o F. Eggs should be cooked until the yolk is firm.
SEPARATE: Don't cross-contaminate one food with another. Avoid cross-contaminating foods by washing hands, utensils, and cutting boards after they have been in contact with raw meat or poultry and before they touch another food. Put cooked meat on a clean platter, rather back on one that held the raw meat.
CHILL: Refrigerate leftovers promptly. Bacteria can grow quickly at room temperature, so refrigerate leftover foods if they are not going to be eaten within 4 hours. Large volumes of food will cool more quickly if they are divided into several shallow containers for refrigeration.
CLEAN: Wash produce. Rinse fresh fruits and vegetables in running tap water to remove visible dirt and grime. Remove and discard the outermost leaves of a head of lettuce or cabbage. Because bacteria can grow well on the cut surface of fruit or vegetable, be careful not to contaminate these foods while slicing them up on the cutting board, and avoid leaving cut produce at room temperature for many hours. Don't be a source of foodborne illness yourself. Wash your hands with soap and water before preparing food. Avoid preparing food for others if you yourself have a diarrheal illness. Changing a baby's diaper while preparing food is a bad idea that can easily spread illness.
REPORT: Report suspected foodborne illnesses to your local health department. The local public health department is an important part of the food safety system. Often calls from concerned citizens are how outbreaks are first detected. If a public health official contacts you to find our more about an illness you had, your cooperation is important. In public health investigations, it can be as important to talk to healthy people as to ill people. Your cooperation may be needed even if you are not ill.
Are some people more likely to contract a foodborne illness? If so, are there special precautions they should take?
Some persons at particularly high risk should take more precautions.
- Pregnant women, the elderly, and those weakened immune systems are at higher risk for severe infections such as Listeria and should be particularly careful not to consume undercooked animal products. They should avoid soft French style cheeses, pates, uncooked hot dogs and sliced deli meats, which have been sources of Listeria infections. Persons at high risk should also avoid alfalfa sprouts and unpasteurized juices.
- A bottle-fed infant is at higher risk for severe infections with Salmonella or other bacteria that can grow in a bottle of warm formula if it is left at room temperature for many hours. Particular care is needed to be sure the baby's bottle is cleaned and disinfected and that leftover milk formula or juice is not held in the bottle for many hours.
- Persons with liver disease are susceptible to infections with a rare but dangerous microbe called Vibrio vulnificus, found in oysters. They should avoid eating raw oysters.
What can consumers do when they eat in restaurants?
You can protect yourself first by choosing which restaurant to patronize. Restaurants are inspected by the local health department to make sure they are clean and have adequate kitchen facilities. Find out how restaurants did on their most recent inspections, and use that score to help guide your choice. In many jurisdictions, the latest inspection score is posted in the restaurant. Some restaurants have specifically trained their staff in principles of food safety. This is also good to know in deciding which restaurant to patronize.
You can also protect yourself from foodborne disease when ordering specific foods, just as you would at home. When ordering a hamburger, ask for it to be cooked to a temperature of 160oF and send it back if it is still pink in the middle. Before you order something that is made with many eggs pooled together, such as scrambled eggs, omelets or French toast, ask the waiter whether it was made with pasteurized egg, and choose something else if it was not.
There is only so much the consumer can do. How can food be made safer in the first place?
Making food safe in the first place is a major effort, involving the farm and fishery, the production plant or factory, and many other points from the farm to the table. Many different groups in public health, industry, regulatory agencies, and academia have roles to play in making the food supply less contaminated. Consumers can promote general food safety with their dollars, by purchasing foods that have been processed for safety. For example, milk pasteurization was a major advance in food safety that was developed 100 years ago. Buying pasteurized milk rather than raw unpasteurized milk still prevents an enormous number of foodborne diseases every day. Now juice pasteurization is a recent important step forward that prevents E. coli O157:H7 infections and many other diseases. Consumers can look for and buy pasteurized fruit juices and ciders. In the future, meat and other foods will be available that has been treated for safety with irradiation. These new technologies are likely to be as important a step forward as the pasteurization of milk.
Foodborne diseases are largely preventable, though there is no simple one-step prevention measure like a vaccine. Instead, measures are needed to prevent or limit contamination all the way from farm to table. A variety of good agricultural and manufacturing practices can reduce the spread of microbes among animals and prevent the contamination of foods. Careful review of the whole food production process can identify the principal hazards, and the control points where contamination can be prevented, limited, or eliminated. A formal method for evaluating the control of risk in foods exists is called the Hazard Analysis Critical Control Point, or HACCP system. This was first developed by NASA to make sure that the food eaten by astronauts was safe. HACCP safety principles are now being applied to an increasing spectrum of foods, including meat, poultry, and seafood.
For some particularly risky foods, even the most careful hygiene and sanitation are insufficient to prevent contamination, and a definitive microbe-killing step must be included in the process. For example, early in the century, large botulism outbreaks occurred when canned foods were cooked insufficiently to kill the botulism spores. After research was done to find out exactly how much heat was needed to kill the spores, the canning industry and the government regulators went to great lengths to be sure every can was sufficiently cooked. As a result, botulism related to commercial canned foods has disappeared in this country. Similarly the introduction of careful pasteurization of milk eliminated a large number of milk-borne diseases. This occurred after sanitation in dairies had already reached a high level. In the future, other foods can be made much safer by new pasteurizing technologies, such as in-shell pasteurization of eggs, and irradiation of ground beef. Just as with milk, these new technologies should be implemented in addition to good sanitation, not as a replacement for it.
In the end, it is up to the consumer to demand a safe food supply; up to industry to produce it; up to researchers to develop better ways of doing so; and up to government to see that it happens, to make sure it works and to identify problems still in need of solutions.
What is CDC doing to control and prevent foodborne disease?
CDC is part of the U. S. Public Health Service, with a mission to use the best scientific information to monitor, investigate, control and prevent public health problems. Using the tools of epidemiology and laboratory science, CDC provides scientific assessment of public health threats. CDC works closely with state health departments to monitor the frequency of specific diseases and conducts national surveillance for them. CDC provides expert epidemiologic and microbiologic consultation to health departments and other federal agencies on a variety of public health issues, including foodborne disease, and it stations epidemiologists in state health departments to help with the surveillance and investigation of many problems. CDC can also send a team into the field to conduct emergency field investigations of large or unusual outbreaks, in collaboration with state public health officials. CDC researchers develop new methods for identifying, characterizing and fingerprinting the microbes that cause disease. We translate laboratory research into practical field methods that can be used by public health authorities in States and counties.
CDC is not a regulatory agency. Government regulation of food safety is carried out by the Food and Drug Administration (FDA) , the U.S. Department of Agriculture (USDA), the National Marine Fisheries Service, and other regulatory agencies. CDC maintains regular contact with the regulatory agencies.
When new public health threats appear, CDC learns what they are and how they can be controlled through rapid scientific field and laboratory investigation. CDC shares the results of these investigations with the states, with the regulatory federal agencies and with the industries themselves. Although we do not regulate the safety of food, CDC assesses the effectiveness of current prevention efforts. We provide independent scientific assessment of what the problems are, how they can be controlled, and of where there are gaps in our knowledge.
What are some unsolved problems in foodborne disease?
As new foodborne problems emerge, several questions need to be answered before the problem can be successfully controlled. It takes careful scientific observation and research to answer these questions. Some pressing unanswered questions include:
How do the foodborne pathogens spread among the animals themselves, and how can this be prevented? This includes E. coli O157:H7 among cattle, Salmonella Enteritis among egg-laying hens, and Campylobacter in broiler chickens. If we could prevent the animals from becoming infected in the first place, we would not have as much illness in the humans who eat them. What is the microbial cause of outbreaks in which no pathogen can be identified by current methods? This is true for over half of the reported foodborne outbreaks. Will wider application of existing experimental diagnostic methods help, or are these outbreaks caused by pathogens we simply do not yet know how to identify? What would be the impact of basic food safety education of restaurant workers on the risk of foodborne disease among restaurant patrons? How can the food and water that animals consume be made safer? How can we dispose of animal manure usefully, without threatening the food supply and the environment? How can basic food safety principles be most effectively taught to school children? How can we be sure food safety standards in other countries are as good as those in the United States? As we import more of our fresh foods from other countries, we need to be confident that they are produced with the same level of safety as food in the United States. What control strategies in the slaughter plant will reduce the contamination of poultry meat with Campylobacter? How can irradiation pasteurization of certain high risk foods, such as ground beef, be used most effectively? How do raspberries in Central America get contaminated with Cyclospora in the first place? Does this parasite have an animal reservoir? How can alfalfa sprouts and other raw sprouts be produced safely? Sprouts are unique among foods in that the conditions for sprouting are also perfect for bacterial growth, and they are not cooked after that.
Keeping Food-Borne Illnesses at Bay
By Jane E. Brody : NY Times : August 26, 2013
Each year, one in six Americans becomes sick from eating contaminated food. But while outbreaks of food-borne illness linked to processing plants or imported products capture the public’s attention and raise fears about the safety of the food supply, as many as 70 percent of food poisoning cases originate in the kitchen.
People, not products, are the main cause of food-borne illnesses, and they can be avoided by following certain basic principles of food safety.
Unfortunately, some of the best advice, like using disposable paper towels in place of reusable cloths and sponges, butts headfirst against modern efforts to be “green.” Other measures, like discarding leftovers after two days, are antithetical to the “waste not, want not” philosophy I was raised on. (Just before writing this paragraph, I reheated and ate a plate of delicious well-cooked leftovers that I had prepared for a dinner party six days earlier and promptly refrigerated.)
Still, there are many noncontentious steps that can be taken to minimize the risk that anyone will be sickened by the food you buy and prepare.
SHOPPING
Seek stores that are clean, well-organized and appear to have high product turnover: you can tell partly by checking the expiration and sell-by dates on the goods. Reject expired products and those in damaged or leaking packages. Don’t buy more perishables than you can use.
Pick up dry products first, then those that should be kept cold or frozen. In warm weather, or if there will be delays getting home, bring a cooler with ice or a freezer pack to keep items cold. Put all raw meats, poultry and fish in separate plastic bags before placing them in the shopping cart. At checkout, have them bagged separately from the dry foods and produce.
STORAGE
Separate raw meats, poultry and fish from other foods in the refrigerator, placing them on the lowest shelf, in a bin or on a tray to prevent dripping. Freeze meats that will not be cooked within two or three days. Use eggs within three to five weeks of purchase. In the pantry, place newly bought products behind older ones, which should be used first.
Place thermometers in the refrigerator and freezer, if they are not built in. Make sure the temperatures are at or below 40 degrees in the refrigerator and 2 degrees in the freezer. Defrost all uncooked foods in the refrigerator, the microwave or in a bowl of ice water.
PREPARATION
Start by washing your hands with soap and warm water. Pin long hair back or cover it; remove rings and bracelets, and put on a clean apron.
If you should sneeze, have to blow your nose or use the bathroom while working with food, wash your hands again. Half of people harbor the infectious Staphylococcus bacteria in their nasal passages. Also wash if you pet the dog or hand-feed it while preparing food.
Wash all produce, including melons, lemons and limes and fruits that will be peeled, before picking up a knife. If the fruit’s surface contains infectious organisms, they can spread to its flesh when the fruit is cut.
Although some suggest that poultry and meats not be rinsed lest they contaminate the sink, I find that hard to avoid. Instead, I rinse them, then clean the sink with a bleach spray. And I do use clean paper towels to dry raw food.
Work on well-washed cutting boards, using separate ones for produce and raw animal products. I use plastic boards that can be cleaned with a bleach spray or in the dishwasher, but wood is fine as long as all implements and boards are washed immediately after each chore. Never reuse an unwashed knife, plate or board on cooked food that was in contact with raw food without washing it first. Cross-contamination from raw to cooked food is a common cause of food-borne illness.
If making dishes a day or more ahead, cover them well, chill them quickly, and keep them cold until it is time to reheat or serve.
COOKING
You can’t always tell if a food is contaminated by its appearance: foods containing harmful organisms can look, smell and taste O.K. A goal of cooking is to destroy most infectious organisms.
It’s best to use a food thermometer and to heed recommended final temperatures when preparing meats, poultry, fish and seafood, and eggs. Whole cuts of beef, veal and lamb should be cooked to an internal temperature of 145 degrees, followed by a three-minute rest off the heat; pork and fresh ham should reach 145 degrees, followed by a three-minute rest (heat precooked ham to 140 degrees).
Ground meats should reach 160 degrees; poultry (whole or ground), 165 degrees and fish, 145 degrees (or until it is opaque and separates easily with a fork). Shrimp, lobster and crab should be cooked until the flesh is pearly and opaque. Clams, mussels and oysters should be cooked until the shells open, and scallops until the flesh is milky white or opaque and firm. Cook eggs until the yolk and white are firm, and cook egg dishes to 160 degrees.
If a recipe calls for raw or partly cooked eggs in a dish that will not be cooked (like eggnog, mayonnaise or Caesar salad dressing), use only pasteurized eggs, which are available in most large markets.
If you taste a dish while cooking, use a clean spoon each time.
If serving foods buffet-style over a period of hours, use hot plates or cold trays. Leftovers should be refrigerated as soon as possible. Reheat leftover meats and other animal products to 165 degrees.
CLEANING
You don’t have to become a clean freak; some exposure to infectious organisms is necessary for a healthy immune system. But do take steps to reduce the risk of food-borne illness.
Kitchen sponges and dishcloths are notorious for harboring and breeding germs. Wash them often in the dishwasher or in the sink with hot, soapy water, or clean them with a bleach solution. Never wipe the floor with sponges used on countertops and food preparation equipment.Consider investing in a large package of microfiber cloths. Use separate cloths for the floor, counters and to dry utensils. Put soiled cloths in the laundry.
When hand-washing dishes and pots, use very hot water and put them on a rack to air-dry. Damp dish towels can harbor bacteria.
Thoroughly clean the refrigerator, stovetop and countertops often. I use a bleach solution on most surfaces, especially those that come in contact with foods.
By Jane E. Brody : NY Times : August 26, 2013
Each year, one in six Americans becomes sick from eating contaminated food. But while outbreaks of food-borne illness linked to processing plants or imported products capture the public’s attention and raise fears about the safety of the food supply, as many as 70 percent of food poisoning cases originate in the kitchen.
People, not products, are the main cause of food-borne illnesses, and they can be avoided by following certain basic principles of food safety.
Unfortunately, some of the best advice, like using disposable paper towels in place of reusable cloths and sponges, butts headfirst against modern efforts to be “green.” Other measures, like discarding leftovers after two days, are antithetical to the “waste not, want not” philosophy I was raised on. (Just before writing this paragraph, I reheated and ate a plate of delicious well-cooked leftovers that I had prepared for a dinner party six days earlier and promptly refrigerated.)
Still, there are many noncontentious steps that can be taken to minimize the risk that anyone will be sickened by the food you buy and prepare.
SHOPPING
Seek stores that are clean, well-organized and appear to have high product turnover: you can tell partly by checking the expiration and sell-by dates on the goods. Reject expired products and those in damaged or leaking packages. Don’t buy more perishables than you can use.
Pick up dry products first, then those that should be kept cold or frozen. In warm weather, or if there will be delays getting home, bring a cooler with ice or a freezer pack to keep items cold. Put all raw meats, poultry and fish in separate plastic bags before placing them in the shopping cart. At checkout, have them bagged separately from the dry foods and produce.
STORAGE
Separate raw meats, poultry and fish from other foods in the refrigerator, placing them on the lowest shelf, in a bin or on a tray to prevent dripping. Freeze meats that will not be cooked within two or three days. Use eggs within three to five weeks of purchase. In the pantry, place newly bought products behind older ones, which should be used first.
Place thermometers in the refrigerator and freezer, if they are not built in. Make sure the temperatures are at or below 40 degrees in the refrigerator and 2 degrees in the freezer. Defrost all uncooked foods in the refrigerator, the microwave or in a bowl of ice water.
PREPARATION
Start by washing your hands with soap and warm water. Pin long hair back or cover it; remove rings and bracelets, and put on a clean apron.
If you should sneeze, have to blow your nose or use the bathroom while working with food, wash your hands again. Half of people harbor the infectious Staphylococcus bacteria in their nasal passages. Also wash if you pet the dog or hand-feed it while preparing food.
Wash all produce, including melons, lemons and limes and fruits that will be peeled, before picking up a knife. If the fruit’s surface contains infectious organisms, they can spread to its flesh when the fruit is cut.
Although some suggest that poultry and meats not be rinsed lest they contaminate the sink, I find that hard to avoid. Instead, I rinse them, then clean the sink with a bleach spray. And I do use clean paper towels to dry raw food.
Work on well-washed cutting boards, using separate ones for produce and raw animal products. I use plastic boards that can be cleaned with a bleach spray or in the dishwasher, but wood is fine as long as all implements and boards are washed immediately after each chore. Never reuse an unwashed knife, plate or board on cooked food that was in contact with raw food without washing it first. Cross-contamination from raw to cooked food is a common cause of food-borne illness.
If making dishes a day or more ahead, cover them well, chill them quickly, and keep them cold until it is time to reheat or serve.
COOKING
You can’t always tell if a food is contaminated by its appearance: foods containing harmful organisms can look, smell and taste O.K. A goal of cooking is to destroy most infectious organisms.
It’s best to use a food thermometer and to heed recommended final temperatures when preparing meats, poultry, fish and seafood, and eggs. Whole cuts of beef, veal and lamb should be cooked to an internal temperature of 145 degrees, followed by a three-minute rest off the heat; pork and fresh ham should reach 145 degrees, followed by a three-minute rest (heat precooked ham to 140 degrees).
Ground meats should reach 160 degrees; poultry (whole or ground), 165 degrees and fish, 145 degrees (or until it is opaque and separates easily with a fork). Shrimp, lobster and crab should be cooked until the flesh is pearly and opaque. Clams, mussels and oysters should be cooked until the shells open, and scallops until the flesh is milky white or opaque and firm. Cook eggs until the yolk and white are firm, and cook egg dishes to 160 degrees.
If a recipe calls for raw or partly cooked eggs in a dish that will not be cooked (like eggnog, mayonnaise or Caesar salad dressing), use only pasteurized eggs, which are available in most large markets.
If you taste a dish while cooking, use a clean spoon each time.
If serving foods buffet-style over a period of hours, use hot plates or cold trays. Leftovers should be refrigerated as soon as possible. Reheat leftover meats and other animal products to 165 degrees.
CLEANING
You don’t have to become a clean freak; some exposure to infectious organisms is necessary for a healthy immune system. But do take steps to reduce the risk of food-borne illness.
Kitchen sponges and dishcloths are notorious for harboring and breeding germs. Wash them often in the dishwasher or in the sink with hot, soapy water, or clean them with a bleach solution. Never wipe the floor with sponges used on countertops and food preparation equipment.Consider investing in a large package of microfiber cloths. Use separate cloths for the floor, counters and to dry utensils. Put soiled cloths in the laundry.
When hand-washing dishes and pots, use very hot water and put them on a rack to air-dry. Damp dish towels can harbor bacteria.
Thoroughly clean the refrigerator, stovetop and countertops often. I use a bleach solution on most surfaces, especially those that come in contact with foods.